Abstract
Poor perinatal mental health is a common pregnancy-related morbidity with potentially serious impacts that extend beyond the individual to their family. A possible contributing factor to poor perinatal mental health is discontinuity in health insurance coverage, which is particularly important among low-income people. We examined impacts of Medicaid expansion on prepregnancy depression screening and self-reported depression and postpartum depressive symptoms and well-being among low-income people giving birth. Medicaid expansion was associated with a 16 percent decline in self-reported prepregnancy depression but was not associated with postpartum depressive symptoms or well-being. Associations between Medicaid expansion and prepregnancy mental health measures increased with time since expansion. Expanding health insurance coverage to low-income people before pregnancy may improve perinatal mental health.
Poor perinatal mental health is a common pregnancy-related morbidity, affecting between 13 percent1 and 25 percent2 of people who have recently given birth, with higher prevalence among low-income birthing people.3,4 Mental health is central to the well-being of the birthing person, their children, and their family, and if left untreated, poor perinatal mental health may lead to detrimental and cascading sequelae including mortality during pregnancy and the first year postpartum.5
Having health insurance before, during, and after pregnancy is plausibly an important determinant of perinatal mental health because insurance increases one’s ability to obtain timely and effective care. However, many pregnant and birthing people, particularly those with low incomes, do not have health insurance or experience changes or lapses in health insurance coverage before, during, or after pregnancy.6 As a result, uninsured (or underinsured) pregnant and birthing people might not be able to obtain the care required to detect and treat poor mental health. A lack of health insurance is also associated with financial distress,7 which may cause or exacerbate poor mental health.
Before 2010 Medicaid eligibility in most states was limited to children, parents of dependent children, pregnant people, people with disabilities, and people age sixty-five or older whose household incomes fell below a certain threshold (often varying by state).8 As of April 1990 all fifty states were required to provide Medicaid to pregnant people with household incomes up to 133 percent of the federal poverty level,8 although many states used higher income cutoffs (for example, by 2003 Iowa used a cutoff of 200 percent of poverty and now uses a cutoff of 380 percent).9 Yet in most states, before the Affordable Care Act (ACA), there were no income eligibility thresholds for nonpregnant, nondisabled adults with no dependent children.10 This remains the case in states that did not expand Medicaid under the ACA,10 meaning that low-income people in these states may lack insurance before pregnancy and thus lack access to preconception care. Moreover, birthing people who qualify for Medicaid during pregnancy typically lose pregnancy-related Medicaid coverage after sixty days postpartum6 and must requalify under parental income guidelines (which are often less generous), find alternative insurance, or go without.6 In fact, during the period 2005–13, 65 percent of pregnant people with Medicaid in the month of delivery were uninsured for at least one month in the nine months before delivery, and only 41 percent had the same type of insurance six months after delivery.6
Under the ACA, thirty-two states plus Washington, D.C., expanded Medicaid to adults with household incomes less than 138 percent of poverty between 2014 and 2016, and an additional seven states are expected to expand Medicaid by the end of 2021.11 Prior studies demonstrate that these Medicaid expansions increased insurance coverage among women of reproductive age,12,13 increased preconception Medicaid coverage,14 and increased continuity of health care during the perinatal period.15 Medicaid expansions have also been linked to reduced self-reported psychological distress16 and days of poor mental health17 in low-income adults. To our knowledge, however, no prior work has examined whether Medicaid expansion affected perinatal mental health. In this study we tested the hypothesis that the ACA Medicaid expansions improved measures of prepregnancy mental health screening and self-reported depression, as well as postpartum depressive symptoms.
Study Data And Methods
OVERVIEW
We used a difference-in-differences study design, which estimates the change in outcomes post–Medicaid expansion compared with preexpansion among pregnant people in expansion states compared with those in nonexpansion states. States expanding Medicaid during January–April 2014 are defined as expansion states (see online appendix exhibit A1).18 For prepregnancy mental health measures, we defined exposure to Medicaid expansion based on conception year (determined by date of birth minus length of gestation), and for postpartum mental health measures, we defined exposure based on birth year. For both sets of measures, 2014–18 was considered postexpansion.
DATA AND SAMPLE
We used data from the Pregnancy Risk Assessment Monitoring System (PRAMS) phases 7 (2012–15) and 8 (2016–18). PRAMS is a compendium of state surveys—with each survey representative of people in that state who had a recent live birth—that obtain information about experiences before, during, and shortly after pregnancy.We included in our sample people likely eligible for Medicaid under ACA expansions (appendix exhibit A2).18 That is, we included respondents age eighteen or older whose reported household income category included a value equal to or less than 137 percent of poverty. (The PRAMS income categories included some people with incomes greater than 137 percent of poverty but did not include anyone with incomes greater than 200 percent of poverty.) We thus ensured that we captured information on all people likely eligible for Medicaid even though we also captured information on some ineligible people.
We excluded observations with missing information on key covariates, and we excluded residents of states that expanded Medicaid income eligibility before or after 2014 (appendix exhibit A2).18
Ideally, to produce the most nationally generalizable estimates, we would have included all forty-four of the states in PRAMS to study the effects of Medicaid expansion. However, not all states contributed data in every year, resulting in an unbalanced panel of states (appendix exhibit A1).18 To address this, we grouped conception and birth years into one-to-three-year periods, each of which is exclusively pre- or postexpansion. The groupings resulted in a balanced panel of states that contributed data in all periods. Conception years are grouped as 2011–12, 2013, 2014, 2015–16, and 2017–18; birth years are grouped as 2012, 2013, 2014–15, and 2016–18.
Our final analytic sample included 54,977 observations in seventeen states for prepregnancy mental health measures and 56,965 observations in eighteen states for postpartum mental health measures. Missing data for each outcome made up less than 3 percent of the sample (appendix exhibit A2).18
OUTCOMES
We examined Medicaid insurance coverage before pregnancy and at the time of the survey. We examined two measures of prepregnancy mental health: depression screening and self-reported depression. (For screening, PRAMS phase 7 asked whether the respondent was “checked for depression,” and phase 8 asked whether the respondent was asked about depressive symptoms during the twelve months before pregnancy. For self-reported depression, phase 7 asked whether the participant was told by a health care worker before pregnancy that they had depression, and phase 8 asked whether the respondent had depression in the three months before pregnancy.) To account for changes in these measures between survey waves, we controlled for survey wave in our analyses.
Finally, we measured postpartum depressive symptoms as answering “Always” or “Often” to questions about how often mothers “felt down, depressed, or hopeless” or “had little interest or pleasure in doing things” since their babies were born. We defined postpartum well-being as answering “Never” or “Rarely” to both items (methods appendix A1).18
STATISTICAL ANALYSIS
We calculated the unadjusted means and differences for key sociodemographic covariates and outcomes overall and stratified by state Medicaid expansion status in the pre- and postexpansion periods. We then used generalized difference in differences and event study research designs to estimate the association between time since Medicaid expansion and prepregnancy and postpartum mental health measures. For prepregnancy outcomes we used multivariable, linear probability models that included interactions between each conception period, with 2013, the year before expansion, as the reference group and a binary variable indicating expansion status of the state. We also estimated a model where all postexpansion periods were combined (2014–18) as the treated group and all preexpansion periods were combined (2011–13) as the reference group. All models include fixed effects for state of residence, conception period, survey phase, and individual-level covariates. We used wild-cluster bootstrap standard errors to account for clustering of data by state and survey weights to account for the PRAMS sampling strategy. Postpartum outcomes were estimated similarly but using birth periods instead of conception periods. (See methods appendix A2 for statistical details.)18
We assessed the identification assumption of the difference-in-differences approach—that trends in outcomes were the same between expansion and nonexpansion states in the preexpansion period—by visually examining event study plots and by testing whether the preexpansion event study coefficients differed significantly from each other.
We conducted several robustness analyses (methods appendix A3).18 First we compared our findings with those from a balanced panel of states, having dropped all states that did not contribute to all years of data (fourteen states, n = 45,114 observations) and to a larger set of states (twenty-five states, n = 70,577 observations) containing those expanding Medicaid after 2014 and those that contributed data in most years. Second, we imputed Medicaid expansion eligibility based on demographics for the 10 percent of participants missing income and used imputed income to define our sample. Third, because income can be affected by changes in health insurance policies, we also reestimated our sample using a high school education or less to define eligibility. Fourth, we stratified our results by whether mothers had a previous live birth because mothers with other children have different Medicaid income eligibility guidelines in some states. Finally, we reestimated models without the use of survey weights.
LIMITATIONS
This study was subject to a number of limitations. First, our analyses were limited by the available information about mental health in the PRAMS surveys (for example, self-reported measures).We did not have medical record data that could confirm screening or diagnosis of depression, and a complete depressive symptom inventory such as the Edinburgh Postnatal Depression Scale was not included. However, the available questions are similar to those in the Patient Health Questionnaire-2, which is used to screen for major depression in community samples and has shown good validity,19 and previous research has used similar PRAMS survey data to examine postpartum maternal depressed mood and anhedonia.20 Second, the depression self-report question changed across survey phases. However, including survey phase fixed effects absorbed variation attributable to these differences in question format over time. Third, the measure of prepregnancy screening asks respondents about the twelve months before pregnancy, and conception year might not precisely reflect this time frame.
Fourth, our measure of postpartum well-being was not a validated measure. Fifth, as a result of the categorical reporting of income, our sample included some people with incomes of 138–200 percent of poverty who might not be eligible for Medicaid. Including those who might not have benefited from Medicaid expansion would likely bias our findings toward the null. Because income can be affected by changes in health insurance policies, we reestimated our sample including only participants with a high school education or less and found similar results. Sixth, because not all states contribute data to PRAMS in all years, our findings may not generalize beyond the states included in our analysis.
Study Results
Exhibit 1 presents selected descriptive statistics for our analytic sample. The sample was 49 percent non-Hispanic White, 18 percent non-Hispanic Black, 24 percent Hispanic, and less than 10 percent each non-Hispanic Native American, Native Alaskan, or Native Hawaiian; Asian; or mixed/other, based on self-reported race and ethnicity. About 27 percent of PRAMS respondents reported being screened for depression before pregnancy, 16 percent reported having depression before pregnancy, and 16 percent reported postpartum depressive symptoms. Before adjustment, Medicaid expansion was associated with increases in prepregnancy and postpartum Medicaid insurance coverage, declines in prepregnancy self-reported depression, and increases in prepregnancy screening and postpartum well-being.
EXHIBIT 1.
Prevalence of selected covariates and outcomes in the Pregnancy Risk Assessment Monitoring System sample of low-income birthing people, overall and by state Medicaid expansion status, 2012–18
| Covariates | Overall weighted mean | Expansion states |
Nonexpansion states |
Difference-in-differencesb | ||
|---|---|---|---|---|---|---|
| Preexpansion | Postexpansiona | Preexpansion | Postexpansiona | |||
| MATERNAL CHARACTERISTICS | ||||||
|
| ||||||
| Race and ethnicity | ||||||
| Whitec | 49.1% | 43.3% | 43.6% | 61.9% | 59.3% | 2.9*** |
| Blackc | 17.5 | 19.6 | 19.1 | 13.3 | 14.1 | −1.3*** |
| Hispanic | 24.4 | 29.0 | 28.6 | 14.7 | 15.9 | −1.6*** |
| Native American, Native Alaskan, Native Hawaiianc | 3.0 | 3.3 | 3.4 | 2.3 | 2.5 | −0.1*** |
| Asianc | 2.1 | 1.7 | 1.5 | 3.3 | 3.1 | 0.0*** |
| Mixed/otherc | 4.0 | 3.1 | 3.9 | 4.5 | 5.1 | 0.2*** |
| Marital status | ||||||
| Married | 40.1 | 39.2 | 40.2 | 40.7 | 40.8 | 0.9*** |
| Parity | ||||||
| Previous live birth | 69.7 | 69.1 | 70.6 | 68.5 | 69.4 | 0.6*** |
|
| ||||||
| OUTCOMES | ||||||
|
| ||||||
| Medicaid | ||||||
| Prepregnancy | 44.4% | 40.6% | 53.9% | 34.0% | 37.4% | 9.9*** |
| Postpartumd | 56.1 | 52.9 | 64.2 | 45.5 | 47.8 | 9.0*** |
| Mental health | ||||||
| Prepregnancy | ||||||
| Depression self-report | 16.3 | 12.3 | 16.5 | 15.9 | 22.1 | −2.0*** |
| Depression screening | 27.1 | 21.7 | 31.0 | 23.1 | 29.7 | 2.7*** |
| Postpartum | ||||||
| Depressive symptomsd | 16.3 | 15.2 | 15.5 | 17.6 | 18.6 | −0.7*** |
| Well-beingd | 68.2 | 68.8 | 71.5 | 62.6 | 63.4 | 1.9*** |
SOURCE Authors’ analysis of data from the Pregnancy Risk Assessment Monitoring System, 2012-18. NOTES N = 54,977 observations in seventeen states. Some conception periods are presented in two-year ranges because some states did not report data for all years; see the text for details.
All maternal characteristics and prepregnancy outcomes use the post period definition based on conception period, whereas postpartum outcomes use the post period definition based on birth period.
Crude difference-in-differences (percentage points) is the difference between prevalence in the preexpansion and postexpansion periods among expansion states minus the difference in nonexpansion states.
Non-Hispanic.
N = 56,965 observations in eighteen states.
p < 0.01
Exhibit 2 shows the percentage-point difference between expansion and nonexpansion states in prepregnancy mental health measures by year of conception after adjustment for state, conception period, survey phase, and individual covariates. The 2011–12 estimate was not statistically significantly different from the 2013 estimate, supporting the assumption of parallel trends in the outcomes before expansion. Similar plots for other outcome measures are in appendix exhibit A3.18
EXHIBIT 2. Changes in 2 prepregnancy mental health measures for low-income birthing people associated with Medicaid expansion, by conception period, 2011–18.
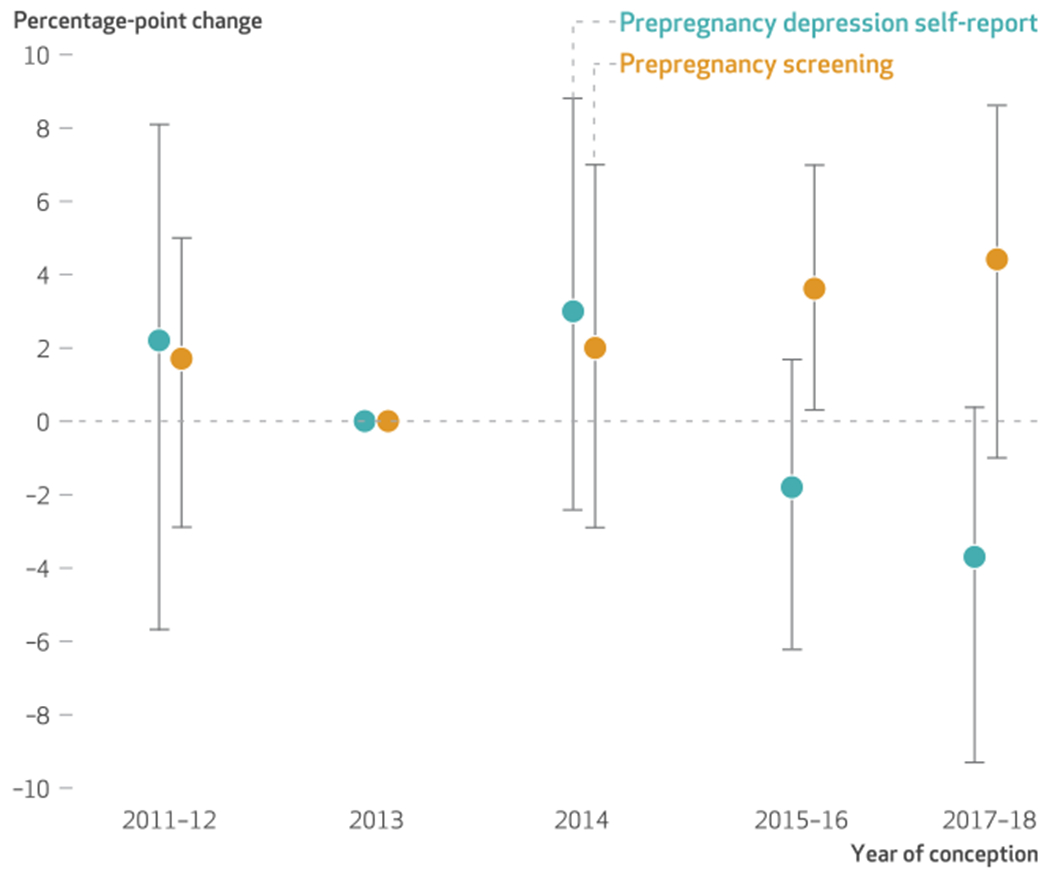
SOURCE Authors’ analysis of data from the Pregnancy Risk Assessment Monitoring System, 2012–18. NOTES N = 54,977. The exhibit shows percentage-point difference-in-differences estimates between Medicaid expansion and control states, adjusted for years of education, age, race and ethnicity, marital status, parity, survey phase, and state and year fixed effects. Some conception periods are presented in two-year ranges because some states did not report data for all years; see the text for details.
Medicaid expansion was associated with a 9.6-percentage-point increase in prepregnancy Medicaid insurance and a 2.5-percentage-point decrease in prepregnancy depression self-report overall for conceptions during 2014–18 (exhibit 3). Furthermore, the event-study analysis suggested that associations between Medicaid expansion prepregnancy mental health measures increased with time since expansion (exhibits 2 and 3). That is, Medicaid expansion was associated with a 1.8-percentage-point decrease in prepregnancy self-reported depression in 2015–16, which became a 3.7-percentage-point decrease in 2017–18. Expansion was associated with 2.0-percentage-point increase in prepregnancy depression screening in 2014, followed by increases of 3.6 and 4.4 percentage points in prepregnancy depression screening in 2015–16 and 2017–18, respectively. In general, Medicaid coverage did not increase in a linear fashion (see appendix exhibit A3, panel 1).18
EXHIBIT 3.
Changes in prepregnancy mental health measures for low-income birthing people associated with Medicaid expansion, by conception period, 2011–18
| Prepregnancy measuresa |
|||
|---|---|---|---|
| Conception periods | Medicaid coverage | Depression self-report | Screening |
| 2011–13 | Ref | Ref | Ref |
| 2014–18 versus 2011–13 | 9.6** | −2.5** | 2.3 |
|
| |||
| 2013 | Ref | Ref | Ref |
| 2011–12 versus 2013 | −3.3* | 2.2 | 1.7 |
| 2014 versus 2013 | 6.7* | 3.0 | 2.0 |
| 2015–16 versus 2013 | 6.8 | −1.8 | 3.6** |
| 2017–18 versus 2013 | 9.5** | −3.7* | 4.4* |
|
| |||
| Observationsb | 54,888 | 54,103 | 54,325 |
SOURCE Authors’ analysis of data from the Pregnancy Risk Assessment Monitoring System, 2012–18. NOTES N = 54,977 observations in seventeen states. Reference value is 0. Some conception periods are presented in two-year ranges because some states did not report data for all years; see the text for details.
Difference-in-differences estimates in percentage points. Models controlled for years of education, age, race and ethnicity, marital status, parity, survey phase, and state and year fixed effects.
Of these observations, 89 were missing Medicaid coverage, 874 were missing depression self-report, and 652 were missing screening.
p < 0.10
p < 0.05
Medicaid expansion was also associated with a 9.0-percentage-point increase in Medicaid coverage postpartum (exhibit 4). However, all associations between Medicaid expansion and postpartum depressive symptoms and our well-being measure were smaller than 1 percentage point and were not significant.
EXHIBIT 4.
Changes in postpartum measures for low-income birthing people associated with Medicaid expansion, by birth period, 2011-18
| Postpartum measuresa |
|||
|---|---|---|---|
| Birth periods | Medicaid coverage | Depressive symptoms | Well-being |
| 2011–13 | Ref | Ref | Ref |
| 2014–18 versus 2011–13 | 9.0* | −0.0 | 0.9 |
|
| |||
| 2013 | Ref | Ref | Ref |
| 2012 versus 2013 | −3.1* | −1.4 | −1.2 |
| 2014–15 versus 2013 | 8.6** | −0.4 | 0.4 |
| 2016–18 versus 2013 | 6.5 | −1.0 | 0.1 |
|
| |||
| Observationsb | 56,838 | 56,219 | 56,219 |
SOURCE Authors’ analysis of data from the Pregnancy Risk Assessment Monitoring System, 2012–18. NOTES N = 56,965 observations in eighteen states. Reference value is 0. Some birth periods are presented in two-year ranges because some states did not report data for all years; see the text for more details.
Difference-in-differences estimates in percentage points. Models controlled for years of education, age, race and ethnicity, marital status, parity, and state and year fixed effects.
Of these observations, 127 were missing Medicaid coverage, and 746 were missing depressive symptoms and well-being.
p < 0.10
p < 0.05
In the sample of balanced states, Medicaid expansion was associated with a significant increase in prepregnancy Medicaid coverage (11.4 percentage points; p < 0.05) and with a marginally significant increase in screening (2.4 percentage points; p < 0.10) and a decrease in self-reported depression (2.9 percentage points; p < 0.10) (appendix exhibit A6) but was not associated with postpartum mental health measures (appendix exhibit A7).18 When we looked at time since expansion, we found the largest impact of Medicaid expansion on both Medicaid coverage and prepregnancy screening when we compared 2017–18 with 2013 (10.5 and 5.3 percentage points, respectively; p < 0.10), but associations with prepregnancy self-reported depression were no longer significant. In other robustness analyses (appendix exhibit A8),18 we found similar results: Medicaid expansion before conception overall was associated with decreased prepregnancy self-reported depression, and these associations tended to increase over time.
Among people with no previous live births, Medicaid expansion was associated with decreased depressive symptoms. Among people with previous live births, Medicaid expansion was associated with increased prepregnancy screening for depression (appendix exhibit A8).18 In no specification was Medicaid expansion associated with substantial changes in postpartum outcomes (data not shown).
Discussion
In this study we tested the hypothesis that expansion of Medicaid under the ACA to low-income people improved measures of prepregnancy mental health screening and self-reported depression and postpartum depressive symptoms. Using survey data from low-income people giving birth between 2012 and 2018, we found that Medicaid expansion was significantly associated with a 9.6-percentage-point (22 percent) increase in prepregnancy Medicaid coverage, a 2.5-percentage-point (16 percent) decrease in self-reported prepregnancy depression, and a nonsignificant increase of 2.3 percentage points (9 percent) in prepregnancy screening for depression. With increasing time (three to four years) since Medicaid expansion, we found even larger associations between Medicaid expansion and prepregnancy depression (a 3.7-percentage-point decrease; p < 0.10) and screening (a 4.4-percentage-point increase; p < 0.10), although power declined with fewer observations in the smaller time increments. Medicaid expansion was not associated with substantial changes in postpartum depressive symptoms or well-being.
Our finding that Medicaid expansion decreased prepregnancy self-reported depression and may have increased prepregnancy screening for depression suggests that low-income people gaining Medicaid insurance used more preventive health care before pregnancy than those not gaining Medicaid coverage, or that insurance coverage and increased preventive care improve some measures of mental health. This is consistent with other research showing that Medicaid expansion was associated with increased access to and use of preventive care among low-income women of reproductive age12,13,21 and with findings from the Oregon Health Insurance Experiment, which found that Medicaid coverage reduced depressive symptoms22,23 and increased days in “good” mental health.23 The expansion of Medicaid coverage to parents in some states between 1998 and 2010 was also associated with reduced moderate (but not severe) psychological distress.16 Potential mechanisms by which health insurance may improve mental health include increased diagnosis and treatment (whether pharmaceutical or behavioral) or reduced financial distress. Notably, we also found that the decrease in self-reported depression occurred primarily among people with no previous live births, whereas the increase in prepregnancy screening occurred among people with a previous live birth. This finding may indicate that Medicaid expansion increases access to preventive care—and thus screening—during the interconception period between births.
Our analysis also suggests that impacts of Medicaid expansion on prepregnancy self-reported depression and screening increase over time. Although this increasing impact of the expansion on outcomes over time is consistent with other work showing rising rates of enrollment in Medicaid postexpansion,24 there is limited evidence in our data showing that prepregnancy enrollment in Medicaid increased in a linear fashion over time. Instead, our findings suggest that the pattern of increasing impacts of Medicaid expansion on prepregnancy self-reported depression and screening may reflect the cumulative effects of health insurance on individual-level access, utilization, and health, even in the absence of increased enrollment at the population level. Continuous health insurance during the perinatal period (compared with switching between private and public coverage or having periods of uninsurance) has been shown to increase the use of preventive care,25 but our findings indicate even greater impacts on depression and screening with multiple years of eligibility for Medicaid.
Medicaid expansion was not associated with postpartum depressive symptoms or our measure of well-being.Why we did not find an effect on this outcome is an area for future research. Some possible explanations are that determinants of postpartum depressive symptoms are multifactorial and include severe life events, social support, and biological factors,2,26 which might not be influenced by health insurance or care. In contrast, if prepregnancy screening for depression increased (as suggested by our findings), people who would have been at risk for postpartum depressive symptoms may have already been receiving treatment before delivery. Importantly, most birthing people receive only one six-week postpartum check-up (in contrast to monthly prenatal appointments), limiting the potential for health care providers to identify or treat postpartum depressive symptoms. Indeed, the American College of Obstetricians and Gynecologists has identified the need for policy changes that support a continuum of postpartum care rather than a single visit.27
Conclusion
Despite ample evidence that Medicaid expansion increased health insurance coverage and health care use among pregnant and birthing people12–14,21,25,28 and prior data showing links between insurance coverage and improved mental health,16,17,22,23 to our knowledge, our study is the first to examine whether the ACA Medicaid expansions affected prepregnancy or postpartum mental health and well-being. Using data from PRAMS, the only national source of data collected from people who recently had a live birth, we showed that Medicaid expansion was associated with a decline in self-reported prepregnancy depression that increased with time since expansion. Expanding health insurance coverage to low-income people before pregnancy may improve perinatal mental health. ■
Supplementary Material
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institute for Child Health and Human Development through Grant No. R01HD095951 to Claire Margerison and Robert Kaestner and Grant No. R01HD095951-02S1 to Margerison, Kaestner, and Sidra Goldman-Mellor). Kaestner received compensation from Columbia University and Stephan Zouras LLP in the past twelve months.
Contributor Information
Claire E. Margerison, Department of Epidemiology and Biostatistics, Michigan State University, in East Lansing, Michigan.
Katlyn Hettinger, a graduate research assistant in the Department of Epidemiology and Biostatistics and a doctoral student in the Department of Economics, Michigan State University.
Robert Kaestner, Harris School of Public Policy, University of Chicago, in Chicago, Illinois.
Sidra Goldman-Mellor, University of California Merced, in Merced, California.
Danielle Gartner, Department of Epidemiology and Biostatistics, Michigan State University.
NOTES
- 1.O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol. 2013;9:379–407. [DOI] [PubMed] [Google Scholar]
- 2.Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cook CAL, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME. Psychiatric disorders and treatment in low-income pregnant women. J Womens Health (Larchmt). 2010;19(7):1251–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ertel KA, Rich-Edwards JW, Koenen KC. Maternal depression in the United States: nationally representative rates and risks. J Womens Health (Larchmt). 2011;20(11):1609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez-Cabezas L, Clark C. Psychiatric emergencies in pregnancy and postpartum. Clin Obstet Gynecol. 2018;61(3):615–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women in the United States experience high rates of coverage “churn” in months before and after childbirth. Health Aff (Millwood). 2017;36(4):598–606. [DOI] [PubMed] [Google Scholar]
- 7.Miller S, Hu L, Kaestner R, Mazumder B, Wong A. The ACA Medicaid expansion in Michigan and financial health. J Policy Anal Manage. 2021;40(2):348–75. [Google Scholar]
- 8.Bitler MP, Zavodny M. Medicaid: a review of the literature [Internet]. Cambridge (MA): National Bureau of Economic Research; 2014. May [cited 2021 Aug 17]. (NBER Working Paper No. 20169). Available from: http://www.nber.org/papers/w20169 [Google Scholar]
- 9.Henry J Kaiser Family Foundation. Medicaid and CHIP income eligibility limits for pregnant women as a percent of the federal poverty level [Internet]. San Francisco (CA): KFF; 2021. Jan [cited 2021 Aug 17]. Available from: https://www.kff.org/health-reform/state-indicator/medicaid-and-chip-income-eligibility-limits-for-pregnant-women-as-a-percent-of-the-federal-poverty-level/ [Google Scholar]
- 10.Henry J Kaiser Family Foundation. Medicaid income eligibility limits for adults as a percent of the federal poverty level [Internet]. San Francisco (CA): KFF; 2021. Jan [cited 2021 Aug 17]. Available from: https://www.kff.org/health-reform/state-indicator/medicaid-income-eligibility-limits-for-adults-as-a-percent-of-the-federal-poverty-level/ [Google Scholar]
- 11.Henry J Kaiser Family Foundation. Status of state action on the Medicaid expansion decision [Internet]. San Francisco (CA): KFF; 2021. Aug [cited 2021 Aug 17]. Available from: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ [Google Scholar]
- 12.Margerison CE, MacCallum CL, Chen J, Zamani-Hank Y, Kaestner R. Impacts of Medicaid expansion on health among women of reproductive age. Am J Prev Med. 2020;58(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston EM, Strahan AE, Joski P, Dunlop AL, Adams EK. Impacts of the Affordable Care Acts Medicaid expansion on women of reproductive age: differences by parental status and state policies. Womens Health Issues. 2018;28(2):122–9. [DOI] [PubMed] [Google Scholar]
- 14.Clapp MA, James KE, Kaimal AJ, Daw JR. Preconception coverage before and after the Affordable Care Act Medicaid expansions. Obstet Gynecol. 2018;132(6):1394–400. [DOI] [PubMed] [Google Scholar]
- 15.Daw JR, Winkelman TNA, Dalton VK, Kozhimannil KB, Admon LK. Medicaid expansion improved perinatal insurance continuity for low-income women. Health Aff (Millwood). 2020;39(9):1531–9. [DOI] [PubMed] [Google Scholar]
- 16.McMorrow S, Gates JA, Long SK, Kenney GM. Medicaid Expansion increased coverage, improved affordability, and reduced psychological distress for low-income parents. Health Aff (Millwood). 2017;36(5):808–18. [DOI] [PubMed] [Google Scholar]
- 17.Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the first two years of the ACA Medicaid expansions. J Policy Anal Manage. 2017;36(2):390–417. [DOI] [PubMed] [Google Scholar]
- 18.To access the appendix, click on the Details tab of the article online.
- 19.Levis B, Sun Y, He C,Wu Y, Krishnan A, Bhandari PM, et al. Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: systematic review and meta-analysis. JAMA. 2020;323(22):2290–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu CH, Tronick E. Prevalence and predictors of maternal postpartum depressed mood and anhedonia by compensation from Columbia University and Stephan Zouras LLP in the past twelve months. race and ethnicity. Epidemiol Psy-chiatr Sci. 2014;23(2):201–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myerson R, Crawford S, Wherry LR. Medicaid expansion increased preconception health counseling, folic acid intake, and postpartum contraception. Health Aff (Millwood). 2020;39(11):1883–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, et al. The Oregon experiment— effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finkelstein A, Taubman S, Wright B, Bernstein M, Gruber J, Newhouse JP, et al. The Oregon Health Insurance Experiment: evidence from the first year [Internet]. Cambridge (MA): National Bureau of Economic Research; 2011. [cited 2021 Aug 17]. (NBER Working Paper No. 17190). Available from: https://www.nber.org/papers/w17190.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gates A, Rudowtiz R, Artiga S, Snyder L. Two year trends in Medicaid and CHIP enrollment data: findings from the CMS Performance Indicator Project [Internet]. San Francisco (CA): Henry J. Kaiser Family Foundation; 2016. Jun [cited 2021 Aug 17]. Available from: https://files.kff.org/attachment/Issue-Brief-Two-Year-Trends-in-Medicaid-and-CHIP-Enrollment-Data [Google Scholar]
- 25.Admon LK, Daw JR, Winkelman TNA, Kozhimannil KB, Zivin K, Heisler M, et al. Insurance coverage and perinatal health care use among low-income women in the US, 2015–2017. JAMA Netw Open. 2021;4(1):e2034549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yim IS, Tanner Stapleton LR, Guardino CM, Hahn-Holbrook J, Dunkel Schetter C. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American College of Obstetricians and Gynecologists. ACOG committee opinion no. 736: optimizing postpartum care. Obstet Gynecol. 2018;131(5):e140–50. [DOI] [PubMed] [Google Scholar]
- 28.Clapp MA, James KE, Kaimal AJ, Sommers BD, Daw JR. Association of Medicaid expansion with coverage and access to care for pregnant women. Obstet Gynecol. 2019; 134(5):1066–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


