Summary:
We present a case report of hyaluronic acid (HA) injected in the subcutaneous fat of the lateral face, deep fat compartments of the mid-face, and a combination of deep and superficial injection of HA in the chin. MRI demonstrates longevity of HA in the lateral face and deep fat compartments of the mid-face versus almost complete degradation of HA in the chin 19 months from injection. The MRI signal demonstrated no migration of HA and persistence of HA at 27 months in the lateral face and mid-face.
A 47-year-old man presented with mid-face volume loss, lack of jawline definition, and chin projection. Informed consent was obtained to treat with hyaluronic acid (HA) fillers and to perform sequential MRIs. The patient underwent three treatments with HA filler. The first treatment (not performed by an author) was with Restylane Lyft (Galderma, Lausanne, Switzerland) 1 ml total, with 0.5 ml injected into each lateral and medial sub-orbicularis oculi fat (SOOF) compartments, using a 27G needle in the supra-periosteal plane for mid-face volume loss. Two years later, a second treatment with Juvederm Ultra Plus (Allergan, Pringy, France), 1 ml total, was injected by the second author via a 25G cannula into the lateral and medial SOOF, pyriform recess, and buccal fat pad bilaterally using a threading technique for additional volumization of the mid-face.
Two months after the second treatment, a third treatment was performed by the second author, with 4 ml of Restylane Defyne to re-volumize the lateral face, improve jawline definition, and project the chin. Restylane Defyne, 1.5 ml per side, was injected via a 22G, 70-mm cannula, using a fanning technique, within the anatomical lateral temporal-cheek fat compartment,1 extending from the zygomatic arch to the angle of the mandible, using two entry points. A further Restylane Defyne 1 ml was injected in the prejowl sulcus, mental crease, mentalis, pogonion, gnathion, and menton, via a 27G needle using a bolus and threading technique into both superficial and deep fat compartments and within the mentalis muscles (See Video [online], which displays slides with diagrams on the patient’s photograph, showing the first, second, and third treatments. The third treatment has been filmed, demonstrating the 22G, 70-mm cannula using a fanning technique, within the anatomical lateral temporal-cheek fat compartment, extending from the zygomatic arch to the angle of the mandible, using two entry points).
Video 1. This video displays slides with diagrams on the patient’s photo, showing the first, second and third treatments. The third treatment has been filmed, demonstrating the 22G, 70mm cannula using a fanning technique, within the anatomical lateral temporal-cheek fat compartment, extending from the zygomatic arch to the angle of the mandible, using 2 entry points.
MRIs were performed 2 days, 19 months, 21 months, and 27 months after the third treatment. Author 1, the radiologist, interpreted all the MRIs and made a direct comparison of the appearances of the deposits over the 27-month period. The aim was to focus on the location and appearance of HA in the lateral temporal-cheek fat compartment of the third treatment.
DISCUSSION
Review of the current literature found no sequential imaging studies describing long-term follow-up of HA in the face. In one study, HA was reported to last for up to 12 years depending on the location and product in some patients.2 The aim of this case report was to focus on the MRI appearance of HA injected following the third treatment, over a 27-month period.
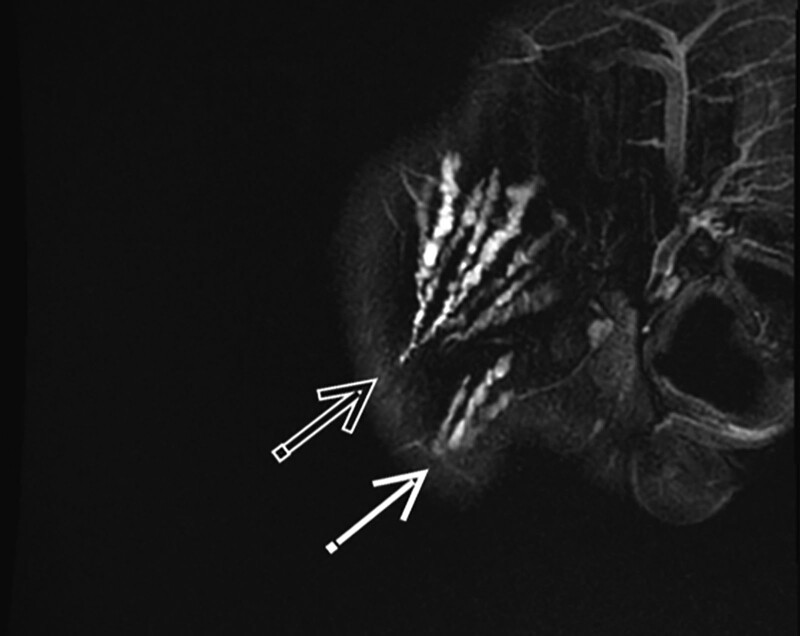
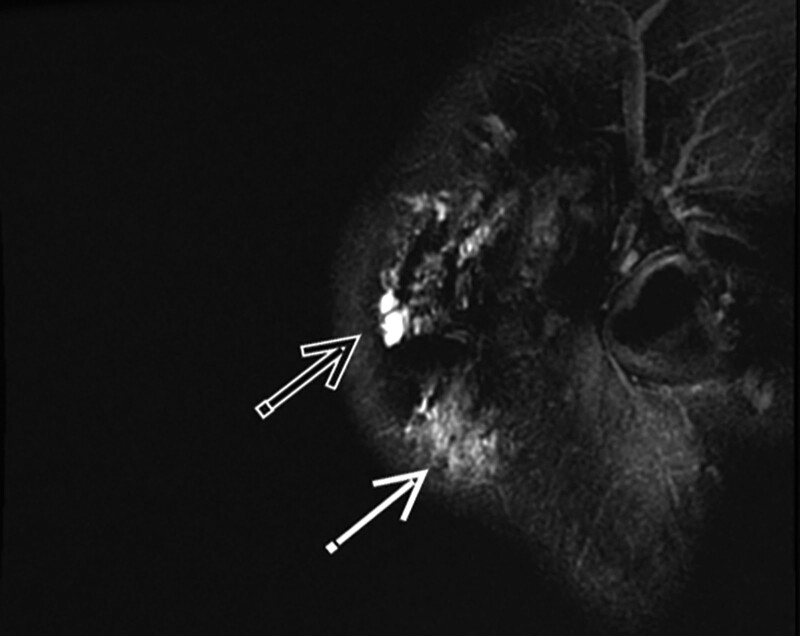
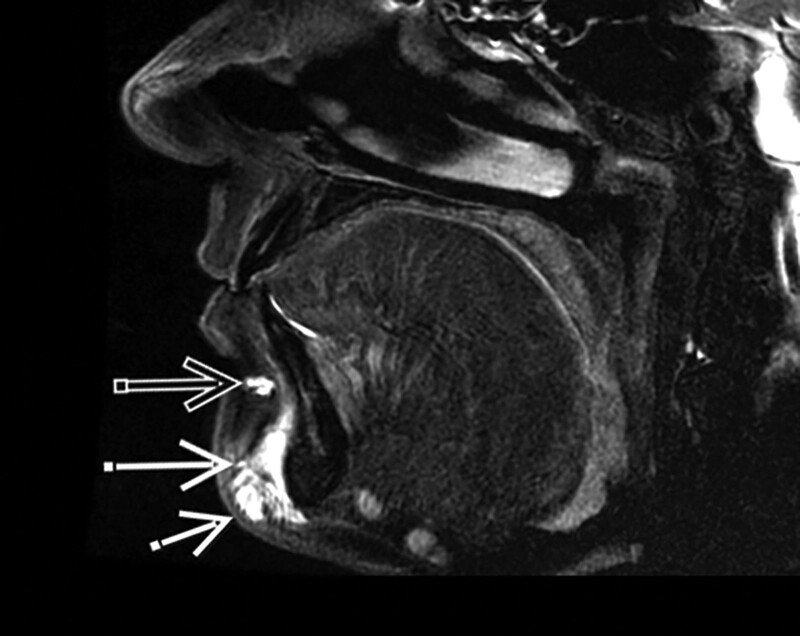
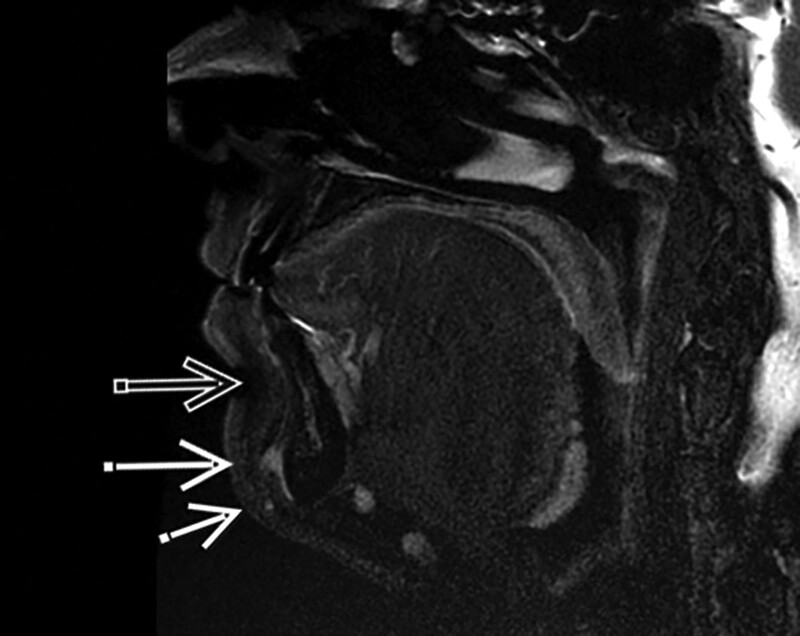
The initial MRI showed well-defined linear threads of HA signal in the lateral temporal-cheek fat compartments (Fig. 1). The HA in these areas demonstrated progressive ill-definition and decrease in the signal on T2, over a period of 19 months from injection, then appeared to stabilize from 19 months to the 27-month period (Fig. 2). The initial imaging confirmed HA signal in the prejowl sulcus, mental crease, mentalis, pogonion, gnathion, and menton (Fig. 3). At 19 months, complete resolution of the HA signal was seen in the prejowl sulcus, mental crease, and mentalis. At 27 months, there was resolution in the mental crease, mentalis, pogonion, and gnathion, with only trace signals remaining over the menton (Fig. 4). Incidentally, all MRIs demonstrated persistent HA deposits in the anatomic location of the first two treatments in the region of the medial and lateral SOOF and pyriform recesses. There was no evidence that the HA had migrated to other fat compartments over this 27-month study.3-5
Fig. 1.
Initial MRI sagittal T2 fat saturation, showing HA signal in a fanning pattern in the right preauricular region (open arrow) and jawline, superficially (closed arrow).
Fig. 2.
MRI sagittal T2 fat saturation at 27 months, showing the HA signal of the same fan, with a more ill-defined horizontal spread in preauricular region (open arrow) and jawline, superficially (closed arrow).
Fig. 3.
Initial MRI sagittal T2 fat saturation, showing HA signal in the mental crease (open arrow), mentalis and gnathion (closed arrow), and mentalis and the menton (short arrow).
Fig. 4.
MRI sagittal T2 fat saturation 19 months later, showing the HA signal resolved in the mental crease (open arrow) and mentalis and gnathion (closed arrow), with only trace signal remaining over the menton (short arrow).
Longevity seems to be related to the location, depth of filler placement, and volume of HA injected.6 HA injected in the superficial fat compartment of the lateral temporal-cheek maintained HA signal over the 27 months, whilst the chin demonstrated almost complete degradation of HA at 19 months. A factor contributing to the latter may be the total volume of HA injected in the lateral face was greater than that used for chin augmentation. Another factor may be the lack of mobility and subcutaneous placement in the lateral face, leading to persistence of filler compared with the mobile chin.7 Placement of HA in the deep fat compartments of the mid-face also demonstrated longevity on MRI. A limitation of this study was that MRI was not performed directly following treatment one or two. However, these treatments were found to be unchanged in appearance on sequential MRI. A further limitation of this report is that sequential clinical photographs were not taken with the MRIs for correlation.
CONCLUSIONS
MRI evidence of longevity of HA injected into the lateral temporal-cheek fat, pyriform recesses, and medial and lateral SOOF, at 27 months from injection were well demonstrated in this case study. MRI showed a degradation pattern in the same plane the HA filler was injected, with no evidence of migration. This study may be early evidence that the more mobile chin region may lead to more rapid resorption of HA than the lateral face and mid-face. Further MRI studies with larger cohorts, documenting the long-term pattern of degradation of HA fillers, with differing rheological properties, are needed.
Footnotes
Published online 13 April 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Fundarò S. Anatomy and aging of cheek fat compartments. Med Dent Res. 2018;1:3-7. [Google Scholar]
- 2.Master M. Hyaluronic acid filler longevity and localization – MRI evidence. Plast Reconstr Surg. 2020;147:50e–53e. [DOI] [PubMed] [Google Scholar]
- 3.Lin CH, Chiang CP, Wu BY, et al. Filler migration to the forehead due to multiple filler injections in a patient addicted to cosmetic fillers. J Cosmetic Laser Therapy. 2017;19:124–126. [DOI] [PubMed] [Google Scholar]
- 4.Jordan DR, Stoica B. Filler migration: a number of mechanisms to consider. Ophthalmic Plast Reconstr Surg. 2015;31:257–262. [DOI] [PubMed] [Google Scholar]
- 5.Lin CH, Chiang CP, Wu BY, et al. Filler migration to the forehead due to multiple filler injections in a patient addicted to cosmetic fillers. J Cosmet Laser Ther. 2017;19;124–126. [DOI] [PubMed] [Google Scholar]
- 6.Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36:753–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourgeois P, Peters E, Van Mieghem A, et al. Edemas of the face and lymphoscintigraphic examination. Sci Rep. 2021;11:6444. [DOI] [PMC free article] [PubMed] [Google Scholar]