Background:
Health literacy of plastic surgery patients may affect surgical decision-making and perioperative outcomes. In addition to consulting a plastic surgeon, patients often refer to online-based resources to learn about surgical options. The aim of this scoping review was to identify evidence detailing the state of health literacy of plastic surgery patients and available resources to highlight areas of improvement for clinical practice and future research.
Methods:
Utilizing PubMed and Web of Science databases, 46 eligible studies that analyzed health literacy in plastic surgery patients and readability of plastic surgery resources were included. Extracted characteristics from eligible studies included study size, type of analysis, findings, and conclusions.
Results:
Regardless of plastic surgery procedure or subspecialty, resources presenting plastic surgery information to patients exceeded the American Medical Association and National Institutes of Health recommended sixth- to eighth-grade reading level. Plastic surgery patients demonstrated greater knowledge of preoperative indications and surgical benefits compared with postoperative outcomes and surgical risks.
Conclusions:
Most health literacy research in plastic surgery focuses on readability of written internet-based resources as opposed to direct assessment of health literacy in plastic surgery patients. Plastic surgery resources exceed the recommended mean reading grade level. Dedicated efforts to recognize and accommodate a patient’s level of health literacy in plastic surgery should be considered.
Takeaways
Question: What is the status of health literacy in plastic surgery?
Findings: Of the 46 eligible studies assessing health literacy in plastic surgery, 78% analyzed the readability of plastic surgery resources. Regardless of subspecialty or surgical procedure, plastic surgery resources exceeded the American Medical Association and National Institutes of Health recommended sixth to eigth grade reading level. Plastic surgery patients demonstrated greater knowledge of preoperative indications and surgical benefits compared with postoperative outcomes and surgical risks.
Meaning: Dedicated efforts to recognize and accommodate a patient’s level of health literacy in plastic surgery may lead to improved perioperative outcomes.
INTRODUCTION
Patient health literacy affects surgical decision-making and outcomes. Health literacy is the ability of patients to access, comprehend, and apply medical information.1 In the surgical context, patient health literacy is leveraged in discussions about surgical details, risks, options for intervention, and postoperative regimens for optimal recovery. Limited surgical patient health literacy has been associated with decreased adherence to postoperative protocols, longer lengths of stay and time to recovery, and poorer surgical outcomes.2 In a meta-analysis of 40 studies encompassing 18,895 surgical patients, 31.7% of patients were found to have limited health literacy.2 This study, however, did not stratify for plastic surgery patients. Plastic surgery is a unique surgical specialty, as patients often decide for themselves which surgical procedures to pursue among many aesthetic and reconstructive options. Patients often refer to internet-based plastic surgery resources to guide decision-making and treatment plans in addition to consulting a plastic surgeon.3–6 A plastic surgery patient’s health literacy can therefore have a direct effect on surgical outcomes and postoperative satisfaction.7,8 The purpose of this scoping review was to identify evidence detailing the state of health literacy in plastic surgery patients and available resources to help highlight areas of improvement in clinical practice and future research.
METHODS
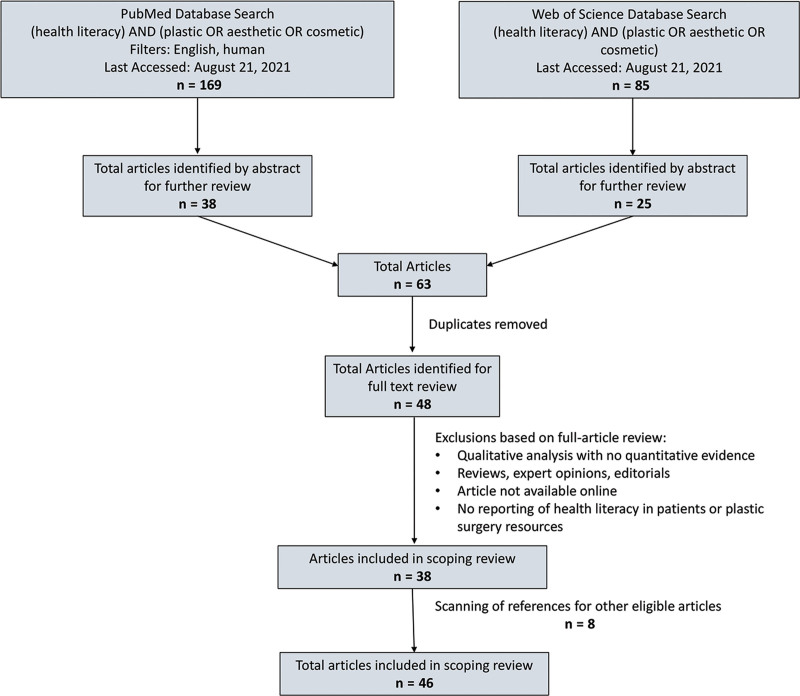
A scoping review of health literacy in plastic surgery was conducted using the PubMed and Web of Science databases adhering to PRISMA guidelines (Fig. 1).9 Inclusion criteria entailed studies analyzing health literacy of plastic surgery patients, and literacy analysis of plastic surgery resources. Exclusion criteria included (1) qualitative analysis with no quantitative evidence; (2) reviews, expert opinions, and editorials; (3) lack of availability online or in English; and (4) no reporting of health literacy in plastic surgery. Extracted characteristics from eligible studies included study size, type of analysis, findings, and conclusions.
Fig. 1.
Flowchart of selection process for articles included in scoping review.
RESULTS
Articles Included
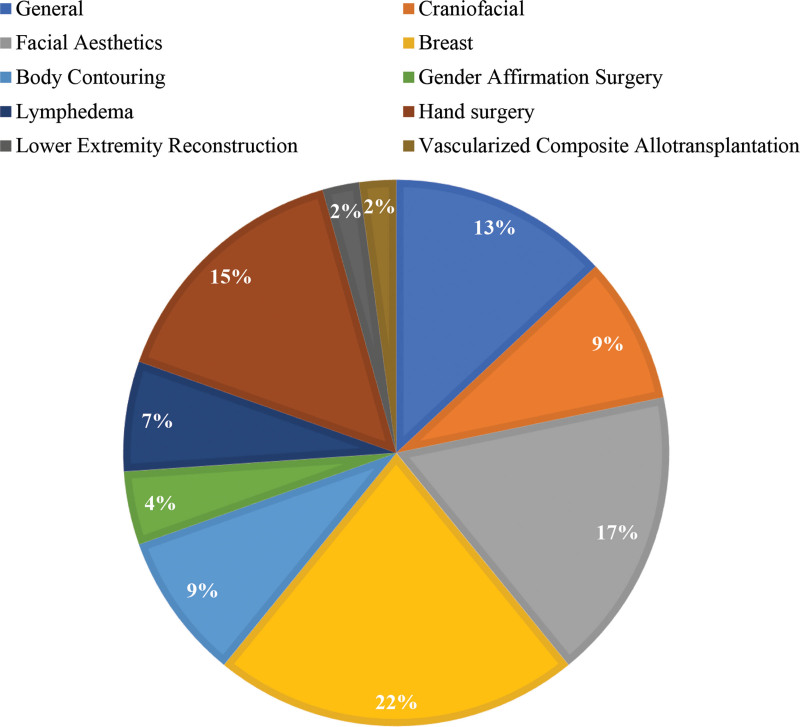
Database search and review of article references revealed 46 eligible articles for inclusion in this scoping review (Table 1).8,10–54 These articles represented the spectrum of plastic surgery, including breast (22%), facial aesthetics (17%), general plastic surgery (13%), hand surgery (15%), f (9%), craniofacial (9%), lymphedema (7%), gender affirmation surgery (4%), lower extremity reconstruction (2%), and vascularized composite allotransplantation (2%) (Fig. 2). Of these 46 articles, 78% analyzed the readability of plastic surgery resources, and 22% analyzed the state of health literacy in plastic surgery patients.
Table 1.
Distribution of Articles by Plastic Surgery Subtopic and Type of Analysis Conducted
| Plastic Surgery Subtopic | No. Articles | Analysis of Readability of Resources | Analysis of Patient Health Literacy |
|---|---|---|---|
| General | 6 | 3 | 3 |
| Craniofacial | 4 | 3 | 1 |
| Facial aesthetics | 8 | 8 | 0 |
| Breast | 10 | 10 | 0 |
| Body contouring | 4 | 3 | 1 |
| Gender affirmation surgery | 2 | 2 | 0 |
| Lymphedema | 3 | 3 | 0 |
| Hand surgery | 7 | 2 | 5 |
| Lower extremity reconstruction | 1 | 1 | 0 |
| Vascularized composite allotransplantation | 1 | 1 | 0 |
| Total no. articles | 46 | 36 | 10 |
Fig. 2.
Percentage of eligible articles by plastic surgery subtopic.
Analysis of Readability of Plastic Surgery Resources
Patients increasingly refer to internet-based resources for medical and surgical information both before and after clinical visits. Patient-directed health information can play a critical role in patient understanding, health decision-making processes, and compliance with care plans.14 The American Medical Association and National Institutes of Health recommend patient-directed health resources be written at a sixth- to eighth-grade reading level to align with patient health literacy most optimally.55 Extensive research has therefore been conducted to evaluate the readability of internet-based resources using numerous tools based on word and sentence complexity/length, including commonly the Flesch-Kincaid grade level scale, SMOG index, and Coleman Liau index. In this scoping review, the 36 articles that assessed the readability of plastic surgery internet-based resources utilizing these tools demonstrated a mean reading grade level consistently higher than the eighth grade, regardless of the sub topic analyzed (Table 2).8,10–44
Table 2.
Analysis of Readability of Resources
| Plastic Surgery Subtopic | Reference | Resources Analyzed | Mean Reading Grade Level* |
|---|---|---|---|
| General | Johnson et al19,38 | 10 websites | 10.19 |
| Aliu and Chung31 | 12 websites | 11.9 (ASPS) 12.0 (ASAPS) 8.9–11.5 (popular sites) |
|
| Chen et al35 | 234 tweeted articles | 17.7 (full access) 17.5 (open access) 13.9 (patient directed) |
|
| Craniofacial | Wasserburg et al15 | 143 websites (CP) 144 websites (CL) |
8.88–12.76 (CP)+8.61–12.32 (CL)+ |
| Patel et al39 | 3 websites | 13.8–15.2 (eMedicine) 7.5–10.7 (FACES) 11.9 —13.8 (WCF) |
|
| Sanghvi et al40 | 41 patient materials | 9.89–12.98+ | |
| Facial aesthetics | Mehta et al12 | 41 websites | 10.42 (academic site) 8.79 (physician site) |
| Awal and Hills17 | 200 websites | 11.0–14.0+ | |
| Rayess et al18 | 45 websites | 10.6 (private) 11.7 (other) |
|
| Gupta et al21 | 36 websites | 6.9–13.9 | |
| Barbarite et al26 | 32 websites | 10.7 | |
| Ziai et al32 | 50 websites | 9.22–12.16+ | |
| Santos et al42 | 10 websites | 12.2+ | |
| Misra et al43 | 17 AAFPRS patient materials | 8.3–18.2+ | |
| Breast | Chen et al10 | 20 websites | 12.4 (autologous) 12.1 (implant-based) |
| Powell et al8 | 97 websites | 13.04–13.64+ (academic) 10.91–11.82+ (nonacademic) |
|
| Nnamani Silva et al13 | 58 websites | 10.7–11.4+ | |
| Vargas14 | 10 websites | 10.7–15.8+ | |
| Doval et al20 | 10 websites | 10.4 (academic) 10.8 (private) |
|
| Cheah et al22 | 20 websites | 12.2 – 15.0+ | |
| Vargas et al23 | 10 websites | 9.7—13.0+ | |
| Kennedy et al27 | 10 websites | 11.0 | |
| Ricci et al29 | 12 websites | 12.7—15.0+ | |
| Vargas et al37 | 12 websites | 13.3+ | |
| Body contouring | Oleck et al11 | 10 websites | 13.0 |
| Vargas et al25 | 80 articles | 13.6+ | |
| Phillips et al28 | 10 websites | 8.7–15.2+ | |
| Gender affirmation surgery | Kiwanuka et al24 | Online search | 12.6–14.2+ |
| Vargas et al36 | 10 websites | 14.7+ | |
| Lymphedema | Seth et al30 | 12 websites | 12.6 |
| Tran et al33 | 10 websites | 14.0 | |
| Johnson et al38 | 10 websites | 9.8 | |
| Hand surgery | Hadden et al41 | 77 ASSH patient materials | 9.3+ |
| Santos et al44 | 10 websites | 9.7 – 14.4+ | |
| Lower extremity reconstruction | Hughes et al34 | 10 websites | 12.2 |
| Vascularized composite allotransplantation | Noel et al16 | 23 websites | 13.95+ |
*Modalities utilized to assess readability varied among articles (eg, FKGL, SMOG).
+Multiple analyses conducted in article for assessment.
In addition to readability, several studies also evaluated the understandability and actionability of internet-based plastic surgery resources utilizing the Patient Education and Materials Assessment Tool that appraises content, organization, layout, and use of visual aids. Understandability reflects the feasibility of patients of various backgrounds and health literacy levels to process the presented information. Actionability estimates a reader’s ability to apply written information to a task, such as surgical decision-making. Chen et al demonstrated that while the mean understandability did not differ between implant-based and autologous breast reconstruction resources (62.5% versus 60.5%, P = 0.65), implant-based breast reconstruction resources had a higher mean actionability score (24% versus 19.5%, P = 0.04).10 When analyzing internet-based resources on gluteal augmentation and cosmetic botulinum toxin as further examples, the mean understandability scores were 51% and 62.8%, and the mean actionability scores were 18.9% and 36.2% respectively.11,26
Factors Associated with Readability
Several articles evaluated whether stratification of internet-based resources by certain factors influenced readability. For instance, Powell et al found that internet-based materials on breast reconstruction had higher mean reading grade levels on academic websites compared with nonacademic websites (13.04–13.64 versus 10.91–11.82, P = 0.04).8 Seth et al showed that lymphedema materials on conservative management had greater readability than those detailing surgical intervention (12.7 versus 15.6, P < 0.001).30 In an analysis of internet-based resources on mastopexy, Vargas et al found that the mean reading grade level of materials detailing risks was higher than those explaining benefits of the surgical procedure (14.1 versus 11.6, P < 0.05).37 Aliu et al demonstrated that the American Society of Plastic Surgeons (ASPS) and the Aesthetic Society (formerly the American Society for Aesthetic Plastic Surgery, or ASAPS) internet-based materials had higher mean reading grade level scores compared with the top 10 popular websites on plastic surgery procedures (P < 0.05).31 There was however no significant difference in readability when comparing materials for autologous versus implant-based breast reconstruction (12.4 versus 12.1, P = 0.65), cleft palate versus cleft lip (8.88–12.76 versus 8.61–12.32, P > 0.05), and top versus bottom gender affirmation surgery (13.0 versus 12.6, P > 0.05).10,15,24
Resources Available in Different Languages
Several articles focused on the readability and cultural sensitivity of plastic surgery information presented in Spanish. In the analysis of online Spanish lymphedema resources, the mean reading grade level was 9.8, and the mean cultural sensitivity score was 2.27, which is below the recommended level of 2.5 by the Cultural Sensitivity and Assessment Tool.38 Furthermore, the mean reading grade levels and cultural sensitivity scores of online Spanish materials on cosmetic surgery and breast reconstruction were 10.19 and 10.4, and 2.20 and 2.9, respectively.19,20 In this scoping review, Spanish was the only language besides English that was assessed in the context of readability of plastic surgery resources.
Social Media
Social media is increasingly becoming a resource that patients utilize to access information on plastic surgery procedures. Chen et al analyzed the readability of articles shared by top-rated tweets under the Twitter hashtag #plasticsurgery.35 Of the 234 articles, the majority were academic journal articles (71%), with the remaining being patient information articles (29%). Full access and open-access journal articles that were shared had a higher mean reading grade level compared with patient information articles, though both exceeded the eighth grade level (17.7/17.5 versus 13.9, P < 0.0001). In this scoping review, Twitter was the only social media platform analyzed in relation to plastic surgery health literacy.
Evaluating Health Literacy in Plastic Surgery Patients
Varying levels of health literacy may impact the effectiveness of communication between patients and plastic surgeons during clinical visits.46 In this scoping review, several articles assessed patient health literacy at the time of outpatient clinical encounters. Menendez et al administered the Newest Vital Sign (NVS) health literacy tool, which assesses an individual’s ability to interpret and apply information depicted on a nutrition label seen on packaged food items, and a sociodemographic survey to 200 new hand surgery patients.50 Forty-three percent of the patients had limited health literacy, which included 33% of the English-speaking patients and 100% of the Spanish-speaking patients. Factors associated with limited health literacy included advanced age per 10-year increase (OR 1.3, P = 0.037), lower income (OR 3.5, P = 0.010), and public/no health insurance (OR 3.1, P = 0.008). Roy et al similarly applied the NVS to 185 patients with Dupuytren contracture and found 44% had limited health literacy.53 Decreased health literacy in these patients was associated with lower household income (P = 0.0006), immigration (P = 0.003), native language other than English (P = 0.03), increased age (P = 0.002), less education (P = 0.002), unemployment/retirement (P = 0.039), and other comorbidities (P = 0.039). In another study that audio-recorded patient encounters during hand surgery appointments, patients with limited health literacy determined by the NVS screening tool asked fewer questions about their therapeutic regimen (P < 0.001) and hand condition (P = 0.022).51 Health literacy measured by NVS in 112 new hand surgery patients, however, was not significantly associated with the time spent to acquire scheduled clinical visits (P = 0.13), or with patient satisfaction with clinical visits (P = 0.22).52
When evaluating patient health literacy during clinical encounters, physicians may often rely on subjective assessment rather than objective screening tools. In a 2014 national survey of American Society of Plastic Surgeons (ASPS), members aimed to assess plastic surgeons’ perceptions of patient health literacy, 73.8% of respondents answered they assessed patient health literacy through general impression (62.2%), and patient employment characteristics (37.3%).46 When counseling patients, plastic surgeons employed the following methods: lay terminology (94%), pictures/diagrams (84.6%), and teach-back strategies (8.1%). Sixty-two percent of plastic surgeon respondents reported spending at least 20 minutes counseling new patients with these methods. In another survey of 21 plastic surgeons, 67% agreed they had difficulty communicating with patients of different cultural backgrounds and, 29% stated they had educational material available to offer to low health literacy patients.49 Of these plastic surgeons, 71% were unaware of hospital policies to support low health literacy patients, and 76% reported they would be interested in learning how to improve communication with patients.
A few studies surveyed patients on their understanding of internet-based plastic surgery resources. Hoppe et al administered two surveys to 100 patients to assess comprehension of ASPS and The Aesthetic Society (ASAPS, at the time of the study) internet-based materials on breast reconstruction and rhinoplasty, with specific focus on preoperative indications and perioperative outcomes.45 The mean number of correct answers out of five questions was 3.56 for the rhinoplasty survey and 3.26 for the breast augmentation survey, with no significant difference in scores between ASPS and The Aesthetic Society materials (P > 0.05). Patients scored higher on questions regarding preoperative information compared with postoperative outcomes and complications (76.5% versus 62.7%, P < 0.001). In another study, 60 parents of cleft patients completed a survey assessing comprehension of materials available on ASPS and American Cleft Palate-Craniofacial Association websites about the cause, surgical management, and perioperative care of their child’s cleft condition. The mean score was 4.35 out of five questions, with no significant difference between ASPS and American Cleft Palate-Craniofacial Association materials (4.4 versus 4.29, P < 0.05). On multivariate analysis, level of education, ethnicity, and income were not associated with parent test scores (P = 0.38, P = 0.15, P = 0.3).
Several studies retrospectively characterized patient communication with plastic surgeons regarding their clinical encounters. Cho et al analyzed patient inquiries sent to the plastic surgery clinic during the perioperative period of postbariatric body contouring surgical procedures.48 Of the 212 communications identified, 167 (79%) were postoperative concerns regarding the surgical site (38%), medications (10%), and activity restrictions (10%). Fifty-seven percent of these concerns were resolved with patient re-education, but 16% required in-person evaluation. When 106 patients were surveyed about their communication with plastic surgery providers, 51% agreed that better communication with their provider would improve their health status, and 14% agreed provided written instructions were difficult to understand.49 Moreover, Tarabochia et al found that 78% of new hand surgery patients preferred a more active/collaborative role rather than a passive role during clinical encounters. In this study, preference to have an active decision-making role was not associated with health literacy assessed by the NVS assessment tool (OR 1.0, P = 0.93).
DISCUSSION
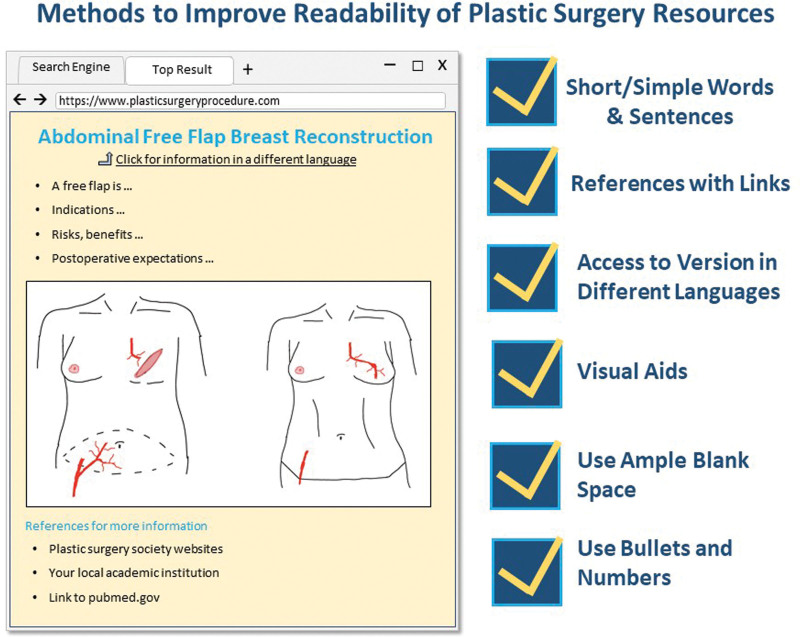
Though patient health literacy can affect surgical decision-making and outcomes, there is limited evidence of dedicated efforts to assess and accommodate patient health literacy in plastic surgery. The majority of health literacy in plastic surgery research focuses on readability of written internet-based resources as opposed to assessment of the reading grade levels or other measures of health literacy directly in plastic surgery patients. The available evidence demonstrates that the readability of plastic surgery resources does not meet recommended guidelines by American Medical Association and National Institutes of Health to be presented at a sixth- to eight-grade reading level, and that plastic surgery resources have subpar actionability, with scores commonly below 50%. Plastic surgery patients are therefore referring to unclear and complex materials that may provide confusion and hesitancy. Interventions to improve readability of materials may include shorter/simpler words and sentences, use of visual aids, improving access, and cultural sensitivity of resources in languages other than English, and inclusion of references on websites (Fig. 3).10,20,21,41 Efforts to improve readability of patient-facing materials may also extend to plastic surgery informed consent documents and the newly instated breast implant checklists.56 Future research may consider investigating whether interval efforts have been made to improve the readability and quality of internet-based plastic surgery resources by institution and plastic surgery society websites.
Fig. 3.
Infographic illustrating methods to improve readability of plastic surgery resources.
Plastic surgeons typically rely on subjective perceptions of patient health literacy based on overall impression and patients’ education/occupation. In this scoping review, limited health literacy was associated with low income, less education, lack of insurance, increased age, comorbidities, and native language other than English. Although several hand surgery studies demonstrated the use of a health literacy screening tool with the NVS, a health literacy assessment tool has not been adopted on a large scale in plastic surgery. Although a screening tool may identify patients with limited health literacy more accurately and help guide communication during clinical encounters, the use of the same may add clinical time and risk patient embarrassment and stigmatization.53 Future research may consider investigating whether the level of health literacy measured by screening tools such as the NVS are associated with perioperative outcomes in plastic surgery patients.
The majority of patients prefer to play an active/collaborative role with surgeons during clinical encounters. Rather than relying on quick heuristics based on risk factors or a screening tool to identify limited health literacy, plastic surgeons may practice a collaborative approach to communication to better identify gaps in knowledge by addressing patient questions, and to guide surgical decision-making by resolving specific concerns. Evidence in this scoping review showed that patients typically have decreased understanding of postoperative expectations, surgical details, and surgical risks when compared with conservative management, preoperative indications, and surgical benefits. Plastic surgeons may consider devoting greater efforts to discuss these topics with patients during clinical encounters and to provide resources with high readability for patients to reference during their surgical journey. To achieve this aim, plastic surgeons may also consider offering patients decision aids in surgical planning. Several studies in breast reconstruction have shown that the application of decision aids in preoperative consultations improved patient knowledge, increased confidence about surgical decisions, decreased anxiety, and enhanced satisfaction with postoperative results.57–65 These tools included personalized risk assessment for perioperative complications, visual aids, interactive digital modules with quizzes, videos, and oral presentations. Providing patients with access to decision aids and video education tools before clinical consultation may improve the quality of patient-plastic surgeon communication and surgical decision-making. Moreover, several guidelines on how to provide patients with health information to promote patient education have been shared. For instance, the American Academy of Family Physicians recommends a practice maintain an adequate supply of patient education materials of all types, including written, audiovisual, and computer-based. These materials should be tailored to the appropriate reading and comprehension level, to the learning style, and to the cultural and ethnic diversity of the patient.66 The Agency for Healthcare Research and Quality advises practitioners to ensure patients know how to access accurate internet resources and how to use audiovisual materials that are recommended.67 Resources provided to and recommended to patients should be monitored regularly and modified according to patient feedback. Importantly, these health information tools are a supplement and not a substitute for patient-physician discussions about treatment plans.
Strengths and Limitations
This scoping review summarizes the evidence of health literacy analyzed in plastic surgery resources and patients, and highlights areas of improvement in clinical practice and future research. Although a thorough review of the literature was conducted to identify eligible studies meeting inclusion and exclusion criteria, there may have been additional eligible studies that were not captured in our search. Among the eligible studies, there was heterogeneity in types of analyses and quantitative measures conducted across the spectrum of plastic surgery subspecialties, which precluded pooled analysis.
CONCLUSIONS
Patient health literacy influences surgical decision-making and outcomes. Forty-six eligible studies analyzing health literacy in plastic surgery patients and readability of plastic surgery internet-based resources were included in this scoping review. Seventy-eight percent of eligible articles analyzed the readability of plastic surgery resources. Plastic surgery resources exceeded the recommended mean reading grade level regardless of subspecialty or surgical procedure. Plastic surgery patients exhibited greater knowledge of preoperative indications and surgical benefits compared with postoperative outcomes and surgical risks. Both plastic surgeons and plastic surgery patients reported that better communication would improve overall patient health outcomes.
Footnotes
Published online 13 April 2022.
Disclosure: Dr. Jeffrey Janis receives royalties from Thieme and Springer Publishing. All the other authors have no financial interests to declare in relation to the content of this article.
REFERENCES
- 1.Berkman ND, Sheridan SL, Donahue KE, et al. Health literacy interventions and outcomes: an updated systematic review. Evid ReportTechnology Assess. 2011;(199):1–941. [PMC free article] [PubMed] [Google Scholar]
- 2.Roy M, Corkum JP, Urbach DR, et al. Health literacy among surgical patients: a systematic review and meta-analysis. World J Surg. 2019;43:96–106. [DOI] [PubMed] [Google Scholar]
- 3.Rohrich RJ, Weinstein A. Paging Dr. Google: the changing face of plastic surgery. Plast Reconstr Surg. 2016;138:1133–1136. [DOI] [PubMed] [Google Scholar]
- 4.Montemurro P, Tay VKS, Hedén P. The evolution of patients’ and surgeons’ perspectives towards the role of the internet and social media in breast augmentation over 5 years. Aesthet Surg J. 2021;41:262–268. [DOI] [PubMed] [Google Scholar]
- 5.Long EA, Gabrick K, Janis JE, et al. Board certification in cosmetic surgery: an evaluation of training backgrounds and scope of practice. Plast Reconstr Surg. 2020;146:1017–1023. [DOI] [PubMed] [Google Scholar]
- 6.Patel A, Varghese J, Joshi C, et al. Do websites serve our patients well? A comparative analysis of online information on cosmetic injectables. Plast Reconstr Surg. Published online Accepted 2021. [DOI] [PubMed] [Google Scholar]
- 7.Zhong T, Hu J, Bagher S, et al. Decision regret following breast reconstruction: the role of self-efficacy and satisfaction with information in the preoperative period. Plast Reconstr Surg. 2013;132:724e–734e. [DOI] [PubMed] [Google Scholar]
- 8.Powell LE, Andersen ES, Pozez AL. Assessing readability of patient education materials on breast reconstruction by major US academic hospitals as compared with nonacademic sites. Ann Plast Surg. 2021;86:610–614. [DOI] [PubMed] [Google Scholar]
- 9.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- 10.Chen DH, Johnson AR, Ayyala H, et al. A multimetric health literacy analysis of autologous versus implant-based breast reconstruction. Ann Plast Surg. 2020;85(S1 Suppl 1):S102–S108. [DOI] [PubMed] [Google Scholar]
- 11.Oleck NC, Johnson AR, Tran BNN, et al. A multimetric health literacy analysis of online information for gluteal augmentation with fat grafting. Ann Plast Surg. 2020;85(S1 Suppl 1):S97–S101. [DOI] [PubMed] [Google Scholar]
- 12.Mehta N, Gupta A, Nissan M. All I have learned, I have learned from Google: why today’s facial rejuvenation patients are prone to misinformation, and the steps we can take to contend with unreliable information. Facial Plast Surg. 2019;35:387–392. [DOI] [PubMed] [Google Scholar]
- 13.Nnamani Silva ON, Ammanuel SG, Segobiano BM, et al. Assessing the readability of online patient education resources related to gynecomastia. Ann Plast Surg. 2021;87:123–125. [DOI] [PubMed] [Google Scholar]
- 14.Vargas CR, Kantak NA, Chuang DJ, et al. Assessment of online patient materials for breast reconstruction. J Surg Res. 2015;199:280–286. [DOI] [PubMed] [Google Scholar]
- 15.Wasserburg JR, Sayegh F, Sanati-Mehrizy P, et al. Cleft care readability: can patients access helpful online resources? Cleft Palate Craniofac J. 2021;58:1287–1293. [DOI] [PubMed] [Google Scholar]
- 16.Noel DY, Kimberly LL, DeMitchell-Rodriguez EM, et al. Comprehensive assessment of vascularized composite allotransplantation patient-oriented online resources. Ann Plast Surg. 2019;83:217–223. [DOI] [PubMed] [Google Scholar]
- 17.Awal DH, Mills C. Cosmetic facial surgery: are online resources reliable and do patients understand them? Br J Oral Maxillofac Surg. 2018;56:124–128. [DOI] [PubMed] [Google Scholar]
- 18.Rayess H, Zuliani GF, Gupta A, et al. Critical analysis of the quality, readability, and technical aspects of online information provided for neck-lifts. JAMA Facial Plast Surg. 2017;19:115–120. [DOI] [PubMed] [Google Scholar]
- 19.Johnson AR, Bravo MG, Granoff MD, et al. Cultural insensitivity pervasive in Spanish online cosmetic surgery resources: a call to action. Ann Plast Surg. 2019;82(4S Suppl 3):S228–S233. [DOI] [PubMed] [Google Scholar]
- 20.Doval AF, Riba L, Tran BNN, et al. Literacy analysis of Spanish online resources for breast reconstruction. Ann Plast Surg. 2018;80(4 Suppl 4):S189–S195. [DOI] [PubMed] [Google Scholar]
- 21.Gupta A, Nissan ME, Bojrab DI, II, et al. Do patients access appropriate information online? Facial Plast Surg. 2017;33:428–433. [DOI] [PubMed] [Google Scholar]
- 22.Cheah MA, Sarmiento S, Bernatowicz E, et al. Online patient resources for breast implant-associated anaplastic large cell lymphoma: a readability analysis. Ann Plast Surg. 2020;84:346–350. [DOI] [PubMed] [Google Scholar]
- 23.Vargas CR, Koolen PGL, Chuang DJ, et al. Online patient resources for breast reconstruction: an analysis of readability. Plast Reconstr Surg. 2014;134:406–413. [DOI] [PubMed] [Google Scholar]
- 24.Kiwanuka E, Mehrzad R, Prsic A, et al. Online patient resources for gender affirmation surgery: an analysis of readability. Ann Plast Surg. 2017;79:329–333. [DOI] [PubMed] [Google Scholar]
- 25.Vargas CR, Ricci JA, Chuang DJ, et al. Online patient resources for liposuction: a comparative analysis of readability. Ann Plast Surg. 2016;76:349–354. [DOI] [PubMed] [Google Scholar]
- 26.Barbarite E, Shaye D, Oyer S, et al. Quality assessment of online patient information for cosmetic botulinum toxin. Aesthet Surg J. 2020;40:NP636–NP642. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy AM, Davidson C, Cronin E, et al. Readability and quality of breast reduction on-line resources. J Plast Reconstr Aesthet Surg. 2019;72:137–171. [DOI] [PubMed] [Google Scholar]
- 28.Phillips NA, Vargas CR, Chuang DJ, et al. Readability assessment of online patient abdominoplasty resources. Aesthetic Plast Surg. 2015;39:147–153. [DOI] [PubMed] [Google Scholar]
- 29.Ricci JA, Vargas CR, Chuang DJ, et al. Readability assessment of online patient resources for breast augmentation surgery. Plast Reconstr Surg. 2015;135:1573–1579. [DOI] [PubMed] [Google Scholar]
- 30.Seth AK, Vargas CR, Chuang DJ, et al. Readability assessment of patient information about lymphedema and its treatment. Plast Reconstr Surg. 2016;137:287e–295e. [DOI] [PubMed] [Google Scholar]
- 31.Aliu O, Chung KC. Readability of ASPS and ASAPS educational web sites: an analysis of consumer impact. Plast Reconstr Surg. 2010;125:1271–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ziai H, Levin M, Roskies M. Readability of internet-based resources for cosmetic facial botulinum toxin injections. Facial Plast Surg Aesthet Med. 2021;23:146–147. [DOI] [PubMed] [Google Scholar]
- 33.Tran BNN, Singh M, Lee BT, et al. Readability, complexity, and suitability analysis of online lymphedema resources. J Surg Res. 2017;213:251–260. [DOI] [PubMed] [Google Scholar]
- 34.Hughes CD, Tran BNN, Rinkinen J, et al. Readability, suitability, and complexity of online resources for lower extremity reconstruction. Ann Plast Surg. 2019;82:2–6. [DOI] [PubMed] [Google Scholar]
- 35.Chen AD, Ruan QZ, Bucknor A, et al. Social media: is the message reaching the plastic surgery audience? Plast Reconstr Surg. 2019;144:773–781. [DOI] [PubMed] [Google Scholar]
- 36.Vargas CR, Ricci JA, Lee M, et al. The accessibility, readability, and quality of online resources for gender affirming surgery. J Surg Res. 2017;217:198–206. [DOI] [PubMed] [Google Scholar]
- 37.Vargas CR, Chuang DJ, Lee BT. The readability of online resources for mastopexy surgery. Ann Plast Surg. 2016;77:110–114. [DOI] [PubMed] [Google Scholar]
- 38.Johnson AR, Doval AF, Egeler SA, et al. A multimetric evaluation of online Spanish health resources for lymphedema. Ann Plast Surg. 2019;82:255–261. [DOI] [PubMed] [Google Scholar]
- 39.Patel PP, Hoppe IC, Ahuja NK, et al. Analysis of comprehensibility of patient information regarding complex craniofacial conditions. J Craniofac Surg. 2011;22:1179–1182. [DOI] [PubMed] [Google Scholar]
- 40.Sanghvi S, Cherla DV, Shukla PA, et al. Readability assessment of internet-based patient education materials related to facial fractures. Laryngoscope. 2012;122:1943–1948. [DOI] [PubMed] [Google Scholar]
- 41.Hadden K, Prince LY, Schnaekel A, et al. Readability of patient education materials in hand surgery and health literacy best practices for improvement. J Hand Surg Am. 2016;41:825–832. [DOI] [PubMed] [Google Scholar]
- 42.Santos PJF, Daar DA, Paydar KZ, et al. Readability of online materials for rhinoplasty. World J Plast Surg. 2018;7:89–96. [PMC free article] [PubMed] [Google Scholar]
- 43.Misra P, Agarwal N, Kasabwala K, et al. Readability analysis of healthcare-oriented education resources from the American Academy of Facial Plastic and Reconstructive Surgery. Laryngoscope. 2013;123:90–96. [DOI] [PubMed] [Google Scholar]
- 44.Santos PJF, Daar DA, Badeau A, et al. Readability of online materials for Dupuytren’s contracture. J Hand Ther. 2018;31:472–479. [DOI] [PubMed] [Google Scholar]
- 45.Hoppe IC, Ahuja NK, Ingargiola MJ, et al. A survey of patient comprehension of readily accessible online educational material regarding plastic surgery procedures. Aesthet Surg J. 2013;33:436–442. [DOI] [PubMed] [Google Scholar]
- 46.Vargas CR, Chuang DJ, Lee BT. Assessment of patient health literacy: a national survey of plastic surgeons. Plast Reconstr Surg. 2014;134:1405–1414. [DOI] [PubMed] [Google Scholar]
- 47.Jodeh DS, Pringle AJ, Rottgers SA. Comprehension of online educational material regarding orofacial clefts. Cleft Palate Craniofac J. 2019;56:1206–1212. [DOI] [PubMed] [Google Scholar]
- 48.Cho HE, Huynh KA, Corriere MA, et al. Developing strategies for targeted improvement of perioperative education for postbariatric surgery body-contouring patients. Ann Plast Surg. 2021;86:463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barton N, Janis JE. Missing the mark: the state of health care literacy in plastic surgery. Plast Reconstr Surg Glob Open. 2020;8:e2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Menendez ME, Mudgal CS, Jupiter JB, et al. Health literacy in hand surgery patients: a cross-sectional survey. J Hand Surg Am. 2015;40:798–804.e2. [DOI] [PubMed] [Google Scholar]
- 51.Menendez ME, van Hoorn BT, Mackert M, et al. Patients with limited health literacy ask fewer questions during office visits with hand surgeons. Clin Orthop Relat Res. 2017;475:1291–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alokozai A, Bernstein DN, Sheikholeslami N, et al. Impact of health literacy on time spent seeking hand care. Hand (N Y). 2018;13:538–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roy M, Okrainec K, Novak CB, et al. Universal measures of support are needed: a cross-sectional study of health literacy in patients with Dupuytren’s disease. Plast Reconstr Surg. 2019;143:350e–358e. [DOI] [PubMed] [Google Scholar]
- 54.Tarabochia M, Menendez ME, Ring D. Health literacy and decisional preferences in hand surgery. J Hand Surg Am. 2021;46:70.e1–70.e8. [DOI] [PubMed] [Google Scholar]
- 55.Eysenbach G, Powell J, Kuss O, et al. Empirical studies assessing the quality of health information for consumers on the world wide web: a systematic review. JAMA. 2002;287:2691–2700. [DOI] [PubMed] [Google Scholar]
- 56.US Food & Drug Administration (USFDA). FDA Strengthens Safety Requirements and Updates Study Results for Breast Implants. Silver Spring, Md.: USFDA. https://www.fda.gov/news-events/press-announcements/fda-strengthens-safety-requirements-and-updates-study-results-breast-implants. Published online October 27, 2021. Accessed January 28, 2022. [Google Scholar]
- 57.Politi MC, Lee CN, Philpott-Streiff SE, et al. A randomized controlled trial evaluating the BREASTChoice tool for personalized decision support about breast reconstruction after mastectomy. Ann Surg. 2020;271:230–237. [DOI] [PubMed] [Google Scholar]
- 58.Fan KL, Black CK, DeFazio MV, et al. Bridging the knowledge gap: an examination of the ideal postoperative autologous breast reconstruction educational material with A/B testing. Plast Reconstr Surg. 2020;145:258–266. [DOI] [PubMed] [Google Scholar]
- 59.Familusi O, Rios-Diaz AJ, Tilahun ED, et al. Post-mastectomy breast reconstruction: reducing the disparity through educational outreach to the underserved. Support Care Cancer. 2021;29:1055–1063. [DOI] [PubMed] [Google Scholar]
- 60.Heller L, Parker PA, Youssef A, et al. Interactive digital education aid in breast reconstruction. Plast Reconstr Surg. 2008;122:717–724. [DOI] [PubMed] [Google Scholar]
- 61.Sherman KA, Shaw LE, Winch CJ, et al. ; BRECONDA Collaborative Research Group. Reducing decisional conflict and enhancing satisfaction with information among women considering breast reconstruction following mastectomy: results from the BRECONDA randomized controlled trial. Plast Reconstr Surg. 2016;138:592e–602e. [DOI] [PubMed] [Google Scholar]
- 62.Luan A, Hui KJ, Remington AC, et al. Effects of a novel decision aid for breast reconstruction: a randomized prospective trial. Ann Plast Surg. 2016;76(Suppl 3):S249–S254. [DOI] [PubMed] [Google Scholar]
- 63.Hoffman AS, Cantor SB, Fingeret MC, et al. Considering breast reconstruction after mastectomy: a patient decision aid video and workbook. Plast Reconstr Surg Glob Open. 2019;7:e2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Metcalfe K, Zhong T, O’Neill AC, et al. Development and testing of a decision aid for women considering delayed breast reconstruction. J Plast Reconstr Aesthet Surg. 2018;71:318–326. [DOI] [PubMed] [Google Scholar]
- 65.Varelas L, Egro FM, Evankovich N, et al. A randomized controlled trial to assess the use of a virtual decisional aid to improve knowledge and patient satisfaction in women considering breast reconstruction following mastectomy. Cureus. 2020;12:e12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Patient education. American academy of family physicians. Am Fam Physician. 2000;62:1712–1714. [PubMed] [Google Scholar]
- 67.Use Health Education material effectively: Tool #12. AHRQ Health Literacy Universal Precautions Toolkit, second edition. Published online September 2020. Available at https://www.ahrq.gov/health-literacy/improve/precautions/tool12.html. Accessed January 17, 2022.