Henna grows across Africa and Asia, where it has been used as a natural reddish dye for hair and skin since time immemorial. Although the U.S. Food and Drug Administration (FDA) considers natural henna safe for use on hair (although not skin),1 its cosmetic properties are sometimes enhanced by the addition of dangerous ingredients, including lead.2,3 When Dilek Battal, an associate professor in the Department of Pharmaceutical Toxicology at Mersin University in Turkey, decided to study hazardous additives in henna, one of her students visited popular henna shops to obtain samples. But most henna merchants—who mix their products themselves and add their own special ingredients—did not want to give her samples. Once the investigators managed to obtain some of the powders, the reason for their reluctance became clear. All 25 henna samples contained trace amounts of lead, along with other heavy metals and the highly allergenic colorant -phenylenediamine. At least four of them contained no henna at all.4
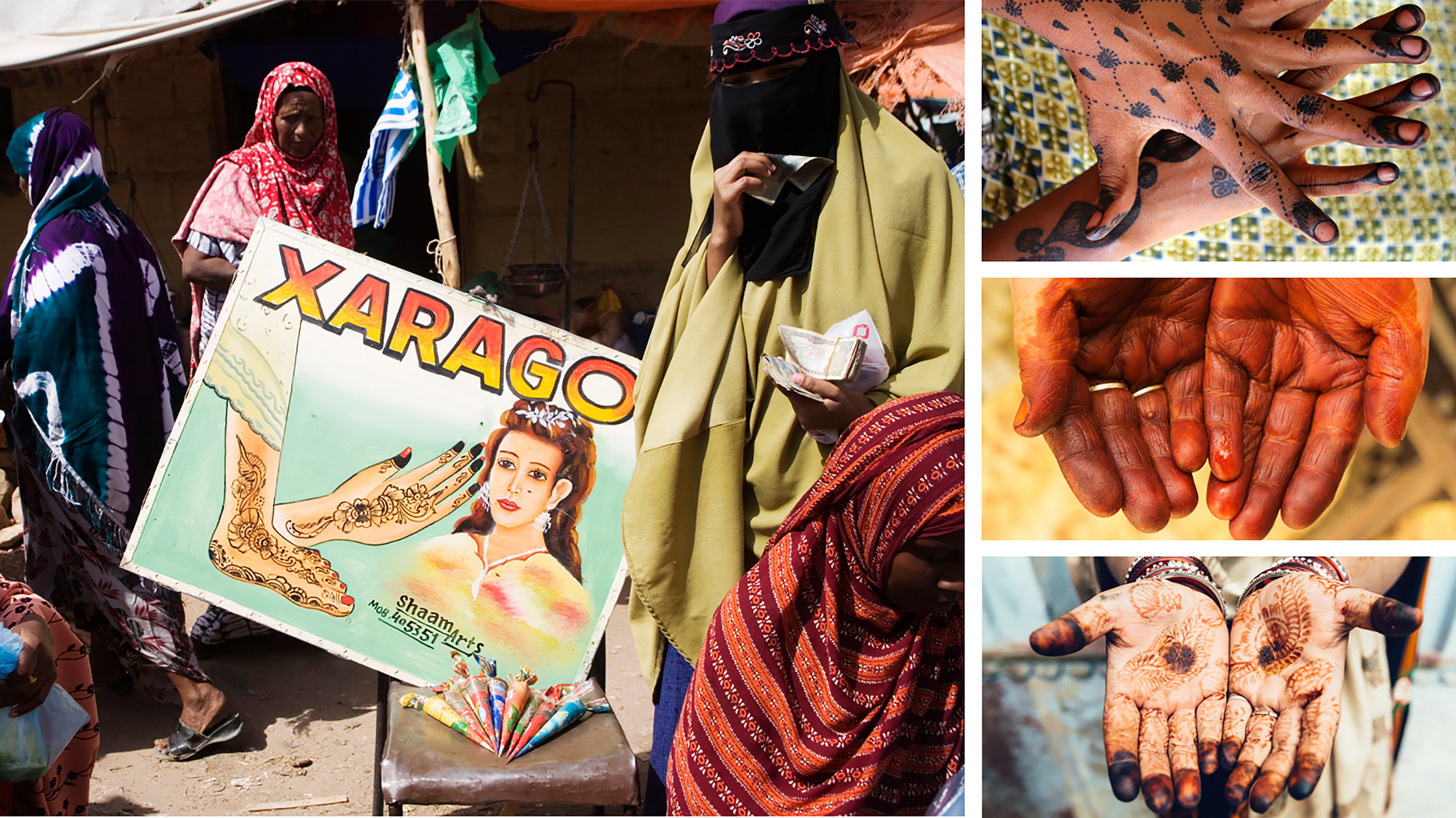
Henna is widely used as a temporary adornment in countries such as (clockwise from left) Somaliland, Nigeria, Turkey, and India. Traditional designs vary widely, from intricate tracery to fully painted palms. Images: ©Liba Taylor/Panos Pictures; © Giacomo Pirozzi/Panos Pictures: © iStockphoto/tunart; © iStockphoto/ferrantraite.
The amounts of lead found in these and other studies may fall below limits suggested by agencies such as the FDA, which currently recommends no more than (expressed as ppm) lead in cosmetics as an impurity.5 However, the frequent and long-term use of contaminated cosmetics raises the risk of cumulative exposure. Lead persists in the body for decades. In pregnant women, lead has been associated with spontaneous abortion, hypertension, and poor birth outcomes.6 During pregnancy, it can be resorbed from a woman’s bones into her blood, exposing her developing fetus.7
Perhaps the best-known consequences for children exposed to lead are neurotoxic effects. Relatively low exposures are associated with deficits in intelligence quotient,8,9 cognitive and behavioral disorders,10,11,12 and reduced motor skills.12 In one U.S. study of adults, higher cumulative lead exposure was associated with lower cognitive scores at 52–79 years of age.13 Other associated health effects in adults include hypertension, coronary heart disease, and other cardiovascular-related diseases.7,14
“Everywhere on Earth, I think, people are familiar with the fact that lead can poison and that people are poisoned by lead,” says Andrew McCartor, the vice president of strategy and partnerships at Pure Earth, a nonprofit that works to help clean up and prevent toxic pollution around the world. “But I don’t think that people realize the extent to which there is broad-based lead poisoning across entire populations.”
Over the years, campaigns to remove lead from gasoline and paint have been real public health success stories. However, lead still hides in many industrial sources, foods, and spices, as well as in everyday cosmetics, says researcher Emmanuel Obeng-Gyasi, an assistant professor of environmental health and safety at North Carolina Agricultural and Technical State University.
Lead often turns up in cosmetics as a contaminant, possibly because it was in the same rock from which mineral-based colorants and mica powder were made.15 Obeng-Gyasi says it may also be added intentionally because lead makes cosmetic colors pop and helps products resist moisture. Dozens of countries have developed even stricter controls of lead in cosmetics than the FDA, including 65 countries that have banned it outright.16 But in many low- and middle-income countries, regulations to limit lead exposure either do not exist or falter because of lack of enforcement.17
Lead in Cosmetics throughout History
Only relatively recently have the health effects of lead—even in small amounts—become more fully understood.18,19 By comparison, lead has been added to cosmetics for millennia. The earliest known lipstick has been dated to 3500 BCE, when the ancient Sumerian queen Puabi colored her lips with a fine powder of crushed red rock mixed with white lead.20 The ancient Egyptians lined their eyes with kohl, sometimes made from galena—a dull gray mineral containing lead sulfide—or antimony, which is less toxic but also scarcer and more expensive.21 Archaeologists have found galena presumably destined for cosmetic use in the tombs of Egyptian kings from circa 3000 BCE22; the mineral is still used in kohl today.23
The kohl that ancient Egyptians used had both cosmetic and protective functions. In addition to making a person’s eyes look larger and more defined, kohl was believed to protect against infection, from the relentless rays of the sun on the edge of the desert, and from a more nebulous danger—the evil eye.24,25
Kohl use spread across the African continent to the Levant and the Indian subcontinent, possibly as much because of its allure as a cosmetic as for its medicinal properties in sunny landscapes. Other names for kohl include, in Nigeria, tiro for the Yoruba and tozali for the Hausa, and both surma and kajal in South and Central Asia.26 Islamic culture has also played a role in its widespread use. The Prophet Muhammed told his disciples to use kohl on the eyes as “it brightens the eyesight and strengthens and increases the growth of the eyelashes.”27

Women have used lead-based cosmetics for millennia in accordance with the beauty standards of the day. Clockwise from top left: Queen Puabi of Sumer (c. 2500–2300 BCE); Queen Nefertiti of Egypt (c. 1370–1330 BCE); a Chinese woman (middle sixth century CE); late 19th-century American advertisement for Laird’s Bloom of Youth; Queen Elizabeth I of England (1533–1603 CE). Images: University of Massachusetts Amherst Libraries; Neues Museum/CC BY-SA 3.0; Boston Museum of Fine Arts; Boston Public Library; United Kingdom National Portrait Gallery/CC BY-NC-ND 3.0.
Lead was used in many other products over the centuries. In Greece, the first-century physician Dioscorides described a recipe using lead oxide, sodium carbonate, and salt to produce a white powder that was used for “eye medications, for unseemly scars and for faces full of wrinkles and blemishes.”28 Court ladies in sixth-century China developed a trend of coloring their foreheads bright yellow with a product that may have contained lead; the style would last for centuries.29 Some historians believe that England’s Queen Elizabeth I used a mixture of lead and vinegar known as Venetian ceruse to achieve smooth skin of the palest white.30,31 Halfway around the world in 17th-century Japan, noblemen and -women used lead-based powders to make their skin look whiter as a sign that they were people of leisure, above laboring in a blazing sun that would darken their complexion.32 (The quest for white skin continues today, albeit using toxic agents other than lead.33)
Lead-filled creams and powders continued to be in fashion until the early 20th century, leaving a trail of mysterious illnesses and even some deaths in their wake. A lotion called Laird’s Bloom of Youth was popular in the 1860s. Eventually the preparation, which was “highly impregnated with acetate and carbonate of lead,”34 was shown to cause lead palsy, a kind of localized paralysis.22 In 1922, the Journal of the American Medical Association published the curious case of a woman who complained of constant tremors, nausea, and vomiting. The culprit was poisoning from her Owl Enamel Toilet Cream, a product she had used for the previous 12 years, which also was found to contain high levels of lead.35
In 1938, the U.S. Congress passed the Food, Drug, and Cosmetic Act, which stated that a cosmetic would be considered adulterated “[i]f it bears or contains any poisonous or deleterious substance which may render it injurious to users.”36 Although the modern era ushered in a suite of new product safety standards in the United States and elsewhere, potentially hazardous products that escape regulation where they are produced and sold continue to be available to the public.
Traditional Cosmetics, Contemporary Problems
In a study from Ghana, Marian Asantewah Nkansah, an associate professor of chemistry at Kumasi’s Kwame Nkrumah University of Science and Technology, investigated the lipsticks sold in her country. “I decided to work on lipstick in particular,” says Nkansah, “since it is applied on the lips and users have the tendency to lick and swallow. I was curious to know if the products were safe.” Many were, but some were not. Although the Ghana Standards Authority sets a permissible lead limit of in cosmetics,37 a couple of the samples surpassed that limit by a wide margin, with concentrations of up to .38
“Most of the colored pigments used in lipstick production are from heavy metal complexes,” says Nkansah. “Some manufacturers may get away with noncompliance to the set standards if the regulatory bodies are not vigilant.” She says she hopes her research can raise awareness about the dangers of certain low-quality lipsticks.

Multiple studies suggest that shimmery lipsticks tend to contain especially high concentrations of lead, possibly because lead may occur in rocks alongside the mineral mica, which adds the sparkle.15 In some tests, brown and bright pink shades tended to contain more lead than other colors.15,51 Image: © iStockphoto/Rawpixel.
In Pakistan, researcher Laila Shahzad, an assistant professor at Government College University in Lahore, has a similar goal. An analysis she conducted on heavy metals in lipsticks sold in Pakistan showed that 7 of 15 lipsticks sampled contained lead.39 The maximum detected was , more than five times the FDA’s recommended limit.
“We bought our samples from the local market, and a few had packages like Revlon or L’Oréal Paris, but they were not made by the same company. They were fake products,” says Shahzad. “Many are prepared locally. But consumers don’t know. They are just looking at color and the product without looking at who is creating them.” However, even bona fide name-brand products can contain high levels of lead and other metals.40,41,42,43
No example shows how regulations fail more than the continued use of kohl in many countries. Although India, like the United States, restricts the amount of lead in cosmetic color additives to ,44 surma or kajal found in the market often contains excessive amounts of lead. In one study in Kolkata, researchers found that locally purchased surma samples averaged (depending on color) as much as one-third lead by weight.45 In that community, parents were using surma on babies and young children to protect them from the evil eye and because the product was thought to strengthen their eyesight. Children who received two or three applications of kohl or surma per day had blood lead levels much higher than their peers who did not wear the products, with mean concentrations of and , respectively. By comparison, the U.S. Centers for Disease Control and Prevention recommends intervention if a child’s blood lead reaches .46
Kohl continues to be used in many countries and is even available at specialized markets and stores in Europe, says Montserrat Filella, a research chemist at the University of Geneva in Switzerland. When Filella was writing a book on antimony, she noticed that multiple sources said one of the first uses of antimony was in kohl in ancient Egypt. So she decided to investigate whether kohl is still made with the metal.
Filella started collecting samples in several European countries; some were bought directly in shops, and others were purchased from online retailers such as Amazon and eBay. When she analyzed the first samples, she found little antimony but a good deal of lead. Other products were soon tested with similar results—many with packaging that promised the product was free of antimony or lead. Of 23 samples, only 4 contained any antimony, and then only trace amounts. Lead, however, was present in 17 samples, including some that were more than 40% lead by weight.23
“This [adulterated] kohl is, in fact, illegal in European countries and in the United States,” says Filella. “But in spite of being forbidden, it’s easily available.”

From left: The eyes of a baby in India have been lined with kohl; a boy in Bangladesh has kohl applied to his eyes before prayers. In some cultures, kohl and similar products are believed to help children’s eyes develop as well as protect them against ill magic. Images: © iStockphoto/bambam kumar jha; © G.M.B. Pakash/Panos Pictures.
Kohl is not the only product of concern that escapes regulatory frameworks. Women in South Asia use a powder called sindoor to apply a bindi (dot) to their forehead; they also use it to decorate the part of their hair. Sindoor sometimes contains mercury sulfide and is often mixed with lead, says Virendra Shende, an associate professor of forensic biology at the Government Institute of Forensic Science in Nagpur, India.47 “Due to the reddish color of the lead oxide, they mix that particular component in the market to give it the bright color,” he says. Many women apply it every day, he says.
Building Better Methods
The global cosmetic market continues to grow exponentially with a predicted value of by 2024.48 Issues with contamination are likely to continue to grow as well, as people are unlikely to give up age-old traditions such as using henna, kohl, or sindoor. “It’s tough,” says McCartor of Pure Earth, noting that education is less effective for public health issues that are embedded in a population’s culture. “You could tell people that this product is toxic. But if that product is part of their cultural tradition and religion, then the odds are low that they change their behavior simply because some unnamed person in a public education campaign said so.”

Married women in South Asia wear bright red or orange sindoor in the part in their hair to indicate marriage status. Sindoor is also applied to the forehead for cosmetic or religious purposes. A 2017 study52 found that 43% of sindoor samples purchased in India exceeded FDA limits on lead in cosmetics, compared with 19% of samples imported from India and sold in the United States. Image: © iStockphoto/rnmitra.
However, more ways to detect contamination could help protect people from dangerous cosmetics and potentially pave the way for more protective regulations. Shahzad in Pakistan is planning to start a new project on henna temporary tattoos, also known as mehndi, later this year. She will sample both red and black varieties of henna and different preparations available at the market. Shahzad is also researching possible testing methods that would be effective and accessible to her in Pakistan with limited research funds. “I’ll be looking for all the heavy metals,” she says, “whatever the lab will allow me.”
In India, Virendra Shende is working on a more cost-effective method to detect the presence of lead in sindoor. “We found a simple technique, a filter paper technique, so that everyone can easily use it to find out if there’s lead,” he says. His research team used filter papers treated with a reagent that turns pink or purple if lead is present.47 “We have to go for more cost-effective ways to detect trace amount of lead contamination and protect people from dangerous health-related issues due to cosmetics.”
In Brazil, Márcia Foster Mesko, a professor at Universidade Federal de Pelotas, is working on safer and more sensitive methods to detect ever-smaller traces of lead in lipsticks.49 “Usually the limit of detection using conventional analytical methods is quite high, around .” She says this is typically a function of the challenges50 involved in converting solid samples into a solution. Of her methods, Mesko says, “We have made it four times lower, so around , and avoided the use of hydrofluoric acid, which is extremely dangerous.”
According to Mesko, the results achieved with more sensitive testing can help regulatory agencies establish limits for lead in cosmetics. She also suggests industry should be required to add labeling information about potential contaminants in products. “In this case, the consumers can choose the products according to the quality, presence of contaminants, and price,” she says. “Moreover, with clear regulation of contaminants such as lead in lipsticks, the industry will use better raw materials for their products.”
Biography
Jori Lewis writes about the environment and agriculture mostly from the Global South. Her first book, Slaves for Peanuts: A Story of Conquest, Liberation, and a Crop That Changed History, was published in 2022.
References
- 1.U.S. Food and Drug Administration. Henna. Code of Federal Regulations, Title 21 §73.2190. https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-73/subpart-C/section-73.2190 [accessed 16 March 2022].
- 2.Jallad KN, Espada-Jallad C. 2008. Lead exposure from the use of Lawsonia inermis (henna) in temporary paint-on-tattooing and hair dying. Sci Total Environ 397(1–3):244–250, PMID: , 10.1016/j.scitotenv.2008.02.055. [DOI] [PubMed] [Google Scholar]
- 3.Ibrahim SY, Fawzi MM, Saad MG, Rahman SMA. 2016. Determination of heavy metals and other toxic ingredients in henna (Lawsonia inermis). J Environ Anal Toxicol 6(3):1000364, 10.4172/2161-0525.1000364. [DOI] [Google Scholar]
- 4.Aktas Sukuroglu A, Battal D, Burgaz S. 2017. Monitoring of Lawsone, p‐phenylenediamine and heavy metals in commercial temporary black henna tattoos sold in Turkey. Contact Dermatitis 76(2):89–95, PMID: , 10.1111/cod.12702. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Food and Drug Administration. 2016. Draft Guidance for Industry: Lead in Cosmetic Lip Products and Externally Applied Cosmetics: Recommended Maximum Level. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/draft-guidance-industry-lead-cosmetic-lip-products-and-externally-applied-cosmetics-recommended [accessed 16 March 2022].
- 6.Bellinger DC. 2005. Teratogen update: lead and pregnancy. Birth Defects Res A Clin Mol Teratol 73(6):409–420, PMID: , 10.1002/bdra.20127. [DOI] [PubMed] [Google Scholar]
- 7.Wani AL, Ara A, Usmani JA. 2015. Lead toxicity: a review. Interdiscip Toxicol 8(2):55–64, PMID: , 10.1515/intox-2015-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lanphear BP, Hornumg R, Khoury J, Yolton K, Baghurst P, Bellinger DC, et al. 2005. Low-Level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect 113(7):894–899, PMID: , 10.1289/ehp.7688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canfield RL, Henderson CR Jr, Cory-Slechta DA, Cox C, Jusko TA, Lanphear BP. 2003. Intellectual impairment in children with blood lead concentrations below 10 μg per deciliter. N Engl J Med 348(16):1517–1526, PMID: , 10.1056/NEJMoa022848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kordas K, Canfield RL, López P, Rosado JL, Vargas GG, Cebrián ME, et al. 2006. Deficits in cognitive function and achievement in Mexican first-graders with low blood lead concentrations. Environ Res 100(3):371–386, PMID: , 10.1016/j.envres.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Roy A, Bellinger D, Hu H, Schwartz J, Ettinger AS, Wright RO, et al. 2009. Lead exposure and behavior among young children in Chennai, India. Environ Health Perspect 117(10):1607–1611, PMID: , 10.1289/ehp.0900625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chiodo LM, Jacobson SW, Jacobson JL. 2004. Neurodevelopmental effects of postnatal lead exposure at very low levels. Neurotoxicol Teratol 26(3):359–371, PMID: , 10.1016/j.ntt.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Weuve J, Korrick SA, Weisskopf MG, Ryan LM, Schwartz J, Nie H, et al. 2009. Cumulative exposure to lead in relation to cognitive function in older women. Environ Health Perspect 117(4):574–580, PMID: , 10.1289/ehp.11846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obeng-Gyasi E, Armijos RX, Weigel MM, Filippelli GM, Sayegh MA. 2018. Cardiovascular-related outcomes in U.S. adults exposed to lead. Int J Environ Res Public Health 15(4):759, PMID: , 10.3390/ijerph15040759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Saleh I, Al-Enazi S, Shinwari N. 2009. Assessment of lead in cosmetic products. Regul Toxicol Pharmacol 54(2):105–113, PMID: , 10.1016/j.yrtph.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Michalek IM, Benn EKT, Dos Santos FLC, Gordon S, Wen C, Liu B. 2019. A systematic review of global legal regulations on the permissible level of heavy metals in cosmetics with particular emphasis on skin lightening products. Environ Res 170:187–193, PMID: , 10.1016/j.envres.2018.12.029. [DOI] [PubMed] [Google Scholar]
- 17.Obeng-Gyasi E. 2019. Sources of lead exposure in various countries. Rev Environ Health 34(1):25–34, PMID: , 10.1515/reveh-2018-0037. [DOI] [PubMed] [Google Scholar]
- 18.Perlstein MA, Attala R. 1966. Neurologic sequelae of plumbism in children. Clin Pediatr (Phila) 5(5):292–298, 10.1177/000992286600500510. [DOI] [Google Scholar]
- 19.Needleman HL, Gunnoe C, Leviton A, Reed R, Peresie H, Maher C, et al. 1979. Deficits in psychologic and classroom performance of children with elevated dentine lead levels. N Engl J Med 300(13):689–695, PMID: , 10.1056/NEJM197903293001301. [DOI] [PubMed] [Google Scholar]
- 20.Schaffer SE. 2007. Reading our lips: the history of lipstick regulation in Western seats of power. Food Drug Law J 62(1):165–225, PMID: , http://www.jstor.org/stable/26660916 [accessed 16 March 2022]. [PubMed] [Google Scholar]
- 21.Navarro-Tapia E, Serra-Delgado M, Fernández-López L, Meseguer-Gilabert M, Falcón M, Sebastiani G, et al. 2021. Toxic elements in traditional kohl-based eye cosmetics in Spanish and German markets. Int J Environ Res Public Health 18(11):6109, PMID: , 10.3390/ijerph18116109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Witkowski JA, Parish LC. 2001. You’ve come a long way baby: a history of cosmetic lead toxicity. Clin Dermatol 19(4):367–370, PMID: , 10.1016/S0738-081X(01)00196-1. [DOI] [PubMed] [Google Scholar]
- 23.Filella M, Martignier A, Turner A. 2020. Kohl containing lead (and other toxic elements) is widely available in Europe. Environ Res 187:109658, PMID: , 10.1016/j.envres.2020.109658. [DOI] [PubMed] [Google Scholar]
- 24.Mahmood ZA, Azhar I, Ahmed SW. 2019. Kohl Use in Antiquity: Effects on the Eye. In Toxicology in Antiquity. 2nd ed. Wexler P, ed. London, UK: Academic Press, 93–103. [Google Scholar]
- 25.Tapsoba I, Arbault S, Walter P, Amatore C. 2010. Finding out Egyptian gods’ secret using analytical chemistry: biomedical properties of Egyptian black makeup revealed by amperometry at single cells. Anal Chem 82(2):457–460, PMID: , 10.1021/ac902348g. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. 2012. Infant lead poisoning associated with use of tiro, an eye cosmetic from Nigeria—Boston, Massachusetts, 2011. MMWR Morb Mortal Wkly Rep 61(30):574–576, PMID: . [PubMed] [Google Scholar]
- 27.Tiffany-Castiglioni E, Barhoumi R, Mouneimne Y. 2012. Kohl and surma eye cosmetics as significant sources of lead (Pb) exposure. J Local Global Health Sci 2012(1):1, 10.5339/jlghs.2012.1. [DOI] [Google Scholar]
- 28.Beck L, Caffy I, Delqué-Količ E, Moreau C, Dumoulin JP, Perron M, et al. 2018. Absolute dating of lead carbonates in ancient cosmetics by radiocarbon. Commun Chem 1(1):34, 10.1038/s42004-018-0034-y. [DOI] [Google Scholar]
- 29.Schafer EH. 1956. The early history of lead pigments and cosmetics in China. Toung Pao 44(1):413–438, 10.1163/156853256X00135. [DOI] [Google Scholar]
- 30.Blanco-Dávila F. 2000. Beauty and the body: the origins of cosmetics. Plast Reconstr Surg (1963) 105(3):1196–1204, 10.1097/00006534-200003000-00058. [DOI] [PubMed] [Google Scholar]
- 31.Thomas LM. 2020. Beneath the Surface: A Transnational History of Skin Lighteners. Durham, NC: Duke University Press. [Google Scholar]
- 32.Nakashima T, Matsuno K, Matsushita M, Matsushita T. 2011. Severe lead contamination among children of samurai families in Edo period Japan. J Archaeol Sci 38(1):23–28, 10.1016/j.jas.2010.07.028. [DOI] [Google Scholar]
- 33.Zero Mercury Working Group. 2022. Skin Lighteners Still Online Despite Mercury Findings. https://eeb.org/wp-content/uploads/2022/03/ZMWG-Skin-2022-Report-Final.pdf [accessed 16 March 2022].
- 34.Sayre LA. 1869. Three cases of palsy from the use of a cosmetic called “Laird’s Bloom of Youth.” Extracted from the Transactions of the American Medical Association. http://resource.nlm.nih.gov/101636361 [accessed 16 March 2022].
- 35.Woltman HW. 1922. Lead poisoning from face enamel. JAMA 79(20):1685, 10.1001/jama.1922.26420200001013. [DOI] [Google Scholar]
- 36.U.S. Food and Drug Administration. Adulterated Cosmetics. Code of Federal Regulations, Title 21 §361. https://www.law.cornell.edu/uscode/text/21/361 [accessed 16 March 2022].
- 37.Ghana Standards Authority. 2017. Ghana Standard GS 227-3:2017. Code of Practice for Cosmetics Industries: list of Substances Restricted in Cosmetic Products. Accra, Ghana: Ghana Standards Authority. [Google Scholar]
- 38.Nkansah MA, Owusu-Afriyie E, Opoku F. 2018. Determination of lead and cadmium contents in lipstick and their potential health risks to consumers. J Verbrauch Lebensm 13(4):367–373, 10.1007/s00003-018-1180-y. [DOI] [Google Scholar]
- 39.Munir A, Hayyat MU, Shahzad L, Sharif F, Farhan M, Ghafoor GZ. 2020. Assessment of heavy metals concentrations in commercially available lipsticks in Pakistan. Environ Forensics 21(3–4):259–266, 10.1080/15275922.2020.1771632. [DOI] [Google Scholar]
- 40.Consumer Education and Research Centre. 2016. Shocking! Arsenic on your lips and lead in your eyes. https://cercindia.org/first-test-report/ [accessed 16 March 2022].
- 41.Liu S, Hammond K, Rojas-Cheatham A. 2013. Concentrations and potential health risks of metals in lip products. Environ Health Perspect 121(6):705–710, PMID: , 10.1289/ehp.1205518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.U.S. Food and Drug Administration. 2020. Limiting lead in lipstick and other cosmetics. [Website.] Updated 25 February 2022. https://www.fda.gov/cosmetics/cosmetic-products/limiting-lead-lipstick-and-other-cosmetics [accessed 16 March 2022].
- 43.Campaign for Safe Cosmetics. 2007. A Poison Kiss: the Problem of Lead in Lipstick. https://www.womensvoices.org/wp-content/uploads/2010/06/PoisonKiss1.pdf [accessed 16 March 2022].
- 44.Sahu R, Saxena P, Johnson S. 2014. Heavy Metals in Cosmetics. PML/PR-45/2014. https://cdn.cseindia.org/userfiles/Heavy_Metals_in_Cosmetics_Report.pdf [accessed 21 July 2021].
- 45.Goswami K. 2013. Eye cosmetic ‘surma’: hidden threats of lead poisoning. Indian J Clin Biochem 28(1):71–73, PMID: , 10.1007/s12291-012-0235-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. 2021. Recommended actions based on blood lead level. [Website.] Last reviewed 15 March 2022. https://www.cdc.gov/nceh/lead/advisory/acclpp/actions-blls.htm [accessed 16 March 2022].
- 47.Paikrao HM, Shende VA. 2020. Investigation of adulteration in kumkum. Mater Today Proc 29(pt 3):801–806, 10.1016/j.matpr.2020.04.754. [DOI] [Google Scholar]
- 48.Global Cosmetics Products Market-Analysis of Growth, Trends and Forecasts (2018–2023), Mordor Intelligence, Texas, USA, 2018. Cited in: Mesko MF, Novo DLR, Costa VC, Henn AS, Flores EMM. 2020. Toxic and potentially toxic elements determination in cosmetics used for make-up: a critical review. Anal Chim Acta 1098:1–26, PMID: , 10.1016/j.aca.2019.11.046. [DOI] [PubMed] [Google Scholar]
- 49.Mesko MF, Novo DLR, Rondan FS, Pereira RM, Costa VC. 2017. Sample preparation of lipstick for further cd and Pb determination by ICP-MS: is the use of complexing acids really necessary? J Anal At Spectrom 32(9):1780–1788, 10.1039/C7JA00139H. [DOI] [Google Scholar]
- 50.Mesko MF, Novo DLR, Costa VC, Henn AS, Flores EMM. 2020. Toxic and potentially toxic elements determination in cosmetics used for make-up: a critical review. Anal Chim Acta 1098:1–26, PMID: , 10.1016/j.aca.2019.11.046. [DOI] [PubMed] [Google Scholar]
- 51.Khalid A, Bukhari IH, Riaz M, Rehman G, Ain Q, Bokari TH, et al. 2013. Determination of lead, cadmium, chromium, and nickel in different brands of lipsticks. Int J Biol Pharm Allied Sci 2(5):10031009. [Google Scholar]
- 52.Shah MP, Shendell DG, Strickland PO, Bogden JD, Kemp FW, Halperin W. 2017. Lead content of sindoor, a Hindu religious powder and cosmetic: New Jersey and India, 2014–2015. Am J Public Health 107(10):1630–1632, PMID: , 10.2105/AJPH.2017.303931. [DOI] [PMC free article] [PubMed] [Google Scholar]


