Case presentation
A 76-year-old woman was admitted for surgical aortic valve replacement for severe aortic valve stenosis and left atrial appendage occlusion. The pre-operative coronary angiography showed patent coronary arteries with anomalous origin of the left circumflex (LCX) arising as a side branch from the right coronary artery (Figure 1A and B). The surgery was successfully performed without complications and a bioprosthetic Edwards Perimount aortic valve of 21 mm has been implanted. Four days after surgery, the patient developed an acute respiratory distress requiring 3 L of oxygen with positive troponin level that rises from 1800 to 2100 ng/L (normal range <14 ng/L). The transthoracic echocardiography (TTE) showed new onset hypokinaesia of the lateral myocardial wall and 12-lead electrocardiogram (EKG) showed significantly depressed ST-segment on infero-lateral leads. She was diagnosed with non-ST-elevation myocardial infarction (NSTEMI) and underwent emergent coronary angiography which revealed subocclusive stenosis of the LCX related to an extrinsic compression by the bioprosthetic aortic valve (Figure 1C and D). On observing the clinical context and acute setting of NSTEMI, we decided to proceed with percutenaous coronary intervention (PCI) and stent implantation rather than re-do surgery. After crossing the obstructive lesion via a guidewire, we dilated a 2 mm × 15 mm balloon and deployed a 3 mm × 22 mm drug-eluting stent. Then, a post-dilation via a 3 mm × 12 mm non-compliant balloon permits to alleviate the residual in-stent stenosis (Figure 1E and F). We note instant improvement of the clinical condition, normalization of EKG abnormalities, reduction in troponin level, and a good outcome in completely asymptomatic patient with normal TTE at 6 months of follow-up.
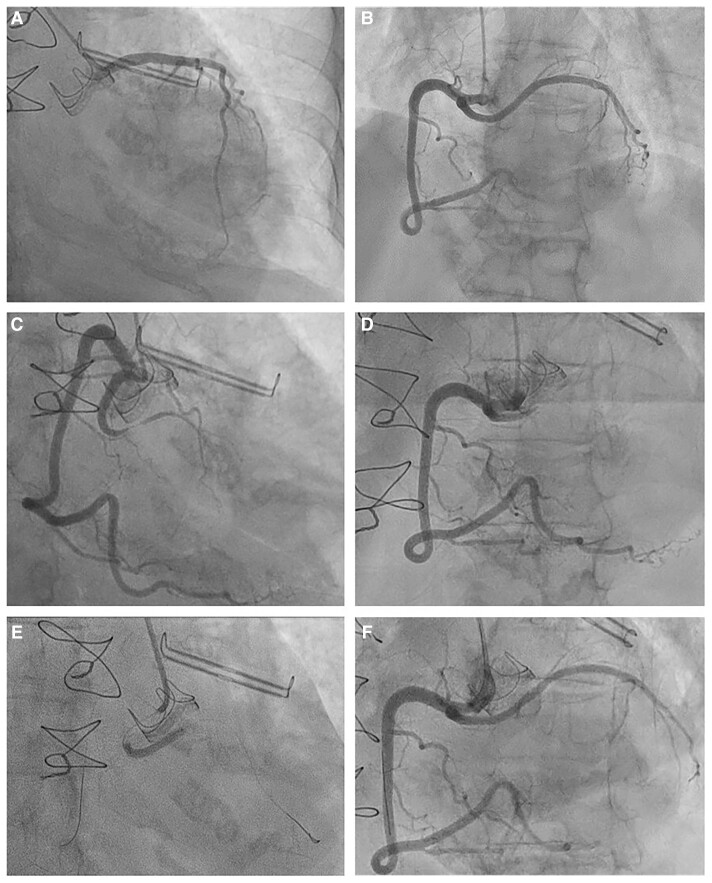
Figure 1.
(A and B) Pre-operative coronary angiograms showed patent left coronary arteries and right coronary artery with anomalous origin of left circumflex artery. (C and D) Post-operative coronary angiograms showed a subocclusive stenosis of the left circumflex coronary successfully treated by (E and F) percutaneous stent angioplasty.
The risk of coronary compression is particularly reconsidered before transcatheter pulmonary valve implantation and represents the major contra-indication.1,2 Data from the literature have identified the anomalous course of coronary arteries as independent risk factor.2 The appropriate management of coronary compression syndrome is not well defined but establishment of normal blood flow is the main purpose. Herein, we report on the feasibility of PCI despite the technical challenges and risk of restenosis (11%),3 especially in high-surgical-risk patients.
All authors have contributed equally for this manuscript.
Lead author biography

Dr Clément Servoz is an interventional cardiologist at University Hospital of Toulouse, France. His research interests include coronary physiology assessment, coronary microvascular disease, and angioplasty.
Consent: The authors confirm that consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidelines.
Conflict of interest: none declared.
Funding: This work was funded by the Toulouse University Hospital.
References
- 1. Morray BH, McElhinney DB, Cheatham JP, Zahn EM, Berman DP, Sullivan PM, Lock JE, Jones TK. Risk of coronary artery compression among patients referred for transcatheter pulmonary valve implantation. Circ Cardiovasc Interv 2013;6:535–542. [DOI] [PubMed] [Google Scholar]
- 2. Rinaldi E, Sadeghi S, Rajpal S, Boe BA, Daniels C, Cheatham J, Sinha S, Levi DS, Aboulhosn J. Utility of CT angiography for the prediction of coronary artery compression in patients undergoing transcatheter pulmonary valve replacement. World J Pediatr Congenit Heart Surg 2020;11:295–303. [DOI] [PubMed] [Google Scholar]
- 3. Aydin M, Ozeren A, Peksoy I, Cabuk M, Bilge M, Dursun A, Elbey MA. Myocardial ischemia caused by a coronary anomaly: left circumflex coronary artery arising from right sinus of valsalva. Tex Heart Inst J 2004;31:273–275. [PMC free article] [PubMed] [Google Scholar]