Abstract
Background
The unprecedented challenges introduced by the Coronavirus disease 2019 (COVID-19) pandemic may be amplified for children with autism spectrum disorder (ASD) and their families.
Aims
The current study aimed to describe the experiences of children with ASD and their families during the pandemic and to identify the needs of this community during emergency situations.
Methods and procedures
Participants were 122 parents of 122 children and adolescents (aged 3–18 years; one parent per family participated) with ASD living in Arizona, USA who participated in the first time point (July/August 2020) of a larger longitudinal survey study. A qualitative approach based in grounded theory methodology was used to analyze six open-ended survey questions.
Outcomes and results
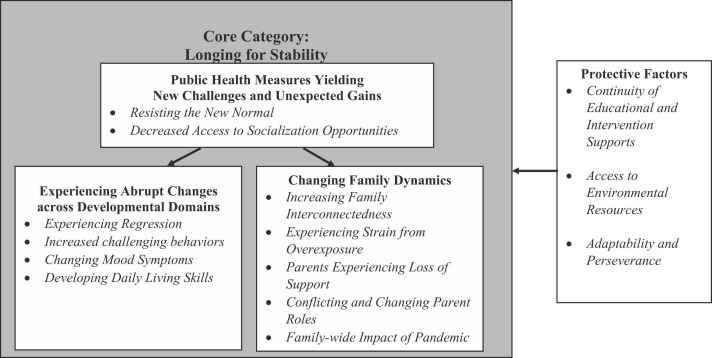
The resulting conceptual model included a core category, Longing for Stability, and four main categories: Public Health Measures Yielding New Challenges and Unexpected Gains, Experiencing Abrupt Changes across Developmental Domains, Changing Family Dynamics, and Protective Factors.
Conclusions
Findings add to limited research examining whether, and how, emergency events uniquely impact the ASD community, identifying potential methods by which services can be proactively adapted to best support the needs of children with ASD.
Keywords: COVID-19, Autism spectrum disorder, Children, Adolescents, Caregivers
1. Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by social communication challenges and restricted and repetitive behaviors (American Psychiatric Association, 2013). Although individuals with ASD have many strengths, they often demonstrate behaviors that negatively affect their own and family members’ quality of life (e.g., meltdowns, aggression, self-injury; Baghdadli, Pry, Michelon, & Rattaz, 2014; Özgür, Aksu, & Eser, 2018), and restricted and repetitive behaviors (e.g., self-stimulatory behaviors, rigidity; Gabriels, Cuccaro, Hill, Ivers, & Goldson, 2005) that may impede functional independence. Many require medical (Liptak, Stuart, & Auinger, 2006), educational (Brookman-Frazee et al., 2009), and behavioral (Kohler, 1999, Thomas et al., 2007) supports throughout the lifespan. Thus, families often pursue services focused on core and associated symptoms, and some of these services are argued to be medically necessary (National Conference of State Legislatures, 2018).
Considering the additional resources and support required by many individuals with ASD (Kalb et al., 2021), this population was especially vulnerable to the unprecedented challenges introduced by the Coronavirus disease 2019 (COVID-19) pandemic. In a review of the literature, Stough, Ducy, and Kang (2017) found that prior to the pandemic, research on the impact of disasters and other emergency events on individuals with ASD was markedly limited. They also highlighted the alarming paucity of research on the experiences of children with disabilities during disasters or terrorism and the need for research regarding the resiliency and mental health of children with disabilities in response to these events.
Although still limited, there is a growing body of literature focused on the experiences of individuals with ASD during the pandemic. Early research suggested that public health measures implemented to slow the spread of COVID-19 reduced many families’ access to autism-related services (SPARK: Simons Foundation Powering Autism Research for Knowledge, 2020, Jeste et al., 2020). Further, some individuals with ASD have challenges adhering to public health guidelines such as mask-wearing, proper hand-washing techniques, and maintaining distance from others (Kalb et al., 2021). This is especially concerning as research suggests that individuals with ASD are four times more likely to be hospitalized due to COVID-19 than individuals without ASD (Karpur, Vasudevan, Shih, & Frazier, 2021).
A parent survey study conducted in Northern Italy (an area severely impacted by the first wave of the pandemic) in April 2020 found that the majority of more than 500 families faced increased challenges managing daily activities and more than one third reported increased intensity and/or frequency of their child’s behavior problems (Colizzi et al., 2020). Other survey studies conducted outside of the United States indicate increased sleep disruption in children with ASD during a home confinement period (Türkoğlu, Uçar, Çetin, Güler, & Tezcan, 2020), limited academic and therapeutic support, heightened levels of parent stress (Alhuzimi, 2021), and significant increases in ASD-related behaviors such as self-stimulatory behavior, self-injury, and hypersensitivity (Mutluer, Doenyas, & Aslan Genc, 2020). A mixed-methods study conducted in Michigan, USA three days after a stay-at-home order was issued in the state found that greater ASD symptom severity was associated with higher levels of caregiver stress. Thematic analyses in the same study highlighted themes related to caregiver stressors (e.g., financial; health), person with ASD stressors (e.g., behavior concerns; change in routine), services stressors (e.g., school absence; therapeutic concerns), and concerns about in-home respite care (Manning, Billian, Matson, Allen, & Soares, 2021). Several studies conducted in multiple countries suggest that parents of children with ASD experienced heightened stress compared to parents of children without ASD (Cheng, Yang, & Deng, 2021, China; Kalb et al., 2021, US; Siracusano et al., 2021, Italy) which may be a downstream effect of the unique challenges faced by their children.
Despite findings indicating mostly negative changes, qualitative inquiries have also identified growth experienced by individuals with ASD and their families. In a qualitative analysis of the experiences of 15 parents of children with ASD, parents expressed challenges explaining safety precautions, new transitions, fewer opportunities to interact with peers, frustration related to e-learning, and stress specifically related to keeping their children safe from the virus. However, some families reported positive changes, including improvements in daily living skills and reduced anxiety, self-injury, and other behavioral issues due to reduced academic demands (Parenteau et al., 2020). Echoing reports of challenges and growth, a mixed-method study of parents of children with ASD and developmental disorders in Turkey reported reduced access to educational resources and socialization opportunities, and increased conflict among family members. However, findings also documented increased time with family and progress in child verbal behaviors and self-care skills (Meral, 2021).
The current study contributes to limited literature describing the experiences of children with ASD and their parents during the pandemic. We conducted qualitative analysis of open-ended survey questions collected as a part of a longitudinal study examining the experiences of parents of children with ASD living in Arizona, USA. This analysis focuses on responses during the first wave of data collection (July/August 2020), which occurred approximately 4–5 months after initial stay at-home orders and school closures were issued in Arizona. Parents’ retrospective responses reflect their experiences over approximately two months of telelearning (March to May 2020) and two-to-three months of summer break. Research questions included: (1) How is the pandemic affecting children with ASD and their families? and (2) What additional resources, if any, do children with ASD and their families need during emergency situations like the COVID-19 pandemic?
2. Methods
2.1. Participants
Participants were 122 parents of 122 children and adolescents (ages 3–18 years) with ASD living in Arizona. One parent of each child was recruited to participate in the study. Participant demographics are reported in Table 1. Parents were recruited through social media and outreach to families who have agreed to be contacted about research within a non-profit autism center’s database. To reduce the possibility of enrolling participants who did not have a child with ASD, parents completed a phone screening prior to enrolling. Participants were emailed links to two separate survey instruments, hosted by JotForm.com and WPS Online. The first survey included an electronic consent form, which indicated that participants must be able to read and write fluently in English. Surveys were completed in July or August of 2020 and participants received a $15 gift card to an online retailer after completing both surveys. Twenty participants did not complete both surveys and were excluded from the study. All study procedures were approved by the Arizona State University Institutional Review Board.
Table 1.
Participant demographics (n = 122).
| M (SD) or % | |
|---|---|
| Parent Age | 39.76 (8.91) |
| Parent Gender | |
| Male | 9.0% |
| Female | 89.3% |
| Did Not Report | 1.6% |
| Focal Child Age | 8.42 (4.39) |
| Focal Child Gender | |
| Male | 75.4% |
| Female | 22.1% |
| Did Not Report | 2.5% |
| Focal Child Race | |
| American Indian/Alaska Native | 1.6% |
| Asian/Asian American | 4.1% |
| Black/African American | 2.5% |
| White/Caucasian | 81.1% |
| Multiple/Other | 9.8% |
| Did Not Report | 0.8% |
| Focal Child Ethnicity | |
| Hispanic or Latino | 24.6% |
| Not Hispanic or Latino | 74.6% |
| Did Not Report | 0.8% |
| Household Income (US dollars) | |
| < $24,999 | 6.6% |
| $25,000–49,999 | 13.9% |
| $50,000–74,999 | 21.3% |
| $75,000–99,999 | 13.9% |
| $100,000–149,000 | 18.0% |
| $150,000–199,999 | 7.4% |
| > $200,000 | 18.0% |
| Did Not Report | 0.8% |
| ABAS-3 Adaptive Functioning | |
| General Adaptive Composite | 69.54 (13.75) |
| Conceptual | 70.71 (14.32) |
| Social | 72.40 (14.76) |
| Practical | 73.31 (14.30) |
Note. ABAS-3 = Adaptive Behavior Assessment System, Third Edition
2.2. Measures
2.2.1. Child adaptive functioning
To characterize the sample, parents were asked to report on their child’s adaptive functioning using the Adaptive Behavior Assessment System, Third Edition (ABAS-3; Harrison & Oakland, 2015), a norm-referenced assessment that evaluates adaptive functioning across three domains: conceptual, social, and practical. Domain scores and the General Adaptive Composite (GAC) score are standardized, with a mean of 100 and standard deviation of 15. Higher scores indicate better adaptive functioning. ABAS-3 scores are reported in Table 1 for sample characterization only and were not intended to be used for mixed-methods analysis.
2.2.2. Investigator-generated online survey
Parents completed an investigator-generated online survey that prompted them to report demographic information and to answer six open-ended survey questions:
-
1)
What negative changes, if any, have you observed in the focal child’s behavior since preventative measures related to COVID-19 were implemented?
-
2)
What positive changes, if any, have you observed in the focal child’s behavior since preventative measures related to COVID-19 were implanted?
-
3)
How have societal changes related to COVID-19 changed the focal child’s service needs?
-
4)
What services, resources, and/or activities have been most helpful to the focal child since preventative measures related to COVID-19 were implemented?
-
5)
How have societal changes related to COVID-19 changed your family’s needs?
-
6)
Is there anything else you think we should know about your child’s or family’s experience during the COVID-19 pandemic?
2.3. Data analysis
Responses were analyzed using strategies from a widely used qualitative approach, grounded theory methodology (Charmaz, 2014). This approach was chosen due to limited existing qualitative research on the current topic and the need for theoretical descriptions of processes contributing to the experiences of the ASD community during emergency events. However, we acknowledge that a true grounded theory analysis, including theoretical sampling, was not feasible due to the data collection method (i.e., survey questions). Responses were coded line-by-line by a team of two coders. One coder was a developmental psychologist who has studied ASD for over a decade. The other coder was a post-baccalaureate research assistant with a degree in psychology who had 1.5 years of experience working as a registered behavior technician with children and adults with ASD. All codes were discussed weekly by both coders to ensure consistency and agreement. Analysis was approached from a constructionist epistemology, which acknowledges the social construction of experiences and the influence of the coders’ pre-existing biases on analysis and interpretation.
Throughout the analytic process, we engaged in constant comparison of codes and memos. During open coding, survey responses were broken into thematic fragments, which were then assigned codes that captured the participant's written response. Axial coding allowed for the organization of open codes into hierarchical categories, which facilitated the focused coding processes and the generation of core and main categories. Resulting categories and how they relate to one another were written into a conceptual model. Trustworthiness was documented through member checking, analyst triangulation, and negative case analysis.
To provide additional context to qualitative findings, post-hoc quantitative analyses examined the frequency of participants who endorsed positive or negative changes in their child’s behavior since the onset of the pandemic. Responses to questions 1 (negative behavioral changes) and 2 (positive behavioral changes) were coded by separate raters as either a “0” if the parent’s response did not endorse anything negative/positive about the child’s behavior, or a “1” if the parent endorsed anything negative/positive about the child’s behavior. Two coders independently coded 100% of the responses. Intraclass correlation coefficients (ICC) and their 95% confidence intervals were calculated based on a single rater, absolute agreement, 2-way mixed-effects model (Question 1 ICC =0.85, 95% CI =0.79–0.89, Cronbach’s alpha =0.92; Question 2 ICC =0.88, 95% CI =0.83–0.92, Cronbach’s alpha =0.94). Disagreements were resolved by discussion.
3. Results
Post-hoc quantitative analyses are reported first to provide context for qualitative findings. Out of a total of 122 participants, 2.5% reported no negative or positive behavioral changes; 26.2% reported at least one negative behavioral change and no positive behavioral changes; 4.9% reported at least one positive behavioral change and no negative behavioral changes, and 66.4% of participants reported both negative and positive behavioral changes. Thus, 92.6% of participants reported at least one negative behavioral change, whereas 71.3% of the sample reported at least one positive behavioral change. Qualitative analysis identified the conceptual model described below and depicted in Fig. 1.
Fig. 1.
Conceptual model. Note. The core category and main categories are bolded; subcategories are italicized. Longing for Stability was pervasive in the reports of children and parents’ experiences and provides background against which the main categories can be understood. Longing for Stability represents increased parent distress and worry regarding their child(ren) with ASD due to instability induced by the pandemic. The main category, Public Health Measures Yielding New Challenges and Unexpected Gains, describes challenges faced as a direct result from public health measures, including children resisting these restrictions and changes, as well as a decrease in access to socialization opportunities. Experiencing Abrupt Changes across Developmental Domains and Changing Family Dynamics were directly influenced by changes caused by public health measures, as these limitations led to child behavioral changes as well as family system wide changes when adjusting to the new normal. Protective Factors mediated the relationship between all main categories.
3.1. Core category: Longing for Stability
Longing for Stability was observed across conceptual categories and represents statements from parents indicating that they were experiencing distress and worry regarding their child(ren) with ASD. Parents frequently indicated that their child “needed” normalcy, reliability, and/or structure. While the definition of stability differed across families, responses highlighted how the pandemic disrupted day-to-day living for most families, and how increased dependency on technology exacerbated disruption to many facets of families’ lives. Themes within this category included the need for reliable technology (e.g., internet access and virtual resources) to foster continued education and health-care services, in-person school, reliable service providers, and general structure and stimulation. Some of these themes represent families’ eagerness to return to pre-pandemic life; however, the core category largely encapsulates families’ reported desire to find structure amidst barriers that emerged during the pandemic. Speaking to the impact of the absence of routine on her child’s autism-related characteristics, the mother of a 6-year-old wrote, “The loss of routine of schooling and in person therapy is absolutely horrible. Behaviors we haven’t seen in 4 years are back. Our hearts are broken and were completely helpless. He’s lost everything [that] propelled him forward. These things cannot be taught and implemented on a computer or in a home.” 1 .
Some parents’ responses suggested that challenges associated with the pandemic were exacerbated by their child’s ASD characteristics. Parents highlighted specific barriers unlikely to be experienced by families with only neurotypical children, including an increase in ASD-related therapy needs due to regression across developmental domains, the emergence of new maladaptive behaviors, and/or increased ASD symptom severity (see Experiencing Abrupt Changes across Developmental Domains). Additionally, parents reported increased specialized childcare needs due to remote learning, changes in parent roles, and job instability. Notably, variance was observed in the level of distress and concern expressed by parents, and a small minority (n = 6) indicated that pandemic-related restrictions had only positive impacts on their child(ren) and families. These sentiments are captured in the category Protective Factors.
3.2. Public Health Measures Yielding New Challenges and Unexpected Gains
Parents described various challenges that stemmed from stay-at-home orders and other public health measures. Although less frequently discussed, parents also reported unexpected positive behavioral outcomes. Two subcategories emerged: (1) Resisting the New Normal, and (2) Decreased Access to Socialization Opportunities.
3.2.1. Resisting the New Normal
Children experienced confusion regarding environmental changes and restrictions resulting from the public health measures. Additionally, some parents reported that their children demonstrated refusal to adapt to the new safety precautions (i.e., social distancing; mask wearing), which, for some, influenced the frequency of tantrums and outbursts. Beyond increased behavioral challenges, parents described instances where their child was unable to comply with the public safety measures, which added to their family’s isolation to the home environment. The parent of a 4-year-old shared, “He can’t wear a mask.we’ve tried and tried but he won’t. So he can’t go many places, we have to find a babysitter just to go grocery shopping.”
Serving as counterexamples to negative outcomes of public health measures, some parents identified unexpected positive behavioral outcomes and growth. Examples include children demonstrating adaptability by learning to wear a mask regularly, learning compassion for those who are sick, demonstrating a desire to keep people safe, and following safety protocols.
3.2.2. Decreased Access to Socialization Opportunities
Many parents discussed the negative impact of pandemic-related restraints on their child’s social development. For example, the parent of a 3-year-old shared: “He is having zero opportunities to practice his social skills. He was starting to follow other children and observe other children more in [school name redacted] when the shutdown occurred. Now he has not left the house except to go for a ride in the car since March.” Discussed in the Experiencing Regression subcategory below, parents reported that regression in social communication skills occurred because of a loss of socialization opportunities, with some parents anticipating a need to play “catch-up” on social skills after the pandemic ends.
Many parents reported that their children experienced negative emotional responses to decreased socialization. Some parents described their children experiencing loneliness and isolation, resulting in various emotional responses including sadness, anger, and overall frustration. The parent of an 8-year-old shared that, “My son yearns for friendship and socialization with peers. He cries a lot because he cannot have a playdate or be in his learning clubs.” Whereas parents encouraged socialization through virtual platforms, some children still expressed the desire to see their peers, providers, and family in person.
The loss of social opportunities appeared to have negative consequences for most children in the current study. However, a minority of parents (n = 5) shared that reduced social interactions resulted in reduced stress for their child. Parent responses suggested that prior to the pandemic, social settings and interactions often resulted in stress and/or aggressive behaviors because of the social communication challenges associated with ASD. The absence of group settings was reported to increase the child's ability to choose their own developmental trajectory, reduce pressure to behave a certain way, and/or allow the child to thrive without social stressors. For example, the parent of an 8-year-old shared: “During school, there are extreme behavior issues such as hitting and kicking peers and teachers. He was extremely stressed and under pressure to act appropriately in school. In the absence of in person education, he has not been hitting and kicking others.”
3.3. Experiencing Abrupt Changes across Developmental Domains
Most parents reported that their children demonstrated both negative and positive changes across various domains. Further, many parents reported ripple effects on their own well-being. This category included four subcategories: (1) Experiencing Regression, (2) Increased Challenging Behaviors, (3) Changing Mood Symptoms, and (4) Developing Independent Living Skills.
3.3.1. Experiencing Regression
Regressions in previously mastered skills or behaviors were reported across multiple domains, including social communication (i.e., regression of speech, communication of needs, social skills, and non-verbal communication skills like eye contact), self-care, executive functioning, emotional control, and fine motor skills. Parents feared that social communication regression would negatively impact their child’s transition back into community and public spaces following the pandemic, and many expressed that they may need assistance re-integrating their child into social situations. Regression across these developmental domains contributed to the challenging behaviors discussed in the Increased Challenging Behaviors category described below. For example, the parent of an 8-year-old reported,
“I can see that [her] social skills, ability to relate to others and show empathy, and self-regulation is deteriorating. She has never needed any therapy or services prior to this experience, but I believe she will now. She is choosing more and more to be alone and the repetitive play activities she enjoys, like she did as a toddler, rather than choosing to interact with us as a family.”
Parents often reported that their child’s regression had a negative impact on their own well-being, causing increased stress and frustration. The parent of a 6-year-old male shared: “We have seen such regression its heartbreaking…We worked 4 years to get to the point of sending [him] to a mainstream kindergarten and online kindergarten is exacerbating the stress and regression. IT IS AWFUL!!!!!.”
3.3.2. Increased Challenging Behaviors
Parents reported that their children demonstrated increased or new behaviors that were challenging for the parent. These included meltdowns, aggression, self-injurious behavior, property destruction, elopement, use of inappropriate language, defiance, reduced patience, and/or the inability for parents to reach compromises with their children. Parents suggested multiple potential triggers for these undesired behaviors, including the need for constant attention from parents, difficulty tolerating a mask or face covering, and lack of access to the child’s preferred activities. A few parents also reported on other challenging behavioral changes, such as sleep disturbances, hyperactivity, and behaviors specific to fear or misunderstanding of the virus.
Parents’ reports indicated that some children demonstrated increased rigidity. Some children developed new routines that were difficult to interrupt, whereas others displayed the inability to transition from one activity to the next without experiencing distress. Many parents reported that their child demonstrated increased motor and vocal self-stimulatory behaviors.
3.3.3. Changing Mood Symptoms
Parents reported that children demonstrated mood changes, including increased negative affect, general anxiety, general fear, and fears and anxiety specific to COVID-19. Parents described their child “feeling down”, being “emotional” or “unhappy”, with some depicting the changing mood symptoms as depression. Relatedly, parents discussed that heightened stress related to the pandemic contributed to decreased happiness among children and family members alike. Some parents also reported that their child’s pre-existing anxiety increased in general, while others described added fear and anxiety specific to the pandemic. Examples include fears of social opportunities, family members catching the virus, being alone if family members died from COVID-19, and losing hope that the pandemic would end.
3.3.4. Developing Independent Living Skills
Some parents highlighted that increased time at home provided opportunities for growth, increased autonomy, and new independent living skills. Parents reported progress in self-care skills such as toileting, teeth brushing, showering, and dressing. Some children became more proficient at completing tasks around the home, like preparing snacks/meals and completing chores. The parent of a 17-year-old shared: “[She] has made great strides in some of the independent living activities around the house that we have more time to work on now. She still needs prompting, but can complete new tasks and can more easily complete old ones.” A few parents also commented that telelearning assisted children in developing computer skills.
3.4. Changing Family Dynamics
Changes to family dynamics were widely reported. This theme diverges from the concepts previously discussed in that parents discussed changes that also impacted other family members rather than experiences isolated to their child with ASD. Five subcategories were included within this category including: (1) Increasing Family Interconnectedness, (2) Experiencing Strain from Overexposure, (3) Parents Experiencing Loss of Support, (4) Conflicting/Changing Parent Roles, and (5) Family-wide Impact of Pandemic.
3.4.1. Increasing Family Interconnectedness
Many parents reported positive family outcomes resulting from increased time spent at home. Parents reported that they spent more time playing games together, eating together, communicating with one another, and a general increased closeness among family members. Changes in sibling dynamics were also noted, with parents sharing that their child with ASD bonded with, displayed increased interest in, and/or developed friendships with their sibling(s). Some parents expressed gratefulness for increased time with their family and the opportunity to develop an increased awareness of their family’s needs. A few parents also noted that increased time with their children opened their eyes to skills that needed improvement, the integral role of therapy services, and the identification of behaviors that may impact their child’s transition into adulthood.
3.4.2. Experiencing Strain from Overexposure
Excessive contact led to strain for some families. Strain resulted from two main sources: sibling conflict and parent-child burnout. Some parents reported that their children experienced sibling conflict, often due to an inability to separate from one another due to environmental constraints. The mother of a 6-year-old female discussed the lengths she went through to adapt their home environment to create individual spaces to combat the increased conflict and overexposure among her children.
“Kids don’t have alone time and also made them go crazy…I converted a space into a bedroom so they could have their own ‘rooms’ and made more ‘alone-time’ sensory spots throughout the house by rearranging furniture and building tents.”
Some parents reported that constant contact with their children, including those without ASD, led to exhaustion, difficulty maintaining patience, inability to partake in hobbies, and burnout.
3.4.3. Parents Experiencing Loss of Support
Many parents reported a loss of support systems on which they previously depended, including in-home service/habilitation providers, access to childcare providers, and social institutions like schools, clubs, and sports. Some parents reported that these losses led to feelings of helplessness and inadequacy to support their own children. These feelings were coupled with parents losing access to their own self-care routines, such as therapy, health services, and receiving support from friendships and extended family members. Some parents also experienced distress due to their child’s regression (discussed under Experiencing Regression above). They reported the inability to manage their children’s maladaptive behavior and a lack of knowledge to help their children cope with the pandemic, causing an overall feeling of loss of control.
3.4.4. Conflicting and Changing Parent Roles
Parents reported difficulty in adopting the roles of teacher, therapist, and a full-time employee in addition to being a parent. There were reports of conflicting priorities, such as working from home impeding the parent’s ability to spend time assisting their children with school and autism-related services. For example, the mother of a 12-year-old female shared: “I'm having to work twice as hard. My job has gone to work from home, so while I’m trying to work, I still have to facilitate my child's therapies and all her schoolwork.” The inability for parents and children to have separate environments and non-familial supports during the day increased parent stress, and in some cases forced parents to prioritize necessity (i.e., work/income) over child supports (e.g., therapy). Parents reported the need to juggle work and provide constant support to their children across a variety of contexts. To be successful, parents had to demonstrate flexibility in filling different roles to meet their children’s needs without supports they were accustomed to prior to the pandemic. Some parents indicated that a state-wide executive order allowing them to become a direct service provider for their child was a helpful resource, whereas other parents indicated that this was not an effective option. For example, the parent of a 12-year-old male shared, “We need (non-parent) habilitation and respite but the risk is too high.”
3.4.5. Family-wide Impact of Pandemic
Although the aim of this study was to identify challenges experienced by children with ASD, responses indicated that siblings and immediate family members also experienced challenges. Parents reported similarities across their other children in longing for socialization, difficulty adapting to change, and limited effectiveness of remote learning. For example, one parent reported:
“I have a 9 year old who is a social butterfly. This has really been difficult on her. My friends are my support. When I can’t meet up with them to talk and relax, my mental health takes a hit. My husband is working from home which is challenging. We all need help and support but we can’t get it because it’s not safe to be around anyone but each other. We’re stuck.”
Another parent described challenges related to parenting multiple children on the autism spectrum during the pandemic:
“This study was about my eldest child with autism; I have a younger son with autism and ADHD as well. His schooling and accommodations have taken much more of my time as I am not a special education teacher or a speech therapist…As a family, we have to decide whose needs come first and who is losing the most ground academically.”
Additionally, some parents elaborated on how contracting COVID-19 negatively impacted their family and how having high risk individuals in their household (e.g., immune compromised) impacted their family’s outcomes. For example, the mother of a 3-year-old shared, “…I got sick with COVID and had to quarantine away from my family for 18 days. This was extremely difficult and traumatic for both of my children, but especially for [my son]. Therapy was stopped for 25 days and I have seen regression from [him] as a result.”
3.5. Protective Factors
Amidst the multiple adverse outcomes resulting from pandemic-related public health measures, parents reported on key resources that provided effective support. Notably, some parents reported that the absence of these resources detracted from their child’s or their own ability to adapt. This section includes three subcategories: (1) Continuity of Educational and Intervention Supports, (2) Access to Environmental Resources, and (3) Adaptability and Perseverance.
3.5.1. Continuity of Educational and Intervention Supports
One of the most consequential changes reported by parents was the transition from in-person to remote learning and autism-related therapies. For some, the continuity of educational and intervention supports through remote platforms was a protective factor, providing parents with necessary resources to adapt to the changes of the pandemic. In contrast, other children faced challenges making the transition to remote learning and/or therapy, creating a distinct obstacle to the child’s functioning and development.
Parents reported multiple protective factors within the context of remote learning, including continued education, virtual meetings with classmates to facilitate socialization, and individualized lesson plans. Notably, a handful of parents (n = 7) indicated increased concentration and motivation to learn from home and/or reductions in maladaptive behaviors. For example, the parents of a 12-year-old shared,
“Home is [his] safe space, and school was extremely challenging due to social challenges and distractions. He was severely depressed due to school and giving up on his academics. Since being home in his “safe” space, he is more motivated to learn and keep up with his schoolwork.”
Further, some parents shared examples of teachers or providers working to individualize remote learning or therapy for their child. The parent of a 17-year-old shared:
“[Her] school has gone out of their way to individualize her tele-school experience. She couldn’t handle watching videos of school staff on the computer…(she doesn’t like people being viewed out of place and our home was the wrong place?), so they arranged a new independent study just for her with You Tube videos and worksheet that I could upload… It took a little bit, but it’s on track now. Of course now she wants tele-school forever.”
Considerably more parents reported barriers to success during the transition to, and maintenance of, remote learning. Barriers included decreased academic progress, lack of school preparation, difficulty adapting to online learning, and the lack of supports to facilitate telelearning (i.e., the loss of 1:1 aids and classroom accommodations). For example, a parent shared that telelearning uncovered her son’s aversion to being on screen, and his school was unable to find an effective solution:
“I had no idea he had aversions to being on screen…it made learning from home impossible, and no one could help us…He attends a private school for unique learners. He has the best of the best team, who are experienced with kids just like him, but this was new and no one had answers for me or my kid.”
Taken together, parents' responses indicated that child preference for being at home and effective teaching strategies promoted resilience during remote learning for a small number of children. Unfortunately, far more families reported difficulties transitioning to remote learning and felt that schools were grossly unprepared to facilitate effective remote learning for children with special needs.
Many autism-related services transitioned to telehealth or moved from being in-clinic to in-home. Again, parent perceptions of outcomes were mixed. Many parents indicated that the continuity of therapies in-home and/or via telehealth modalities were beneficial. Some parents even reported that the switch to receiving applied behavior analysis (ABA) therapies in-home versus in-clinic allowed for increased treatment hours, which appeared to facilitate increased advancements in their child’s development. Other parents reported that the telehealth services were ineffective and caused multiple issues, such as child intolerance of virtual therapy sessions, decreased ability to attend or maintain engagement, lack of feasibility to enact some forms of therapy (i.e., occupational therapy) virtually, and limitations of virtual versus in-person therapy modalities. Parents also reported a general loss of access to ASD-related services and increased difficulty finding new services/service providers during the pandemic.
3.5.2. Access to Environmental Resources
Many parents described that access to various environmental resources served as “life-savers” amidst the closures of community and public spaces. Examples include recreational activities (e.g., swimming pools and outdoor activities), structured activities (e.g., toys, crafts, and movies), technological resources (e.g., reliable internet; videogames), and virtual social activities (e.g., zoom calls with friends and family, multiplayer online games/chat rooms). Parents who lacked access to these types of resources highlighted the absence as a barrier to their child’s and family’s well-being throughout the pandemic.
3.5.3. Adaptability and Perseverance
A concept supported by a handful of parents (n = 9) was that their child demonstrated adaptability and resilience to the constantly changing environment. Parents shared that their children were “faring better than expected”, continuing to develop functional skills despite the pandemic, and were adapting to the loss of routines. Some parents reported on increases in positive affectivity, self-awareness, executive functioning, prosocial behaviors, social communication, decreased tantrums, and anxiety. For example, the parent of an 8-year-old shared, “He has also responded positively to having a less busy and regimented schedule (no extra-curricular activities, no play dates, shorter duration of the school day). He is less tired in the evenings, which has led to fewer emotional meltdowns late in the day.” 2 .
4. Discussion
Prior to the COVID-19 pandemic, research on the experiences of children with ASD and their families during emergencies was virtually non-existent, leaving families and professionals with minimal guidance to assist children with ASD in adapting during the pandemic. Findings from the current study highlight deficits in the therapeutic and educational service systems that resulted in disruptions to care and support for children with ASD. Additionally, findings suggest the need for services and support to help parents address skill regressions and new maladaptive behaviors believed to be a result of public health measures associated with the pandemic. Together with other recent research, findings begin to provide a framework for preparing vulnerable populations for future emergency situations or other times of uncertainty.
Data collection for the current study coincided with a particularly vulnerable time for state of Arizona. Families had already lived through four to five months of the pandemic and some reports indicated that Arizona had the highest rate of per capita infections in the United States during data collection (Fifield, 2020). Despite this, stay-at-home orders had been relaxed, government officials offered mixed guidance regarding mask-mandates (State of Arizona Executive Order, 2020–40, 2020), and mixed opinions regarding modality of schooling was pervasive amidst the start of the school year. Thus, findings from this study offer unique insight into the experiences of parents of children with ASD during an ongoing and constantly evolving emergency event.
With some exceptions, parents generally described their experiences over the first five months of the pandemic as challenging. A sense of longing was palpable in the responses of many parents who expressed a desire for normalcy, or at least increased stability. Some parents acknowledged that the pandemic was challenging for all people, but that adjusting to the new normal with a child with ASD exacerbated challenges. The sense of longing for stability was observed across all other main categories identified through qualitative analysis; thus, Longing for Stability was elevated to the core category.
Responses from most parents indicated that their child experienced negative behavioral changes, including regression in a variety of skill areas, increased or new maladaptive behaviors, and increased mood symptoms. Importantly, a handful of families believed that their child was adjusting well, or even thriving, during the pandemic. These parents discussed how increased time with their children benefitted not only the child, but the entire family. For some these benefits were associated with increased flexibility of parent work (e.g., ability to provide care when working from home). Additionally, these parents noted increases in their children’s daily living skills and/or reduced stress associated with decreased exposure to group settings. Discrepancies in children’s responses to the pandemic-related changes underscore the diversity among individuals on the autism spectrum, but also highlight the potential influence of pre-pandemic variables. For example, the ability to work from home is not an option for all parents and is likely more common for families of higher socioeconomic status. Indeed, all but two of the parents who reported that their child was doing well or thriving also reported household incomes above the median income for Arizona. However, this convenience sample consisted mostly of Caucasian, middle- and high-income families, which precludes a more thorough analysis of the impact of pre-existing differences in socioeconomic status. Findings suggest that experiences during the pandemic were challenging for most families in the current sample. It stands to reason that the experiences of lower income or otherwise marginalized families were equally or more challenging than those reported by participants in the current study.
A common concern among parents was the absence of socialization opportunities for their children. Whereas some families attempted to fill this void with virtual socialization (e.g., video calls and online gaming), other parents lamented that their children would require considerable “catch up” in developing appropriate social skills following the pandemic. These responses highlight the importance of socialization opportunities for children with ASD and may be informative for families considering online or homeschooling outside of emergency events. Further, future research is needed to determine whether virtual socialization platforms provide the same opportunities for social development as in-person interaction.
Many parents described challenges transitioning to telelearning and/or telehealth services, with some children demonstrating adverse reactions, and many parents indicating that remote learning and/or intervention was ineffective or less effective than in-person modalities. Moving forward, it may be advantageous for educators and therapists to consider hybrid curricula or treatment plans that combine in-person learning/therapy with telelearning/teletherapy, respectively, to prepare children with ASD, who often demonstrate difficulty with change, for future disruptions to school and/or therapy. Increased flexibility in the mode of education and service delivery could also reduce missed learning/therapy opportunities if children move, go on vacation, or have unreliable transportation to receive services. Hybrid education and service delivery would provide continuity of learning as sessions and lessons could be held virtually in instances where the child would otherwise miss these services. Further, it is likely beneficial for children to develop social communication skills for both in-person and online settings. A small minority of parents reported that their child preferred learning from home and may not want to return to in-person settings when safe. It will be important for future research to examine whether the benefits introduced by remote learning (i.e., reduced stress/anxiety) outweigh potential adverse effects of children losing opportunities for socialization and in-person learning. Very few participants highlighted difficulties accessing technology, which is consistent with the relatively high socioeconomic status of the current sample. As recently summarized by Kumm, Viljoen, and de Vries (2021), it is essential that future research closely examine the experiences of lower income families with telelearning and teleservices to better understand and minimize disparities within the ASD community.
Continuity of effective educational or intervention services was identified as a protective factor for many children. Children were better able to adapt to the changes associated with the pandemic if their school was able to provide effective telelearning activities, they responded well to telehealth-delivered interventions, or they were able to continue in-person therapies. Some families indicated that their child was able to receive more in-person therapy hours than before the pandemic, which yielded positive outcomes. In contrast, other families reported unpredictable hours of service delivery or the inability to uptake hours due to service provider or parent illness. Instability of service hours and/or schedules was generally associated with negative outcomes for child functioning.
One method to better prepare families for emergency situations and other disruptions to routine could be increased parent/caregiver training in effective educational and intervention strategies (e.g., positive behavior supports). Parents who undergo training would likely be better equipped to promote development and minimize challenging behaviors in the event of future emergency events. Research suggests feasibility, acceptability, and effectiveness of parent training in behavior analytic strategies (Matson et al., 2009, Patterson et al., 2012) and social skills education (Laugeson, Frankel, Gantman, Dillon, & Mogil, 2012); however, the availability of parent training is currently limited. Publicly supported parent training could assist families in non-emergency situations, and may also contribute to continuity of care, reduced parenting stress, and increased family quality of life during emergency events. The Arizona Department of Developmental Disabilities allowed parents to serve as habilitation providers during the pandemic (Division of Developmental Disabilities, 2020), a change that was valued by some parents in the current sample but identified as an issue by others. Although this flexibility was valuable, it may have been more impactful if more parents had training in effective strategies for promoting development of functional skills and managing challenging behaviors. Barriers to the effective dissemination of parent-training have been previously documented (Pickard, Wainer, Bailey, & Ingersoll, 2016). Thus, considerable advocacy would be necessary to increase access and feasibility of parent training for families who do not already have access to this resource.
Importantly, not all parents reported negative changes, and consistent with two other qualitative studies on this topic (Meral, 2021, Parenteau et al., 2020), some reported positive changes and/or the development of new skills. A handful of parents commented on the resilience of their children and some parents reported increased interconnectedness within their family. Further, many parents reported that their child developed new independent living skills during stay-at-home orders.
Lastly, Changing Family Dynamics were described by many parents. Whereas increased time spent at home resulted in increased interconnectedness for some families, other parents described increased sibling conflict and parent fatigue due to overexposure. Generally, parents reported the loss of important supports like childcare and therapies, which required parents to balance multiple roles, sometimes unsuccessfully. Parents reported needing to make difficult decisions about whether therapy hours would need to be missed to accommodate work schedules. They also described the pandemic as having negative effects on the entire family, including their own psychological well-being. A recent large-scale quantitative study found that close to half of parents of children with ASD experienced substantial psychological distress during the early months of the pandemic compared to only 25% of a representative sample of US parents (Kalb et al., 2021). This is consistent with the indication from many parents in the current study that challenges associated with the pandemic are exacerbated for families of children with ASD.
4.1. Limitations
While this study contributes valuable information about the experiences of individuals with ASD and their families during the first four to five months of pandemic, it has several limitations. First, data analyzed for this study were collected at a single time point, which precludes analysis of trends over time or comparison to challenges experienced by families prior to the pandemic. Further, parent accounts at a single time point likely differed from accounts collected earlier or later in the pandemic due to the evolving nature of the pandemic and differing levels of familiarity with changes to daily life.
Qualitative responses were collected through an online survey which was investigator-generated and was unfortunately not piloted prior to data collection because of constraints related to timely data collection. Piloting survey questions may have increased appropriateness (e.g., reading level, clarity of topics, and terminology). Additionally, an interview format may have provided an opportunity for parents to provide additional information and would have allowed for theoretical sampling (Charmaz, 2014). The sample was predominantly Caucasian and middle to upper-middle class. Demographic variables likely influenced families’ experiences (e.g., access to resources, continuity of childcare, parental job security) throughout the pandemic. Thus, current findings may not generalize to other populations. Participants were recruited from a single state within the United States to minimize confounding environmental variables (e.g., mandates; level of community spread). However, there were differences across communities within the state related to these variables that were not measured in the current study and may have impacted participants’ individual experiences.
5. Conclusion
Most children with ASD and their families experienced considerable challenges during the early months of the COVID-19 pandemic, which were perceived by parents to be more difficult than challenges experienced by families of neurotypical children. Families would benefit from increased supports to address child regression and parent distress, including increased flexibility across educational and clinical services, access to parent/caregiver training, and public supports for low-income/marginalized populations. Knowledge gained from the current study and others may be valuable for stakeholders as they develop programming for children with ASD during and after the pandemic.
What this paper adds
This study contributes to the growing body of research illuminating the experiences of individuals with autism spectrum disorder (ASD) and their families during the early months of the Coronavirus disease 2019 (COVID-19) pandemic. Using a qualitative approach, the study aimed to identify how the pandemic affected children and adolescents with ASD and their families and to understand what additional resources, if any, children with ASD and their families may need during emergency situations. Findings revealed that children with ASD and their families experienced considerable challenges during the early months of the pandemic, including skill regression, changing mood symptoms, loss of stability, and challenges transitioning to remote delivery of educational and therapy services. Outcomes also highlight protective factors that promoted well-being, adding to the current body of literature by revealing both challenges and benefits experienced by families of children with ASD. These varied experiences shed light on methods stakeholders may use to adapt programs and resources to better prepare for future emergencies or other disruptive events that result in uncertainty for individuals with ASD and their families.
Funding
Flinn Foundation, United States, Grant Number 2239.
CRediT authorship contribution statement
Jenna Stadheim: Formal analysis, Writing – original draft. Ashley Johns: Investigation, Writing – original draft. Melissa Mitchell: Investigation, Writing – review & editing. Christopher J. Smith: Conceptualization, Methodology, Writing – review & editing, Funding acquisition. B. Blair Braden: Conceptualization, Methodology, Writing – review & editing. Nicole L. Matthews: Conceptualization, Methodology, Formal analysis, Writing – original draft, Project administration, Funding acquisition.
Declarations of interest
None.
Acknowledgements
We would like to thank the families who participated in this research and the parents who participated in member checking. We would also like to thank the Southwest Autism Research & Resource Center staff and interns who assisted with data collection.
Footnotes
Quotes are reported exactly as written by participants except when deidentification was necessary.
Notably, seven of the nine families whose responses supported this category reported household incomes above the median household income for Arizona.
References
- Alhuzimi T. Stress and emotional wellbeing of parents due to change in routine for children with autism spectrum disorder (ASD) at home during COVID-19 pandemic in Saudi Arabia. Research in Developmental Disabilities. 2021;108 doi: 10.1016/j.ridd.2020.103822. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596. [DOI]
- Baghdadli A., Pry R., Michelon C., Rattaz C. Impact of autism in adolescents on parental quality of life. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2014;23(6):1859–1868. doi: 10.1007/s11136-014-0635-6. [DOI] [PubMed] [Google Scholar]
- Brookman-Frazee L., Baker-Ericzén M., Stahmer A., Mandell D., Haine R.A., Hough R.L. Involvement of youths with autism spectrum disorders or intellectual disabilities in multiple public service systems. Journal of Mental Health Research in Intellectual Disabilities. 2009;2(3):201–219. doi: 10.1080/19315860902741542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz, K. (2014). Constructing grounded theory (2nd ed.). Thousand Oaks, CA: Sage.
- Cheng S., Yang Y., Deng M. Psychological stress and perceived school success among parents of children with developmental disabilities during the COVID-19 pandemic. Journal of Autism and Developmental Disorders. 2021:1–8. doi: 10.1007/s10803-021-05209-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: An online parent survey. Brain Sciences. 2020;10(6):341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Division of Developmental Disabilities. (2020, April 8). Parents temporarily becoming direct care workers during the COVID-19 emergency. Arizona Department of Economic Security. Retrieved September 12, 2021, from 〈https://des.az.gov/sites/default/files/DCW_COVID19_English.pdf?time=1586389453810%27〉.
- Fifield, J. (2020, July 9). Is COVID-19 spreading more rapidly in Arizona than anywhere else in the world? Here's what data shows. AZ Central. Retrieved from 〈https://www.azcentral.com/story/news/local/arizona-health/2020/07/09/how-arizonas-covid-19-cases-compares-rest-world/5399832002/〉.
- Gabriels R.L., Cuccaro M.L., Hill D.E., Ivers B.J., Goldson E. Repetitive behaviors in autism: relationships with associated clinical features. Research in Developmental Disabilities. 2005;26(2):169–181. doi: 10.1016/j.ridd.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Harrison, P. L., & Oakland, T. (2015). ABAS-3: Adaptive behavior assessment system. Western.
- Jeste S., Hyde C., Distefano C., Halladay A., Ray S., Porath M.…Thurm A. Changes in access to educational and healthcare services for individuals with intellectual and developmental disabilities during COVID-19 restrictions. Journal of Intellectual Disability Research: JIDR. 2020 doi: 10.1111/jir.12776. [DOI] [PubMed] [Google Scholar]
- Kalb L.G., Badillo-Goicoechea E., Holingue C., Riehm K.E., Thrul J., Stuart E.A.…Fallin D. Psychological distress among caregivers raising a child with autism spectrum disorder during the COVID-19 pandemic. Autism Research. 2021 doi: 10.1002/aur.2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karpur A., Vasudevan V., Shih A., Frazier T. Brief report: Impact of COVID-19 in individuals with autism spectrum disorders: Analysis of a national private claims insurance database. Journal of Autism and Developmental Disorders. 2021 doi: 10.1007/s10803-021-05100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler F.W. Examining the services received by young children with autism and their families: A survey of parent responses. Focus on Autism and Other Developmental Disabilities. 1999;14(3):150–158. doi: 10.1177/108835769901400304. [DOI] [Google Scholar]
- Kumm A.J., Viljoen M., de Vries P.J. The digital divide in technologies for autism: Feasibility considerations for low- and middle-income countries. Journal of Autism and Developmental Disorders. 2021 doi: 10.1007/s10803-021-05084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laugeson E.A., Frankel F., Gantman A., Dillon A.R., Mogil C. Evidence-based social skills training for adolescents with autism spectrum disorders: The UCLA PEERS program. Journal of Autism and Developmental Disorders. 2012;42(6):1025–1036. doi: 10.1007/s10803-011-1339-1. [DOI] [PubMed] [Google Scholar]
- Liptak G.S., Stuart T., Auinger P. Health care utilization and expenditures for children with autism: Data from U.S. national samples. Journal of Autism and Developmental Disorders. 2006;36(7):871–879. doi: 10.1007/s10803-006-0119-9. [DOI] [PubMed] [Google Scholar]
- Manning J., Billian J., Matson J., Allen C., Soares N. Perceptions of families of individuals with autism spectrum disorder during the COVID-19 crisis. Journal of Autism and Developmental Disorders. 2021;51(8):2920–2928. doi: 10.1007/s10803-020-04760-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson M.L., Mahan S., Matson J.L. Parent training: A review of methods for children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2009;3(4):868–875. doi: 10.1016/j.rasd.2009.02.003. [DOI] [Google Scholar]
- Meral B.F. Parental views of families of children with autism spectrum disorder and developmental disorders during the COVID-19 pandemic. Journal of Autism and Developmental Disorders. 2021 doi: 10.1007/s10803-021-05070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutluer T., Doenyas C., Aslan Genc H. Behavioral implications of the Covid-19 process for autism spectrum disorder, and individuals’ comprehension of and reactions to the pandemic conditions. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.561882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Conference of State Legislatures. (2018, August 8). Autism and insurance coverage: State laws. 〈https://www.ncsl.org/research/health/autism-and-insurance-coverage-state-laws.aspx〉.
- Özgür B.G., Aksu H., Eser E. Factors affecting quality of life of caregivers of children diagnosed with autism spectrum disorder. Indian Journal of Psychiatry. 2018;60(3):278–285. doi: 10.4103/psychiatry.IndianJPsychiatry_300_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parenteau C.I., Bent S., Hossain B., Chen Y., Widjaja F., Beard M., Hendren R.L. COVID-19 related challenges and advice from parents of children with autism spectrum disorder. SciMedicine Journal. 2020;2:73–82. doi: 10.28991/SciMedJ-2020-02-SI-6. [DOI] [Google Scholar]
- Patterson S.Y., Smith V., Mirenda P. A systematic review of training programs for parents of children with autism spectrum disorders: Single subject contributions. Autism: The International Journal of Research and Practice. 2012;16(5):498–522. doi: 10.1177/1362361311413398. [DOI] [PubMed] [Google Scholar]
- Pickard K.E., Wainer A.L., Bailey K.M., Ingersoll B.R. A mixed-method evaluation of the feasibility and acceptability of a telehealth-based parent-mediated intervention for children with autism spectrum disorder. Autism: The International Journal of Research and Practice. 2016;20(7):845–855. doi: 10.1177/1362361315614496. [DOI] [PubMed] [Google Scholar]
- Siracusano M., Riccioni A., Gialloreti L., Segatori E., Arturi L., Vasta M.…Mazzone L. Parental stress and disability in offspring: A snapshot during the COVID-19 pandemic. Brain Sciences. 2021;11(8):1040. doi: 10.3390/brainsci11081040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPARK: Simons Foundation Powering Autism Research for Knowledge. (2020). Impact of COVID-19 on families and children with autism. SPARK for Autism. 〈https://d2dxtcm9g2oro2.cloudfront.net/wp-content/uploads/2020/04/03195500/spark-covid-survey-results.pdf〉.
- State of Arizona Executive Order 2020-40, § § A.R.S. 26–303 and 36–787 (2020). 〈https://azgovernor.gov/sites/default/files/eo_2020–40.pdf〉.
- Stough L.M., Ducy E.M., Kang D. Addressing the needs of children with disabilities experiencing disaster or terrorism. Current Psychiatry Reports. 2017;19(4):24. doi: 10.1007/s11920-017-0776-8. [DOI] [PubMed] [Google Scholar]
- Thomas K.C., Ellis A.R., McLaurin C., Daniels J., Morrissey J.P. Access to care for autism-related services. Journal of Autism and Developmental Disorders. 2007;37(10):1902–1912. doi: 10.1007/s10803-006-0323-7. [DOI] [PubMed] [Google Scholar]
- Türkoğlu S., Uçar H.N., Çetin F.H., Güler H.A., Tezcan M.E. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiology International. 2020;37(8):1207–1213. doi: 10.1080/07420528.2020.1792485. [DOI] [PubMed] [Google Scholar]