Abstract
Mucormycosis is a rare but life-threatening opportunistic fungal infection caused by a group of molds that belong to Zygomycetes of the order Mucorales. These fungi are found in the environment such as soil, decaying vegetation, and organic matters. Sporangiospores present in the environment enter the human body through inhalation or direct skin inoculation by trauma or ingestion and result in pulmonary, cutaneous, and gastrointestinal mucormycosis, respectively, in immunocompromised hosts. Patients with uncontrolled diabetes, hematological malignancies, high-dose glucocorticoid therapy, iron overload, and organ transplantation are at high risk of acquiring mucormycosis. The second wave of severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2] affected India severely with the highest number of cases and deaths compared to all other countries. Additionally, the country was affected by emergence of rare but life-threatening mucormycosis. Currently, many coronavirus disease 2019 patients with underlying risk factors such as uncontrolled diabetes, high-dose steroid therapy, and exposure to mechanical ventilation have developed mucormycosis. Inhalation is the most common mode of transmission that results in colonization of sporangiospores in the nose. In immunocompromised host, sporangiospores germinate, and subsequently form hyphae. These hyphae invade into tissues, and produce tissue infarction, necrosis, and thrombosis. Angioinvasion causes hematogenous dissemination to many organs, predominantly to brain, that result in rhino-orbital-cerebral mucormycosis. Clinical characteristics, radio imaging, fungal culture, histopathology, and molecular techniques are the key diagnostic methods. Surgical intervention and aggressive antifungal therapy are the main management strategies. Amphotericin B is the drug of choice for treatment of mucormycosis, whereas posaconazole or isavuconazole is used for step-down therapy and salvage therapy.
Key Words: Amphotericin B, coronavirus disease 2019, corticosteroids, fungal culture, ketoacidosis, mucormycetes
INTRODUCTION
Coronavirus disease 2019 (COVID-19), a major pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in large number of deaths worldwide.[1,2] Recent studies reported many fungal opportunistic infections such as mucormycosis, aspergillosis, and candidiasis in patients who had suffered COVID-19.[3,4,5] Mucormycosis is increasingly identified recently among post COVID-19 patients worldwide, with the greatest number arising from India.[3,4] Mucormycosis, colloquially referred to as “black fungus” due to its dark pigmentation, produces invasive, and potentially life-threatening infections with diverse clinical features, predominantly in immunocompromised individuals.[6,7] The first case of mucormycosis was described in 1876 by Furbinger in a German cancer patient who died of pulmonary hemorrhage. Fungal hyphae with sporangia were demonstrated in the lung biopsy of deceased individual, thus suggesting the diagnosis of mucormycosis.[8] Arnold Paltauf described the first case of disseminated mucormycosis in 1885 and he named it as “Mycosis Mucorina.”[8] Over time, more cases were identified globally, and the incidence has increased gradually, especially among immunocompromised patients. In recent times during COVID-19 pandemic, phenomenal rise in number of mucormycosis cases was noticed worldwide, predominantly in India.[8] This article briefly explains the etiological agent, pathophysiology, epidemiology, clinical features, laboratory diagnosis, and management of mucormycosis.
Mucormycosis is a serious but rare opportunistic fungal infection caused by a group of molds of genus Rhizopus, Mucor, Rhizomucor, Cunninghamella, and Lichtheimia (formerly Absidia) that belong to class Zygomycetes of the order Mucorales.[9] Rhizopus oryzae is the most common species that accounts for more than half of the mucormycosis in humans, and majority (90%) of the life-threatening angioinvasive rhino-orbital-cerebral mucormycosis (ROCM).[10] Table 1 represents the medically important Mucorales according to the updated taxonomy. The Mucorales are a harmless environmental mold commonly found in moist areas such as soil, damp walls of old buildings, ventilators, and humidifiers, decaying fruits and vegetables, and manure.[11] They grow rapidly and release a large number of sporangiospores that become airborne. Inhalation of sporangiospores present in the environment is the primary mode of transmission of mucormycosis. Cutaneous inoculation through trauma and oral ingestion are the other less commonly recognized modes of transmission.[4,12] They are generally harmless to immunocompetent individuals. However, in overt immunocompromised individuals such as patients with poorly controlled diabetes, diabetic ketoacidosis (DKA), stem cell or organ transplantation, hematological malignancies, persistent neutropenia, high-dose glucocorticoid therapy, and chelation therapy with deferoxamine, Mucorales can result in life-threatening necrotizing infections.[13] Mucormycosis affects multiple organs, and based on clinical presentation, it is categorized into pulmonary, cutaneous, rhino-cerebral, gastrointestinal, and disseminated forms.[14] However, ROCM and pulmonary mucormycosis are the most recognized clinical presentations globally. The area of involvement largely depends upon the underlying comorbid condition.[4] In patients with uncontrolled diabetes and DKA, ROCM is more frequently observed, whereas pulmonary mucormycosis is more often seen in patients suffering from prolonged neutropenia, hematological malignancies, and who had an organ transplantation. Gastrointestinal mucormycosis is more common among premature and low birth weight infants <1 month of age, and who had surgery or received medications including prolonged antibiotic therapy that lowers their immune status.[4] Extensive angioinvasion resulting in vessel thrombosis and subsequent ischemic tissue necrosis is the hallmark of mucormycosis.[15] Ischemic necrosis of the infected tissue further impairs host defenses by obstructing the flow of leukocytes and antifungal agents to the affected site.[16] Furthermore, angioinvasion contributes to dissemination of fungi to other target organs, especially to brain, but can also affect other organs such as heart, spleen, kidney, lungs, bones, joints, skin, and others.[16]
Table 1.
Medically important Mucorales as per the updated taxonomy
| Previous nomenclature | Current nomenclature |
|---|---|
| Rhizopus oryzae | Rhizopus arrhizus (incl. var. delemar) |
| Rhizopus microsporus var. azygosporus, var. chinensis, var. oligosporus, var. rhizopodiformis, var. tuberosus | Rhizopus microsporus |
| Mucor circinelloides f. griseocyanus | Mucor griseocyanus |
| Rhizomucor regularior, Rhizomucor variabilis var. regularior | Mucor circinelloides |
| Mucor circinelloides f. janssenii | Mucor janssenii |
| Mucor circinelloides f. lusitanicus | Mucor lusitanicus |
| Rhizomucor variabilis | Mucor irregularis |
| Mucor ellipsoideus, Mucor circinelloides f. circinelloides | Mucor ardhlaengiktus |
| Absidia corymbifera, Mycocladus corymbifer | Lichtheimia corymbifera |
| Absidia ramosa, Mycocladus ramosus | Lichtheimia ramosa |
| Absidia corymbifera, Mycocladus corymbifer | Lichtheimia corymbifera |
| Absidia ornata | Lichtheimia ornata |
During the ongoing COVID-19 pandemic, mucormycosis is increasingly detected among SARS-CoV-2 infected patients worldwide, but majority were reported from India.[4,17] This is due to the fact that India is a home of second largest population of diabetics, out of which 70% have poorly controlled diabetes.[18] Treatment regimen in COVID-19 patients consisting of steroids and antiviral drugs such as remdesivir which are known to cause immunosuppression coupled with uncontrolled diabetes resulting in DKA and mechanical ventilation is a perfect environment for mucormycosis to breakout in epidemic.[18] Corticosteroids are life-saving drugs used to reduce the dysregulated immune response (cytokine storm) in COVID-19 patients. However, they result in hyperglycemia and immunosuppression and thus favor the growth of Mucorales.[19] Moreover, increased iron over load, hyopxemia, and phagocytic dysfunction resulting from COVID-19 favors development of life threatning mucormycosis.[19,20]
PATHOPHYSIOLOGY OF MUCORMYCOSIS
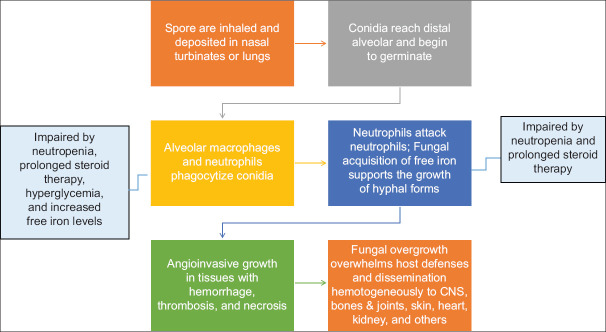
The primary mode of transmission is by inhalation of sporangiospores present in the environment.[21] Cutaneous mucormycosis, another form, is known to develop after the fungus gains entry through abraded skin such as cuts, burns, or trauma. In fact, cutaneous mucormycosis is common among immunocompetent individuals.[22] Inhalation results in deposition of sporangiospores in the nose. Sporangiospores then germinate and form fungal hyphae, invade into tissues, and produce tissue infarction, necrosis, and thrombosis.[23] Mucorales express CotH proteins on their spores and hyphae and bind specifically to glucose-regulated protein 78 (GRP-78) present on endothelial cells and subsequently facilitate angioinvasion. Additionally, elaboration of proteolytic enzymes and mycotoxins supplement fungal invasion.[24,25] Angioinvasion further leads to hematogenous dissemination predominantly to brain, but lungs, skin, bones, joints, heart, and kidney can also be affected.[26] Figure 1 illustrates steps in the pathogenesis of invasive mucormycosis.
Figure 1.
Pathophysiology of invasive mucormycosis
The experimental and clinical data reveal that the individuals who have phagocytic dysfunction or lack phagocytes are predisposed to mucormycosis.[17] For instance, patients with neutropenia are at higher risk of acquiring mucormycosis compared to patients suffering from acquired immunodeficiency syndrome. This would suggest that neutrophils are crucial for inhibition of proliferation of sporangiospores. Furthermore, phagocytes are involved in killing of Mucorales by generation of oxygen-free radicals and by release by cationic peptides such as defensins.[27] Toll-like receptors (TLRs) are well-recognized antigen receptors expressed on innate cells. A recent study revealed that exposure of neutrophils to R. oryzae promotes the upregulation of TLR-2 and robust production of pro-inflammatory cytokines.[28] It is observed that phagocytic dysfunction, impaired chemotaxis, and defective intracellular killing by both oxygen-dependent and oxygen-independent mechanisms are likely to happen in the presence of high glucose levels and acidic pH.[29] This suggests that poorly controlled diabetes with DKA is an important high-risk factor for the development of mucormycosis.
Mucormycosis is less likely to develop in immunocompetent individuals even after exposure to sporangiospores. In animal experiments, it was observed that inhalation of sporangiospores of Mucorales by immunocompetent animals failed to cause the disease.[17] In contrast, animals treated with high-dose corticosteroids or with DKA, developed severe disease with a progressive pulmonary and hematogenous dissemination of an infection.[30] Moreover, germination of inhaled sporangiospores and formation of hyphae are crucial for development of the disease.[17] Alveolar macrophages have the ability to engulf and prevent germination of sporangiospores of Mucorales.[31] In mouse experiments, it was observed that an immunosuppressed animal failed to prevent germination of sporangiospores after intranasal infection.[32] In line with this finding, studies have shown that malignancy, high-dose corticosteroid therapy, and other immunosuppressive conditions leading to neutropenia are the key risk factors for the development of severe mucormycosis in humans.[8,21,25,33] The exact mechanism by which diabetes mellitus, ketoacidosis, and corticosteroid therapy impair phagocytic function is yet to be determined. However, it is believed that Mucorales might have unique virulence factors that help to exploit the immunosuppressive status in this subset of patients.[17]
Another major virulence strategy adapted by Mucorales is their ability to acquire iron from the host. Iron is an essential element that contributes for several vital processes involved in the cell growth and development.[34] In mammalian hosts, iron is bound to many host carrier proteins such as ferritin, lactoferrin, and transferrin. This sequestration of iron is a key host defense mechanism as it not only deprives various pathogens, particularly Mucorales, from iron required for their metabolic activity but also protects the host cells from the toxic effect of free iron.[35,36] Therefore, factors that contribute to increase in the serum level of free iron is regarded as a high-risk factor for the development of mucormycosis.[36] Deferoxamine that chelates iron contributes an increase in serum iron level. The deferoxamine is a siderophore for Rhizopus species, enhances iron uptake by the fungus, and thus stimulates growth and tissue invasion by Mucorales.[37] Thus, clinical conditions associated with increased serum iron load such as DKA and patients suffering from hematological malignancies, who need repeated blood transfusion, are at higher risk acquiring mucormycosis infection.[38]
The prolonged use of certain antifungal agents such as voriconazole and echinocandins for antifungal prophylaxis or treatment, which are effective against Aspergillus but not against Mucorales, may result in increased survival of Mucorales, especially among profoundly immunosuppressed patients. Animal studies have demonstrated that prolonged use of these drugs may increase the virulence of certain Mucorales.[8,39] This has resulted in continued emergence of breakthrough invasive mucosal infections despite their susceptibility against newly introduced azoles such as posaconazole and isavuconazole.[8] A single-center study report from Austria revealed that 13% of haematopoietic stem cell transplantation (HSCT) patients receiving posaconazole prophylaxis developed breakthrough invasive fungal infections, out of which 55% resulted from Mucorales.[40] However, another review study reported that breakthrough invasive fungal infection varies depending on local epidemiology, patient characteristics, and the use of specific antifungal prophylaxis.[41]
Multiple reports of health-care-associated mucormycosis are also published. Nonsterile products such as bandages, adhesives, and nitroglycerin patches; various medical and surgical interventions such as ventilation, insertion of tubes, and surgeries; and hospital environment contaminated with mold such as water, air, and dust act as a source of infection. Hospital construction work and defective ventilation system may increase the risk of invasive fungal infection.[8]
EPIDEMIOLOGY
The global incidence of mucormycosis is increasing, however, the rise is highest in India, especially among the patients with poorly controlled diabetes.[38] The prevalence of mucormycosis rose from 0.7 cases per million in 1997 to 1.2 cases per million in 2006 as per the national population-based study conducted in France.[42] Similarly, a study from Belgium reported an increase in the prevalence from 0.019 cases/10,000 patient-days during 2000 to 0.148 cases/10,000 patient-days during 2009.[43] The recent estimate in the year 2019−2020 revealed that the global prevalence of mucormycosis varied from 0.005 to 1.7 per million population, whereas its prevalence in India was approximately 80 times higher (0.14 per 1000) compared to developed countries.[8,38]
Generally, diabetes mellitus has been cited as the leading risk factor for mucormycosis globally including in India. However, hematological malignancies and organ transplant were the most recognized risk factors for mucormycosis in the USA and Europe.[4] Table 2 summarizes the global reports of risk factors for mucormycosis. Prolonged use of glucocorticoids is often associated with development of several opportunistic infections such as mucormycosis and aspergillosis. Even short-course steroid therapy has been linked to development of mucormycosis, particularly in patients with diabetes mellitus.[4] Hoang et al. documented the development of mucormycosis in diabetic patients who were treated with short-course steroid therapy for 5−7 days.[21]
Table 2.
Summary of global studies regarding associated common risk factors for mucormycosis
| Characteristics of Studies | Risk Factors/Underlying Diseases (%) | References | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||
| Countries of Origin of Cases | Prospective Study | Multicenter Study | Time Period | Total no. of pts | DM | HM | HSCT | SOT | CORT /AI | Trauma/ Surgery | HIV | None | |
| France | No | Yes | 2005–2007 | 101 | 23 | 50 | 12 | 44230 | 13 | 18 | 1 | 1 | Lanternier et al. 2012[42] |
| Mexico | No | Yes | 1982–2016 | 418 | 72 | 17 | 0 | 1/ | 1 | 2.3 | 0.7 | 4 | Corzo-Leon et al. 2017[49] |
| Global | No | Yes | 1940–2003 | 929 | 36 | 15.8 | 5 | 7 | 1 | 8 | 2 | 19 | Roden et al. 2005[70] |
| Global | No | Yes | 2000–2017 | 851 | 40 | 32 | 0 | 44210 | 12114 | 20 | 0 | 18 | Jeong et al. 2019[71] |
| Italy | Yes | Yes | 2004–2007 | 60 | 18 | 62 | 3 | 8/ | 18323 | 2 | 17 | 3 | Pagano et al. 2009[72] |
| USA | No | Yes | 2005–2014 | 555 | 52 | 40 | 11 | 44362 | NA | 4 | 2 | NA | Kontoyiannis et al. 2016[73] |
| South America | No | Yes | 1960–2018 | 143 | 42 | 11 | 2 | /13 | NA | 20 | 2 | 7.7 | Nucci et al. 2019[74] |
| Europe | Yes | Yes | 2005–2007 | 230 | 17 | 44 | 0 | 44320 | 44 | 17 | 2 | 8 | Skiada et al. 2011[75] |
| India | Yes | Yes | 2016–2017 | 465 | 74 | 8 | 1 | 1.5/6.5 | /3.7 | 6.9 | - | 11.8 | Patel et al. 2020[76] |
| Iran | No | Yes | 2008–2014 | 208 | 75 | 3 | 2 | 44258 | NA | 4 | - | 2 | Dolatabadi et al. 2018[77] |
| Iran | No | Yes | 1990–2015 | 98 | 48 | 6 | 1 | /23 | NA | 1 | - | 10 | Vaezi et al. 2016[78] |
| Lebanon | No | No | 2008–2018 | 20 | 35 | 65 | 0 | 5 | 70 | - | - | - | El Zein et al. 2018[79] |
| Australia | No | Yes | 2004–2012 | 74 | 27 | 48.6 | 18 | 44266 | 19694 | 23 | 0 | 11 | Kennedy et al. 2016[80] |
| Middle East and North Africa | No | Yes | 1968–2019 | 310 | 49.7 | 16.5 | 0 | 17 | 21.6 | 12 | 0.3 | 5.8 | Stemler et al. 2020[81] |
DM: Diabetes mellitus, HM: Hematological malignancy, HSCT: Hematopoietic stem cell transplantation, SOT: Solid organ transplantation, CORT/AI: Corticosteroids/ Autoimmunity, HIV: Human immunodeficiency virus
The second wave of SARS-CoV-2 infection affected India substantially with the highest number of cases and deaths compared to all other countries. Another imminent threat that greatly affected India is emergence of a rare but life-threatening fungal function, namely mucormycosis, often referred as “black fungus” in patients infected with COVID-19. The published literature from December 2019 till the beginning of April 2021, indicate that the India was worst affected country, accounting for 70% of the global mucormycosis cases in COVID-19 patients during this period.[4,44] As of May 28, 2021, around 15,000 cases of mucormycosis with the highest number from Gujarat (approximately 3750 cases) have been documented. The steep increase in number of cases and deaths due to mucormycosis in COVID-19 patients was also noticed in other states, namely Maharashtra, Rajasthan, Andhra Pradesh, Karnataka, Haryana, Madhya Pradesh, Uttarakhand, and Delhi. Multiple states have already declared it as an epidemic and a notifiable disease to the national health authorities.[45,46] The poorly controlled diabetes, increased use of corticosteroids for immunosuppression, and long-term stays in the intensive care unit are attributed to steep rise of mucormycosis in COVID-19 patients. Furthermore, increased use of corticosteroids results in severe hyperglycemia, thus predisposing COVID-19 patients, especially those suffering from diabetes.[47] The sudden rise in these unusual infections carries an immense public health importance as they are associated with high mortality rate. Rhino-orbital-cerebral mucormycosis is the most common as well as the most lethal form associated with high mortility as high as 90%.[47] Moreover, its ability of angioinvasion and rapid dissemination, especially to brain, and even delay of 12−24 h in the diagnosis and management could be highly fatal.[4]
DIAGNOSIS
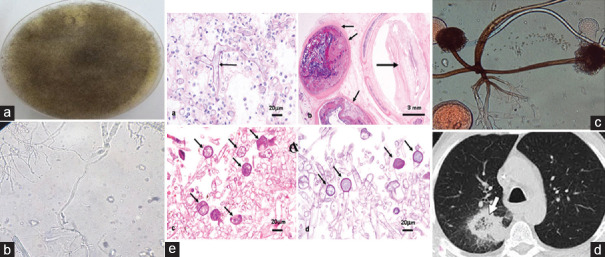
Early diagnosis and early initiation of aggressive treatment are key to the better outcome in mucormycosis. However, despite these efforts, the mortality of the disease remains to be high.[8] Diagnosis is comprised of evaluation of clinical manifestations, assessment of risk factors, early use of radio imaging techniques, and laboratory investigations such as fungal culture, histopathology, and molecular assays.[8,48] Figure 2 illustrates the key diagnostic characteristics of Rhizopus species.
Figure 2.
Common diagnostic features of Rhizopus species (a) Growth of Rhizopus spp. on Saboraud's dextrose agar (SDA) medium, (b) Potassium hydroxide (KOH) wet mount demonstrating fungal hyphae and spores, (c) Microscopy of LPCB stained preparation demonstrating morphology of Rhizopus spp. (non-septate hyphae, sporangiophore, sporangium and spores), (d) Chest computerized tomography (CT) scan demonstrating cavitary lesion, (e) Histopatholgy examination of the tissue specimen
CLINICAL DIAGNOSIS
The successful management lies in early diagnosis. However, early diagnosis is quite challenging due to subtle clinical features. Headache, nasal congestion, black nasal crusts, facial pain, periorbital swelling, proptosis, palatine ulcer, pain in the eyes/diplopia or blurring of vision are important early signs of ROCM, whereas fever, cough, and shortness of breath are commonly noticed features in pulmonary mucormycosis. These features developing in a patient with an underlying immunosuppressive conditions such uncontrolled diabetes, corticosteroid therapy, and others should give suspicion of mucormycosis.[18,49] However, detection of mucormycosis in few COVID-19 patients who had no history of underlying immunosuppression, makes it more confusing in early diagnosis.[18] The presence of any of these findings warrants prompt use of radio imaging immediately. Subsequently, it requires collection of samples for culture, histopathology, and molecular analysis.[8,49] Similarly, a neutropenic patient presenting with fever, pleuritic chest pain, nonproductive cough, and not responding to the broad-spectrum antibiotics would give suspicion of pulmonary mucormycosis. However, it is generally indistinguishable from pulmonary aspergillosis, fusariosis, and tuberculosis in countries where prevalence of TB is high.[8,50] The presence of multiple nodules and signs of pleural effusion in radiological imaging, and the presence of reverse halo sign on computed tomography (CT scan), would strongly indicate pulmonary mucormycosis.[8,51] The positron emission tomography-CT with 18F-fluorodeoxyglucose is another newer technique which aids in the diagnosis and management of mucormycosis.[52] These tests are not conclusive evidence but suggest the quick performance of laboratory tests to confirm the diagnosis.[8]
LABORATORY INVESTIGATIONS
Direct smear examination, fungal culture, and histopathology of biopsied specimen are the cornerstones for the diagnosis of mucormycosis. Microscopy of the clinical specimens stained with Calcofluor white or potassium hydroxide and demonstration of nonseptate hyphae allows rapid presumptive diagnosis of mucormycosis.[53] Tissue sections are better stained with hematoxylin and eosin/Grocott-Gomori methenamine silver/periodic acid−Schiff stains.[54] Histopathology of tissue specimens in invasive disease demonstrates prominent infarcts and angioinvasion. Furthermore, the demonstration of fungal hyphae in biopsy specimen plays a crucial role in distinguishing fungus as a pathogen in the specimen from a culture contaminant.[8]
Fungal culture is indispensable for the diagnosis of mucormycosis. It permits identification of the causative agent to the species level.[8] Most Mucorales are nonfastidious and capable of growing at 37°C on Sabouraud's dextrose agar or any other routine fungal culture media. The colonies usually appear within 24−48 hours, and the growth is identified by colony morphology and characteristic microscopic appearance. A positive growth from sterile site confirms the diagnosis. However, positive growth from nonsterile site should always be distinguished from possible contamination by combining with clinical, radiological, and histopathological examinations.[8]
Fungal culture has a low sensitivity, and nearly 50% may yield false-negative results in mucormycosis patients.[55] The possible reasons attributed to this are improper sampling and handling of the specimen before examination, distortion of fungal elements while grinding or homogenization of tissue specimens for culture, requirement of special culture conditions for certain species, recent or ongoing antifungal therapy, and lack of expertise. Therefore, addressing all these issues is essential to reduce false-negative results.[8] Fungal culture is useful in distinguishing Mucorales from other opportunistic fungi. However, they lack the accuracy in distinguishing between the different species of Mucorales.[56] Currently available molecular techniques have several advantages over conventional diagnostic methods. Serum quantitative polymerase chain reaction is rapid (turnaround time is about 3 hours), highly reliable for the diagnosis of angioinvasive disease, highly specific, able to identify species accurately, and the rapid diagnosis in immunocompromised patients, much earlier than the conventional methods.[57] Therefore, they are appropriate for screening and monitoring of high-risk patients and thus would benefit in terms of increasing survival chance of the patients.[8,58]
MANAGEMENT
Mucormycosis is a rare but devastating condition, and delay in management may result in poor outcome. The management of mucormycosis involves prompt diagnosis and multidisciplinary approach: surgical debridement of affected tissues, early initiation of antifungal therapy, and prompt use of adjunctive therapy.[59] Additionally, the elimination of underlying risk factors that predispose for infection, namely hyperglycemia, metabolic acidosis, neutropenia, immunosuppressive therapy, and iron overload, is also crucial.[60] A study by Chamilos et al. revealed delay in initiation of amphotericin B for 6 or more days after the diagnosis resulted in twofold increase in mortality at 12 weeks after diagnosis.[61] The intravenous administration of liposomal amphotericin B is the choice of initial therapy.[62] Patients who have responded well to amphotericin B were treated with either posaconazole or isavuconazole as step-down therapy. These azoles are useful even for salvage therapy in patients who do not respond to initial amphotericin B therapy.[63] However, the use of these drugs either intravenous or oral depends on severity of the patients’ illness and the gastrointestinal tract functional status.[64] Furthermore, since the disease is scarce, there is not enough evidence to suggest whether combination of antifungal therapy is more beneficial compared to monotherapy.[8]
Surgical debridement of involved tissues is highly warranted as soon as any form of mucormycosis is diagnosed.[65] Literature studies reveal immediate surgical removal of necrotic tissue, and early initiation of antifungal therapy has been associated with better outcome in terms of survival of the patients.[66] In the case of ROCM, extensive debridement involving removal of palate, nasal cartilage, and the orbit may often lead to disfigurement.[66] However, recent advances in surgical approach through endoscopic surgery accomplish limited tissue removal.[67] There were several reports revealing cure of pulmonary mucormycosis with lobectomy.[68,69] In some patients with extensive involvement or thrombocytopenia where surgery is precluded, it is advised for every effort to optimize medical conditions, antifungal therapy, and reverse immunosuppression.[8]
CONCLUSION
Surge in mucormycosis cases worldwide, particularly in India among COVID-19 patients, is a serious concern not only in terms of mortality but also other impacts that result from the disease such as financial burden, mental strain, and fate of the other family members. Widespread use of corticosteroids and prolonged length of hospital stay as part of the armamentarium against COVID-19 are the most recognized contributing factors that more likely predispose high-risk individuals such as diabetes mellitus, hematological malignancies, organ transplantation, and others to these life-threatening invasive fungal infections. Therefore, physicians must be aware of early signs and symptoms of these secondary invasive fungal infections in COVID-19 patients, especially with preexisting risk factors, and should consider early prompt diagnosis and quick initiation of aggressive antifungal therapy and surgery. Prevention is better than cure. Therefore, reevaluation of prevention strategies such as control of diabetes and usage of steroids in terms of dose and duration, apart from public awareness regarding self-hygiene, is critical to reduce the burden of mucormycosis in patients who are already greatly affected by COVID-19.
Research quality and ethics statement
This report was exempt from the requirement of approval the Institutional Review Board / Ethics Committee. No specific EQUATOR Network (http://www.equator-network.org/) guideline is available for narrative reviews.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sannathimmappa MB, Nambiar V, Patil R. Emerging and re-emerging viral infections in the 21 century: Microbiological and public health perspectives. J Krishna Inst Med Sci Univ. 2021;10:1–20. [Google Scholar]
- 2.Mohan BS, Nambiar V. COVID-19: An Insight into SARS-CoV-2 Pandemic Originated at Wuhan City in Hubei Province of China. J Infect Dis Epidemiol. 2020;6:146. doi.org/10.23937/2474-3658/1510146. [Google Scholar]
- 3.Kubin CJ, McConville TH, Dietz D, Zucker J, May M, Nelson B, et al. Characterization of bacterial and fungal infections in hospitalized patients with COVID-19 and factors associated with healthcare-associated infections. Open Forum Infect Dis. 2021;8:ofab201. doi: 10.1093/ofid/ofab201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15:102146. doi: 10.1016/j.dsx.2021.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta S, Pandey A. Rhino-orbital mucormycosis associated with COVID-19. Cureus. 2020;12:e10726. doi: 10.7759/cureus.10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choudhary NK, Jain AK, Soni R, Gahlot N. Mucormycosis: A deadly black fungus infection among COVID-19 patients in India. Clin Epidemiol Glob Health. 2021;12:100900. doi: 10.1016/j.cegh.2021.100900. doi: 10.1016/j.cegh.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kumar M, Sarma DK, Shubham S, Kumawat M, Verma V, Singh B, et al. Mucormycosis in COVID-19 pandemic: Risk factors and linkages. Curr Res Microb Sci. 2021;2:100057. doi: 10.1016/j.crmicr.2021.100057. doi: 10.1016/j.crmicr.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skiada A, Pavleas I, Drogari-Apiranthitou M. Epidemiology and diagnosis of mucormycosis: An update. J Fungi (Basel) 2020;6:E265. doi: 10.3390/jof6040265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walther G, Wagner L, Kurzai O. Updates on the taxonomy of mucorales with an emphasis on clinically important taxa. J Fungi (Basel) 2019;5:E106. doi: 10.3390/jof5040106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spellberg B, Edwards J, Jr, Ibrahim A. Novel perspectives on mucormycosis: Pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18:556–69. doi: 10.1128/CMR.18.3.556-569.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haleem Khan AA, Mohan Karuppayil S. Fungal pollution of indoor environments and its management. Saudi J Biol Sci. 2012;19:405–26. doi: 10.1016/j.sjbs.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13:236–301. doi: 10.1128/cmr.13.2.236-301.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas L, Tay SY, Howard D, Falhammar H. Mucormycosis in a 40-year-old woman with diabetic ketoacidosis. CMAJ. 2020;192:E431–3. doi: 10.1503/cmaj.191364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CastrejɃn-Pȳrez AD, Welsh EC, Miranda I, Ocampo-Candiani J, Welsh O. Cutaneous mucormycosis. An Bras Dermatol. 2017;92:304–11. doi: 10.1590/abd1806-4841.20176614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yinadsawaphan T, Ngamskulrungroj P, Chalermwai W, Dhitinanmuang W, Angkasekwinai N. Gastrointestinal mucormycosis due to Rhizopus microsporus following Streptococcus pyogenes toxic shock syndrome in an HIV patient: A case report. BMC Infect Dis. 2020;20:817. doi: 10.1186/s12879-020-05548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibrahim AS, Spellberg B, Walsh TJ, Kontoyiannis DP. Pathogenesis of mucormycosis. Clin Infect Dis. 2012;54(Suppl 1):S16–22. doi: 10.1093/cid/cir865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Revannavar SM, Supiya PS, Samaga L, Vineeth VK. COVID-19 triggering mucormycosis in a susceptible patient: A new phenomenon in the developing world? BMJ Case Rep. 2021;14:e241663. doi: 10.1136/bcr-2021-241663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suvvari TK, Arigapudi N, Kandi VR, Kutikuppala LS. Mucormycosis: A killer in the shadow of COVID-19. J Mycol Med. 2021;31:101161. doi: 10.1016/j.mycmed.2021.101161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rudramurthy SM, Hoenigl M, Meis JF, Cornely OA, Muthu V, Gangneux JP, et al. ECMM and ISHAM. ECMM/ISHAM recommendations for clinical management of COVID-19 associated mucormycosis in lowand middle-income countries. Mycoses. 2021;64:1028–1037. doi: 10.1111/myc.13335. doi: 10.1111/myc.13335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cavezzi A, Troiani E, Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin Pract. 2020;10:1271. doi: 10.4081/cp.2020.1271. doi:10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoang K, Abdo T, Reinersman JM, Lu R, Higuita NI. A case of invasive pulmonary mucormycosis resulting from short courses of corticosteroids in a well-controlled diabetic patient. Med Mycol Case Rep. 2020;29:22–4. doi: 10.1016/j.mmcr.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bhat I, Beg MA, Athar F. A contemporary intimidation for COVID-19 patients coinfected with mucormycosis in India. J Bacteriol Mycol Open Access. 2021;9:69–71. [Google Scholar]
- 23.Muszewska A, Paw̢owska J, Krzy͇ciak P. Biology, systematics, and clinical manifestations of Zygomycota infections. Eur J Clin Microbiol Infect Dis. 2014;33:1273–87. doi: 10.1007/s10096-014-2076-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Challa S. Mucormycosis: Pathogenesis and pathology. Curr Fungal Infect Rep. 2019;13:11–20. doi: 10.1007/s12281-022-00443-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shumilov E, Bacher U, Perske C, Mohr A, Eiffert H, Hasenkamp J, et al. In Situ Validation of the endothelial cell receptor GRP78 in a case of rhinocerebral mucormycosis. Antimicrob Agents Chemother. 2018;62:e00172–18. doi: 10.1128/AAC.00172-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.King J, Pana ZD, Lehrnbecher T, Steinbach WT, Warris A. Recognition and clinical presentation of invasive fungal disease in neonates and children. J Pediatr Infect Dis Soc. 2017;6:S12–21. doi: 10.1093/jpids/pix053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghuman H, Voelz K. Innate and adaptive immunity to mucorales. J Fungi (Basel) 2017;3:E48. doi: 10.3390/jof3030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chamilos G, Lewis RE, Lamaris G, Walsh TJ, Kontoyiannis DP. Zygomycetes hyphae trigger an early, robust proinflammatory response in human polymorphonuclear neutrophils through toll-like receptor 2 induction but display relative resistance to oxidative damage. Antimicrob Agents Chemother. 2008;52:722–4. doi: 10.1128/AAC.01136-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alba-Loureiro TC, Munhoz CD, Martins JO, Cerchiaro GA, Scavone C, Curi R, et al. Neutrophil function and metabolism in individuals with diabetes mellitus. Braz J Med Biol Res. 2007;40:1037–44. doi: 10.1590/s0100-879x2006005000143. [DOI] [PubMed] [Google Scholar]
- 30.Chikley A, Ben-Ami R, Kontoyiannis DP. Mucormycosis of the central nervous system. J Fungi (Basel) 2019;5:E59. doi: 10.3390/jof5030059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicolȥs FE, Murcia L, Navarro E, Navarro-Mendoza MI, Pȳrez-Arques C, Garre V. Mucorales species and macrophages. J Fungi (Basel) 2020;6:E94. doi: 10.3390/jof6020094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobsen ID. Animal models to study mucormycosis. J Fungi (Basel) 2019;5:E27. doi: 10.3390/jof5020027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morales-Franco B, Nava-Villalba M, Medina-Guerrero EO, Sȥnchez-NuɁo YA, Davila-Villa P, Anaya-Ambriz EJ, et al. Host-Pathogen Molecular Factors Contribute to the Pathogenesis of Rhizopus spp. in Diabetes Mellitus. Curr Trop Med Rep. 2021:1–12. doi: 10.1007/s40475-020-00222-1. doi: 10.1007/s40475-020-00222-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stanford FA, Voigt K. Iron assimilation during emerging infections caused by opportunistic fungi with emphasis on mucorales and the development of antifungal resistance. Genes (Basel) 2020;11:E1296. doi: 10.3390/genes11111296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nairz M, Weiss G. Iron in infection and immunity. Mol Aspects Med. 2020;75:100864. doi: 10.1016/j.mam.2020.100864. [DOI] [PubMed] [Google Scholar]
- 36.Ibrahim A, Spellberg B, Edwards J. Iron acquisition: A novel prospective on mucormycosis pathogenesis and treatment. Curr Opin Infect Dis. 2009;21:620–5. doi: 10.1097/QCO.0b013e3283165fd1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Larcher G, Dias M, Razafimandimby B, Bomal D, Bouchara JP. Siderophore production by pathogenic mucorales and uptake of deferoxamine B. Mycopathologia. 2013;176:319–28. doi: 10.1007/s11046-013-9693-5. [DOI] [PubMed] [Google Scholar]
- 38.Prakash H, Chakrabarti A. Global epidemiology of mucormycosis. J Fungi (Basel) 2019;5:E26. doi: 10.3390/jof5010026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lamaris GA, Ben-Ami R, Lewis RE, Chamilos G, Samonis G, Kontoyiannis DP. Increased virulence of zygomycetes organisms following exposure to voriconazole: A study involving fly and murine models of zygomycosis. J Infect Dis. 2009;199:1399–406. doi: 10.1086/597615. [DOI] [PubMed] [Google Scholar]
- 40.Auberger J, Lass-FlɆrl C, Aigner M, Clausen J, Gastl G, Nachbaur D. Invasive fungal breakthrough infections, fungal colonization and emergence of resistant strains in high-risk patients receiving antifungal prophylaxis with posaconazole: Real-life data from a single-centre institutional retrospective observational study. J Antimicrob Chemother. 2012;67:2268–73. doi: 10.1093/jac/dks189. [DOI] [PubMed] [Google Scholar]
- 41.Lionakis MS, Lewis RE, Kontoyiannis DP. Breakthrough invasive mold infections in the hematology patient: Current concepts and future directions. Clin Infect Dis. 2018;67:1621–30. doi: 10.1093/cid/ciy473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanternier F, Dannaoui E, Morizot G, Elie C, Garcia-Hermoso D, Huerre M, et al. A global analysis of mucormycosis in France: The RetroZygo study (2005−2007) Clin Infect Dis. 2012;54:S35–43. doi: 10.1093/cid/cir880. [DOI] [PubMed] [Google Scholar]
- 43.Saegeman V, Maertens J, Meersseman W, Spriet I, Verbeken E, Lagrou K. Increasing incidence of mucormycosis in University Hospital, Belgium. Emerg Infect Dis. 2010;16:1456–8. doi: 10.3201/eid1609.100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.John TM, Jacob CN, Kontoyiannis DP. When uncontrolled diabetes mellitus and severe COVID-19 converge: The perfect storm for mucormycosis. J Fungi (Basel) 2021;7:298. doi: 10.3390/jof7040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raut A, Huy NT. Rising incidence of mucormycosis in patients with COVID-19: Another challenge for India amidst the second wave? Lancet Respir Med. 2021;9:e77. doi: 10.1016/S2213-2600(21)00265-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Black Fungus: Here is a List of States with Highest Number of Mucormycosis Cases. Hindustan Times. 2021. [Last accessed on 2021 May 28]. Available from: https://www.hindustantimes.com/india-news/black-fungus-states-with-highestnumber-of-mucormycosis-cases-101621559394002.html .
- 47.Deutsch PG, Whittaker J, Prasad S. Invasive and non-invasive fungal rhinosinusitis − A review and update of the evidence. Medicina (Kaunas) 2019;55:E319. doi: 10.3390/medicina55070319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sarkar S, Gokhale T, Choudhury SS, Deb AK. COVID-19 and orbital mucormycosis. Indian J Ophthalmol. 2021;69:1002–4. doi: 10.4103/ijo.IJO_3763_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Corzo-LeɃn DE, Chora-Hernȥndez LD, Rodrȷguez-Zulueta AP, Walsh TJ. Diabetes mellitus as the major risk factor for mucormycosis in Mexico: Epidemiology, diagnosis, and outcomes of reported cases. Med Mycol. 2018;56:29–43. doi: 10.1093/mmy/myx017. [DOI] [PubMed] [Google Scholar]
- 50.Aggarwal D, Chander J, Janmeja AK, Katyal R. Pulmonary tuberculosis and mucormycosis co-infection in a diabetic patient. Lung India. 2015;32:53–5. doi: 10.4103/0970-2113.148452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Legouge C, Caillot D, Chrȳtien ML, Lafon I, Ferrant E, Audia S, et al. The reversed halo sign: pathognomonic pattern of pulmonary mucormycosis in leukemic patients with neutropenia? Clin Infect Dis. 2014;58:672–8. doi: 10.1093/cid/cit929. [DOI] [PubMed] [Google Scholar]
- 52.Liu Y, Wu H, Huang F, Fan Z, Xu B. Utility of 18F-FDG PET/CT in diagnosis and management of mucormycosis. Clin Nucl Med. 2013;38:e370–1. doi: 10.1097/RLU.0b013e3182867d13. [DOI] [PubMed] [Google Scholar]
- 53.Lass-FlɆrl C, Aigner M, Nachbaur D, Eschertzhuber S, Bucher B, Geltner C, et al. Diagnosing filamentous fungal infections in immunocompromised patients applying computed tomography-guided percutaneous lung biopsies: A 12-year experience. Infection. 2017;45:867–75. doi: 10.1007/s15010-017-1072-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lass-FlɆrl C. Zygomycosis: Conventional laboratory diagnosis. Clin Microbiol Infect. 2009;15(Suppl 5):60–5. doi: 10.1111/j.1469-0691.2009.02999.x. [DOI] [PubMed] [Google Scholar]
- 55.Walsh TJ, Gamaletsou MN, McGinnis MR, Hayden RT, Kontoyiannis DP. Early clinical and laboratory diagnosis of invasive pulmonary, extrapulmonary, and disseminated mucormycosis (zygomycosis) Clin Infect Dis. 2012;54(Suppl 1):S55–60. doi: 10.1093/cid/cir868. [DOI] [PubMed] [Google Scholar]
- 56.Yang M, Lee JH, Kim YK, Ki CS, Huh HJ, Lee NY. Identification of mucorales from clinical specimens: A 4-year experience in a single institution. Ann Lab Med. 2016;36:60–3. doi: 10.3343/alm.2016.36.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kidd SE, Chen SC, Meyer W, Halliday CL. A new age in molecular diagnostics for invasive fungal disease: Are we ready? Front Microbiol. 2019;10:2903. doi: 10.3389/fmicb.2019.02903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Millon L, Herbrecht R, Grenouillet F, Morio F, Alanio A, Letscher-Bru V, et al. Early diagnosis and monitoring of mucormycosis by detection of circulating DNA in serum: Retrospective analysis of 44 cases collected through the French Surveillance Network of Invasive Fungal Infections (RESSIF) Clin Microbiol Infect. 2016;22:810.e1-8. doi: 10.1016/j.cmi.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 59.Mrittika S, Sumeet L, Tatyarao LP, Ragini P, Santosh HG. Mucor in a viral land. Indian J Ophthalmol. 2021;69:244–52. doi: 10.4103/ijo.IJO_3774_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tissot F, Agrawal S, Pagano L, Petrikkos G, Groll AH, Skiada A, et al. ECIL-6 guidelines for the treatment of invasive candidiasis, aspergillosis and mucormycosis in leukemia and hematopoietic stem cell transplant patients. Haematologica. 2017;102:433–44. doi: 10.3324/haematol.2016.152900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chamilos G, Lewis RE, Kontoyiannis DP. Delaying amphotericin B-based frontline therapy significantly increases mortality among patients with hematologic malignancy who have zygomycosis. Clin Infect Dis. 2008;47:503–9. doi: 10.1086/590004. [DOI] [PubMed] [Google Scholar]
- 62.Cavassin FB, Baɐ-Carneiro JL, Vilas-Boas RR, Queiroz-Telles F. Sixty years of Amphotericin B: An overview of the main antifungal agent used to treat invasive fungal infections. Infect Dis Ther. 2021;10:115–47. doi: 10.1007/s40121-020-00382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jenks JD, Salzer HJ, Prattes J, Krause R, Buchheidt D, Hoenigl M. Spotlight on isavuconazole in the treatment of invasive aspergillosis and mucormycosis: Design, development, and place in therapy. Drug Des Devel Ther. 2018;12:1033–44. doi: 10.2147/DDDT.S145545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ruland MO, Egelund TA, Ng JS, Bradfield SM, Egelund EF. Intravenous and oral posaconazole pharmacokinetics in a five-year-old with mucor: A case report and review of the literature. J Pediatr Pharmacol Ther. 2019;24:528–33. doi: 10.5863/1551-6776-24.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hernȥndez JL, Buckley CJ. Treasure Island (FL): StatPearls Publishing; 2021. [Last updated on 2020 Jun 26]. StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544364/ [Google Scholar]
- 66.Bhandari J, Thada PK, Nagalli S. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. [Last accessed on 2021 May 22; Last updated on 2021 Apr 07]]. Rhinocerebral mucormycosis. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559288/ [PubMed] [Google Scholar]
- 67.Shaikh S, Deopujari C. The endoscope and instruments for minimally invasive neurosurgery. Mini Invasive Surg. 2020;4:89. [Google Scholar]
- 68.Luo Z, Zhang L. Diagnosis and treatment of pulmonary mucormycosis: A case report. Exp Ther Med. 2017;14:3788–91. doi: 10.3892/etm.2017.4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Seifert S, Wiley J, Kirkham J, Lena S, Schiers K. Pulmonary mucormycosis with extensive bronchial necrosis and bronchomediastinal fistula: A case report and review. Respir Med Case Rep. 2020;30:101082. doi: 10.1016/j.rmcr.2020.101082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634–53. doi: 10.1086/432579. [DOI] [PubMed] [Google Scholar]
- 71.Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DC, et al. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26–34. doi: 10.1016/j.cmi.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 72.Pagano L, Valentini CG, Posteraro B, Girmenia C, Ossi C, Pan A, et al. Zygomycosis in Italy: A survey of FIMUA-ECMM (Federazione Italiana di Micopatologia Umana ed Animale and European Confederation of Medical Mycology) J Chemother. 2009;21:322–9. doi: 10.1179/joc.2009.21.3.322. [DOI] [PubMed] [Google Scholar]
- 73.Kontoyiannis DP, Yang H, Song J, Kelkar SS, Yang X, Azie N, et al. Prevalence, clinical and economic burden of mucormycosis-related hospitalizations in the United States: A retrospective study. BMC Infect Dis. 2016;16:1–6. doi: 10.1186/s12879-016-2023-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nucci M, Engelhardt M, Hamed K. Mucormycosis in South America: A review of 143 reported cases. Mycoses. 2019;62:730–8. doi: 10.1111/myc.12958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Skiada A, Pagano L, Groll A, Zimmerli S, Dupont B, Lagrou K, et al. Zygomycosis in Europe: Analysis of 230 cases accrued by the registry of the European Confederation of Medical Mycology (ECMM) Working Group on Zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011;17:1859–67. doi: 10.1111/j.1469-0691.2010.03456.x. [DOI] [PubMed] [Google Scholar]
- 76.Patel A, Kaur H, Xess I, Michael JS, Savio J, Rudramurthy S, et al. A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect. 2020;26:944–e9-15. doi: 10.1016/j.cmi.2019.11.021. [DOI] [PubMed] [Google Scholar]
- 77.Dolatabadi S, Ahmadi B, Rezaei-Matehkolaei A, Zarrinfar H, Skiada A, Mirhendi H, et al. Mucormycosis in Iran: A six-year retrospective experience. J Mycol Med. 2018;28:269–73. doi: 10.1016/j.mycmed.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 78.Vaezi A, Moazeni M, Rahimi MT, de Hoog S, Badali H. Mucormycosis in Iran: A systematic review. Mycoses. 2016;59:402–15. doi: 10.1111/myc.12474. [DOI] [PubMed] [Google Scholar]
- 79.El-Zein S, El-Sheikh J, El-Zakhem A, Ibrahim D, Bazarbachi A, Kanj SS. Mucormycosis in hospitalized patients at a tertiary care center in Lebanon: A case series. Infection. 2018;46:811–21. doi: 10.1007/s15010-018-1195-4. [DOI] [PubMed] [Google Scholar]
- 80.Kennedy KJ, Daveson K, Slavin MA, van Hal SJ, Sorrell TC, Lee A, et al. Mucormycosis in Australia: Contemporary epidemiology and outcomes. Clin Microbiol Infect. 2016;22:775–81. doi: 10.1016/j.cmi.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 81.Stemler J, Hamed K, Salmanton-Garcȷa J, Rezaei-Matehkolaei A, GrȨfe SK, Sal E, et al. Mucormycosis in the middle east and North Africa: Analysis of the FungiScope® registry and cases from the literature. Mycoses. 2020;63:1060–8. doi: 10.1111/myc.13123. [DOI] [PubMed] [Google Scholar]