In December 2019, the SARS-CoV-2 coronavirus was detected for the first time in the Chinese city of Wuhan1. This virus is the cause of the pandemic that has resulted in nearly one million deaths to date, while saturating healthcare systems around the world and modifying surgical activity in our country2, 3. Despite being a respiratory virus, numerous non-respiratory complications have been reported triggered by SARS-CoV-2 infection and derived from its treatment4, 5. An increase in venous and arterial thromboembolic events has been demonstrated in these patients, as well as damage to the microvascularization. It has been suggested that endothelial damage is the main factor causing hypercoagulability in coronavirus disease 2019 (COVID-19)6, 7.
We present the case of a 40-year-old man with no history of interest who came to the emergency room due to abdominal pain in the epigastrium that had progressed over several days, with no other associated symptoms. Physical examination was anodyne, and laboratory tests showed: D-dimer 446 ng/mL, fibrinogen 742 mg/dL, and slightly prolonged prothrombin time (PT) and activated partial thromboplastin time (aPTT). SARS-CoV-2 screening was done with a polymerase chain reaction (PCR) test of a nasopharyngeal exudate sample as part of the hospital protocol, and the patient was discharged with a diagnosis of nonspecific abdominal pain. The next day, the patient received a positive PCR result for SARS-CoV-2. After 12 days of home isolation, the patient returned to the emergency room due to worsening abdominal pain and general malaise. He presented a diffusely tender abdomen with guarding and signs of peritoneal irritation in the epigastrium and mesogastrium. He did not present respiratory symptoms. Laboratory tests revealed increased acute-phase reactants. PT and aPTT remained long, fibrinogen elevated, and D-dimer increased to 947 ng/mL. Chest X-ray showed no pathological findings. A computed tomography (CT) scan was requested, which revealed a thrombus in the superior mesenteric vein originating from the confluence of the mesenteric-portal axis and a section of approximately 50 cm of dilated proximal jejunum with a thickened wall due to submucosal edema with low contrast uptake (Fig. 1 ). No intestinal pneumatosis, pneumoperitoneum or free fluid were observed. Given these findings, we decided to admit the patient in isolation for anticoagulant treatment and close monitoring. The patient had a good evolution, with a progressive decrease in abdominal pain, and was discharged on the sixth day after two negative nasopharyngeal exudate PCR. At discharge, a CT scan showed the resolution of the loop edema and the persistence of the thrombus. Oral anticoagulation was prescribed for six months. Four months later, a coagulopathy study revealed antithrombin III deficiency.
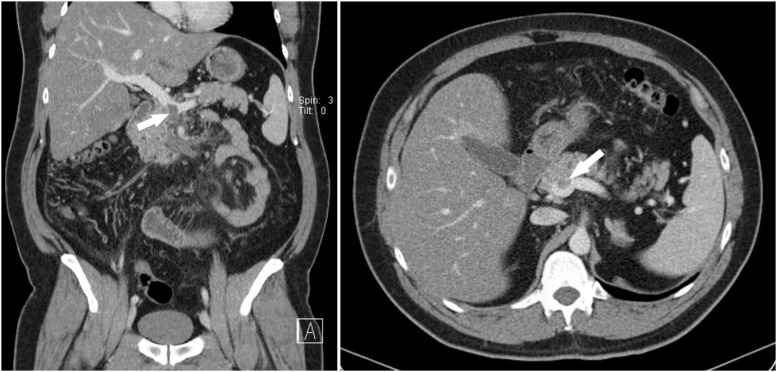
Fig. 1.
Coronal and axial computed tomography images showing the thrombus in the superior mesenteric vein in the confluence of the mesenteric-portal axis (arrow).
SARS-CoV-2 infection causes predominantly respiratory symptoms. However, since the appearance of this new disease, numerous cases of thromboembolic events have been described in patients with COVID-19. Nevertheless, in our review of the literature, we have not found any cases of isolated thrombosis of the superior mesenteric vein as the first and only symptom associated with SARS-CoV-2 infection, as in our case. The pathogenesis of this hypercoagulable state is not fully understood. It seems that endothelial injury plays a major role in the higher incidence of thromboembolic events in these patients. This is due to the fact that the virus enters the organism through the union of its surface protein to the angiotensin converting enzyme 2 (ACE2)8. Other associated factors are the presence of high levels of circulating prothrombotic factors such as fibrinogen or factor VIII and venostasis secondary to less mobilization in hospitalized and/or isolated patients. The most common coagulation abnormalities on lab tests are, as in the present case, a normal or slightly prolonged PT or aPTT, normal or slightly increased platelet count, and an elevated D-dimer9. The most frequent thromboembolic manifestations in these patients are deep vein thrombosis (DVT) and pulmonary embolism (PE)10, and it has even been suggested that many PE are primary thromboses of the pulmonary arteries secondary to endotheliitis. Thromboses of the mesenteric territory associated with SARS-CoV-2 infection are rare and occur mainly in the small vessels. The involvement of the large abdominal vessels is predominantly arterial and in hospitalized patients, while there have been few reported cases of mesenteric venous thrombosis, mostly associated with arterial thrombosis4.
In this second ‘wave’ of COVID-19 with more than 30 000 daily diagnoses in Spain, the number of asymptomatic infections or those with mild symptoms represent the majority of new positives. This is because more diagnostic tests are being performed and asymptomatic contacts traced. As a consequence, more and more forms of presentation and non-respiratory symptoms are being recorded in patients with active SARS-CoV-24 infection4. We have yet to resolve many unknown factors about the pathophysiology of this disease and its consequences in the medium and long term. Given the current healthcare situation and the constant increase in cases, we should include COVID-19 in the differential diagnoses of patients with abdominal thromboembolic events, especially in young patients with no previous pathology or risk factors. Likewise, we should highlight the need for thrombophilia studies in these patients, where COVID-19 can act as a precipitating factor for thromboembolic events in patients with undiagnosed coagulopathies.
Funding
This study has received no funding of any kind.
Conflict of interests
The authors have no conflict of interests to declare.
Footnotes
Please cite this article as: Navarro-Martínez S, Diez Ares JÁ, Peris Tomás N, Gonzálvez Guardiola P, Pérez-Rubio Á. Trombosis de la vena mesentérica superior como única manifestación de la infección por SARS-CoV-2. Cir Esp. 2022;100:245–247.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balibrea J.M., Badia J.M., Rubio Pérez I., Martín Antona E., Álvarez Peña E., García Botella S., et al. Surgical Management of Patients With COVID-19 Infection. Recommendations of the Spanish Association of Surgeons. Cir Esp. 2020;98:251–259. doi: 10.1016/j.ciresp.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Álvarez Gallego M., Gortázar de Las Casas S., Pascual Migueláñez I., Rubio-Pérez I., Barragán Serrano C., Álvarez Peña E., et al. SARS-CoV-2 pandemic on the activity and professionals of a General Surgery and Digestive Surgery Service in a tertiary hospital. Cir Esp. 2020;98:320–327. doi: 10.1016/j.ciresp.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S., et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 5.Gonzálvez Guardiola P., Díez Ares J., Peris Tomás N., Sebastián Tomás J.C., Navarro Martínez S. Intestinal perforation in patient with COVID-19 infection treated with tocilizumab and corticosteroids. Report of a clinical case. Cir Esp. 2020 doi: 10.1016/j.ciresp.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Libby P., Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41:3038–3044. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lowenstein C.J., Solomon S.D. Severe COVID-19 is a Microvascular Disease. Circulation. 2020 doi: 10.1161/circulationaha.120.050354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel A.B., Verma A. COVID-19 and Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: What Is the Evidence? JAMA. 2020;323:1769–1770. doi: 10.1001/jama.2020.4812. [DOI] [PubMed] [Google Scholar]
- 9.Panigada M., Bottino N., Tagliabue P., Grasselli G., Novembrino C., Chantarangkul V., et al. Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bilaloglu S., Aphinyanaphongs Y., Jones S., Iturrate E., Hochman J., Berger J.S. Thrombosis in Hospitalized Patients With COVID-19 in a New York City Health System. JAMA. 2020;324:799–801. doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]