Abstract
Purpose
We investigated the effectiveness of narrative vs non-narrative messages in changing COVID-19-related perceptions and intentions.
Design/Setting
The study employed a between-subjects two-group (narratives vs non-narratives) experimental design and was administered online.
Subjects/Intervention
1804 U.S. adults recruited via Amazon MTurk in September 2020 were randomly assigned to one of two experimental conditions and read either three narrative or three non-narrative messages about social distancing, vaccination, and unproven treatments.
Measures
Perceptions and intentions were assessed before and after message exposure (7-point scales).
Analysis
Using multivariable regression, we assessed main effects of the experimental condition (controlling for baseline measures) and interactions between the condition and pre-exposure perceptions/intentions in predicting post-exposure outcomes.
Results
Compared to non-narratives, narratives led to (1) less positive perceptions about the benefits of unproven treatments (M narrative = 3.60, M non-narrative = 3.77, P = .007); and (2) less willingness to receive an unproven drug (M narrative = 3.46, M non-narrative = 3.77, P < .001); this effect was stronger among individuals with higher baseline willingness to receive unproven drugs (baseline willingness = 2.09: b = −.06, P = .461; baseline willingness = 3.90: b = −.30, P < .001; baseline willingness = 5.71: b = −.55, P < .001). Narratives also led to more positive perceptions of vaccine safety/effectiveness, but only among individuals with lower baseline vaccine perceptions (baseline perceptions = 4.51: b = .10, P = .008; baseline perceptions = 5.89: b = .04, P = .167; baseline perceptions = 7: b = −.01, P = .688).
Conclusion
Narratives are a promising communication strategy, particularly for topics where views are not entrenched and among individuals who are more resistant to recommendations.
Keywords: COVID-19, narratives, misinformation, communication, health communications, disease management
Purpose
From the outset, the course of the COVID-19 pandemic has depended on large-scale behavior change at the population level 1 : slowing the spread of COVID-19 requires individuals to engage in behaviors like mask wearing and social distancing, while bringing the pandemic fully under control depends on individuals receiving vaccines. However, certain segments of the public have been resistant to following recommended protective behaviors. 2 Insufficient adoption of evidence-based behaviors has been aggravated by unprecedented misinformation and politicization surrounding the coronavirus.3,4 Therefore, there is an urgent need for more effective public health communication that encourages individuals to adopt protective health behaviors and prevents them from taking potentially harmful actions. We designed a study to examine the ability of narrative messages (or short personal stories) to improve perceptions and intentions related to recommended health behaviors in the context of COVID-19.
The COVID-19 pandemic poses many unique challenges to public health that necessitate a re-evaluation of existing health communication approaches. The pandemic is occurring at a time when many people report eroding trust in social institutions and experts,5,6 which may increase resistance toward following public health recommendations from sources of authority. 7 Resistance to health messages is not new, but it has been heightened in the context of COVID-19, with some groups arguing that public health directives adopted during the pandemic, like those requiring social distancing or mask wearing, violate their rights.8,9 Another key challenge in communicating about COVID-19 is that rumors and falsehoods about this pandemic, from the severity of the disease to potential treatments, have circulated on social media since COVID-19 emerged. 10 Although misinformation is not a novel phenomenon, the speed and scale at which it spreads in the digital era clearly poses a new challenge to public health response, and strategies to counter its effects are needed.
While unique in some ways, the COVID-19 pandemic also shares features with other public health crises that create communication challenges. Specifically, crises are often characterized by high uncertainty and strong negative emotions, 11 which can impact risk perceptions and attitudes toward recommended behaviors. 12 Further, when people feel threatened, they may experience “mental noise” that can impair information-processing, decision-making, and other key cognitive processes, rendering traditional communication approaches ineffective. 11 Therefore, communication efforts that solely focus on relaying facts and data based on the assumption that people will make rational decisions in response to this information may fall short. 12
Narrative-based messages conveying personal experience could be a potentially effective alternative approach. A narrative is a “representation of connected events and characters that has an identifiable structure, is bounded in space and time, and contains implicit or explicit messages about the topic being addressed”. 13 (p. 222) Research across a variety of health topics suggests that conveying health information through personal experience narratives is a more effective way to motivate and support behavior change than communicating facts and statistics.14-16
Narratives may also be particularly well-suited to relaying information about the COVID-19 pandemic for several reasons. First, narratives inhibit reactance because they are less likely to be recognized as a persuasive attempt17,18, which may make narratives particularly effective in the context of a pandemic characterized by unusual resistance to public health guidance. Second, studies have found that information provided in narrative form is better retrieved than information provided in other formats, 19 which suggests that narrative messages could help individuals process and retain information during a crisis. Finally, narratives may also be effective in correcting misinformation by replacing misbeliefs about COVID-19. Individuals need mental coherence and causal explanations for events. When such coherence is lacking (such as when scientific knowledge about an emerging disease is limited), individuals tend to adopt what information is available, regardless of its accuracy, to complete their mental models of events. 20 These models are difficult to update via simple provision of facts, 21 partially because people are resistant to being told what to do or how to think. 22 Thus, it is possible that by reducing overall resistance to the information in a message, narratives may be distinctly effective at helping individuals update inaccurate mental models.
To date, limited research has examined the effectiveness of narratives in the context of pandemics, and existing studies have shown mixed results.23-25 Bekalu et al 23 found a narrative video clip to be less effective than a non-narrative video in increasing knowledge and perceived response efficacy related to the prevention of pandemic influenza. Similarly, Kuru et al 24 compared the effectiveness of pro-MMR vaccine narratives to expert pro-vaccine science messages containing statistical information and found that the informational message outperformed the narrative one. However, narratives may prove more effective in the context of COVID-19 due to potentially greater resistance to COVID-19 messages, and the novelty of the COVID-19 vaccine compared to MMR/flu vaccines. For example, a recent study found that viewing a visual narrative course on the disease and how to protect oneself was associated with improved self-efficacy and behavioral intentions toward COVID-19 disease prevention (compared to a control course about sleep). 25
To test the effectiveness of narratives in promoting protective behaviors, we conducted an online experimental study to compare participants’ responses (relevant perceptions and intentions) to congruent COVID-19 behavior messages presented in two different formats: personal experience narrative vs non-narrative (didactic) information. We chose three distinct topics—namely, social distancing practices, vaccination, and the use of unproven treatments—to test the robustness of narratives as a messaging strategy across very different behaviors. It is important to note that at the time of the study, no vaccine had yet been authorized for use in the U.S. (although several were under development), and social distancing constituted a top priority for public health messaging and was mandated in several parts of the country. Further, discussion about use of treatments not authorized for COVID-19 (such as hydroxychloroquine) became more salient as the number of COVID-19 infections and deaths continued to rise and prominent public figures endorsed these unproven therapeutics.
We hypothesized that exposure to a narrative (versus non-narrative message) would lead to more positive perceptions of the behavior promoted in the message (H1a) and greater intention to engage in the behavior (H1b). Because the presumed advantage of narratives lies in their ability to reduce resistance to information, we also expected participants who initially held more negative perceptions/intentions toward a given COVID-19-related protective behavior to benefit more from exposure to a narrative. Stated formally, we hypothesized that the positive effect of a narrative vs non-narrative message on post-message exposure perceptions and intentions would be moderated by individuals’ initial perceptions and intentions levels, such that: (a) the effect on post-message exposure perceptions would be stronger for those with more negative initial perceptions of the behavior advocated in the message (H2a); and (b) the effect on post-message exposure intentions would be stronger for those with lower initial intentions to engage in that behavior (H2b).
Methods
Participants
A total of 1830 U.S. adults responded to the study invitation posted on Amazon’s Mechanical Turk (MTurk) platform.26,27 MTurk is an opt-in online crowdsourcing platform that has been used to facilitate recruitment of participants for scientific studies. Individuals who are at least 18 years old and have access to a computer with an internet connection are eligible to join MTurk. Users can then browse available research studies and are remunerated for their participation upon completion of a particular study. Remuneration is set by the study administrator (i.e., the researcher) based on study length. Participants can choose to redeem their earnings as cash or Amazon.com gift cards. 28 Further, MTurk users are vetted by the platform using patented technology that assesses data quality via measures of participant attention and engagement, among others. 29 In addition, our study also included an English proficiency check to ensure participants’ understanding of study materials; data from 26 participants were excluded because they failed this check, resulting in a final sample size of 1804. An overall response rate could not be calculated because the number of potential respondents who see the study invitation but choose not to participate is not recorded by MTurk.
Design and Setting
The online experiment employed a between-subjects two-group (type of message: narrative vs non-narrative) design and was administered via Qualtrics. After consenting to participate in the study, participants answered questions about personal experience with COVID-19 and how closely they followed COVID-19-related news, and responded to pre-exposure measures of perceptions and behavioral intentions relevant to the study topics. They were then randomly assigned to one of two experimental conditions: either personal experience narrative messages or non-narrative (didactic) messages with congruent topical content.
In each experimental condition, participants read three messages in randomized order. The survey software required participants to spend a minimum amount of time reading each message (215 milliseconds per word) before they could advance, to help ensure careful reading. After reviewing each message, participants reported their perceptions of, and intentions to engage in, the behavior discussed in the message. Participants then answered a series of socio-demographic questions. The study was fielded between September 16 and 23, 2020 and received approval from the internal review board of the institution where the study was conducted. Informed consent was obtained from all participants and they were remunerated $2 for completing the study.
Intervention
Participants assigned to the narrative condition read three first-person stories adapted from real news stories (see Appendix A). The social distancing message described the story of a woman whose husband contracted COVID-19 after ignoring social distancing recommendations and subsequently became an advocate of such measures. The vaccine message was about an individual who initially had negative views regarding vaccines but changed their mind after seeing the harm inflicted by COVID-19 and reading about the rigorousness of the vaccine development and review process. In the unproven treatment message, participants read about a COVID-19 patient’s request to take hydroxychloroquine and their subsequent discussion with their provider about potential side effects, which ends with the patient regretting their haste to take an unproven treatment and reiterating the importance of clinical trials. Participants in the non-narrative information condition read three messages on social distancing, vaccines, and unproven treatments that mirrored the information presented in the narrative messages, without the presence of a central character.
Measures
Perceptions
We assessed relevant perceptions (adapted from30,31) both at baseline and after exposure to the message. Participants reported their perceptions of (1) social distancing effectiveness (1 item: “Social distancing is an effective measure against the spread of the coronavirus” (1-strongly disagree to 7-strongly agree)); (2) vaccine safety and effectiveness (3 items: “Overall, vaccines are safe/effective/important to protect the health of others” (1-strongly disagree to 7-strongly agree; 8-don’t know, coded as missing); baseline Cronbach’s α = .94; post-exposure Cronbach’s α = .94); and (3) the benefits of unproven medical treatment (1 item: “What is your view about allowing more people access to experimental drugs for COVID-19 before clinical trials have been completed?” (1-the risks outweigh the benefits to 7-the benefits outweigh the risks)); and the importance of clinical trials (1 item: “How important do you think it is to go through the process of conducting clinical trials, even if it will lengthen the time it takes to make new treatments available to the public?” (1-not at all important to 7-very important)) 1 . These measures of perceptions were chosen because we considered them important drivers of the behaviors addressed in the messages and our messages were designed to influence these perceptions.
Behavioral Intentions
Behavioral intentions were also measured pre- and post-message exposure (adapted from 30 ). Participants reported: (1) intention to engage in social distancing in the next 7 days (1-strongly disagree to 7-strongly agree); (2) intention to take a vaccine to prevent COVID-19 if one were available (1-definitely NOT get the vaccine to 7-definitely get the vaccine); and (3) willingness to take a drug that is being tested in clinical trials and has not yet been approved for the treatment of COVID-19 (1-strongly disagree to 7-strongly agree).
Covariates
Participants reported their personal experience with COVID-19, how closely they had been following news about the virus, employment status, political views, geographic location, whether they had been diagnosed with certain health conditions that put them at risk for COVID-19 complications, whether people in their community wore masks, and basic demographics (age, gender, race, Hispanic ethnicity, and education).
Statistical Analysis
Data were analyzed with Stata 15.1. All potential covariates were significantly correlated with most outcomes (P-values<.10) and were included in the final models 2 . 32 We first ran seven multivariable regression models to assess the main effects of the experimental condition (0-non-narrative; 1-narrative) on each post-exposure outcome, controlling for baseline measures on that particular outcome (in addition to covariates). We then ran another seven multivariable regression models to assess the interaction between the experimental condition and the pre-exposure measure in predicting the post-exposure outcome (perceptions or behavioral intentions). De-identified participant data are available by request.
Results
Table 1 presents descriptive statistics for all covariates included in the analyses and Table 2 presents perception and behavioral intention unadjusted means and standard deviations.
Table 1.
Descriptive Statistics of Covariates Included in the Models.
| Covariate | %/M (SD) |
|---|---|
| Age | 39.10 (11.91) |
| Gender | |
| Male | 51.50 |
| Female | 47.89 |
| Prefer to self-describe (coded as missing) | .61 |
| Race | |
| White | 78.94 |
| Non-White | 21.06 |
| Hispanic | |
| Yes | 7.87 |
| No | 92.13 |
| Education | |
| Less than college | 61.86 |
| College degree or higher | 38.03 |
| Missing | .11 |
| Personal experience with coronavirus | |
| No one had the virus | 88.64 |
| Self/housemate had the virus | 7.43 |
| Missing | 3.94 |
| Employment status | |
| Not having to go to work | 58.04 |
| Having to go to work | 36.47 |
| Missing | 5.49 |
| Living area | |
| City/suburb | 65.47 |
| Small town/rural area | 34.53 |
| Flu shot | |
| No | 56.60 |
| Yes | 42.07 |
| Not sure (coded as missing) | 1.33 |
| Health conditions that increase risk for complications from COVID-19 | |
| No condition | 77.38 |
| At least one condition | 22.28 |
| Mask wearing in respondent’s community (1-never; 4-all the time) | 3.44 (.64) |
| Political views (1-very liberal; 7-very conservative) | 3.38 (1.78) |
| Following news about the virus (1-not at all closely; 7-very closely) | 5.56 (1.36) |
Table 2.
Unadjusted Means (Standard Deviations) by Experimental Condition.
| Variable | Experimental Condition | Total | |
|---|---|---|---|
| Non-narrative | Narrative | ||
| Baseline perceptions of social distancing effectiveness | 6.25 (1.19) | 6.11 (1.29) | 6.18 (1.24) |
| Post-exposure perceptions of social distancing effectiveness | 6.33 (1.21) | 6.22 (1.26) | 6.27 (1.24) |
| Baseline intentions to socially distance | 6.30 (1.32) | 6.22 (1.45) | 6.26 (1.39) |
| Post-exposure intentions to socially distance | 6.39 (1.26) | 6.29 (1.39) | 6.34 (1.33) |
| Baseline perceptions of vaccine safety and effectiveness | 5.92 (1.41) | 5.86 (1.36) | 5.89 (1.38) |
| Post-exposure perceptions of vaccine safety and effectiveness | 5.98 (1.40) | 5.97 (1.32) | 5.97 (1.36) |
| Baseline intentions to receive a vaccine | 4.97 (2.05) | 4.86 (2.02) | 4.91 (2.03) |
| Post-exposure intentions to receive a vaccine | 4.95 (2.06) | 4.89 (2.00) | 4.92 (2.03) |
| Baseline perceptions about the benefits of unproven drugs | 4.03 (1.85) | 3.98 (1.79) | 4.00 (1.82) |
| Post-exposure perceptions about the benefits of unproven drugs | 3.77 (1.77) | 3.57 (1.81) | 3.67 (1.80) |
| Baseline perceptions of importance of clinical trials | 6.25 (1.08) | 6.23 (1.11) | 6.24 (1.09) |
| Post-exposure perceptions of importance of clinical trials | 6.25 (1.06) | 6.27 (1.11) | 6.26 (1.08) |
| Baseline intentions to receive an experimental drug | 3.95 (1.82) | 3.79 (1.79) | 3.90 (1.81) |
| Post-exposure intentions to receive an experimental drug | 3.85 (1.81) | 3.61 (1.78) | 3.61 (1.78) |
Intervention Effects (H1a and H1b)
The experimental condition participants were assigned to had no effect on perceptions of social distancing effectiveness (P = .778); intentions to engage in social distancing in the next 7 days (P = .563); perceptions of vaccine safety and effectiveness (P = .174); intentions to receive a COVID-19 vaccine if one were available (P = .199); or perceptions of the importance of clinical trials (P = .289). In contrast, an effect was observed for the unproven drug outcomes. Participants who read the narrative vs non-narrative message expressed less positive perceptions about the benefits of unproven drugs (b = −.18, P = .007; ηp2 = .005). Further, participants in the narrative vs non-narrative condition reported lower willingness to receive an unproven drug (b = −.30, P < .001; ηp2 = .016). See Appendix B for regression models. Table 3 presents adjusted means by experimental condition.
Table 3.
Adjusted Means (Standard Errors) by Experimental Condition.
| Outcome | Experimental Condition | P-value | |
|---|---|---|---|
| Non-narrative | Narrative | ||
| Post-exposure perceptions of social distancing effectiveness | 6.28 (.02) | 6.29 (.02) | .778 |
| Post-exposure intentions to socially distance | 6.36 (.03) | 6.34 (.03) | .563 |
| Post-exposure perceptions of vaccine safety and effectiveness | 5.96 (.02) | 6.00 (.02) | .174 |
| Post-exposure intentions to receive a vaccine | 4.91 (.02) | 4.96 (.03) | .199 |
| Post-exposure perceptions about the benefits of unproven drugs | 3.77 (.05) | 3.60 (.05) | .007 |
| Post-exposure perceptions of importance of clinical trials | 6.25 (.03) | 6.29 (.03) | .289 |
| Post-exposure intentions to receive an experimental drug | 3.77 (.04) | 3.46 (.04) | <.001 |
Moderation of Intervention Effects by Baseline Measures (H2a and H2b)
The experimental condition did not interact with the corresponding baseline measure of perception and behavioral intention in predicting post-exposure perceived social distancing effectiveness (P = .251), intentions to engage in social distancing in the next 7 days (P = .838), intentions to receive a COVID-19 vaccine if one were available (P = .170), perceived benefits of unproven drugs (P = .268), or perceived importance of clinical trials (P = .756).
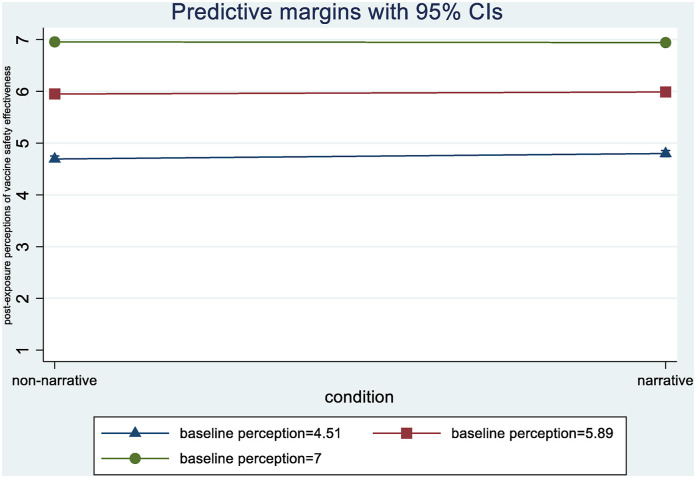
However, the experimental condition interacted with baseline perceptions of vaccine safety and effectiveness in predicting post-exposure vaccine perceptions (b = −.05, P = .018, 95% CI = [−.09; −.01]; ηp2 = .004). Exposure to a narrative (vs non-narrative) message about vaccines led to more positive vaccine safety and effectiveness perceptions, but only for participants who reported the least positive vaccine perceptions at baseline (baseline perceptions = 4.51 (1 SD below the mean): b = .10, P = .008, 95% CI = [.03; 0.18]; baseline perceptions = 5.89 (mean): b = .04, P = .167, 95% CI = [.02; 0.09]; baseline perceptions = 7: b = −.01, P = .688, 95% CI = [−.08; 0.06] 3 ). This interaction is plotted in Figure 1.
Figure 1.
Experimental condition and baseline perceptions of vaccine safety and effectiveness interact in predicting post-exposure perceptions of vaccine safety and effectiveness.
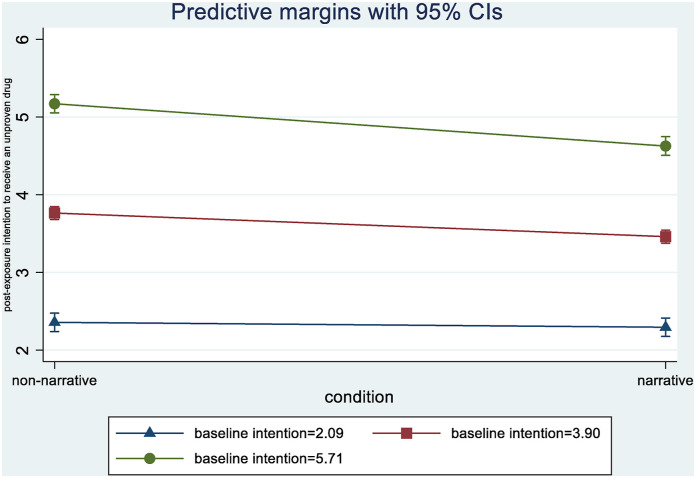
The experimental condition also interacted with baseline willingness to receive an unproven drug in predicting post-exposure willingness to receive such a drug (b = −.13, P < .001; 95% CI = [−.20; −.07]; ηp2 = .01). Exposure to the narrative (vs non-narrative) message led to lower willingness to receive an unproven drug, but only among individuals with average and above average baseline willingness (baseline willingness = 2.09 (1 SD below the mean): b = −.06, P = .461, 95% CI = [−.23; 0.10]; baseline willingness = 3.90 (mean): b = −.30, P < .001, 95% CI = [−.42; −.19]; baseline willingness = 5.71 (1 SD above the mean): b = −.55, P < .001, 95% CI = [−.71; −.38]). This interaction is plotted in Figure 2.
Figure 2.
Experimental condition and baseline intentions to receive an unproven drug interact in predicting post-exposure intentions to receive an unproven drug.
Discussion
COVID-19 communication to date has been fraught with challenges. 33 Effective messaging must not only contend with the usual challenges associated with crisis communication, but also the high levels of polarization, politicization of the pandemic, and the spread of misinformation, which have generated resistance to public health guidance. We explored the utility of narratives in promoting protective COVID-19 health behaviors. The effect of narratives was not uniformly observed across the three topics under study. Specifically, narratives (vs non-narrative messages) led to: (1) more negative perceptions about the benefits of unproven drugs; (2) less willingness to receive an unproven treatment for COVID-19 (especially among individuals with higher baseline willingness to receive an unproven drug); and (3) more positive perceptions of vaccine safety and effectiveness, but only among individuals with lower baseline vaccine perceptions. There were no significant differences between conditions for perceived social distancing effectiveness, intentions to practice social distancing, or intentions to vaccinate.
These findings offer several insights about the use of narratives as a communication strategy, both in the current pandemic and for future public health challenges. First, our results suggest that narratives may be more effective for topics where views are less entrenched. We suspect that narrative messages were effective in dissuading people from wanting to use unproven drugs, but did not have a substantial impact on vaccination or social distancing intentions, because the public had less crystalized views on unproven drugs, which allowed for change to occur via a one-time exposure to a narrative message. This premise is supported by the fact that overall baseline perceptions about the benefits of unproven drugs were closer to the mid-point of the scale (as opposed to vaccination and social distancing perceptions, which were closer to the extremes of the scales). Bode and Vraga 34 similarly found that corrections delivered via news stories were more successful at changing views toward a more novel topic for which public opinion was less established (i.e., health consequences of GMOs), than for the link between vaccines and autism, suggesting our findings could apply beyond the COVID-19 pandemic context.
When views about a health topic are more established, the persuasive advantage of narratives over non-narratives may only manifest for individuals who disagree with the recommendation being promoted because it reduces their scrutiny of the message content. That narratives led to more positive perceptions of vaccine safety and effectiveness, but only among those with the least positive perceptions at baseline, aligns with prior work finding that narratives perform better than statistical evidence when information in a message is value-discrepant. 35
In contrast, we did not observe a similar effect of narratives for intentions to receive a COVID-19 vaccine. Intentions to receive a vaccine may be much harder to change with a one-time exposure to a message, particularly given that no COVID-19 vaccine had been approved at the time of the study. Therefore, it may have been difficult for participants to form and express an intention to accept such a vaccine prior to its approval. Yet, the positive effect on perceptions of safety and effectiveness among those most hesitant about vaccines in our sample is still notable, particularly when considering the large volume of vaccine misinformation in circulation.36,37
The beneficial effects of narratives on vaccine perceptions and willingness to try an unproven drug among participants who at baseline had views that were most divergent with public health recommendations also suggest that narratives may be effective in countering misinformation about the coronavirus. Some participants’ negative views of vaccines and positive views toward trying unproven drugs for COVID-19 at baseline could have been, at least in part, influenced by rampant misinformation about these topics. Then, the observed revision in perceptions/intentions after exposure to narratives would indicate that narratives may have facilitated an update of such inaccurate beliefs. 22
The lack of main effects on social distancing-related perceptions and intentions may be explained by participants’ overall strongly positive baseline perceptions and intentions. This baseline alignment with public health recommendations may have limited both the persuasive advantage of narratives to reduce psychological resistance (since there was likely very little of it, similar to findings observed by Bekalu et al in the context of pandemic influenza 23 ) and the overall ability of a message to induce additional change. When the study was conducted, social distancing was being enforced in many places (e.g., stores, public transit, and restaurants), which may have created a perception of social distancing as normative, in which case participants in the study provided responses that aligned with those perceived norms. 38
The pandemic situation has evolved in important ways since this study was conducted, and our findings should be considered in light of these changes. Notable differences include the actual availability of vaccines today, further politicization of preventive measures, and exacerbated pandemic fatigue. Whereas these changes do not necessarily negate the effectiveness of narratives as a public health messaging strategy, they do have implications for how narrative content should be constructed. For example, the availability of vaccines, coupled with their politicization, means views on vaccination today are both more crystalized and more divided along partisan lines. 39 To successfully address these issues, narrative messages may need to be modified to focus on current concerns (e.g., fertility or myocarditis risk) 40 and highlight values relevant to either side of the political spectrum.41,42 Additionally, the use of unauthorized treatments (e.g., ivermectin) has become an increasingly pressing concern, 43 suggesting that there is an urgent need to effectively communicate about the risks of taking unproven treatments without generating reactance. Narratives, then, could be particularly effective in this context. Finally, pandemic fatigue is higher today than it was when this study was conducted, which may mean that text-based narratives may garner less engagement than they would have earlier in the pandemic and may need to be visually enhanced to be effective (e.g., through videos, cartoons, and virtual reality). 44
Conducted at the height of the COVID-19 pandemic, this study contributes to our understanding of the utility of narrative persuasion in health communication during public health emergencies. Findings show that using narratives to communicate critical information is a promising strategy for novel topics where views are still developing and among individuals who are most likely to be resistant to public health recommendations. We also find evidence that narratives may be persuasive even when a topic is the target of significant misinformation (e.g., vaccination). Whether narratives indeed help update misperceptions about such topics should be further studied using more detailed measures. Although more work is needed, this study adds to our developing understanding of how we can best relay evidence-based recommendations to the public.
Limitations
This study has several limitations. The lack of effects observed on some outcomes may be because the experiment involved a single exposure to each message—findings might have been different if participants were exposed to the messages repeatedly over time, as would occur with a public health campaign. Non-significant findings may also be explained by the pre-post design, where post-measures were administered immediately after message exposure. Others have found a sleeper effect associated with narrative persuasion, such that the magnitude of effects increases over time. 45 Further, the control messages were very detailed and informative, which also could have contributed to the limited intervention effect; however, keeping information congruent across conditions enabled us to hone in on the effect of the narrative format. Moreover, the effects that were observed were small, but this is not unusual in narrative persuasion research 23 and does not mean the findings are not consequential. Small effects for one-time message exposures can have cumulatively large effects via repeated exposure in the context of a long-term public health communication campaign 46 and can have meaningful population-level impact due to their substantial reach. 47
Another limitation concerns the fact that we relied on an online convenience sample which reduces the generalizability of our findings. Specifically, MTurk users tend to be younger, more liberal, and better educated, compared to the U.S. population; further, users may have previously participated in similar studies, affecting their sensitivity to study materials and/or measurements, 48 thus, potentially reducing the effects observed. Finally, the study was conducted in September 2020 and since then perceptions and intentions regarding the topics under study have likely shifted (as explained above). These limitations aside, narrative as a format for COVID-19 communication remains promising, as long as message content is up-to-date and responsive to current concerns and conditions.
SO WHAT?
What is already known on this topic?
Narratives have been shown to be an effective communication strategy across a wide range of health topics.
What does this article add?
In a pandemic context, narratives are more effective than non-narratives (1) when communicating about emerging topics on which views may be less entrenched, and (2) when targeting individuals inclined to be resistant to behavioral recommendations.
What are the implications for health promotion practice or research?
Narratives can be effective in certain situations and can be an important tool for public health practitioners. To optimize this communication approach, more research is needed in the context of pandemics to investigate when narratives are most effective and why.
Appendix A. Study messages
Topic 1:
Social Distancing
| Didactic Message | Narrative Message |
|---|---|
| Social distancing is one of the most effective tools we have to reduce the spread of COVID-19. Social distancing includes staying at least 6 feet from other people, not gathering in groups, and staying out of crowded places. Because people can spread the virus before they feel sick, it is important to stay away from others when possible, even if you—or they—have no symptoms. Following public health researchers’ recommendations, many states passed measures to enforce social distancing, such as ordering all non-essential businesses to close to prevent people from crowding inside stores or restaurants and to slow the spread of the disease. These social distancing restrictions have been found to be effective, and research shows that the measures need to stay in place in order to control the disease and prevent more cases and deaths from COVID-19. It is critical that social distancing measures, even though inconvenient, are followed to the extent possible until this potentially deadly disease is under control |
A few months ago, my husband made some comments on social media criticizing restrictions the governor ordered to enforce social distancing in response to COVID-19. John said that people who stayed at home were just being paranoid. Well, a few weeks later, he got sick and eventually tested positive for COVID-19. I want to make it clear that John is not an irresponsible person. As soon as he tested positive, he called everyone he had been in contact with and told them to quarantine themselves because his doctor said that it’s possible for someone to spread the virus even before they start feeling sick
Thankfully John recovered, and since then he has been encouraging everyone to comply with the state’s social distancing guidelines and public health researchers’ recommendations, like staying 6 feet from other people and avoiding crowded places like stores or restaurants. John understands now that he was wrong. Like many others, we didn’t realize how important these measures were to prevent people from getting this potentially deadly disease, but now we know that even though social distancing might be inconvenient- it’s the right thing to do. We will continue to practice social distancing until the disease is under control |
Topic 2:
Vaccination.
| Didactic Message | Narrative Message |
|---|---|
| Many people who oppose vaccines try to convince others that the vaccines themselves are more dangerous than the diseases they protect against. These groups are similarly trying to downplay the seriousness of COVID-19 in order to discourage individuals from getting a COVID-19 vaccine when one becomes available. But COVID-19 is much deadlier than the flu, and so far 200 000 people in the U.S. have died from the disease. People living in assisted living facilities and those with underlying health conditions are more likely to be infected and suffer complications from the disease. A vaccine is our best hope for preventing people from getting sick, and even dying, from COVID-19. Additionally, because vaccines are given to large numbers of generally healthy people, they have to meet even higher standards for safety and efficacy than products that are meant for people who are already sick. First, a vaccine is tested in animals to see if it works and if it’s safe. Next, a vaccine is tested for safety and efficacy in humans in three phases of clinical trials. If a vaccine produces good results in these trials, it is submitted to the Food and Drug Administration for approval where it further undergoes several layers of safety review. After approving a vaccine, the FDA oversees its production to ensure continuing safety | When my daughter was born, I was really hesitant to get her vaccinated. I had seen a lot of bad things about the dangers of vaccines online, and that’s why I wouldn’t get flu shots either. But this COVID-19 pandemic has completely changed my mind - I’ve now seen firsthand what this disease can do when there’s no vaccine available to control it. My mother lives in an assisted living facility, where several residents have tested positive for COVID-19. She suffers from chronic lung disease, which makes me very afraid about what will happen if she gets COVID-19. This isn’t just a flu – 200 000 people have already died from COVID-19. It’s a scary situation, because it feels like any day, anyone can get sick and there isn’t much we can do to stop it. I have been reading a lot about the pandemic - there has been a lot of news about how a vaccine could finally put a stop to this disease, and how scientists are working to develop one. I now understand how rigorous vaccine oversight is and how vaccines have to go through a lot of safety and efficacy tests to get FDA approval before they can be made available to the public. Now that I know how many systems are in place to ensure vaccines are safe, and that a vaccine is our best hope for stopping this horrible disease, when a vaccine is finally available, I am going to be the first in line to get one |
Topic 3:
Unproven Treatment.
| Didactic Message | Narrative Message |
|---|---|
| Contrary to what you might have read or heard, hydroxychloroquine has NOT been shown to be safe or effective for treating COVID-19. Hydroxychloroquine is not approved for the treatment of COVID-19 patients. Additionally, there is evidence to suggest that hydroxychloroquine can have serious side effects, including heart rhythm problems that can be deadly. There are currently several other potential treatments for COVID-19 being studied in clinical trials. Clinical trials are the primary way that researchers find out if a new treatment is safe and effective in people. Without conducting clinical trials, we do not have enough evidence to know if a treatment is safe and effective, and there is a risk that people will be given treatments that do not work and may even be harmful | On Apr 15, I got a call with news that didn’t surprise me at all: I tested positive for COVID-19. I had been miserable for many days at that point and was very scared. Several friends urged me to take hydroxychloroquine because they heard it could be used to treat COVID-19. I was desperate to try anything, so I asked my doctor for a prescription. My doctor told me that this drug has not been approved to treat COVID-19 and that in some patients, it can cause serious side effects, including heart rhythm problems that can be deadly. She talked me out of it, and in hindsight, I am glad I didn’t take the risk. I eventually felt better and thankfully, the worst is behind me. I’m actually a little embarrassed that I was so willing to try an unproven treatment. There is a reason they conduct clinical trials to prove the efficacy and safety of treatments before people can take them. We need the clinical trials to know what the risks and benefits are so we can make sure we are helping people and not hurting them |
Appendix B. Regression model results for each of the outcomes.
| Predictors in the Model | Coefficient | Standard Error | t | 95% CI | P-value |
|---|---|---|---|---|---|
| Outcome: Perceptions of Social Distancing Effectiveness | |||||
| Experimental condition | .01 | .03 | .28 | −.06; .08 | .778 |
| Baseline perceptions | .80 | .01 | 53.66 | .77; .83 | <.001 |
| Age | −.0003 | .002 | −.18 | −.003; 0.003 | .856 |
| Education (ref: college+) | .04 | .04 | 1.13 | −.03; .11 | .257 |
| Race (ref: white) | −.01 | .04 | −.21 | −.09; .08 | .834 |
| Hispanic (ref: yes) | .01 | .06 | .08 | −.12; .13 | .934 |
| Gender (ref: male) | .03 | .03 | .73 | −.04; .09 | .463 |
| Employment (ref: not having to go to work) | −.04 | .04 | −1.10 | −.11; .03 | .273 |
| Living area (ref: city/suburb) | .04 | .04 | 1.04 | −.03; .11 | .298 |
| COVID-19 experience (ref: no) | −.05 | .07 | −.79 | −.18; .08 | .431 |
| COVID-19 news following | .002 | .01 | .13 | −.02; .03 | .897 |
| Flu shot (ref: no) | .03 | .04 | .84 | −.04; .10 | .400 |
| Mask wearing in one’s community | .08 | .03 | 3.08 | .03; .14 | .002 |
| Political views | −.05 | .01 | −4.70 | −.07; −.03 | <.001 |
| Health condition (ref: none) | −.06 | .04 | −1.32 | −.14; .03 | .188 |
| Outcome: Intention to social distance | |||||
| Experimental condition | −.02 | .04 | −.58 | −.09; .05 | .563 |
| Baseline intentions | .76 | .01 | 54.57 | .73; .79 | <.001 |
| Age | .002 | .002 | 1.31 | −.001; .01 | .190 |
| Education (ref: college+) | .02 | .04 | .59 | −.05; .10 | .558 |
| Race (ref: white) | .05 | .05 | 1.05 | −.04; .14 | .294 |
| Hispanic (ref: yes) | .01 | .07 | .11 | −.13; .14 | .910 |
| Gender (ref: male) | −.03 | .04 | −.81 | −.10; .04 | .418 |
| Employment (ref: not having to go to work) | −.03 | .04 | −.81 | −.10; .04 | .419 |
| Living area (ref: city/suburb) | −.01 | .04 | −.35 | −.09; .06 | .726 |
| COVID-19 experience (ref: no) | .13 | .07 | 1.78 | −.01; .26 | .075 |
| COVID-19 news following | .05 | .01 | 3.42 | .02; .08 | .001 |
| Flu shot (ref: no) | .06 | .04 | 1.53 | −.02; .13 | .125 |
| Mask wearing in one’s community | .09 | .03 | 3.28 | .04; .15 | .001 |
| Political views | −.05 | .01 | −5.07 | −.08; −.03 | <.001 |
| Health condition (ref: none) | −.14 | .05 | −3.15 | −.23; −.05 | .002 |
| Outcome: Perceptions of vaccine safety and effectiveness | |||||
| Experimental condition | .04 | .03 | 1.36 | −.02; .09 | .174 |
| Baseline perceptions | .88 | .01 | 77.86 | .86; .91 | <.001 |
| Age | .001 | .001 | 1.01 | −.001; .004 | .314 |
| Education (ref: college+) | .03 | .03 | 1.02 | −.03; .09 | .308 |
| Race (ref: white) | −.01 | .04 | −.28 | −.08; .06 | .780 |
| Hispanic (ref: yes) | −.04 | .05 | −.82 | −.15; .06 | .412 |
| Gender (ref: male) | −.02 | .03 | −.63 | −.07; .04 | .528 |
| Employment (ref: not having to go to work) | −.01 | .03 | −.39 | −.07; .05 | .697 |
| Living area (ref: city/suburb) | −.02 | .03 | −.56 | −.08; .04 | .578 |
| COVID-19 experience (ref: no) | .02 | .06 | .36 | −.09; .13 | .720 |
| COVID-19 news following | .02 | .01 | 1.90 | −.001; .04 | .057 |
| Flu shot (ref: no) | .02 | .03 | .52 | −.04; .08 | .606 |
| Mask wearing in one’s community | .03 | .02 | 1.15 | −.02; .07 | .249 |
| Political views | −.03 | .01 | −3.07 | −.04; −.01 | .002 |
| Health condition (ref: none) | .004 | .04 | .11 | −.06; .07 | .911 |
| Outcome: Intention to receive a vaccine | |||||
| Experimental condition | .05 | .04 | 1.28 | −.02; .12 | .199 |
| Baseline intentions | .93 | .01 | 95.04 | .92; .95 | <.001 |
| Age | −.001 | .002 | −.62 | −.004; .002 | .535 |
| Education (ref: college+) | .01 | .04 | .15 | −.07; .08 | .879 |
| Race (ref: white) | .01 | .05 | .24 | −.08; .10 | .807 |
| Hispanic (ref: yes) | .07 | .07 | .98 | −.07; .20 | .326 |
| Gender (ref: male) | −.02 | .04 | −.53 | −.09; .05 | .599 |
| Employment (ref: not having to go to work) | .03 | .04 | .82 | −.04; .10 | .412 |
| Living area (ref: city/suburb) | −.04 | .04 | −1.03 | −.12; .04 | .302 |
| COVID-19 experience (ref: no) | .02 | .07 | .33 | −.11; .16 | .739 |
| COVID-19 news following | −.02 | .01 | −1.79 | −.05; .002 | .074 |
| Flu shot (ref: no) | .05 | .04 | 1.27 | −.03; .13 | .204 |
| Mask wearing in one’s community | −.02 | .03 | −.59 | −.07; .04 | .558 |
| Political views | −.03 | .01 | −2.66 | −.05; −.01 | .008 |
| Health condition (ref: none) | .01 | .04 | .26 | −.08; .10 | .793 |
| Outcome: Perceptions about the benefits of unproven drugs | |||||
| Experimental condition | −.18 | .07 | −2.69 | −.31; −.05 | .007 |
| Baseline perceptions | .66 | .02 | 36.26 | .62; .69 | <.001 |
| Age | .005 | .003 | 1.63 | −.001; .01 | .104 |
| Education (ref: college+) | .03 | .07 | .44 | −.11; .17 | .657 |
| Race (ref: white) | −.06 | .08 | −.70 | −.22; .11 | .481 |
| Hispanic (ref: yes) | .32 | .13 | 2.52 | .07; .56 | .012 |
| Gender (ref: male) | −.03 | .07 | −.52 | −.17; .10 | .603 |
| Employment (ref: not having to go to work) | .12 | .07 | 1.75 | −.01; .25 | .080 |
| Living area (ref: city/suburb) | .05 | .07 | .70 | −.09; .19 | .487 |
| COVID-19 experience (ref: no) | .18 | .13 | 1.39 | −.07; .43 | .165 |
| COVID-19 news following | −.01 | .03 | −.42 | −.06; .04 | .673 |
| Flu shot (ref: no) | .08 | .07 | 1.11 | −.06; .21 | .267 |
| Mask wearing in one’s community | .03 | .05 | .65 | −.07; .14 | .513 |
| Political views | .08 | .02 | 4.28 | .04; .12 | <.001 |
| Health condition (ref: none) | −.03 | .08 | −.37 | −.19; .13 | .714 |
| Outcome: Perceptions of importance of clinical trials | |||||
| Experimental condition | .04 | .04 | 1.06 | −.03; .11 | .289 |
| Baseline perceptions | .70 | .02 | 40.66 | .67; .74 | <.001 |
| Age | .003 | .002 | 1.75 | −.0003; .01 | .081 |
| Education (ref: college+) | −.01 | .04 | −.26 | −.09; .07 | .796 |
| Race (ref: white) | .07 | .05 | 1.43 | −.02; .16 | .153 |
| Hispanic (ref: yes) | .004 | .07 | .05 | −.14; .14 | .957 |
| Gender (ref: male) | −.03 | .04 | −.68 | −.10; .05 | .498 |
| Employment (ref: not having to go to work) | .02 | .04 | .45 | −.06; .09 | .653 |
| Living area (ref: city/suburb) | .01 | .04 | .29 | −.07; .09 | .773 |
| COVID-19 experience (ref: no) | −.12 | .07 | −1.65 | −.26; .02 | .099 |
| COVID-19 news following | .04 | .01 | 2.47 | .01; .06 | .013 |
| Flu shot (ref: no) | −.01 | .04 | −.16 | −.08; .07 | .872 |
| Mask wearing in one’s community | −.04 | .03 | −1.52 | −.10; .01 | .128 |
| Political views | −.06 | .01 | −5.12 | −.08; −.03 | <.001 |
| Health condition (ref: none) | −.03 | .05 | −.58 | −.12; .06 | .563 |
| Outcome: Willingness to receive an experimental drug | |||||
| Experimental condition | −.30 | .06 | −4.99 | −.42; −.18 | <.001 |
| Baseline willingness | .71 | .02 | 41.59 | .68; .74 | <.001 |
| Age | .003 | .003 | 1.29 | −.002; .01 | .198 |
| Education (ref: college+) | .09 | .06 | 1.42 | −.03; .22 | .155 |
| Race (ref: white) | −.20 | .08 | −2.55 | −.35; .05 | .011 |
| Hispanic (ref: yes) | −.02 | .12 | −.18 | −.25; .21 | .860 |
| Gender (ref: male) | −.05 | .06 | −.85 | −.17; .07 | .398 |
| Employment (ref: not having to go to work) | .06 | .06 | .95 | −.06; .19 | .340 |
| Living area (ref: city/suburb) | −.10 | .07 | −1.43 | −.23; .04 | .154 |
| COVID-19 experience (ref: no) | .24 | .12 | 2.02 | .01; .47 | .044 |
| COVID-19 news following | −.003 | .02 | −.12 | −.05; .04 | .906 |
| Flu shot (ref: no) | .11 | .06 | 1.71 | −.02; .24 | .088 |
| Mask wearing in one’s community | −.02 | .05 | −.50 | −.12; .07 | .620 |
| Political views | .05 | .02 | 2.92 | .02; .09 | .004 |
| Health condition (ref: none) | −.07 | .08 | −.98 | −.22; .07 | .328 |
Notes
Participants were provided with a definition of “clinical trials”.
The pattern of results did not change in models without covariates.
We probed this interaction at the maximum value on the scale as opposed to the conventional value of one standard deviation above the mean because the latter was outside the scale range (7.27).
Footnotes
Author Contributions: Iles: Conceptualization; Formal analysis; Methodology; Writing – Original Draft Preparation; Writing – Review & Editing; Gaysynsky: Conceptualization; Methodology; Writing – Original Draft Preparation; Writing – Review & Editing; Chou: Conceptualization; Methodology; Writing – Original Draft Preparation; Writing – Review & Editing
Data Availability: De-identified participant data are available to individual investigators by request from the authors.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the National Cancer Institute under contract number HHSN261201800002 B issued to Westat. The funder had no role in the study design; collection, analysis and interpretation of data; writing of the report; or the decision to submit the article for publication.
Correction (May 2024): The affiliations for the authors Anna Gaysynsky and Wen-Ying Sylvia Chou have been corrected. The correction notice can be accessed at the following link: 10.1177/08901171241259295.
Disclaimer: The opinions expressed by the authors are their own and the research presented in this paper should not be interpreted as representing the official viewpoint of the U.S. Department of Health and Human Services, the National Institutes of Health or the National Cancer Institute.
ORCID iDs: Irina A. Iles https://orcid.org/0000-0002-9348-1012
Anna Gaysynsky https://orcid.org/0000-0001-5612-5572
References
- 1.Van Bavel JJ, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020; 4: 460-471. [DOI] [PubMed] [Google Scholar]
- 2.Russ MJ, Sisti D, Wilner PJ. When patients refuse COVID-19 testing, quarantine, and social distancing in inpatient psychiatry: Clinical and ethical challenges. J Med Ethics. 2020; 46(9): 579-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Managing the COVID-19 Infodemic: Promoting Healthy Behaviours and Mitigating the Harm from Misinformation and Disinformation - Joint Statement by WHO, UN, UNICEF, UNDP, UNESCO, UNAIDS, ITU, UN Global Pulse. IFRC; 2020. [Google Scholar]
- 4.Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020; 263: 113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pew Research Center . Americans’ Views of Government: Low Trust, but Some Positive Performance Ratings. 2020. Available at: https://www.pewresearch.org/politics/2020/09/14/americans-views-of-government-low-trust-but-some-positive-performance-ratings/https://www.pewresearch.org/politics/2020/09/14/americans-views-of-government-low-trust-but-some-positive-performance-ratings/. [Google Scholar]
- 6.Johnson Foundation RW, Harvard TH. Chan School of Public Health. The Public's Perspective on the United States Public Health System 2021. [Google Scholar]
- 7.Lalot F, Heering MS, Rullo M, Travaglino GA, Abrams D. The Dangers of Distrustful Complacency: Low Concern and Low Political Trust Combine to Undermine Compliance with Governmental Restrictions in the Emerging Covid-19 Pandemic. Group Processes & Intergroup Relations. 2020; 25(1): 106–121. [Google Scholar]
- 8.Forsyth DR. Group-level resistance to health mandates during the COVID-19 pandemic: A groupthink approach. Group Dynam: Theory, Research, and Practice. 2020; 24(3): 139-152. [Google Scholar]
- 9.Marmarosh CL, Forsyth DR, Strauss B, Burlingame GM. The psychology of the COVID-19 pandemic: A group-level perspective. Group Dynam: Theory, Research, and Practice. 2020; 24: 122-138. [Google Scholar]
- 10.Islam MS, Sarkar T, Khan SH, et al. COVID-19-related infodemic and its impact on public health: A global social media analysis. Am J Trop Med Hyg. 2020; 103(4): 1621-1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guidry JP, Jin Y, Orr CA, Messner M, Meganck S. Ebola on instagram and twitter: How health organizations address the health crisis in their social media engagement. Publ Relat Rev. 2017; 43(3): 477-486. [Google Scholar]
- 12.Reynolds BJ. When the facts are just not enough: Credibly communicating about risk is riskier when emotions run high and time is short. Toxicol Appl Pharmacol. 2011; 254(2): 206-214. [DOI] [PubMed] [Google Scholar]
- 13.Kreuter MW, Green MC, Cappella JN, et al. Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007; 33(3): 221-235. [DOI] [PubMed] [Google Scholar]
- 14.Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: A conceptual, theoretical, and empirical overview. Health Educ Behav. 2007; 34(5): 777-792. [DOI] [PubMed] [Google Scholar]
- 15.Braddock K, Dillard JP. Meta-analytic evidence for the persuasive effect of narratives on beliefs, attitudes, intentions, and behaviors. Commun Monogr. 2016; 83(4): 446-467. [Google Scholar]
- 16.Ballard AM, Davis A, Hoffner CA. The impact of health narratives on persuasion in African American women: A systematic review and meta-analysis. Health Commun. Mar. 2020; 2: 1-12. [DOI] [PubMed] [Google Scholar]
- 17.Kim HK, Niederdeppe J. Effects of self-affirmation, narratives, and informational messages in reducing unrealistic optimism about alcohol-related problems among college students. Hum Commun Res. 2016; 42(2): 246-268. [Google Scholar]
- 18.Ratcliff CL, Sun Y. Overcoming resistance through narratives: Findings from a meta-analytic review. Hum Commun Res. 2020; 46(4): 412-443. [Google Scholar]
- 19.Shaffer VA, Focella ES, Hathaway A, Scherer LD, Zikmund-Fisher BJ. On the usefulness of narratives: an interdisciplinary review and theoretical model. Ann Behav Med. 2018; 52(5): 429-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gerrie MP, Belcher LE, Garry M. 'Mind the gap’: False memories for missing aspects of an event. Appl Cognit Psychol. 2006; 20(5): 689-696. [Google Scholar]
- 21.Johnson HM, Seifert CM. Sources of the continued influence effect: When misinformation in memory affects later inferences. J Exp Psychol Learn Mem Cognit. 1994; 20(6): 1420-1436. [Google Scholar]
- 22.Cappella JN, Maloney E, Ophir Y, Brennan E. Interventions to correct misinformation about tobacco products. Tob Regul Sci. Jul. 2015; 1(2): 186-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bekalu MA, Bigman CA, McCloud RF, Lin LK, Viswanath K. The relative persuasiveness of narrative versus non-narrative health messages in public health emergency communication: Evidence from a field experiment. Prev Med. 2018; 111: 284-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuru O, Stecula D, Lu H, et al. The effects of scientific messages and narratives about vaccination. PLoS One. 2021; 16(3): e0248328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jarreau PB, Su LYF, Chiang ECL, et al. COVID issue: Visual narratives about COVID-19 improve message accessibility, self-efficacy, and health precautions. Frontiers in Communication. 2021; 6: 164. [Google Scholar]
- 26.Buhrmester M, Kwang T, Gosling SD. Amazon's mechanical turk: A new source of inexpensive, yet high-quality, data? Perspect Psychol Sci. 2011; 6(1): 3-5. [DOI] [PubMed] [Google Scholar]
- 27.Jeong M, Zhang D, Morgan JC, et al. Similarities and differences in tobacco control research findings from convenience and probability samples. Ann Behav Med. 2019; 53(5): 476-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amazon Mechanical Turk . FAQ. Available at: https://www.mturk.com/worker/help [Google Scholar]
- 29.Litman L. New Solutions Dramatically Improve Research Data Quality on MTurk. n.d.
- 30.Pew Research Center . 2020. Pew Research Center's American Trends Panel Wave 67. Available at: https://www.pewresearch.org/science/wp-content/uploads/sites/16/2020/05/PS_2020.05.21_trust-in-scientists_TOPLINE.pdf https://www.pewresearch.org/science/wp-content/uploads/sites/16/2020/05/PS_2020.05.21_trust-in-scientists_TOPLINE.pdf. [Google Scholar]
- 31.Larson HJ, de Figueiredo A, Xiahong Z, et al. The state of vaccine confidence 2016: Global insights through a 67-country survey. E Bio Medicine. 2016; 12: 295-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Altman DG. Covariate Imbalance, Adjustment for. Encyclopedia of Biostatistics; 2005. [Google Scholar]
- 33.Noar SM, Austin L. (Mis) communicating about COVID-19: Insights from health and crisis communication. Health communication. 2020; 35: 1-5. [DOI] [PubMed] [Google Scholar]
- 34.Bode L, Vraga EK. In related news, that was wrong: The correction of misinformation through related stories functionality in social media. J Commun. 2015; 65(4): 619-638. [Google Scholar]
- 35.Slater MD, Rouner D. Value-affirmative and value-protective processing of alcohol education messages that include statistical evidence or anecdotes. Commun Res. 1996; 23(2): 210-235. [Google Scholar]
- 36.Merchant RM, South EC, Lurie N. Public health messaging in an era of social media. JAMA. 2021; 29: 223-224. [DOI] [PubMed] [Google Scholar]
- 37.Burki T. The online anti-vaccine movement in the age of COVID-19. The Lancet Digital Health. 2020; 2(10): e504-e505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goldberg MH, Gustafson A, Maibach EW, et al. Social norms motivate COVID-19 preventive behaviors. Preprint. 2020; 5. [Google Scholar]
- 39.Kaiser Family Foundation . KFF COVID-19 Vaccine Monitor: October 2021. 2021. Available at: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-october-2021/ [Google Scholar]
- 40.Gesser-Edelsburg A. Using narrative evidence to convey health information on social media: The case of COVID-19. J Med Internet Res. 2021; 23(3): e24948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hurst K, Stern MJ. Messaging for environmental action: The role of moral framing and message source. J Environ Psychol. 2020; 68: 101394. [Google Scholar]
- 42.Rossen I, Hurlstone MJ, Dunlop PD, Lawrence C. Accepters, fence sitters, or rejecters: Moral profiles of vaccination attitudes. Soc Sci Med. 2019; 224: 23-27. [DOI] [PubMed] [Google Scholar]
- 43.Knowles H, Gowen A, Mark J. Doctors dismayed by patients who fear coronavirus vaccines but clamor for unproven ivermectin. Available at: https://www.washingtonpost.com/health/2021/09/01/ivermectin-covid-treatment/https://www.washingtonpost.com/health/2021/09/01/ivermectin-covid-treatment/ [Google Scholar]
- 44.Nan X, Iles IA, Yang B, Ma Z. Public health messaging during the COVID-19 pandemic and beyond: Lessons from communication science. Health Commun. 2021; 37: 1-19. [DOI] [PubMed] [Google Scholar]
- 45.Appel M, Richter T. Persuasive effects of fictional narratives increase over time. Media Psychol. 2007; 10(1): 113-134. [Google Scholar]
- 46.Prentice DA, Miller DT. When small effects are impressive. Psychol Bull. 1992; 112(1): 160-164. [Google Scholar]
- 47.Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet (London, England). 2010; 376(9748): 1261-1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chandler J, Rosenzweig C, Moss AJ, Robinson J, Litman L. Online panels in social science research: Expanding sampling methods beyond mechanical Turk. Behav Res Methods. 2019; 51(5): 2022-2038. [DOI] [PMC free article] [PubMed] [Google Scholar]