Abstract
Frail older hospital patients are susceptible to malnutrition and iatrogenic sarcopenia. This can be linked to the decreased appetite and oral intake that can arise in largely bed-bound patients who do not get up even for rehabilitation and meals. The KT index was devised as an easy-to-use evaluation tool to address oral intake issues, and it has potential utility for expediting a multidisciplinary comprehensive rehabilitation program. To our knowledge, no reports have described real-world evidence on multidisciplinary team interventions with this tool. Herein, we report the case of a frail older patient whose oral intake improved following a KT Index-based intervention.
Keywords: KT index, oral intake, malnutrition, iatrogenic sarcopenia, case report of frail older adult
Introduction
Frail older patients often experience falls and aspiration pneumonia, and thus tend to be instructed to rest in bed or receive inappropriate nutritional care, such as nil per os (NPO) or parenteral peripheral nutrition (PPN), making them susceptible to activity- and nutrition-related iatrogenic sarcopenia (Nagano et al., 2019). Iatrogenic sarcopenia may in turn contribute to decreased activities of daily living (ADLs) and consequent decreased appetite and meal consumption. At our hospital, we encounter many frail older patients with decreased ADLs and low body mass index (BMI), who spend most of the day in their beds and do not ambulate or leave their beds for rehabilitation or meals. They consume little of their hospital-provided diet orally, which leads to further weight loss and delayed discharge. As a nutritional support team (NST), our objective is to devise interventions to arrest and reverse this negative spiral. Herein, we report one such case where an intervention based on an oral intake balance chart—the KT index—yielded a favorable outcome.
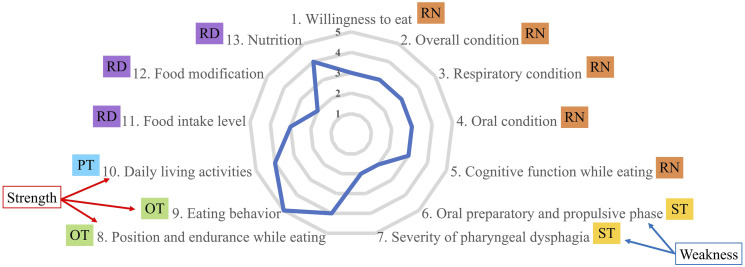
The KT index is a comprehensive evaluation tool for oral intake ability, developed by Japanese health professionals (the term “KT” is derived from the Japanese expression kuchi kara taberu, meaning eat by mouth) (Koyama, 2015). It has validated utility for multidisciplinary rehabilitation aimed at ameliorating low oral intake issues, and it is available in an English version (Maeda et al., 2016). The KT index is an easy-to-use balance chart dividing factors encompassing oral intake ability into 13 categories, thus allowing the strengths and weaknesses of food-eating ability to be identified for the individual patient (Figure 1). Based on these identified strengths and weaknesses, health professionals can design individually tailored multidisciplinary rehabilitation programs to improve oral intake.
Figure 1.
Evaluation of oral intake ability with the KT index. Note. Example of the KT index balance chart showing strengths and weaknesses. RN responsible for 1–5; ST for 6–7; OT for 8–9; PT for 10; and RD for 11–-13 (in our hospital). RN = registered nurse. ST = speech-language-hearing therapist. OT = occupational therapist. PT = physical therapist. RD = registered dietitian. FIM = functional Independence Measure.
Previous reports on the KT index are about its validation as an evaluation tool and its application as a solely nursing care intervention. No previous report has described its clinical application as part of a multidisciplinary approach. Accordingly, in this case report, we present real-world evidence on the efficacy of the KT index as the basis for a team medicine intervention for a frail older patient with malnutrition and suspected iatrogenic sarcopenia.
Case presentation
Patient Profile
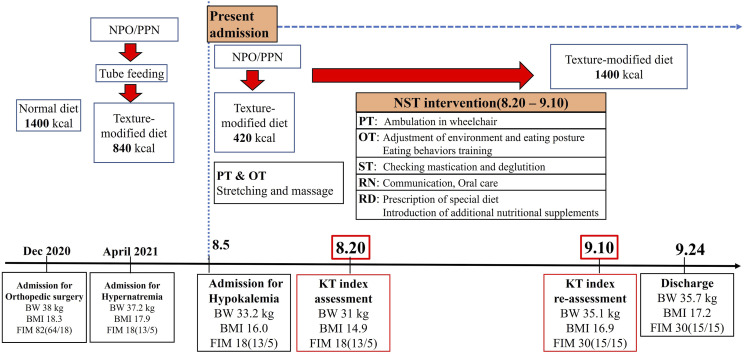
The patient in this case was an 87-year-old woman residing at home with her family (although moving to a nursing home was under consideration due to decreased ADLs and signs of cognitive decline). She had been diagnosed with osteoporosis and Alzheimer’s disease, had a history of thoracic compression and left patellar fracture, and had undergone surgery for right humeral and left trochanteric fracture. Her clinical course is represented on a timeline (Figure 2). When she was admitted for orthopedic surgery in December 2020, her body weight (BW) was 38 kg, BMI was 18.3 kg/m2, and total Functional Independence Measure (FIM) was 82 (motor 64/cognitive 18) points. The patient was provided with normal diet; however, when she was admitted for hypernatremia in April 2021, she required NPO/PPN, enteral nutrition, and a texture-modified diet, and showed decreased BW, BMI and FIM.
Figure 2.
Timeline of events and interventions. Note. NPO = nil per os. PPN = peripheral parenteral nutrition. PT = physical therapist. OT = occupational therapist. ST = speech-language-hearing therapist. RN = registered nurse. RD = registered dietitian. FIM = functional Independence Measure.
Her present admission for hypokalemia occurred on August 5, 2021. Her biometrics and ADL showed further decline at this point, with BW at 33.2 kg, BMI at 16.0 kg/m2, and FIM at 18 (13/5) points. After a period of management with NPO/PPN, oral intake was resumed, and she was provided with a texture-modified diet. However, she continued to show persistent BW and BMI loss and low oral intake, and her attending physician requested the NST intervention on her 15th day of hospitalization.
Assessment and Diagnosis
Before the NST intervention, the patient was 144 cm tall, weighed 31 kg, and had a BMI of 14.9 kg/m2. Her ADLs were evaluated using FIM (total [motor/cognitive]), and she scored 18 (13/5) points. Her feeding status was rated as Functional Oral Intake Scale (FOIS) level 5, suggesting relatively functional mastication and deglutition. Consequently, her diet was texture-modified. Her oral intake amounted to 420 kcal/day (9 kcal/kg ideal BW [IBW]/day), and her laboratory data (albumin: 3.3 g/dL, C reactive protein: 0.84 mg/dL, and white blood cell count: 5370/dL) showed no signs of inflammation. The patient was diagnosed with severe/stage 2 malnutrition using the Global Leadership Initiative on Malnutrition criteria (Mini Nutritional Assessment-Short Form, three points; weight loss, 24.8%/6 months; BMI, 14.9 kg/m2; reduced muscle mass [calf circumference 22 cm], reduced energy intake [only 30% of the provided nutrition was consumed over a 1-week period]) (Cederholm et al., 2019). Iatrogenic sarcopenia was suspected, based on the Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment community setting criteria (calf circumference, 22 cm; SARC-F score, eight points; grip strength, 2 kg) (Chen et al., 2020).
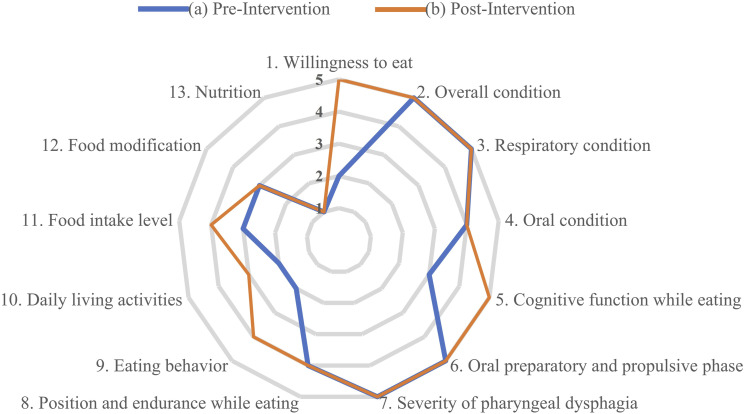
The KT index evaluation demonstrated that her oral intake ability was characterized by good chewing and swallowing function as strengths and lack of appetite, decreased daily living activities, and poor eating behavior as weaknesses (Figure 3a). The graders of the KT index were registered nurses and rehabilitation stuff who had been attending to the patient.
Figure 3.
Pre-and post-intervention KT index. (a) pre-intervention, (b) post-intervention.
Intervention
A meeting was conducted with our hospital NST, which was composed of a physician, physical therapist (PT), occupational therapist (OT), speech-language-hearing therapist (ST), registered dietician (RD), registered nurse (RN), and pharmacist, and an intervention was planned; it was executed over the subsequent 3-week period. Specifically, the interventional strategy was based on the strengths and weaknesses shown by the KT index and aimed to maintain her chewing and swallowing function, boost her daily activity level to increase her daytime awareness and in turn, her willingness to eat, and provide a favorable environment where she could eat without difficulty. To describe the intervention in detail, the PT moved the patient in a wheelchair every day with full assistance, taking her out of her room to increase cognitive, motor, and sensory stimulation. The OT adjusted the patient’s eating environment (adjusting the table’s height and position) and eating posture (adding cushions and towels under her body) and trained her to use eating utensils, as eating behavior rehabilitation. The ST checked the patient’s mastication and deglutition. The RN conversed more frequently with the patient and provided oral care. The RD provided nutritional support by prescribing a special diet and introducing additional oral nutritional supplements. Finally, the outcome of the intervention was evaluated at the end of the 3-week intervention period, when the KT index was evaluated again to re-assess her oral intake function.
Outcome
The post-intervention KT index is presented in Figure 3b. The patient’s appetite, eating behavior, and daily living activities improved after the intervention, and oral intake function was maintained. The improvement seen in the KT index results was reflected in contemporaneous biometrics evaluation results, with improved ADLs and oral intake as shown in Table 1. Her BW and BMI were increased at the 3-week stage, and the improvement in FIM represented a 10-point increase in the cognitive score. Her FOIS level was unchanged. Her oral intake increased from a pre-intervention average of 420 kcal/day (9 kcal/kg IBW/day) to a post-intervention average of 1400 kcal/day (31 kcal/kg IBW/day).
Table 1.
Pre-and Post-Intervention Biometrics, Activities of Daily Living, and Oral Intake Change.
| Pre-Intervention | Post-Intervention | |
|---|---|---|
| BW (kg) | 31 | 35.1 |
| BMI (kg/m2) | 14.9 | 16.9 |
| FIM Total (motor/cognitive) | 18 (13/5) | 30 (15/15) |
| FOIS (level) | 5 | 5 |
| Oral intake (kcal/day) | 420 | 1400 |
Note. ADLs = Activities of Daily Living. FIM=Functional Independence Measure; FOIS = Functional Oral Intake Scale.
Discussion
To the best of our knowledge, this case report represents the first real-world evidence on the KT index as a multidisciplinary rehabilitation intervention aimed to improve oral intake in a frail older patient. The patient in this case showed a significant improvement over the 3-week period following the first KT index assessment of her oral intake and the consequently planned intervention.
Prior to this intervention, the patient showed poor oral intake with continuous weight loss following an NPO/PPN regimen, despite receiving almost fully assisted care during her meals. Furthermore, the patient was bedridden on admission; thus, her rehabilitation was mostly provided to her while being bed-bound, and she showed no interest in leaving her room. Further possible sequelae included malnutrition and nutrition- and activity-related iatrogenic sarcopenia. Following the NST intervention, the patient actively requested fully assisted wheelchair trips outside of her room, which increased her daytime awareness level and communication; this was also reflected in her increased cognitive-FIM. Gradually, she began to show a willingness to eat. Adjusting her eating posture and environment were also effective in weaning her from dependence on a high level of care during mealtimes. By the end of the 3-week multidisciplinary intervention based on the KT index, she had recovered the ability to sit in a stable position in her wheelchair and eat full servings of hospital meals without any assistance, holding her crockery and utensils independently; thus, her BW and BMI increased. NST members also observed that the patient would frequently initiate conversation with medical staff or other patients, participate in handicraft activities, and show signs of positive emotion such as smiling, which were things she could not do before the intervention.
The KT index was validated as an evaluation tool in a previous study (Maeda et al., 2016). In that study, all 13 items were demonstrated to be necessary and sufficient for component assessment, and the total KT index score was shown to correlate significantly with the result of other relevant evaluation measures, such as the FOIS, Barthel Index, Mini Nutritional Assessment-Short Form, and Cognitive Performance Scale. A historical control study conducted in a rehabilitation hospital showed that the KT index improved nutrition-related factors, such as BW and oral intake (kcal), along with ADL (FIM) and discharge rate (Waza et al., 2019). A similar outcome was seen in the present case: the patient experienced improved BW, oral intake (kcal), and ADL, which enabled her to return home. A case series reported the benefits of comprehensive nursing care using the KT index to improve the oral intake of three geriatric patients who had undergone gastrostomy (Aruga et al., 2018). Those patients were encouraged not to eat; however, a resumption of oral eating improved their QOL. However, the authors of that case series stated that nursing care alone was insufficient to effect improvement; other professional assistance—especially to address physical problems, such as position and endurance while eating, and eating behavior—was required. In the present case study, the patient was able to regain oral eating ability and thus her QOL also increased. We consider that provision of rehabilitation by a multidisciplinary team determined through evaluation with the KT index was a key factor in achieving improved oral intake.
Conclusion
The KT index is a comprehensive oral eating evaluation tool allowing health care professionals to focus not only on the chewing and swallowing functions, but also on daily activity, and eating posture and behavior, items which can be neglected when using other evaluation tools.
We suggest that the KT index is a promising tool for addressing oral intake issues in older patients and can expedite comprehensive multidisciplinary rehabilitation tailored for the individual patient. Further investigations are required to fully verify the efficacy of the KT index in multidisciplinary efforts to improve the oral intake of older patients.
Acknowledgments
We would like to thank members of the Nutrition Support Team at Tanegashima Medical Center for their dedication to their work of improving patients' nutritional statuses. We also would like to thank Dr. Sonshin Takao, Director of the Tanegashima Medical Center for suggestive comments and support for ensuring a scientifically sound manuscript, and Henry Smith, Associate Professor, Joint Faculty of Veterinary Medicine, Kagoshima University for assistance with English editing.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical Approval: The Tanegashima Μedical Center Institutional Review Board approved the study protocol: # R3-46.
Informed Consent: The study and intention to publish were thoroughly explained to the patient and her family, and written informed consent was provided for participation in the NST intervention and study.
ORCID iD
Yoshifumi Hidaka https://orcid.org/0000-0002-5015-9242
References
- Aruga Y., Saito A., Aoki Y. (2018). Nursing care using KT (Kuchi-kara Taberu) index radar chart enabling elderly patients with dysphagia to live like human beings after initiating gastrostomy feeding. Proceedings of Singapore Healthcare, 27(2), 136–138. 10.1177/2010105817740374 [DOI] [Google Scholar]
- Cederholm T., Jensen G. L., Correia M. I. T. D., Gonzalez M. C., Fukushima R., Higashiguchi T., Baptista G., Barazzoni R., Blaauw R., Coats A., Crivelli A., Evans D. C., Gramlich L., Fuchs-Tarlovsky V., Keller H., Llido L., Malone A., Mogensen K. M., Morley J. E., Compher C. (2019). GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clinical Nutrition (Edinburgh, Scotland), 38(1), 1–9. 10.1016/j.clnu.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Chen L. K., Woo J., Assantachai P., Auyeung T. W., Chou M. Y., Iijima K., Jang H. C., Kang L., Kim M., Kim S., Kojima T., Kuzuya M., Lee J. S. W., Lee S. Y., Lee W. J., Lee Y., Liang C. K., Lim J. Y., Lim W. S., Arai H. (2020). Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. Journal of the American Medical Directors Association, 21(3), 300–307. 10.1016/j.jamda.2019.12.012 [DOI] [PubMed] [Google Scholar]
- Koyama T. (2015). The comprehensive skill to support pleasure of oral intake of food: Application of KT balance chart and help. Igaku Shoin; (in Japanese). [Google Scholar]
- Maeda K., Shamoto H., Wakabayashi H., Enomoto J., Takeichi M., Koyama T. (2016). Reliability and validity of a simplified comprehensive assessment tool for feeding support: Kuchi-kara taberu index. Journal of the American Geriatrics Society, 64(12), e248–e252. 10.1111/jgs.14508 [DOI] [PubMed] [Google Scholar]
- Nagano A., Nishioka S., Wakabayashi H. (2019). Rehabilitation nutrition for iatrogenic sarcopenia and sarcopenic dysphagia. The Journal of Nutrition, Health & Aging, 23(3), 256–265. 10.1007/s12603-018-1150-1 [DOI] [PubMed] [Google Scholar]
- Waza M., Maeda K., Katsuragawa C., Sugita A., Tanaka R., Ohtsuka A., Matsui T., Kitagawa K., Kishimoto T., Fukui H., Kawai K., Yamamoto M., Isono M. (2019). Comprehensive tool to assess oral feeding support for functional recovery in post-acute rehabilitation. Journal of the American Medical Directors Association, 20(4), 426–431. 10.1016/j.jamda.2018.10.022 [DOI] [PubMed] [Google Scholar]