1. Introduction
The development of persistent pain symptoms can impose a range of cognitive and physical limitations that prevent an individual from participating in long-established routines, valued vocational, and recreational activities.6 Often these activities provide the individual with a sense of meaning and purpose, as well as forming a central element of their identity.31 However, what happens when an individual suffering from persistent pain continues to persevere towards highly valued life goals that, despite their best efforts, are no longer achievable?
Traditionally, the idea of relinquishing important life goals has been seen as an undesirable response to difficulties. However, a growing body of evidence4,27,37,38 suggests that the tenacious pursuit of untenable goals can result in a raft of negative consequences for an individual's long-term psychological adjustment. In this review, we argue that the dilemma of knowing when to persist towards important life goals, and knowing when to disengage from such goals to pursue more viable alternatives, is a central but rarely discussed challenge facing many people with chronic pain.
2. Conceptual understanding of the problem and empirical background
2.1. The perils of tenacious goal pursuit in chronic pain
The chronic pain literature recognises several common scenarios where a dogged tenacity to pursue important but no longer achievable goals can lead to a range of maladaptive behaviours and negative psychological consequences.3
Perhaps the most familiar expression of the counterproductive effects of tenacious goal pursuit in people with chronic pain is referred to as “unhelpful cure-seeking behaviours”7 or “unviable pain control behaviours.”8 Although it is reasonable to seek a medical solution to a pain condition when it first appears, repeated failed procedures and treatments over many months and years can lead to a debilitating cycle of counterproductive help-seeking behaviour. This can in turn result in increased frustration and feelings of hopelessness.10 Indeed, in some cases, this form of tenacious goal pursuit can lead to seeking out increasingly risky and unsuitable medical procedures17,21 or increasing dependence on potentially harmful analgesic medications.22 These negative repercussions are well understood within the clinical literature, as noted by Crombez et al.:
“A slavish fidelity to a misguided agenda for control over pain may inadvertently exacerbate distress and disability, and occlude opportunities for engagement with other valued activities of life.”8 [p. 631].
Another commonly seen clinical presentation where rigid and tenacious goal pursuit can lead to maladaptive outcomes is the plight of many injured workers who attempt to return to previous employment positions and roles. Aside from the financial benefits, the desire to return to a previous employment role is understandable considering that significant personal resources, time, and effort have often been devoted to developing skills and qualifications to perform a particular job. Employment is also a key factor in determining self-worth, social affiliation, and sense of purpose.13,15
Nevertheless, it is also true that the physical or cognitive demands of previous work duties can make it impossible to return to a previous role. Here the individual's own motivation, often stoked by the external pressures from insurance companies and vocational rehabilitation providers, can lead to a cycle of failed return to work attempts, followed by a raft of negative psychological consequences.25 In addition to a sense of failure, shame, and hopelessness, the continued pursuit of unfeasible vocational plans can undermine attempts to apply pain management strategies, such as pacing activities, or even block opportunities for vocational retraining. External pressure to pursue unviable return to work goals can also result in strong feelings of coercion and injustice, adding layers of distress and mistrust to an already emotionally challenging situation.
Although these represent just 2 of many related presentations, it is our contention that the dilemma of knowing when to persist and when to let go of important life ambitions has received relatively limited attention in the pain management literature. This review highlights the importance of fostering flexible goal adjustment when managing the functional limitations associated with chronic pain and explores the clinical implications of failing to recognise this dilemma in planning treatment protocols for chronic pain.
3. Theoretical models of goal adjustment
We would like to introduce 2 theoretical perspectives that recognise the importance of flexible goal adjustment that have received considerable attention in the broader psychological literature.
3.1. Goal Adjustment Model
The Goal Adjustment Model39 suggests that in circumstances where important life goals become unviable, the optimal response requires 2 related psychological processes: the process of disengaging from the unviable goals, followed by the process of reengaging with alternative but viable goals. The capacity to enact this 2-stage process is referred to as the individual's capacity for goal adjustment.33
A large number of studies have demonstrated that a greater capacity for goal disengagement is an important predictor of a range of positive physical health outcomes when an individual is faced with a devastating life event.34–37 Furthermore, although goal reengagement capacity was significantly predictive of well-being, only an increased disposition towards goal disengagement was associated with improved physical health.38
In explaining these findings, the goal adjustment theory by Wrosch et al.38 proposes that the capacity for goal disengagement both directly and indirectly (through ameliorating the negative psychological consequences of failed efforts to succeed) leads to an improved capacity for goal reengagement, which in turn bolsters well-being and consequent psychological adjustment (Fig. 1).
Figure 1.
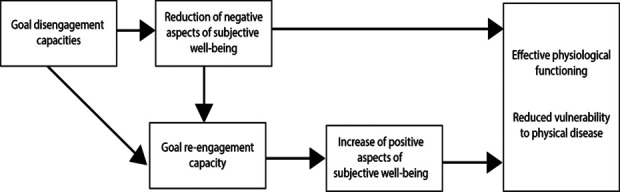
Theoretical model predicting psychological and health-related benefits of goal adjustment capacities. Model adapted from Wrosch C, Scheier MF, Miller EG. Goal adjustment capacities, subjective well-being and physical health. Soc Pers Psychol Compass 2013;7:847–860, with permission.
3.2. Dual-Process Model of Goal Adjustment
The Dual-Process Model of Goal Adjustment suggests there are 2 self-regulation–coping orientations in response to a significant change in functioning,5 such as the development of chronic pain, termed the Assimilative Mode and the Accommodative Mode (Fig. 2). The Assimilative Mode reflects a tenacious goal pursuit approach and is defined as “a persistent effort to actively adjust life circumstances to one's preferences”3 [p. 431]. The Accommodative Mode is associated with flexible goal adjustment and is defined as the “processes whereby personal goals and frames of self-evaluation are adjusted to situational constraints.”3
Figure 2.
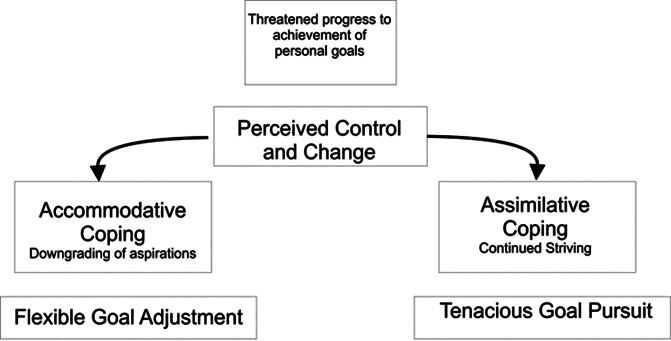
Dual-Process Model of Coping. Model adapted from Schmitz U, Saile H, Nilges P. Coping with chronic pain: flexible goal adjustment as an interactive buffer against pain related distress. PAIN 1996;67:41–51, with permission.
The Dual-Process Model proposes that where goals are viable, the Assimilative Mode of coping is optimal to maximise the chances of success. However, where the goal is unviable, the most adaptive response involves a shift from a predominantly Assimilative to an Accommodative coping mode. Failure to switch coping modes in circumstances where important life goals are no longer viable can produce feelings of helplessness and depression.18,28
4. Goal adjustment and chronic pain
Despite these 2 models of goal adjustment having been applied to various chronic health conditions, the underlying tenants have seen only limited application in chronic pain research.1,2,14,26,28 Schmitz et al.28 evaluated the Accommodation and Assimilation modes of coping with respect to pain-specific coping strategies in a sample of 120 patients with chronic pain. They found that Accommodative coping provided a “protective resource” which resulted in less negative psychological symptoms and higher “positive life perspective” than the Assimilative Mode.28 Furthermore, although high scores on both Assimilation and Accommodation orientations were correlated with lower levels of depression and disability, only the Accommodative Mode predicted better pain outcomes after accounting for other pain-specific active coping strategies.
However, other investigations have not supported goal disengagement as advantageous for psychological adjustment to pain. Two studies by Arends et al.,1,2 which combined the Dual-Process and Goal Adjustment models found that although goal reengagement was positively related to better psychological health in people with arthritis pain, goal disengagement was negatively correlated with adjustment.
Similarly, Ramirez-Maestre et al.26 found that goal disengagement was associated with higher rates of negative rumination and decreased optimism, as well as a decreased likelihood of reengaging in alternative goals. These authors suggested that goal disengagement in the context of chronic pain may be a form of avoidance as described by the fear-avoidance model of pain.9 It may be that an unwillingness to disengage from certain practical goals could reflect the pursuit of important affective avoidance goals, such as avoiding a sense of failure, shame, and grief.
The theoretical distinction between effort vs commitment towards goal achievement can also shed light on these apparently contradictory findings. Goal adjustment theory37 suggests that goal disengagement involves 2 distinct processes (Fig. 3), namely, a reduction of effort in the pursuit of the goal as well as the relinquishment of desire or commitment towards the goal. Both a reduction of effort and a relinquishing of commitment are required to reorientate psychological resources towards alternative achievable goals. Unfortunately, none of the studies examining goal adjustment in chronic pain have assessed these processes independently. Hence, people living with chronic pain may cease making effort towards unviable goals but struggle to relinquish their commitment or aspiration to return to these goals. This distinction would explain the positive association between rumination and goal disengagement previously mentioned.32
Figure 3.
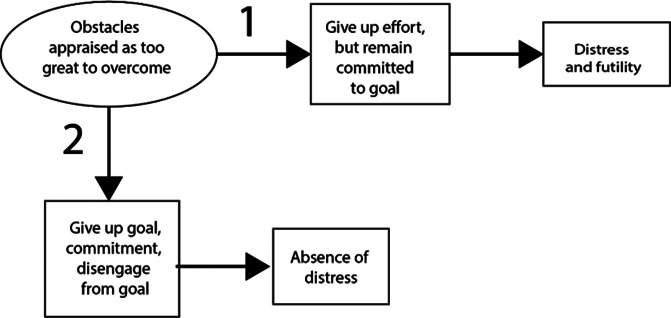
Two aspects of goal disengagement in response to the perception that a goal is unattainable. Model from Wrosch C, Scheier MF, Carver CS, Schulz R. The importance of goal disengagement in adaptive self-regulation: when giving up is beneficial. Self Identity 2003;2:1–20, with permission.
5. Clinical implications
Goal setting forms a key element of most psychological programs for chronic pain. The SMART goal-setting protocol is a widely used and empirically supported intervention used in pain management programs12,24,29 as well as in other psychological interventions.11 While the SMART goal protocol recognises the importance of setting “achievable”and “realistic” goals, the focus of this intervention is on goal setting. The SMART goal-setting protocol does not explicitly recognise the critical step of goal disengagement, as identified in the Goal Adjustment Model.39 In clinical practice, we anticipate experienced clinicians will use the SMART goal protocol in accord with the Goal Adjustment Model 2-stage process, as they review the results of behavioural experiments and other homework assignments on an iterative, problem-solving basis and raise considerations of goal viability as part of those reviews. However, without the protocol identifying goal disengagement as a necessary component of the goal-setting process, there is a risk that patients will fail to relinquish both effort and commitment towards the unviable goal and hence do not reorient available psychological resources towards setting viable SMART goals.
The conceptual resemblance between the notion of flexible goal adjustment and the construct of acceptance has led some researchers to suggest that these terms may be interchangeable. Indeed, the therapeutic approach known as Acceptance Commitment Therapy (ACT16) and the underlying model of psychological flexibility provide a useful framework in which to promote flexible goal adjustment.
The ACT approach introduces a range of terminologies and therapeutic techniques designed to recognise unproductive efforts towards unviable control strategies to encourage more flexible behavioural responses. For example, the therapeutic techniques designed to induce “creative hopelessness”20 or the application of the “pragmatic truth criterion” are a useful framework in which to assist individuals assess the “unworkable” nature of their efforts pursuing unviable goals22 and find alternative goals which remain in accordance with their values. By emphasising higher order values, as opposed to a focus on specific goals, ACT provides a more flexible approach to goal setting. In this way, the model is consistent with the principles of goal disengagement and goal reengagement as advocated by the goal adjustment literature.3,30 However, the assessment of the application of ACT within a chronic pain setting has tended to emphasise the idea of acceptance as it relates specifically to the experience of pain, referred to as a “willingness to accept pain.”32 Although in practice, many ACT practitioners will apply the principles of psychological flexibility to a range of untenable goal pursuit behaviours, studies investigating acceptance from a chronic pain perspective have often relied on the narrower definition of this term as it applies to the willingness to accept the experience of pain. For example, a widely used measure of acceptance in chronic pain research,19,30 the Chronic Pain Acceptance Questionnaire (CPAQ, 27) includes items such as “I kept doing what I was doing without letting pain stop me” and “I did what works best for my goals in life regardless of what I was thinking or feeling at the time.”23 Here, acceptance of pain seems to imply inflexible goal pursuit, in which an individual continues to pursue important life goals in spite of their pain. Equally the CPAQ does not contain any items which assess readiness to relinquish or accept that previously held life goals may no longer be viable. As such, we would argue that the CPAQ does not accurately convey the ACT model of acceptance as it applies to broader life goals and there is a risk that it “sends the wrong signals” in terms of optimal goal pursuit.
Perhaps one reason for the lack of clinical protocols in the chronic pain literature specifically relating to flexible goal adjustment is the fact that it is often unclear, at least in the early phases of recovery, whether someone with a persistent pain condition may be able to eventually achieve many of their long-held goals. Unlike catastrophic injuries and conditions such as spinal cord injury, where ambulatory goals are unlikely to be entertained although very much desired, people suffering from chronic pain can make substantial progress towards achieving many preexisting goals despite continuing to experience pain. Hence, how is it determined that a goal is no longer viable? There is of course no established method for this, but 2 factors seem to be most salient here: there have been repeated unsuccessful attempts to achieve the goal and the efforts to achieve the goal have significant negative repercussions to the individual. Providing the patient with important information about flexible goal adjustment at the outset of treatment (such as the 2-stage model and the effort and commitment components of goal disengagement) may help to prevent tenacious goal pursuit from occurring in the first place. Nevertheless, research is needed to investigate how goal viability is determined and how best to facilitate flexible goal adjustment in chronic pain.
6. Conclusion
The benefits of setting goals and encouraging individuals with chronic pain to pursue important life objectives are well established in the empirical literature.24 Although ACT provides a useful therapeutic framework to discuss the unworkability of pursing unviable goal of pain reduction, the broader literature in chronic pain is relatively silent on the subject of disengaging from unviable important life goals beyond simply reducing pain symptoms.
More than 60 years of research on the Goal Adjustment Model and the Dual-Process Model of Assimilative and Accommodative Coping has revealed the advantages of disengagement from unviable goals and the adoption of flexible goal adjustment leading to better outcomes for people living with chronic illness.
We are calling for a greater focus on the goal pursuit dilemma facing many of our patients. Knowing when to persist and when to pivot away from important but no longer viable goals, to reengage in alternative goal options that are still consistent with that individual's values, can be one of the most challenging issues raised in treatment of chronic pain. Research is needed to understand the psychological factors underpinning flexible goal adjustment to develop effective clinical interventions that can assist people with chronic pain to make their best life choices.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Lawrence Roux, Email: Lawrence.Roux@student.uts.edu.au.
Sylvia M. Gustin, Email: s.gustin@unsw.edu.au.
References
- [1].Arends RY, Bode C, Taal E, Van de Laar MA. The role of goal management for successful adaptation to arthritis. Patient Educ Couns 2013;93:130–8. [DOI] [PubMed] [Google Scholar]
- [2].Arends RY, Bode C, Taal E, van de Laar MA. The longitudinal relation between patterns of goal management and psychological health in people with arthritis: the need for adaptive flexibility. Br J Health Psychol 2016;21:469–89. [DOI] [PubMed] [Google Scholar]
- [3].Bailly N, Joulain M, Herve C, Alaphilippe D. Coping with negative life events in old age: the role of tenacious goal pursuit and flexible goal adjustment. Aging Ment Health 2012;16:431–7. [DOI] [PubMed] [Google Scholar]
- [4].Brandstätter V, Herrmann M, Schüler J. The struggle of giving up personal goals: affective, physiological, and cognitive consequences of an action crisis. Personal Soc Psychol Bull 2013;39:1668–82. [DOI] [PubMed] [Google Scholar]
- [5].Brandtstädter J, Renner G. Tenacious goal pursuit and flexible goal adjustment: explication and age-related analysis of assimilative and accommodative strategies of coping . Psychol Aging 1990;5:58–67. [DOI] [PubMed] [Google Scholar]
- [6].Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. [DOI] [PubMed] [Google Scholar]
- [7].Clarke KA, Iphofen R. Accepting pain management or seeking pain cure: an exploration of patients' attitudes to chronic pain. Pain Manag Nurs 2007;8:102–10. [DOI] [PubMed] [Google Scholar]
- [8].Crombez G, Eccleston C, De Vlieger P, Van Damme S, De Clercq A. Is it better to have controlled and lost than never to have controlled at all? An experimental investigation of control over pain. PAIN 2008;137:631–9. [DOI] [PubMed] [Google Scholar]
- [9].Crombez G, Eccleston C, Van Damme S, Vlaeyen JW, Karoly P. Fear avoidance model of chronic pain: next generation. Clin J Pain 2012;28:475–83. [DOI] [PubMed] [Google Scholar]
- [10].Du S, Hu Y, Bai Y, Hu L, Dong J, Jin S, Zhang H. Emotional distress correlates among patients with chronic nonspecific low back pain: a hierarchical linear regression analysis. Pain Pract 2019;19:510–21. [DOI] [PubMed] [Google Scholar]
- [11].Epton T, Currie S, Armitage CJ. Unique effects of setting goals on behavior change: systematic review and meta-analysis. J Consulting Clin Psychol 2017;85:1182–98. [DOI] [PubMed] [Google Scholar]
- [12].Filoramo MA. Improving goal setting and goal attainment in patients with chronic noncancer pain. Pain Manag Nurs 2007;8:96–101. [DOI] [PubMed] [Google Scholar]
- [13].Gard G, Sandberg AC. Motivating factors for return to work. Physiother Res Int 1998;3:100–8. [DOI] [PubMed] [Google Scholar]
- [14].Goossens ME, Kindermans HP, Morley SJ, Roelofs J, Verbunt J, Vlaeyen JW. Self-discrepancies in work-related upper extremity pain: relation to emotions and flexible-goal adjustment. Eur J Pain 2010;14:764–70. [DOI] [PubMed] [Google Scholar]
- [15].Griep Y, Kinnunen U, Nätti J, De Cuyper N, Mauno S, Mäkikangas A, De Witte H. The effects of unemployment and perceived job insecurity: a comparison of their association with psychological and somatic complaints, self-rated health and life satisfaction. Int Arch Occup Environ Health 2016;89:147–62. [DOI] [PubMed] [Google Scholar]
- [16].Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press, 1999. [Google Scholar]
- [17].Heinzerling KG. Applying best practice guidelines on chronic pain in clinical practice—treating patients who suffer from pain and addiction. In: Danovitch I, Mooney LJ, editors. The assessment and treatment of addiction: best practices and new frontiers. Amsterdam: Elsevier, 2019. p. 137–56. [Google Scholar]
- [18].Heyl V, Wahl H-W, Mollenkopf H. Affective well-being in old age. Eur Psychol 2007;12:119–29. [Google Scholar]
- [19].Kim S, Kratz AL. A review of the use and psychometric properties of the chronic pain acceptance questionnaires. Rehabil Psychol 2021;66:102–5. [DOI] [PubMed] [Google Scholar]
- [20].McCracken LM. Learning to live with pain: acceptance of pain predicts adjustment in persons with chronic pain. PAIN 1998;74:21–7. [DOI] [PubMed] [Google Scholar]
- [21].McCracken LM. Acceptance of chronic pain. In: Contextual cognitive-behavioral therapy for chronic pain. Seattle, WA:IASP Press, 2005. p. 61. [Google Scholar]
- [22].McCracken LM, Eccleston C. Coping or acceptance: what to do about chronic pain? PAIN 2003;105:197–204. [DOI] [PubMed] [Google Scholar]
- [23].McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. PAIN 2004;107:159–66. [DOI] [PubMed] [Google Scholar]
- [24].Murphy JL, Rafie S. Develop goals and a treatment plan. In: Chronic pain and opioid management: strategies for integrated treatment. Washington: American Psychological Association, 2021. p. 81–98. [Google Scholar]
- [25].Newton-John TR, McDonald AJ. Pain management in the context of workers compensation: a case study . Translational Behav Med 2012;2:38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ramirez-Maestre C, Esteve R, Lopez-Martinez AE, Serrano-Ibanez ER, Ruiz-Parraga GT, Peters M. Goal adjustment and well-being: the role of optimism in patients with chronic pain. Ann Behav Med 2019;53:597–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Rothermund K. Hanging on and letting go in the pursuit of health goals: psychological mechanisms to cope with a regulatory dilemma. In: De Ridder D and De Wit J. eds. Self-regulation in health behavior. West Sussex, United Kingdom: John Wiley & Sons, 2006. [Google Scholar]
- [28].Schmitz U, Saile H, Nilges P. Coping with chronic pain: flexible goal adjustment as an interactive buffer against pain related distress. PAIN 1996;67:41–51. [DOI] [PubMed] [Google Scholar]
- [29].Tan V, Cheatle MD, Mackin S, Moberg PJ, Esterhai JL, Jr. Goal setting as a predictor of return to work in a population of chronic musculoskeletal pain patients. Int J Neurosci 1997;92:161–70. [DOI] [PubMed] [Google Scholar]
- [30].Vasiliou VS, Karekla M, Michaelides MP, Kasinopoulos O. Construct validity of the G-CPAQ and its mediating role in pain interference and adjustment. Psychol Assess 2018;30:220–30. [DOI] [PubMed] [Google Scholar]
- [31].Vlaeyen JWS, Morley S, Crombez G. The experimental analysis of the interruptive, interfering, and identity-distorting effects of chronic pain. Behav Res Ther 2016;86:23–34. [DOI] [PubMed] [Google Scholar]
- [32].Vowles KE, Johnson LE, Gertz KJ, Jensen MP. Development and preliminary testing of a screening measure of acceptance and willingness in relation to pain, fatigue, and sadness in chronic pain. Clin J Pain 2017;33:160–5. [DOI] [PubMed] [Google Scholar]
- [33].Wrosch C, Amir E, Miller GE. Goal adjustment capacities, coping, and subjective well-being: the sample case of caregiving for a family member with mental illness. J Pers Soc Psychol 2011;100:934–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wrosch C, Miller EG, Scheier MF, de Pontet SB. Giving up on unattainable goals: benefits for health? Pers Soc Psychol Bull 2007;33:251–65. [DOI] [PubMed] [Google Scholar]
- [35].Wrosch C, Miller GE. You've gotta know when to fold 'em: goal disengagement and systemic inflamation in adolescence. Psychol Sci 2007;18:773–7. [DOI] [PubMed] [Google Scholar]
- [36].Wrosch C, Sabiston CM. Goal adjustment, physical and sedentary activity, and well‐being and health among breast cancer survivors. Psychooncology 2013;22:581–9. [DOI] [PubMed] [Google Scholar]
- [37].Wrosch C, Scheier MF, Carver CS, Schulz R. The importance of goal disengagement in adaptive self-regulation: when giving up is beneficial. Self Identity 2003;2:1–20. [Google Scholar]
- [38].Wrosch C, Scheier MF, Miller EG. Goal adjusment capactities, subjective well-being and physical health. Soc Pers Psychol Compass 2013;7:847–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS. Adaptive self-regulation of unattainable goals: goal disengagement, goal reengagement, and subjective well-being. Pers Soc Psychol Bull 2003;29:1494–508. [DOI] [PubMed] [Google Scholar]


