Abstract
Thyroid nodules are very common in the general population. Most are benign and even those that are malignant are typically slow-growing and do not require treatment. Overdiagnosis and overtreatment of thyroid nodules has resulted in significant healthcare costs. ACR TI-RADS was developed to address these concerns, and reduce the number of unnecessary biopsies and follow-up intervals. ACR TI-RADS offers a point-based risk stratification system centered on five sonographic features: consistency, echogenicity, shape, margins and echogenic foci. While the system has noticeable benefits and comparable accuracy with other available risk stratification systems (ATA, EU-TIRADS and K-TIRADS), there are inherent challenges relating to suboptimal inter-reader agreement. In this article, we include 10 educational tips that may be helpful to the ultrasound practitioner for improving the consistency of nodule interpretation with ACR TI-RADS.
Keywords: education, thyroid nodules, thyroid, ultrasound
Introduction
Thyroid nodules are common and are found in up to 68% of patients on US, 25% on CT, and 18% on MRI(1). The prevalence of nodules is higher in females, and it increases with age(1). Nodules are found in 50% of women over 70 years of age, and the female to male ratio is 4 to 1(1). Most nodules are benign and 7–15% are malignant(2). Most malignant nodules are slow-growing and asymptomatic, and do not lead to death if left alone(3). Surgery on these indolent nodules represents overtreatment, increasing patient anxiety and morbidity, while not having a noticeable impact on survival. The increasing utilization of imaging together with refinements in imaging technologies contribute to overdiagnosis of thyroid nodules. Between 2003 and 2007, overdiagnosis was responsible for 70–80% of thyroid cancers in women and 45% in men in the USA(3). The combination of overdiagnosis and overtreatment of thyroid nodules has a profound impact on healthcare economics. In the USA, the estimated total cost of thyroid cancer treatment was $21.6 billion (2010 to 2019) with $4.5 billion attributed to extra costs from increased incidence(1).
The American College of Radiology (ACR) published its Thyroid Imaging Reporting and Data System (TI-RADS) in 2017, an ultrasound-based risk stratification system for thyroid nodule assessment(3). The purpose of TI-RADS was multifactorial: 1) to reduce the number of unnecessary biopsies and excessive surveillance of thyroid nodules, 2) to be able to characterize all nodules, 3) to provide a robust system that can be easily used by all radiologists, irrespective of their level of training or prior experience, and 4) to standardize reporting and provide consistent management recommendations across practices(1,3–5). In ACR TI-RADS, nodules are risk stratified according to five sonographic features including consistency, echogenicity, shape, margins, and echogenic foci (Tab. 1). Each feature is assigned points which are tallied to determine the nodule’s overall risk level (known as the TR level) – this ranges from TR1 (benign) to TR 5 (highly suspicious). The combination of the nodule’s TR level and maximal size will determine recommendations for either biopsy or follow-up (Tab. 2). There are several other risk stratification systems available, such as the American Thyroid Association (ATA) guidelines, the European Thyroid Association Thyroid Imaging Reporting and Data System (EU-TIRADS), and the Korean Society of Thyroid Radiology Thyroid Imaging Reporting and Data System (K-TIRADS). In comparison, ACR-TI-RADS uses a point-based system rather than a pattern-based approach, and adopts a higher size threshold for biopsy, thereby reducing biopsy recommendation rates by 20–47%(6,7). A meta-analysis of 16 studies by Li et al. showed that ACR-TI-RADS had a pooled sensitivity and specificity of 0.89 (95% CI, 0.81–0.93) and 0.70 (95% CI, 0.60–0.78), respectively(2,6). The study also found that ACR-TI-RADS had at least comparable accuracy with other systems. ACR TI-RADS showed no significant differences in sensitivity and specificity versus ATA, while ACR TI-RADS had a significantly higher specificity compared to K-TIRADS, without showing significant differences in sensitivity(2). Koc et al. compared the diagnostic accuracy of ACR TI-RADS, ATA, and EU-TIRADS in detecting thyroid malignancy in 597 nodules that had cytological analysis(8). The authors found an accuracy of 59.9% with ACR TI-RADS, 55.2% with ATA, and 51.3% with EU-TIRADS. The accompanying sensitivities, specificities, and areas under the curve were 48.9%, 60.6% and 0.55 for ACR TI-RADS, 82.2%, 53.5% and 0.74 for ATA, and 86.7%, 49.0% and 0.73 for EU-TIRADS.
Tab. 1.
Five sonographic categories and their corresponding points for ACR TI-RADS(3)
| Composition (choose 1) | Echogenicity (choose 1) | Shape (choose 1) | Margins (choose 1) | Echogenic Foci (choose all that apply) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Cystic or almost completely cystic | 0 | Anechoic | 0 | Wider than tall | 0 | Smooth | 0 | None or large comet-tail artifacts | 0 |
| Spongiform | 0 | Hyperechoic or isoechoic | 1 | Taller than wide | 3 | Ill-defined | 0 | Macrocalcifications | 1 |
| Mixed cystic and solid | 1 | Hypoechoic | 2 | Lobulated or irregular | 2 | Peripheral (rim) calcifications | 2 | ||
| Solid or almost completely solid | 2 | Very hypoechoic | 3 | Extra thyroidal extension | 3 | Punctate echogenic foci | 3 | ||
Tab. 2.
Criteria for FNA or follow-up ultrasound according to ACR TI-RADS(3)
| Add points from all categories to determine TI-RADS level | ||||
|---|---|---|---|---|
| 0 Points | 2 Points | 3 Points | 4 to 6 Points | 7 Points or more |
| TR1 | TR2 | TR3 | TR4 | TR5 |
| Benign | Not suspicious | Mildly suspicious | Moderately suspicious | Highly suspicious |
| No FNA | No FNA | FNA if ≥2.5 cm | FNA if ≥1.5 cm | FNA if ≥1 cm |
| Follow-up if ≥1.5 cm | Follow-up if ≥1 cm | Follow-up if ≥0.5 cm | ||
Despite the benefits of ACR-TI-RADS, there is room for improvement. Hoang et al. noted that variability in management recommendations may continue after implementation of ACR TI-RADS, due to inter-observer differences in assigning sonographic signs(6). This assertion is supported by several studies assessing inter-reader agreement with ACR TI-RADS. In a study involving 180 thyroid nodules that were independently evaluated by four radiologists, fair-to-moderate agreement was found for composition (κ: 0.327–0.533) and calcifications (κ: 0.229–0.527), but only slight to fair agreement for echogenicity (κ: 0.141–0.355), shape (κ: 0.0729–0.513) and margins (κ: 0.176–0.283)(9). In a study involving 100 thyroid nodules independently evaluated by eight radiologists, agreement was substantial for shape (κ = 0.61) and macro-calcifications (κ = 0.73), but only fair to moderate for all other features and lowest for margins and other types of echogenic foci (κ: 0.25–0.39)(10). Finally, a study involving 100 thyroid nodules independently evaluated by 15 sonographers found only slight agreement for margins (κ = 0.18) and large comet-tail artifact (κ = 0.08), but moderate agreement for macro-calcification (κ = 0.41) and no echogenic foci (κ = 0.52)(11).
Thus, improving the inter-reader agreement is an important issue to address. Herein, we include several educational tips that imaging practitioners may find helpful for enhancing the consistency of thyroid nodule interpretation with ACR TI-RADS.
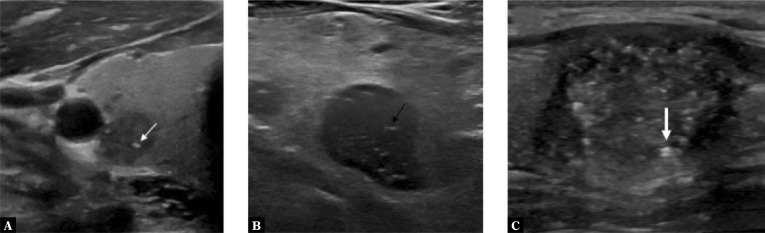
Tip 1. Differentiating punctate echogenic foci, PEF (+3 points) vs. echogenic interfaces (+0 points)
Unlike macro-calcifications, neither of these sonographic observations are associated with posterior acoustic shadowing. Punctate echogenic foci (PEF) are round and ≤1 mm, while echogenic interfaces havea linear or tram like appearance (Fig. 1). Large echogenic foci >1 mm associated with comet-tail artifacts (+0 points) denote colloids, and are benign. In contrast, echogenic foci ≤1 mm with comet-tail artifacts should be treated as PEF (+3 points)(4). Pertinently, if echogenic foci are found both in the nodule and in the surrounding thyroid parenchyma, these should not be classified as PEF(4). Benign observations that can mimic PEF include the back wall of tiny cysts and speckle pattern in normal thyroid parenchyma(4).
Fig. 1.
Greyscale sonographic images of: A. a thyroid nodule with round punctate echogenic foci (white thin arrow); B. a thyroid nodule with linear echogenic interfaces (black arrow); and C. a thyroid nodule with echogenic foci demonstrating a comet-tail artifact, in keeping with a colloid (white thick arrow)
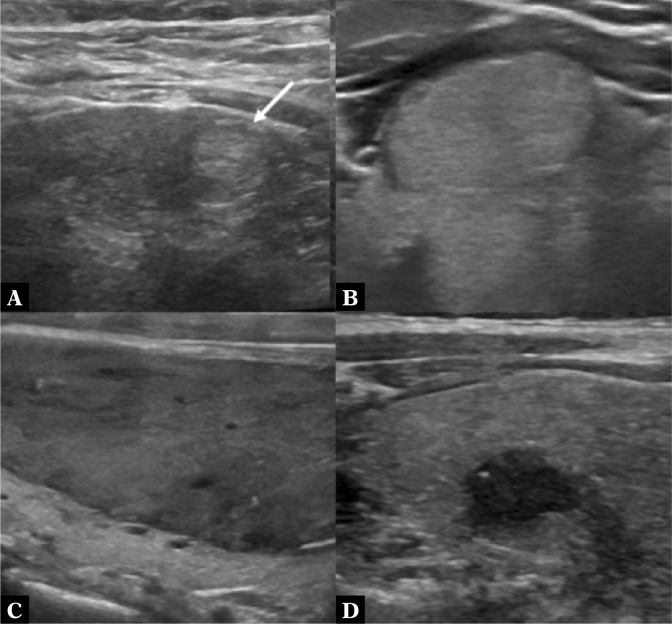
Tip 2. In a solid nodule, how do you determine if it is hyper- or isoechoic (+1 point), hypoechoic (+2 points) or very hypoechoic (+3 points)?
The background thyroid parenchyma and adjacent neck musculature are used as the reference for determining the echogenicity of thyroid nodules. Compared to the thyroid parenchyma, hyperechoic nodules have higher echogenicity, isoechoic nodules have similar echogenicity, while hypoechoic nodules have lower echogenicity (Fig. 2) (3). Conversely, very hypoechoic nodules have lower echogenicity than the neck musculature(3). To improve the accuracy and consistency of interpretation, these findings should be evaluated on several tissue planes on the still and cine images.
Fig. 2.
Greyscale sonographic images of: A. a hyperechoic nodule (white arrow) with higher echogenicity compared to the adjacent thyroid parenchyma; B. an isoechoic nodule with similar echogenicity to the adjacent thyroid parenchyma; C. a hypoechoic nodule with lower echogenicity compared to the adjacent thyroid parenchyma; and D. a very hypoechoic nodule with lower echogenicity compared to the neck musculature
Tip 3. Determining the echogenicity of a mixed cystic and solid nodule
The echogenicity of a mixed cystic and solid nodule should be evaluated based on the appearance of its solid component alone (Fig. 3). An anechoic appearance (+0 points) is therefore not an option, as this feature is synonymous with a cystic consistency. It is also important not to misinterpret debris/blood clot/necrotic tissue in a cyst for viable solid material(4). Doppler US, careful interrogation of the cine clips, and appropriate adjustment of technical parameters (e.g. gain, depth, focal zone, frequency and dynamic range) may help in making this distinction(4).
Fig. 3.
Greyscale sonographic image of a mixed cystic and solid nodule scored as ‘hypoechoic’ based on the echogenicity of the solid component
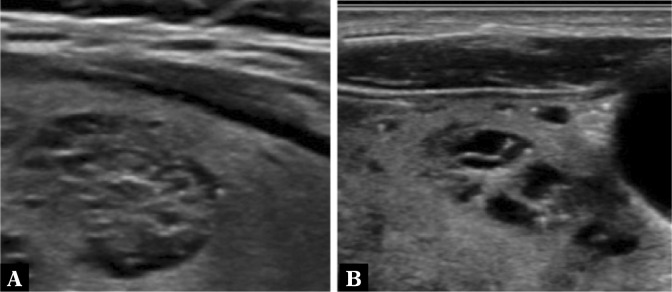
Tip 4. When a solid nodule has a heterogeneous echogenicity, i.e. partially hyper/isoechoic (+1 point) and partially hypoechoic (+2 points), which of these options do you choose?
In this scenario, given the absence of information available in the current literature, we recommend going with the finding that represents >50% volume of the nodule, as this finding is representative of the majority of the nodule (Fig. 4). When it is 50–50, the more conservative option with the lower point score should be selected (i.e. hyper/ isoechoic, +1 point).
Fig. 4.
Greyscale sonographic images of thyroid nodules with heterogeneous echogenicity: A. a mixed isoechoic and hypoechoic thyroid nodule (since >50% of the nodule is hypoechoic, this will be the descriptor selected for scoring); and B. a 50% isoechoic and 50% hypoechoic thyroid nodule (in this case, the more conservative ‘isoechoic’ descriptor will be selected for scoring)
Tip 5. At what point does a mixed cystic-solid nodule (+1 point) become predominantly solid (+2 points)?
This is a judgment call, as this observation represents a continuum and is thus problematic. Tessler et al. in their article (TI-RADS: A User’s Guide) suggested that in general, predominantly solid nodules that contain small cystic components that contain <5% of the overall volume should be considered as solid ( 4 ) . However, we contend that a lower threshold of ≥80% solid volume may be a more practical cut-off for scoring a nodule as solid, as the four-fifths rule of thumb is an easy concept to understand and apply for visual assessment (Fig. 5). This also aligns better with other risk classification systems such as ACR O-RADS, where an adnexal lesion is considered solid if ≥80% of its volume is of solid consistency(12).
Fig. 5.
Greyscale image of a thyroid nodule which would be classified as ‘solid’ based on >80% solid volume
Tip 6. What do you do when a nodule has dense calcification that obscures its composition and echogenicity?
In this scenario, choose solid (+2 points) for composition and iso-or-hyperechoic (+1 point) for echogenicity (Fig. 6)(3).
Fig. 6.
Greyscale sonographic image of a thyroid nodule with circumferential rim calcification. The acoustic shadow from the calcification obscures the composition and echogenicity of the nodule. In this scenario, the descriptors ‘solid’ and ‘iso– or–hyperechoic’ are selected for scoring
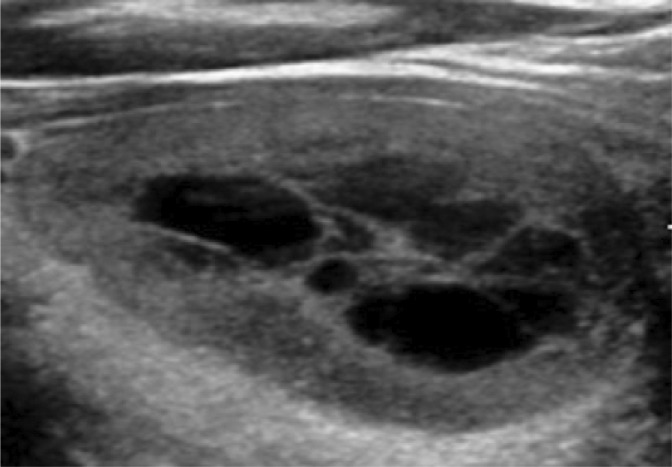
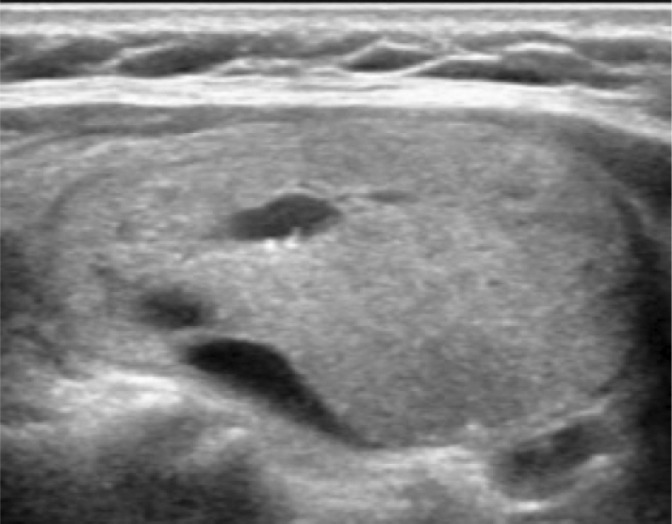
Tip 7. Differentiating a spongiform nodule (+0 points) vs. a mixed cystic and solid nodule (+1 point)
By definition, a spongiform nodule is one that is composed of >50% of small cystic spaces that are evenly distributed throughout the nodule – this appearance resembles a sponge (Fig. 7)(3). Intermediate nodules that do not meet this criterion but show a <80% solid volume should be described as being of mixed cystic and solid composition. When echogenic foci are found in a spongiform nodule, these are not considered as PEF and should be ignored(4).
Fig. 7.
Greyscale sonographic images of: A. spongiform nodule and B. a mixed cystic and solid nodule. Compared to (B), the cystic spaces are smaller and more evenly distributed (A)
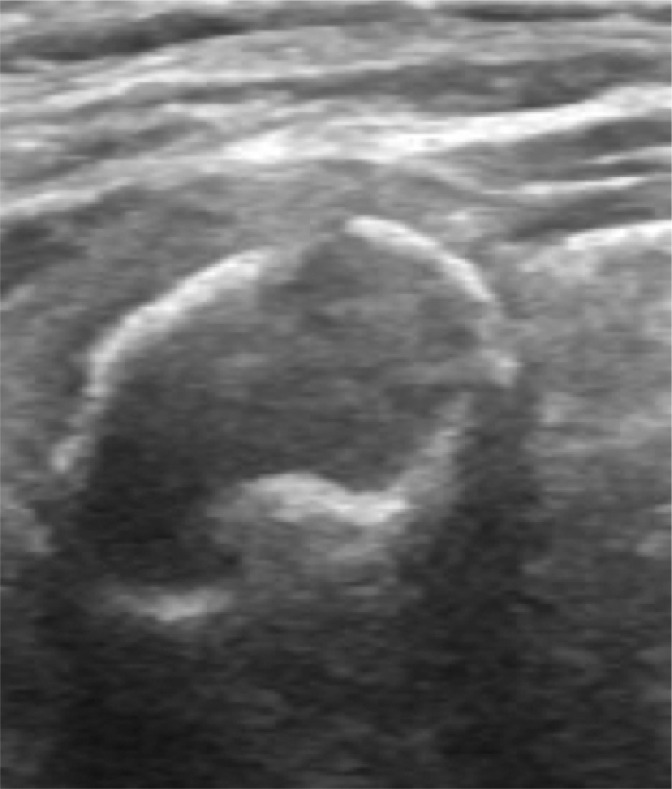
Tip 8. How do you score the shape of a nodule when it is completely round? (i.e. its anteroposterior dimension is equal to its transverse dimension)
The ACR TI-RADS committee recommends a more conservative selection of wider-than-tall, or alternatively, not taller-than-wide (+0 points) (Fig. 8)(4). It is important to note that the shape of the nodule should usually be assessed on the transverse plane of the thyroid gland(3). The ACR TI-RADS committee notes that it may rarely be appropriate to assess this characteristic in the sagittal plane if the nodule is obliquely oriented in that plane(4).
Fig. 8.
Transverse greyscale sonographic image of a completely round thyroid nodule (anteroposterior measurement equals transverse measurement). The more conservative ‘wider-than-tall’ description should be selected for scoring
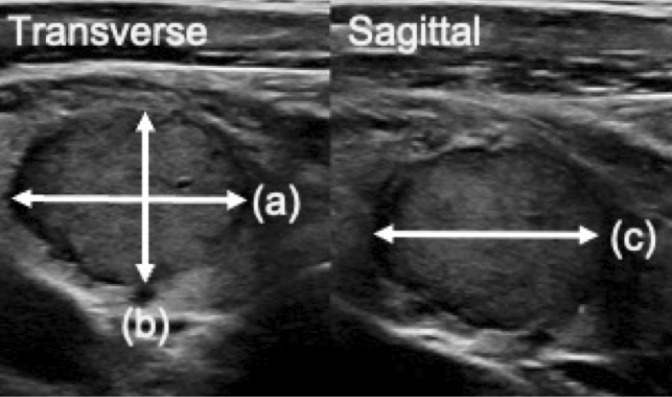
Tip 9. How do you measure the nodule size?
The nodule size should be measured in three dimensions (a × b × c) (Fig. 9). On a transverse sonogram of the thyroid, obtain the dimension of the nodule along its longest axis (a) followed by its largest dimension on a perpendicular plane to this (b). Next, on a sagittal sonogram of the thyroid, obtain the largest cranio-caudal dimension (c)(3,4). Calculating the volume of a nodule (formula = 0.52 × a × b × c) should also be performed, as this can provide a better indication of nodule enlargement compared to assessing measurements in three dimensions separately(13).
Fig. 9.
Greyscale sonographic images of a thyroid nodule, demonstrating how to measure nodule size, (a) × (b) × (c)
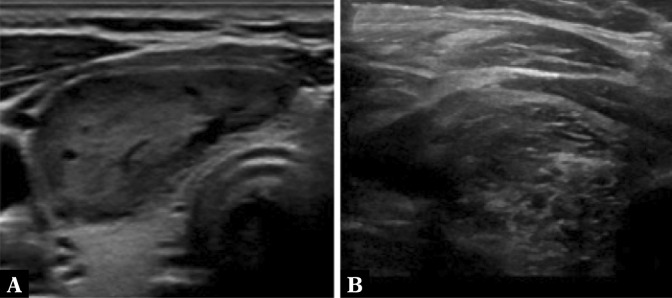
Tip 10. Assessing a nodule’s margins
The margins of a nodule represent its interface/border with the adjacent intra- or extra-thyroidal tissue.
Optimal visualization can be achieved by ensuring that the border of the nodule that is closest to the skin surface is perpendicular to the US beam, and that the appropriate gain and focal zones are used on a high-frequency linear transducer(4). A smooth margin (+0 points) is where the entire circumference of the nodule’s outline is regular and sharply marginated(4). If a nodule’s border is not depicted clearly in spite of optimizing technique and US parameters, then it should be categorized as ill-defined (+0 points). If there are protrusions, angulations or lobulations of parts of the nodule into the surrounding tissues, this should classified as lobulated or irregular (+2 points). Extra-thyroidal extension (+3 points) is a feature reserved for cases where there is an obvious and unequivocal invasion into the surrounding tissues such as the neck muscles, trachea, larynx, vasculature or esophagus(4). Lee et al. found that the combination of two sonographic findings including 1) more than 50% tumor contact with the thyroid capsule and 2) tumor disruption of the thyroid capsule as denoted by loss of the capsule’s outline, had a 23.7% sensitivity, 95.4% specificity, and area under the curve of 0.64 for predicting extra-thyroidal extension(14).
Conclusion
ACR-TI-RADS provides a framework for improving the risk stratification of nodules and reduces the need for unnecessary biopsies. However, there are inherent challenges relating to suboptimal inter-reader agreement. Several educational tips are discussed that may help improve the consistency of nodule interpretation with ACR TI-RADS. This would be a topic for more focused reader education and explanation in future iterations of TI-RADS.
Conflict of interest
The authors do not have any conflicts of interest or financial disclosures.
References
- 1.Tappouni RR, Itri JN, McQueen TS, Lalwani N, Ou JJ. ACR TI-RADS: pitfalls, solutions, and future directions. Radiographics. 2019;39:2040–2052. doi: 10.1148/rg.2019190026. [DOI] [PubMed] [Google Scholar]
- 2.Li W, Wang Y, Wen J, Zhang L, Sun Y. Diagnostic performance of American College of Radiology TI-RADS: a systematic review and metaanalysis. AJR Am J Roentgenol. 2021;216:38–47. doi: 10.2214/AJR.19.22691. [DOI] [PubMed] [Google Scholar]
- 3.Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA, et al. ACR thyroid imaging, reporting and data system (TI-RADS): white paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017;14:587–595. doi: 10.1016/j.jacr.2017.01.046. [DOI] [PubMed] [Google Scholar]
- 4.Tessler FN, Middleton WD, Grant EG. Thyroid imaging reporting and data system (TI-RADS): a user’s guide. Radiology. 2018;287:29–36. doi: 10.1148/radiol.2017171240. [DOI] [PubMed] [Google Scholar]
- 5.Hoang JK. Invited commentary on “ACR TI-RADS: Pitfalls, Solutions, and Future Directions”. Radiographics. 2019;39:2052–2054. doi: 10.1148/rg.2019190195. [DOI] [PubMed] [Google Scholar]
- 6.Hoang JK, Middleton WD, Tessler FN. Update on ACR TI-RADS: successes, challenges, and future directions, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol. 2021;216:570–578. doi: 10.2214/AJR.20.24608. [DOI] [PubMed] [Google Scholar]
- 7.Grani G, Lamartina L, Ascoli V, Bosco D, Biffoni M, Giacomelli L, et al. Reducing the number of unnecessary thyroid biopsies while improving diagnostic accuracy: toward the “Right” TIRADS. J Clin Endocrinol Metab. 2019;104:95–102. doi: 10.1210/jc.2018-01674. [DOI] [PubMed] [Google Scholar]
- 8.Koc AM, Adıbelli ZH, Erkul Z, Sahin Y, Dilek I. Comparison of diagnostic accuracy of ACR-TIRADS, American Thyroid Association (ATA), and EU-TIRADS guidelines in detecting thyroid malignancy. Eur J Radiol. 2020;133:109390. doi: 10.1016/j.ejrad.2020.109390. [DOI] [PubMed] [Google Scholar]
- 9.Itani M, Assaker R, Moshiri M, Dubinsky TJ, Dighe MK. Inter-observer variability in the American College of Radiology thyroid imaging reporting and data system: in-depth analysis and areas for improvement. Ultrasound Med Biol. 2019;45:461–470. doi: 10.1016/j.ultrasmedbio.2018.09.026. [DOI] [PubMed] [Google Scholar]
- 10.Hoang JK, Middleton WD, Farjat AE, Teefey SA, Abinanti N, Boschini FJ, et al. Interobserver variability of sonographic features used in the American College of Radiology thyroid imaging reporting and data system. AJR Am J Roentgenol. 2018;211:162–167. doi: 10.2214/AJR.17.19192. [DOI] [PubMed] [Google Scholar]
- 11.Wildman-Tobriner B, Ahmed S, Erkanli A, Mazurowski MA, Hoang JK. Using the American College of Radiology thyroid imaging reporting and data system at the point of care: sonographer performance and interobserver variability. Ultrasound Med Biol. 2020;46:1928–1933. doi: 10.1016/j.ultrasmedbio.2020.04.019. [DOI] [PubMed] [Google Scholar]
- 12.Andreotti RF, Timmerman D, Strachowski LM, Froyman W, Benacerraf BR, Bennett GL, et al. O-RADS US Risk Stratification and Management System: a consensus guideline from the ACR Ovarian-Adnexal Reporting and Data System Committee. Radiology. 2020;294:168–185. doi: 10.1148/radiol.2019191150. [DOI] [PubMed] [Google Scholar]
- 13.Kwon H, Oh HS, Kim M, Park S, Jeon MJ, Kim WG, et al. Active surveillance for patients with papillary thyroid microcarcinoma: a single center’s experience in Korea. J Clin Endocrinol Metab. 2017;102:1917–1925. doi: 10.1210/jc.2016-4026. [DOI] [PubMed] [Google Scholar]
- 14.Lee DY, Kwon TK, Sung MW, Kim KH, Hah JH. Prediction of extrathyroidal extension using ultrasonography and computed tomography. Int J Endocrinol. 2014;2014:351058. doi: 10.1155/2014/351058. [DOI] [PMC free article] [PubMed] [Google Scholar]