ABSTRACT
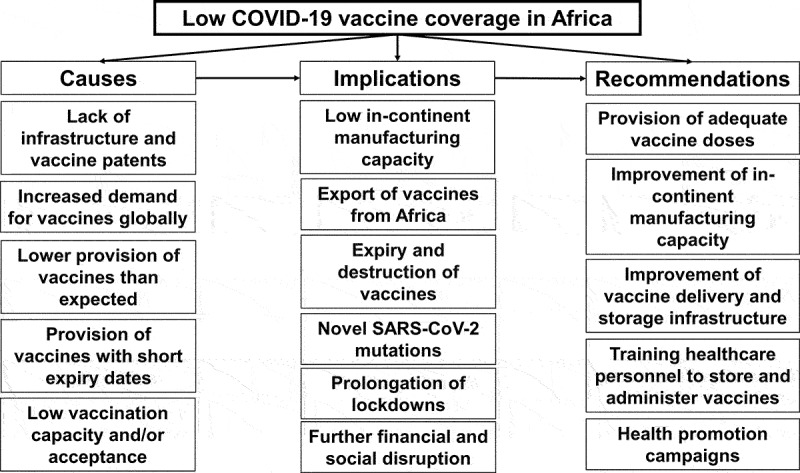
Disparities in COVID-19 vaccine coverage across the globe have uncovered inequities in global healthcare. While more than half of the population of the developed countries have been fully vaccinated, only a small percentage of the African population has received one vaccine dose so far, a far cry from the global vaccination targets. Furthermore, several low and middle income (LMICs) African countries lack the competence, infrastructure, logistics, and financial resources to mass-vaccinate their populations. This paper highlights the causes and implications of the low COVID-19 vaccine coverage on Africa and the global community, and discusses strategies for restructuring and strengthening COVID-19 vaccination in Africa.
KEYWORDS: COVID-19 pandemic, COVID-19 vaccination, vaccine hesitancy, Covid-19 vaccine inequity, SARS-COV-2, disparities, low coverage of vaccine, Africa, LMIC, developing countries
Graphical abstract
Introduction
The development and roll-out of COVID-19 vaccines has been a source of relief, as well as has brought up a new challenge, namely inequity in global access to the COVID-19 vaccines.1 While more than 70% of the population of the developed countries have been fully vaccinated, only around 8% of the African population have been vaccinated, as of 2021 December 31.2 The lack of capacity building by Africa to produce enough vaccine doses has led to a dependency on external producers, and, as a result, the continent is disproportionately affected by vaccine nationalism, stockpiling, and low-economic status.3
The implications of the low coverage of the COVID-19 vaccine in Africa on its already fragile health system and the global economic recovery could be overwhelming and unprecedented.1 This paper highlights the causes and implications of the low COVID-19 vaccine coverage in Africa and makes recommendations to increase vaccination rates in the continent.
Causes and implications
As of 2021 December 31, of the 8 billion COVID-19 vaccine doses administered globally, only about 250 million (3%) doses have been administered in Africa.3 While about 70% of the population in high-income countries and upper-middle-income countries have been fully vaccinated, only around 8% of Africans have been vaccinated.3 At a time when the developed countries have started giving a booster dose to their population, Africa is still struggling to vaccinate its healthcare workers.4 This inequity must be bridged if the COVID-19 pandemic is to end.
There are at least 12 COVID-19 vaccine production facilities (mainly in the pipeline) across the continent set up by foreign pharmaceutical industries, including Pfizer-BioNTech, Johnson & Johnson, Russia’s Sputnik V, and China’s Sinovac vaccines, yet Africa produces less than 1% of all vaccines used in the continent.5 This is because the COVID-19 vaccine production facilities are focused mainly on expanding fill-and-finish capacity at the expense of vaccine-substance manufacturing. The latter is partly related to the unwillingness of licensed pharmaceutical companies to release their rights over their patented intellectual property and technology.5 Other reasons include the lack of specialized infrastructure and personnel required for the entire process of vaccines manufacturing – let alone development. Even if these problems would be addressed, the lack of stable electricity and storage facilities poses significant limitations to full vaccine manufacturing in Africa. Reparatory action would include an increase in state and private investments to industrial infrastructure and capacity. Once these needs were met, African governments and pharmaceutical industry could seek a consensus on the release of COVID-19 vaccines related patents. As of now, in-Africa manufacturing does not mean in-Africa distribution. For instance, Europe has received millions of Johnson & Johnson vaccine doses that went through the fill-and-finish stage of production in South Africa by Aspen Pharmacare.3,6 Meanwhile, South Africa is yet to receive a significant portion of its 31 million Johnson & Johnson doses. This has been identified as a major reason why only 7% of South Africa’s population is fully vaccinated.3 It is not uncommon and easy to fault pharma/biotech companies’ greed for limits on COVID-19 vaccine’s production; however, it should be noted that there are other critical challenges limiting the vaccine’s production in Africa – theses include lack of financial resources to invest in research and manufacturing facilities, lack of expertise working in production as well as clean room and quality control system, lack of infrastructure including stable electricity and storage facilities etc.
The lack of capacity building to manufacture sufficient COVID-19 vaccine doses has led Africa to depend on the COVAX initiative and on donations from developed countries.3 COVAX, a global initiative with a goal to accelerate the development and manufacture of COVID-19 vaccines, and to guarantee fair and equitable access for every country in the world, however, has not met the initial expectations, and the donations from the developed countries have only covered a fraction of Africa’s needs.7 Through the COVAX scheme, which is largely sourced from the Serum Institute of India, 41 African countries are expected to have access to 600 million COVID-19 vaccine doses, estimated to cover 20% of their population by the end of 2021.7 However, vaccine nationalism, stockpiling, and disruption to international supply chains have hindered the scheme, as India has banned the export of COVID-19 vaccine, diverting it to domestic use, and the high-income countries have been ordering more COVID-19 doses in order to provide their citizens with a booster shot.4,7 A report from the United Nations Children’s Fund (UNICEF) shows that G20 members have received 15 times more COVID-19 vaccine doses per capita than sub-Saharan African countries.4 This calls for concern.
While many of the leaders of the high-income countries have pledged to donate their excess doses to Africa and other low-income countries through the COVAX scheme; of the 1.3 billion additional doses promised, only 194 million doses have been donated.4 This is further compounded by donations of COVID-19 vaccines that are near expiry date due to the short shelf-life of the vaccines to African countries, which have resulted in the expiry of some COVID-19 vaccine doses in the continent. At least seven African countries have been reported to have destroyed about 450,000 expired COVID-19 vaccine doses due to expiry.8
Further, there is controversy regarding the pricing of the COVID-19 vaccine with significant variation within and among the various vaccines. For instance, the AstraZeneca vaccine is priced higher in Uganda (7 US Dollars) and South Africa (5.25 US Dollars), in comparison to the European Union (3.50 US Dollars).9
On top of the inequity in access to the vaccine, there is also a lack of adequate resources for effective vaccination, as well as the problem of vaccine hesitancy in Africa. In South Sudan, for instance, limited funds, lack of vaccine storage facilities and vaccinators, coupled with sub-optimal training, poor awareness campaigns, and an inability to capture crucial data and distribute immunization cards are slowing the pace of vaccination.10 The COVID-19 vaccine acceptance rate in Africa ranges from 15% in Cameroon to 86% in Rwanda.11 Vaccine hesitancy is the leading cause of low coverage of COVID-19 vaccination in Zimbabwe and South Africa.12 The high hesitancy is influenced by mistrust for government programs due to a legacy of poor service delivery, lack of confidence in the vaccine’s efficacy and the integrity of the providers, complacency, and anti-vaccine campaigns on social media.12,13
Given these challenges, it is reasonable to assume that Africa may not be able to vaccinate 60% of its population (about 780 million people), a proportion considered necessary for the purpose of achieving herd immunity within 2022.1 Yet, this estimation has not taken into account the fact that the required vaccination coverage to achieve herd immunity has been further increased based on the experience with the Delta SARS-CoV-2 variant.14 The situation has become even more challenging given the emergence of the Omicron SARS-CoV-2 mutation. The global need to accelerate the provision of “booster” vaccination reduces the supply of vaccines to Africa disproportionately to the increased need for vaccination within the continent.15 Consequently, Africa is at risk of a continued scourge of the pandemic and the development of new variants as seen with the Delta and Omicron variants, which could spread globally and resist vaccines, thereby putting us back to “square one” in the fight against the pandemic.3 Increasing awareness that high-velocity transmission of the virus in populations with low vaccination coverage makes the emergence of novel, potentially resistant-to-vaccine variants more likely, provides health bodies and stakeholders sufficient grounds to accelerate vaccination campaigns in Africa. Nevertheless, this entails some indirect benefit for developed countries.
According to Nyenswah,16 African countries need to be conservative with lifting COVID-19 pandemic restrictions because doing so without raising vaccination rates is a recipe for disaster; while this is correct, it is equally important to know that a continued lockdown in the continent will further worsen the social, economic, and health impact of the pandemic, especially for the most vulnerable and the marginalized people. A continued lockdown also affects routine childhood immunization efforts and other essential health services in the continent. Almost half of the African countries have postponed their mass immunization campaigns – placing 228 million people, mostly children at risk of preventable diseases.16 Sadly, there have been outbreaks of measles, monkeypox, and cholera as well as disruption of HIV/AIDS, malaria, and tuberculosis care in Africa amid the pandemic.17–21 This has further strained the already fragile healthcare systems of African countries. This underscores why the world leaders and other stakeholders in partnership with the African governments must urgently widely vaccinate the African population to enable full lifting of the lockdown and promote recovery.
While developed nations are likely to vaccinate and recover economically faster from the COVID-19 epidemic, African countries might not be able to do so and may not achieve pre-COVID-19 levels of economic growth until 2024.2 COVID-19 vaccine inequity is estimated to cost the world economy $2 trillion, and the low-income countries will be largely affected.22 This implies that more disasters loom in Africa. The impending poverty threatens child labor, childhood malnutrition, child neglect, child marriage, and lack of access to basic amenities.4 This is not to say the developed countries will not have their fair share. A report from the Economist Intelligence Unit showed that the developed economies could bear 34% of the global economic loss between the years 2022–2025 if vaccine inequity continues.22 The study also warns that the significant COVID-19 vaccination coverage gap will “reshape the global political and social environment,” fueling discontent, raising the danger of social upheaval, redirecting tourism flows, and allowing developed nations to engage in increased vaccine diplomacy.22 All these call for urgent attention.
Recommendations
To ensure Africa fulfills the COVID-19 vaccination targets, the continent should boost vaccine access and deploy sustainable and technical innovations that address the profound complexities of the region’s health system. We call on concerned stakeholders to urgently deliver the vaccine doses they pledged in addition to providing the essential resources needed to ensure widespread vaccination in Africa.
The world leaders, policymakers, and global organizations in partnership with African leaders should also accelerate the production of COVID-19 vaccine in Africa by removing all barriers to production and distribution, including but not limited to patent waiver, technology, and information sharing, human capacity building, facilitating partnership, promoting research, and providing fund and other essential resources needed.3 There is also the need to ensure vaccines produced in Africa are used in Africa and not diverted to the already saturated high-income countries. This will increase Africa’s access to the vaccine, reduce the cost of transportation, and address the challenge of vaccines expiring before getting to health facilities.
African governments can negotiate with pharmaceutical industries for this purpose and call upon the governments of non – African countries that receive vaccines manufactured in Africa. Nevertheless, putting pressure on the industry to relinquish its COVID-19 vaccines related intellectual and commercial rights remains controversial. Although it may seem as an urgent solution, such a move would discourage pharmaceutical companies from investing in the development of vaccines for future pandemics, or even for novel vaccine-resistant variants of SARS-CoV-2. At a greater scale, relying on such a practice may reverberate on both the willingness and the financial capacity of the industry to advance its drug development efforts in other crucial fields, such as cancer and cardiovascular diseases. Hence, political pressure and negotiation with the industry should be based on arguments and actions that do not put the continuity of vaccines development and production in peril.
From a technical point of view, action is required to ensure the efficiency of cold chains during all stages of the transportation of vaccines across the continent. The challenge of poor electricity supply needed for cold storage and distribution can be overcome by using solar direct-drive refrigerators (SDD). This SDD technology directly utilizes solar energy directly, cold storage materials and using energy stored in the frozen bank to keep the refrigerator cold during the night and cloudy days.23 As a result, the geographic location of the continent that falls under a high sunshine belt is capitalized to promote vaccine equity.24 For the COVID-19 and other vaccines, this sustainable technology has the potential to solve numerous difficulties with off-grid vaccine refrigeration, enabling nationwide vaccination and extending cold chains to hard-to-reach places. The cost-effectiveness and sustainability of this solar technology is a promising solution to the challenge of electricity. Such goals must be actively promoted by Global Alliance Vaccine Initiative (GAVI), World Health Organization (WHO), and other public health multinational organizations driving health equity in low-middle-income countries.
Furthermore, vaccine cold-chain officers and immunization officers must be properly trained in handling and storing the vaccines. They also need to learn proper data management and Geographic Information System (GIS) maps. The GIS maps provide information about what is located in even the hardest areas to reach, thereby managing logistical problems with the distribution of vaccines to healthcare facilities, and aiding efficient microplanning for the process of vaccination.25 The maps have the potential to provide information on not only the location of health facilities, but also the population density of towns and the placement of key structures such as churches, mosques, and markets, all of which are possible target groups for mass outreach campaigns. When health workers are provided with these maps and properly equipped with the technical and analytical skills needed to use and read the maps, or better still, provided the devices to access these maps online, there will be better coordination, microplanning, and record-keeping for the vaccination process.
And lastly, the challenge of vaccine hesitancy must be addressed. To obtain the best results, a multi-purpose framework oriented at individuals, socio-political situations, and specific social groupings must be established.13 Good policies, transparency, accountability, diplomacy, and participatory engagement of the public in vaccine clinical trials, approval, and purchase are effective strategies that must be adopted to increase public trust and confidence in the vaccines.13 Proper health literacy advocacy projects must also be used as an intervention to promote awareness of the COVID-19 with accurate facts and details whilst also educating the public on the vaccine safety and effectiveness, and why they should be vaccinated. It is also important to use a socio-cultural sensitive vaccination promotion strategy such as engagement of community and religious leaders in the vaccination campaigns and the spread of correct information about the vaccine safety and effectiveness through influencers on social media.12
Laid out above are opportunities and future potentials in restructuring and strengthening the COVID-19 vaccines supply and distribution in Africa and other developing countries. It is important that African leaders pool resources together to finance and adopt these innovations and provide technical support and capacity building to all essential workers. African private entities and individuals with a high net worth can also step up and contribute at local, national, or continental level. Governments can provide tax incentives to such individuals and entities, as long as they contribute to the development of infrastructure and resources that will benefit health and access to medicines in Africa during and after the pandemic. There cannot be a better time to end Africa’s over reliance on developed nations than now.
Conclusion
The coronavirus continues to mutate and thus has the potential to cause great damages to the health and economic system of Africa and the rest of the world. To properly mitigate the disease and its threats, massive interventions and innovations that target and address the challenges specific to the continent must be put in place. Laid out above are opportunities and future potentials in restructuring and strengthening the COVID-19 vaccine supply and distribution. By fully adopting these innovations and providing technical support and capacity building to health workers, Africa has the potential to achieve a streamlined flow of information and the necessary equipment not just for the continent-wide COVID-19 vaccination process but in many ways Africa’s entire health system. Just like the WHO Director-General, Dr Tedros Adhanom Ghebreyesus, stated: Vaccine inequity is the world’s biggest obstacle to ending this pandemic and recovering from COVID-19. Economically, epidemiologically and morally, it is in all countries’ best interest to use the latest evidence available to make life saving vaccines available to all.
Acknowledgments
We are thankful to Prof. T.M Akande for reviewing this project. We appreciate Melody Okereke for providing insights to this project.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.The World Health Organisation . Vaccine inequity undermining global economic recovery. Geneva; 2021. July 22 [accessed 2021 Sept 10]. https://www.who.int/news/item/22-07-2021-vaccine-inequity-undermining-global-economic-recovery. [Google Scholar]
- 2.Our World in Data . Coronavirus (COVID-19) vaccinations. 2021. Sept 1 [accessed 2021 Dec 31]. https://ourworldindata.org/covid-vaccination.
- 3.One Africa . Data dive: the astoundingly unequal vaccine rollout (online). 2021. Oct 30 [accessed 2021 Dec 31]. https://www.one.org/africa/issues/covid-19-tracker/explore-vaccines/#.
- 4.United Nations Children’s Fund (UNICEF) . G20 members have received 15 times more COVID-19 vaccine doses per capita than sub-Saharan African countries (online). 2021. Oct 27 [accessed 2021 Dec 31]. https://www.unicef.org/nigeria/press-releases/g20-members-have-received-15-times-more-covid-19-vaccine-doses-capita-sub-saharan.
- 5.Zainab U, Juliette O.. Is there any COVID-19 vaccine production in Africa? Carnegie Endowment for International Peace; 2021. Sept 13 [accessed 2021 Sept 18]. https://carnegieendowment.org/2021/09/13/is-there-any-covid-19-vaccine-production-in-africa-pub-85320. [Google Scholar]
- 6.Robbins R, Mueller B. Covid-19 vaccines produced in Africa are being exported to Europe. New York Times; 2021. Aug 16 [accessed 2021 Dec 8]. https://www.nytimes.com/2021/08/16/business/johnson-johnson-vaccine-africa-exported-europe.html.
- 7.Abiodun A, Andersen H, Mamo LT, Sisay OB. Vaccine manufacturing in Africa: what it takes and why it matters. Tony Blair Institute for Global Change; 2021. Apr 1 [accessed 2021 Sept 12]. https://institute.global/advisory/vaccine-manufacturing-africa-what-it-takes-and-why-it-matters. [Google Scholar]
- 8.Peter M. Covid-19 vaccines: why some African states can’t use their vaccines. BBC Reality Check; BBC news; 2021. May 7 [accessed 2021 Sept 10]. https://www.bbc.com/news/56940657. [Google Scholar]
- 9.Global Health Centre at the Graduate Institute, Geneva . COVID-19 vaccine access (online). 2021. Oct 7 [accessed 2021 Oct 30]. https://www.knowledgeportalia.org/covid19-vaccine-arrangements.
- 10.Nachega JB, Sam-Agudu NA, Masekela R, van der Zalm MM, Nsanzimana S, Condo J, Ntoumi F, Rabie H, Kruger M, Wiysonge CS, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob Health. 2021. June;9(6):e746–5. doi: 10.1016/S2214-109X(21)00097-8. Epub 2021 Mar 10. PMID: 3371363x3; PMCID: PMC7946417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wirsiy FS, Nkfusai CN, Ako-Arrey DE, Dongmo EK, Manjong FT, Cumber SN. Acceptability of COVID-19 vaccine in Africa. Int J MCH AIDS. 2021;10(1):134–38. doi: 10.21106/ijma.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dzinamarira T, Nachipo B, Phiri B, Musuka G. COVID-19 vaccine roll-out in South Africa and Zimbabwe: urgent need to address community preparedness, fears and hesitancy. Vaccines. 2021;9(3):250. doi: 10.3390/vaccines9030250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aborode AT, Fajemisin EA, Ekwebelem OC, Tsagkaris C, Taiwo EA, Uwishema O, Awoniyi OO, Ahmad S, Essar MY, Adanur I. Vaccine hesitancy in Africa: causes and strategies to the rescue. Ther Adv Vaccines Immunother. 2021. Sept 28;9:25151355211047514.doi: 10.1177/25151355211047514. PMID: 34604696; PMCID: PMC8481750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eslava-Schmalbach J, Rosero EB, Garzón-Orjuela N. Global control of COVID-19: good vaccines may not suffice. Rev Panam Salud Publica. 2021. Dec 10;45:e148. doi: 10.26633/RPSP.2021.148. Published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adepoju P. As COVID-19 vaccines arrive in Africa, Omicron is reducing supply and increasing demand. Nat Med. Published online ahead of print 2021. Dec 13. doi: 10.1038/d41591-021-00073-x. [DOI] [PubMed] [Google Scholar]
- 16.Nyenswah TG. Vaccine hesitancy and Africa’s Covid-19 vaccination woes present a pandemic paradox. The Africa Report (online); 2021. May 14 [accessed 2021 Sept 10]. https://www.theafricareport.com/88538/africas-covid-19-vaccination-woes-present-a-pandemic-paradox/. [Google Scholar]
- 17.Uwishema O, Taylor C, Lawal L, Hamiidah N, Robert I, Nasir A, Chalhoub E, Sun J, Akin BT, Adanur I, et al. The syndemic burden of HIV/AIDS in Africa amidst the COVID-19 pandemic. Immun Inflamm Dis. Published online ahead of print 2021. Oct 4;2021:10. doi: 10.1002/iid3.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aborode AT, Tsagkaris C, Jain S, Ahmad S, Essar MY, Fajemisin EA, Adanur I, Uwishema O. Ebola outbreak amid COVID-19 in the Republic of Guinea: priorities for achieving control. Am J Trop Med Hyg. 2021. Apr 14;104(6):1966–69. doi: 10.4269/ajtmh.21-0228. Epub ahead of print. PMID: 33852428; PMCID: PMC8176515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aborode AT, David KB, Uwishema O, Nathaniel AL, Imisioluwa JO, Onigbinde SB, Farooq F. Fighting COVID-19 at the expense of malaria in Africa: the consequences and policy options. Am J Trop Med Hyg. 2021. Jan;104(1):26–29. doi: 10.4269/ajtmh.20-1181. PMID: 33205743; PMCID: PMC7790111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Uwishema O, Adriano LF, Torbati T, Onyeaka H. Measles crisis in Africa amidst the COVID-19 pandemic: delayed measles vaccine administration may cause a measles outbreak in Africa. J Med Virol. 2021;93(10):5697–99. doi: 10.1002/jmv.27150. [DOI] [PubMed] [Google Scholar]
- 21.Wada YH, Musa MK, Musa SS, Khalid GM, Lucero Prisno DE 3rd. Dual burden of COVID-19 and TB in Africa. Clin Epidemiol Glob Health. 2021;12:100847. doi: 10.1016/j.cegh.2021.100847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Economic Intelligence Unit . How much will vaccine inequity cost? London; 2021. [accessed 2021 Nov 1]. https://www.eiu.com/n/campaigns/how-much-will-vaccine-inequity-cost/. [Google Scholar]
- 23.World Health Organization . Solar direct-drive vaccine refrigerators and freezers. Geneva; 2017. March 1 [accessed 2021 Sept 10]. Solar direct-drive vaccine refrigerators and freezers (who.int). [Google Scholar]
- 24.Bamisile O, Dagbasi M, Babatunde A, Ayodele O. A review of renewable energy potential in Nigeria; solar power development over the years. Eng Appl Sci Res. 2017;44:242–48. [Google Scholar]
- 25.Inah O. Uses, applications and prospects of GIS in Nigeria. Cross River State (Nigeria): University of Calabar (UNICAL); 2015. [accessed 2021 Sept 10]. http://geospatiallinks.com.ng/wp-content/uploads/2017/08/Uses_Applications_and_Prospects_of_GIS_in_Nigeria_by_Dr-Inah_Okon_GIS_DAY_2015.pdf. [Google Scholar]


