Introduction
In the early days of the first global wave of the COVID-19 pandemic, the potential for a postviral syndrome to manifest following COVID-19 infection was first recognized. Here, we present an analysis of a case series of the first 20 patients’ data collected in clinical practice to evaluate the potential of a possible alternative treatment for Long COVID.
Methods
Face-to-face treatment sessions with Perrin techniqueTM practitioners occurred weekly involving effleurage/other manual articulatory techniques. The individuals being treated also undertook daily self-massage along with gentle mobility exercises. Patients recorded symptom severity using the self-report 54-item profile of fatigue-related states (PFRS) before and after treatment.
Results
The mean age of male patients was 41.8 years (range, 29–53 years), and for female patients, 39.3 years (range, 28–50 years). None of the participants had a prior diagnosis of chronic fatigue syndrome, and all were new attendees to the clinics at the time of initial assessment. The average number of treatment sessions was 9.7 in men and 9.4 in women. The reduction in PFRS scores was 41.8% in men and 60.5% in women. The highest subscale scores on average were for fatigue, with the lowest for somatic symptoms. All subscale scores showed, on average, a similar reduction of approximately 50% postintervention, with the reduction in score relating to a decrease in the severity of symptoms.
Conclusion
Our findings suggest that a specific manual lymphatic drainage intervention may help to reduce fatigue symptoms related to Long COVID, perhaps preventing acute symptoms through early intervention.
Keywords: fatigue, Long COVID, lymphatic drainage, treatment
Introduction
During the first global wave of the COVID-19 pandemic, we reported on the potential for the emergence of a postviral syndrome following COVID-19 infection in a letter to the editor [1]. This type of postviral illness was previously reported following severe acute respiratory syndrome (SARS) infection, also a coronavirus, when some patients, many of them healthcare workers, went on to develop a prolonged chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME)–like illness that nearly 20 months on prevented them from returning to work [2]. This by its nature puts people at increased risk of weight gain and so of type 2 diabetes and, consequently, cardiovascular disease.
We have proposed [1] that once an acute COVID-19 infection had been overcome, a subgroup of remitted patients were likely to experience long-term adverse effects resembling CFS/ME symptomatology such as persistent fatigue, diffuse myalgia, depressive symptoms, and nonrestorative sleep. This post-COVID syndrome now being termed ‘Long COVID’ [3] is emerging as a global health issue. We previously pointed out that an early intervention applying management techniques used in patients with CFS/ME appears to help reduce the fatigue-related symptoms of Long COVID [1].
An evidence-based hypothesis [4] suggests that post-COVID-19 fatigue syndrome may result from damage to olfactory sensory neurons, causing an increased resistance to cerebrospinal fluid outflow and further leading to congestion of the glymphatic (glial lymphatic) system with subsequent toxic buildup within the central nervous system. This is supported by findings that SARS-CoV-2 can enter the nervous system by crossing the olfactory mucosa [5] and that the spike protein of the virus crossed the blood–brain barrier in mouse studies [6]. Our manual treatment appears to facilitate central lymphatic drainage, improve mechanics, and to reduce the inflammation of the cranium and spine, while also reducing allostatic load by improving the sympathetic tone.
Halpin et al. [3] reportedly established an integrated COVID-19 rehabilitation pathway that provides targeted intervention for people with Long COVID, based on their symptoms and needs. These authors classified Long COVID as ‘postacute COVID’ when the symptoms persisted beyond 3 weeks and ‘chronic post-COVID syndrome’ beyond 12 weeks after infection. It was suggested that these phases are complex multisystem syndromes requiring a multidisciplinary team to manage and treat the physical, cognitive, psychological, social, and vocational domains of this health condition. Investing in such specialist multidisciplinary rehabilitation services may help to reverse these symptoms before they become established.
We have previously described a case study [1] that pointed to success in treating a man with Long COVID/chronic post-COVID-19 fatigue using a manual intervention for CFS/ME [7,8]. This type of intervention has the potential to be applied more widely after thorough and comprehensive evaluation. Utilizing manual treatments, accredited UK osteopaths and physiotherapists among our practitioner network have reported treating patients with post-COVID illness and incorporating the routine recording of the profile of fatigue-related states (PFRS) [9] as an outcome assessment measure within the clinical setting.
Previously osteopathic treatment of chronic illness symptoms has shown positive findings in a variety of clinical contexts [10–12]. Here, we present an analysis of a case series of the first 20 patients’ data collected to evaluate the potential of one particular osteopathic intervention [7,8] with Long-COVID patients.
Methods
Patients seen by a qualified Perrin TechniqueTM practitioner (osteopath or physiotherapist) were asked to complete the PFRS prior to entry (baseline) and again around 3 months after receiving a manual treatment protocol for fatigue-related to Long COVID. The diagnosis of Long COVID was made on the basis of a positive PCR test for COVID-19 and continuing fatigue manifest for more than 12 weeks after an acute COVID-19 infection. Based on clinical interviews, none of the patients in this clinical case study had any history of mental illness, significant physical health issues, or a prior diagnosis of CFS/ME. All were new attendees to the clinic at the time of initial assessment. We asked practitioners to submit the patients’ completed questionnaires as anonymized data to RP by the end of January 2021.
Intervention
Treatment sessions with practitioners were completed once a week as described in Perrin [8], which involved effleurage of the neck/back/chest plus soft tissue stretching of paravertebral thoracic muscles, trapezii and levator scapulae, suboccipital musculature, and gentle cranial osteopathic techniques. Treated patients also followed a daily home-based self-massage routine of the head, neck, and chest combined with alternating warm and cool gel packs on the upper spine to encourage a reduction of spinal inflammation and further aid lymph drainage of the brain and spine. These home-based techniques included regular gentle mobility exercises involving rotational movement of the thoracic region to improve spinal mobility. The number of practitioner-based treatment sessions conducted was recorded prior to data extraction.
Outcome measure
Six practitioners collected 20 sets of patient-recorded symptoms severity scores on the self-report 54-item PFRS [9], immediately before treatment and at 12 weeks or after the final treatment session if earlier. Responses were scored on a 7-point Likert-scale ranging from 0 (not at all) through 3 (moderately) to 6 (extremely). A higher score on the PFRS indicates a higher level of symptomatology summated over specific domains. The PFRS has four subscales: emotional distress, cognitive difficulty, fatigue, and somatic symptoms [9]. Importantly, the PFRS measure covers symptom areas (such as difficulty in standing for long, slowness of thought, feeling anxious, feeling faint, limbs feeling heavy, and the slightest effort induces physical tiredness) that are core to the presentation of Long COVID, apart from respiratory symptoms and loss of taste. The measure has shown high reliability, high internal consistency, and good convergence with comparison measures [9].
Data analysis
The data were analyzed in Microsoft Office EXCEL 2016 and in Stata 14 (College Station, Texas, USA). We have not conducted inferential analyses, as the study is not formally powered. Therefore, we present descriptive data on the study sample and their responses on the PFRS questionnaire. Spearman’s rank correlation was calculated as an indication of association between the number of treatment sessions and change in PFRS score.
We have summarized the total PFRS score and its subscales (Tables 2 and 3). Table 2 shows data for patients who completed all items on the specified subscale and overall (i.e. there were no missing data). Where data were missing on an item, we ‘imputed’ the mean score by using the responses to other items on the subscale answered by the patient (as these are more likely to be correlated with each other than with responses from other patients) [13]. If more than half of the items on a particular subscale were missing, the subscale score was considered to be missing. This only happened once (Table 3).
Results
The mean age of men was 41.8 years (range, 29–53 years), and for women, 39.3 years (range, 28–50 years) (Table 1). The mean time interval between onset of corona virus symptoms and start of treatment for Long COVID was similar between men and women at just over 20 weeks. The average number of treatment sessions was similar at 9.7 in men and 9.4 in women (with a maximum of 12 weekly treatment sessions).
Table 1.
Description of the patient group and reported change inprofile of fatigue-related states from baseline to completion of3-month course of treatment
| Male (6) | Female (14) | |
|---|---|---|
| Minimum Age | 29 | 28 |
| Maximum Age | 53 | 50 |
| Average PFRS 0 months | 152.7 | 127.9 |
| Average PFRS 3 months | 88.9 | 50.5 |
| Change in Average PFRS | 63.8 | 77.4 |
| % Change in PFRS | 41.8 | 60.5 |
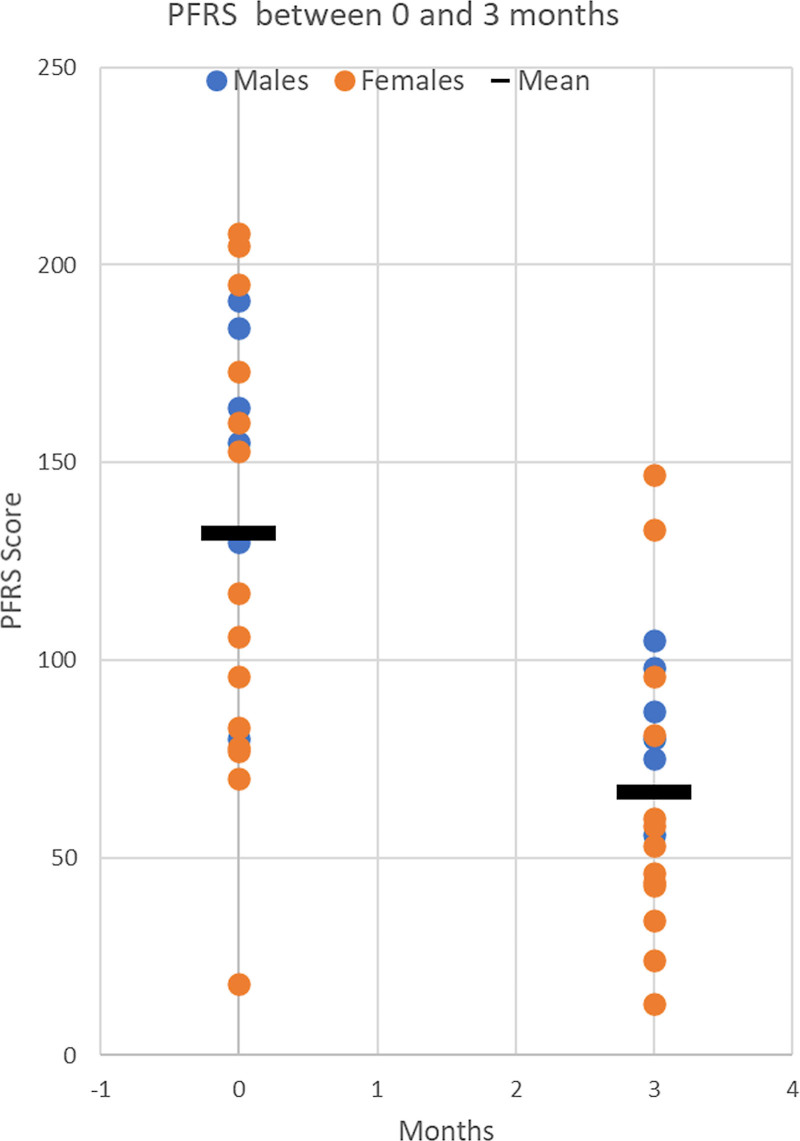
The change in absolute overall PFRS scores post-intervention was lower in men (mean change = −63.8 units) than in women (mean = −77.4 units) (Table 1 and Fig. 1). The items that specifically showed improvement were physical fatigue (decreased), concentration (increased), energy (increased), postexertional malaise (decreased), back pain (decreased), lack of restorative sleep (improved), mental fatigue (decreased), and depression (decreased).
Fig. 1.
Profile of fatigue-related states score pre- and postinterventions for men and women. Months refers to months after start of treatment.
We have summarized the PFRS subscale data in Tables 2 and 3. Table 2 shows data for patients who completed all items on the specified subscale and overall (i.e. there were no missing data), and Table 3 shows imputed data. As the two sets of results are similar, we only present the mean, median, and range in Table 3. The highest average scores, at both baseline and 3-month postintervention, were for fatigue, and the lowest were for somatic symptoms, with intermediate scores for cognitive function and for emotion. All subscales showed a similar reduction (in average patient scores) of approximately 50% postintervention, with the reduction in score relating to a decrease in the severity of symptoms.
Table 2.
Changes in PFRS sub-scales for complete cases from baseline to 3 months
| Complete cases | No. items | Max poss. score | Baseline | 3 Months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subscale | N | Mean (SD) | Median (IQR) | Range | N | Mean (SD) | Median (IQR) | Range | ||
| Emotional | 15 | 90 | 19 | 36.8 (22.3) | 39 (15–59) | 9–80 | 18 | 18.9 (13.9) | 17 (6–30) | 0–51 |
| Cognitive | 11 | 66 | 19 | 28.0 (14.1) | 26 (19–40) | 2–51 | 17 | 13.5 (9.6) | 13 (9–16) | 0–34 |
| Fatigue | 12 | 72 | 19 | 43.9 (14.8) | 47 (33–57) | 16–67 | 18 | 19.9 (14.5) | 16 (9–31) | 0–48 |
| Somatic | 16 | 96 | 20 | 23.3 (10.1) | 20 (16–31) | 7–43 | 18 | 11.6 (7.3) | 11 (8–14) | 0–33 |
| PFRS total | 54 | 324 | 18 | 130.1 (49.7) | 118 (82–176) | 73–208 | 15 | 62.5 (37.2) | 58 (43–87) | 0–147 |
IQR, interquartile range; PFRS, profile of fatigue-related states.
Table 3.
Changes in PFRS sub-scales for using mean-item imputation from baseline to 3 months
| Mean-item imputation | No. items | Max poss. score | Baseline | 3 months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subscale | N | Mean | Median | Range | N | Mean | Median | Range | ||
| Emotional | 15 | 90 | 20 | 38.5 | 39 | 9–80 | 19 | 17.9 | 15 | 0–51 |
| Cognitive | 11 | 66 | 20 | 29.7 | 27 | 2–63 | 20 | 13.1 | 12 | 0–34 |
| Fatigue | 12 | 72 | 20 | 43.9 | 47 | 16–67 | 20 | 19.9 | 16 | 0–48 |
| Somatic | 16 | 96 | 20 | 23.3 | 20 | 7–43 | 20 | 10.9 | 11 | 0–33 |
| PFRS Total | 54 | 324 | 20 | 135.3 | 141 | 73–208 | 19 | 62.6 | 56 | 0–147 |
PFRS, profile of fatigue-related states.
A weak rank correlation (Spearman’s ρ = 0.34) was found between the number of treatment sessions and reduction in total PFRS score, as a marker of overall symptomatology.
Discussion
Although an uncontrolled study, our results potentially suggest that a manual lymphatic technique could have benefit for Long COVID patients, as indicated by improvement in PFRS fatigue scores in our Long COVID patients. It may be that early intervention and supportive treatments at the end of the acute phase of COVID-19 can help to lessen acute phase symptoms and prevent them from becoming chronic/enduring. We have described in this report how one type of alternative intervention could potentially achieve this goal.
Any intervention that can improve energy and activity levels in people with Long COVID will have health benefits in terms of reduction in cardiometabolic risk, given the potential for Long COVID to lead to weight gain [14].
As this was not a controlled trial, we cannot state that the specific treatment given is superior to no treatment/usual care as it is recognized that in many individuals post-COVID/Long COVID symptoms decline over 60–90 days follow-up without intervention [15]. Nevertheless, without effective therapeutic interventions in place, managing these Post-COVID-19 syndrome cases, in addition to existing clinical workloads, will place additional burdens on our already hard-pressed healthcare systems in the UK, and elsewhere in the world.
PFRS scale scores are significantly related to work status, reported disability, lived experience of ongoing fatigue, and to the perceived course of the illness [9] and, hence, the utilization of the PFRS in this study.
In light of the above considerations, we suggest that priority be given to explore pragmatic relatively low-cost techniques as presented in this article. Also the addition of these techniques may enhance the multidisciplinary approach established by Halpin et al. [3] in the UK to treat the postviral fatigue-related states, to alleviate symptoms and to improve the quality of life for those affected by the longer term sequelae of COVID-19. This approach may have the additional benefit of preventing to some significant degree the emergence of postviral symptoms that are resistant to treatment.
The average cost per patient of the intervention that we describe is £450 (approximately $620). If the intervention is found to be efficacious in controlled trials, it would be subject to full health economic evaluation by UK Institute for Health and Care Excellence prior to being adopted by the National Health Service. We are shortly to embark on a funded feasibility study of the self-help treatment element described in this intervention (IRAS 291940), in order formally to evaluate its efficacy.
Study limitations
This was an uncontrolled study with a relatively small number of patients. In addition, data were not collected on patient application of the assigned daily self-help exercises of contrast bathing and spinal mobility exercises.
In addition, people undergoing this intervention were self-pay as this treatment is not routinely provided by the National Health Service. This might mean that the type of patients in whom these results were found are not representative of the affected population of Long COVID sufferers.
The above point might include older individuals who were not included in the study who may have more severe symptoms of Long COVID. It is anticipated that any formal evaluation of this intervention will include more people over the age of 50 years.
Like many questionnaires, the overall PFRS score and its subscales are a summation of individual ordinal items and, as such, have no dimensionality (i.e. units to quantify it). Thus, a 50% reduction in scores does not equate to a halving of symptoms in patients.
Conclusion
This uncontrolled study suggested that a specific manual lymphatic technique may have benefit for Long COVID patients. It may be that early intervention and supportive treatments at the end of the acute phase of COVID-19 can help overcome acute phase symptoms and prevent them becoming chronic/enduring, while also improving activity levels. Potentially, this exploratory study could be a first step in helping people with Long COVID back to health.
Acknowledgements
The authors would like to thank the members of the Perrin Technique Practitioner Network who contributed anonymized patient data for inclusion in this analysis.
R.P. led on the writing of the article with contributions in terms of literature search and current perspective from L.R., A.W., and A.H. M.S. undertook the statistical analysis regarding PFRS change scores, and M.H. provided statistical advice and undertook the subscale PFRS analysis. A.M. provided further academic input and also senior review. All authors contributed to the final version of the manuscript and approved the final version.
The NIHR Greater Manchester Patient Safety Translational Research Centre supported L.R. (award number: PSTRC-2016-003). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflicts of interest
R.P. developed the Perrin Technique which was used in this case series. For the remaining authors, there are no conflicts of interest.
References
- 1.Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: post-viral syndrome post COVID-19. Med Hypotheses 2020;144:110055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol 2011;11:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halpin S, O’Connor R, Sivan M. Long COVID and chronic COVID syndromes. J Med Virol 2021;93:1242–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wostyn P. COVID-19 and chronic fatigue syndrome: is the worst yet to come? Med Hypotheses 2021;146:110469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meinhardt J, Radke J, Dittmayer C, Franz J, Thomas C, Mothes R, et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat Neurosci 2021;24:168–175. [DOI] [PubMed] [Google Scholar]
- 6.Rhea EM, Logsdon AF, Hansen KM, Williams LM, Reed MJ, Baumann KK, et al. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nat Neurosci 2021;24:368–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perrin RN, Edwards J, Hartley P. An evaluation of the effectiveness of osteopathic treatment on symptoms associated with myalgic encephalomyelitis. A preliminary report. J Med Eng Technol 1998;22:1–13. [DOI] [PubMed] [Google Scholar]
- 8.Perrin RN. The Perrin technique 2nd edition. How to diagnose and treat chronic fatigue syndrome/ME and fibromyalgia via the lymphatic drainage of the brain. Chap 10: Treating the patient. Hammersmith Press; 2021; pp.272–308. [Google Scholar]
- 9.Ray C, Weir WRC, Phillips L, Cullen S. Development of a measure of symptoms in chronic fatigue syndrome: the profile of fatigue related symptoms (PFRS). Psychol Health 1992;7:27–43. [Google Scholar]
- 10.Cicchitti L, Martelli M, Cerritelli F. Chronic inflammatory disease and osteopathy: a systematic review. PLoS One 2015;10:e0121327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rist PM, Hernandez A, Bernstein C, Kowalski M, Osypiuk K, Vining R, et al. The impact of spinal manipulation on migraine pain and disability: a systematic review and meta-analysis. Headache 2019;59:532–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomas E, Cavallaro AR, Mani D, Bianco A, Palma A. The efficacy of muscle energy techniques in symptomatic and asymptomatic subjects: a systematic review. Chiropr Man Therap 2019;27:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell ML, Fairclough DL, Fiero MH, Butow PN. Handling missing items in the Hospital Anxiety and Depression Scale (HADS): a simulation study. BMC Res Notes 2016;9:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaggwa MM, Favina A, Najjuka SM, Zeba Z, Mamun MA, Bongomin F. Excessive eating and weight gain: a rare post-acute COVID-19 syndrome. Diabetes Metab Syndr 2021;15:102252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021;397:220–232. [DOI] [PMC free article] [PubMed] [Google Scholar]