Abstract
Odronextamab is a fully‐human IgG4‐based CD20xCD3 bispecific antibody that binds to CD3 on T cells and CD20 on B cells, triggering T‐cell‐mediated cytotoxicity independent of T‐cell‐receptor recognition. Adequate safety, tolerability, and encouraging durable complete responses have been observed in an ongoing first‐in‐human (FIH) study of odronextamab in patients with relapsed/refractory (R/R) B‐cell non‐Hodgkin lymphoma (B‐NHL; NCT02290951). We retrospectively evaluated the pharmacokinetic, pharmacodynamic, and antitumor characteristics of odronextamab in a series of in vitro/in vivo preclinical experiments, to assess their translational value to inform dose escalation for the FIH study. Half‐maximal effective concentration values from in vitro cytokine release assays (range: 0.05–0.08 mg/L) provided a reasonable estimate of odronextamab concentrations in patients associated with cytokine release at a 0.5 mg dose (maximum serum concentration: 0.081 mg/L) on week 1/day 1, which could therefore be used to determine the week 1 clinical dose. Odronextamab concentrations resulting in 100% inhibition of tumor growth in a Raji xenograft tumor mouse model (1–10 mg/L) were useful to predict efficacious concentrations in patients and inform dose‐escalation strategy. Although predicted human pharmacokinetic parameters derived from monkey data overestimated projected odronextamab exposure, they provided a conservative estimate for FIH starting doses. With step‐up dosing, the highest‐tested weekly odronextamab dose in patients (320 mg) exceeded the 1 mg/kg single dose in monkeys without step‐up dosing. In conclusion, combination of odronextamab in vitro cytokine data, efficacious concentration data from mouse tumor models, and pharmacokinetic evaluations in monkeys has translational value to inform odronextamab FIH study design in patients with R/R B‐NHL.
Study Highlights.
WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?
Odronextamab is an IgG4‐based CD20xCD3‐targeting bispecific antibody being evaluated in a first‐in‐human (FIH) study in patients with relapsed/refractory (R/R) B‐cell non‐Hodgkin lymphoma (B‐NHL). Preliminary clinical data indicate adequate safety and tolerability, and encouraging response rates.
WHAT QUESTION DID THIS STUDY ADDRESS?
This retrospective analysis assessed the translational value of odronextamab preclinical data to inform FIH study design.
WHAT DOES THIS STUDY ADD TO OUR KNOWLEDGE?
In vitro cytokine data, efficacious concentration data in Raji xenograft tumor mouse models, and pharmacokinetic evaluations in cynomolgus monkeys have translational value to inform the odronextamab starting dose and dose escalation strategy, but not the projected target dose, for the FIH study in patients with R/R B‐NHL.
HOW MIGHT THIS CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE?
These data demonstrate the value of odronextamab preclinical data to aid efficient FIH clinical study design, some aspects of which may be generalized qualitatively to other bispecific antibodies.
INTRODUCTION
Bispecific antibodies (bsAbs) represent a novel class of immunotherapy in which the antibody structure features two different antigen‐binding sites, allowing it to bind to two distinct epitopes. 1 In the context of B‐cell malignancies, T‐cell‐engaging bsAbs allow efficient T‐cell‐mediated killing of B cells, previously unachievable with naked B‐cell‐targeting antibodies alone. 1 , 2
Odronextamab (REGN1979), a CD20xCD3‐targeting bsAb, is currently being evaluated for the treatment of CD20+ B‐cell malignancies, such as diffuse large B‐cell lymphoma and follicular lymphoma, and is designed to cross‐link and activate CD3‐expressing T cells upon contact with CD20+ B cells, triggering redirected T‐cell killing of B cells. 2 , 3 Early preclinical data showed that odronextamab induced target‐dependent T‐cell‐mediated lysis of B cells in vitro, displayed potent antitumor efficacy in mouse tumor models, and potently depleted B cells in cynomolgus monkeys. 2 Odronextamab is a fully human immunoglobulin (Ig)G4‐based anti‐CD20xCD3 bsAB, which has several advantages associated with native antibodies, including good stability, low tendency to aggregate, low immunogenicity, and favorable pharmacokinetics (PK) in monkeys. 2
An important challenge for first‐in‐human (FIH) studies of bsAbs is to determine appropriate dosing steps and regimens for dose escalation, including step‐up dose, full dose, and dosing frequency. These optimizations can mitigate known safety concerns of T‐cell targeting therapy, such as cytokine release syndrome (CRS) in early weeks following treatment initiation, while providing a robust antitumor response. 4 Preliminary data from the dose‐escalation portion of the FIH odronextamab monotherapy study (NCT02290951) demonstrated that it has an acceptable safety profile and is associated with clinically meaningful, durable complete responses in heavily pretreated patients with relapsed/refractory (R/R) B‐cell non‐Hodgkin lymphoma (B‐NHL). 5 , 6
The purpose of this paper is to collectively evaluate the PK, pharmacodynamic, and antitumor characteristics of odronextamab in a series of in vitro and in vivo preclinical experiments, and to retrospectively assess how these data could be used to inform the clinical development of odronextamab. Specifically, we address the following questions:
Can relevant in vitro experiments be designed to identify the concentration range of odronextamab associated with transient cytokine release in patients?
Which preclinical data are useful for the selection of the initial dose for dose escalation and minimal efficacious clinical doses of odronextamab in patients?
Which preclinical data may be supportive for selection of higher odronextamab doses for evaluation in patients?
What are the limitations of the preclinical data, in the context of their translational value?
Hence, we compare preclinical odronextamab data with preliminary data from the FIH study to assess their translational value to inform dose escalation for the FIH study. The results suggest that data from in vitro cytokine experiments, in vivo mouse models, and monkey PK and toxicity data have translational value for the FIH study design of odronextamab in patients with R/R B‐cell malignancies, which is potentially useful for the FIH study design of other bsAbs.
METHODS
In vitro whole blood cytokine release assay
An in vitro assay, in which human whole blood samples (Bioreclamation and HemaCare Corp.) were incubated with odronextamab or a control antibody with no binding affinity for CD20 or CD3, was used to evaluate cytokine release (interferon‐γ, interleukin 6, and tumor necrosis factor‐α [IFN‐γ, IL‐6, and TNF‐α]). These whole blood samples were used as a source of CD3 T cells and CD20 B cells from healthy donors. Cytokine concentrations were analyzed with the Human ProInflammatory‐4 Plex Kit (Meso Scale Discovery®), following the manufacturer’s instructions. The half‐maximal effective concentration (EC50) values for cytokine release were determined using GraphPad PrismTM software with values calculated using a four‐parameter non‐linear regression analysis: Y = bottom + (top‐bottom) / (1 + 10^((LogEC50‐X)*HillSlope)). The median and range of EC50 values, and maximum cytokine detected in the plasma, were obtained from 10 independent experiments.
Additional details for the in vitro whole blood assay are included in Supplementary Methods.
In vitro cytotoxicity and cytokine release in lymphoma cell lines
The ability of odronextamab to mediate target‐dependent tumor lysis of various CD20+ lymphoma cell lines by human T cells was determined using a multi‐day fluorescent activated cell sorting‐based cytotoxicity assay. Lymphoma cell lines were selected based on (a) representation of a variety of NHL subtypes, (b) CD20 expression level, and (c) regular use in mouse in vivo tumor models.
Human peripheral blood mononuclear cells (PBMCs) were plated in complete media at 1 × 106 cells/ml and incubated overnight at 37°C to deplete adherent cells. CD20‐expressing Nalm6 tumor cells (1 × 106/ml) were labeled with 1 μM Violet Cell Tracker fluorescent tracking dye, plated at 0.25 × 106/ml in 50 µl media and incubated overnight at 37°C, whereas other CD20‐expressing tumor cell lines (Raji, Raji‐Luc, Ramos, WSU‐DLCL2, 2.5 × 106/ml) were each labeled with 1 μM CFDA‐SE fluorescent tracking dye on the day of assay set up.
The following day, the PBMCs (5 × 106/ml) were labeled with 1 μM Violet Cell Tracker fluorescent tracking dye, except in the Nalm6 experiment where PBMCs were not labeled. All labeled tumor cells (2.5 × 104/ml) were plated with labeled PBMCs (effector/target cell ratio 10:1 for Raji and Raji‐Luc; 5:1 for WSU‐DLCL2 and Ramos; 8:1 for Nalm6 [non‐labeled PBMCs]) and serial dilutions of odronextamab or IgG1 isotype control in complete media for 48–96 h at 37°C. Surviving target cells and T‐cell activation were analyzed by flow cytometry as previously described. 7
At the end of culture, cells were washed with cold phosphate‐buffered saline and stained with a LIVE/DEAD Fixable Dead Cell Stain to identify viable cells. To assess Nalm6 killing, cells were gated on live violet‐labeled populations. For assessment of Raji, Raji‐Luc, Ramos, and WSU‐DLCL2 killing, cells were gated on live CFDA‐SE populations. The percent live population was recorded and used to calculate survival. Percent viability was normalized to control condition (target cells in the presence of PBMCs only). Cytotoxicity in Raji cells was also determined in the presence of dexamethasone 300 nM.
Levels of cytokines (including IL‐6/TNF‐α/IFN‐γ) in cell‐culture supernatants from the Raji cytotoxicity study in the presence or absence of dexamethasone were quantified using a BD Cytometric Bead Array Human Th1/Th2/Th17 Cytokine Kit according to the manufacturer’s instructions.
EC50 values for cytokine release were determined using GraphPad PrismTM software with values calculated using a four‐parameter nonlinear regression analysis.
Antitumor effect in mouse tumor models and odronextamab exposures
Raji cell xenograft tumor models in mice were established to evaluate the in vivo PK and antitumor effects of odronextamab. Female non‐obese diabetic (NOD) severe combined immunodeficiency (scid) gamma mice (NOD‐scid IL2Rgamma‐null [NSG]) ~6 weeks old at study initiation were used (Jackson Laboratories). In these mice, the scid mutation and loss of IL‐2 receptor γ‐chain leads to a deficiency in mature B cells, T cells, and natural killer cells, allowing for engraftment of human hematopoietic stem cells 8 or PBMCs. 9
Human PBMCs were obtained from a single healthy donor (Reach Bio), stored in liquid nitrogen, and thawed immediately before use. Mice were implanted subcutaneously with a mixture of Raji cells (2 × 106/mouse) and human PBMCs (5 × 105/mouse). Ten days later, 50 mice (mean tumor volume, 220 ± 41 mm3) were grouped (10 per cohort) to receive odronextamab 0.04, 0.1, 0.4, or 1.0 mg/kg, or vehicle control (phosphate‐buffered saline). Mice received a single intraperitoneal injection of odronextamab or vehicle the following day (day 0).
Blood was collected 4 h and 1, 2, 3, 7, 14, and 21 days postdose to determine serum concentrations of odronextamab using the GyroLab xPlore platform (Gyros) immunoassay (see Supplementary Methods). Mice were weighed and tumor growth measured twice weekly using calipers (tumor volume = [length × width2]/2). Statistical analysis was performed using tumor volumes on day 21 and two‐way analysis of variance with GraphPad PrismTM software.
All experiments were approved by the Regeneron Institutional Animal Care and Use Committee (IACUC) and performed in accordance with approved guidelines.
Pharmacokinetics and cytokine release in cynomolgus monkeys
Odronextamab PK, and the relationship between odronextamab concentrations and cytokine release, were determined in cynomolgus monkeys following single or multiple intravenous (i.v.) dose(s). Full details for housing and care are provided in Supplementary Methods. All procedures were followed in compliance with applicable animal welfare acts, approved by the local IACUC, and carried out in accordance with approved guidelines.
For the PK concentration–time profile (derived from two independent studies), animals were randomized to receive a single i.v. infusion of odronextamab 0.001, 0.01, 0.1 mg/kg (four males per cohort), or 1 mg/kg (two females). Blood samples were collected throughout the timecourse of the study. For cytokine analysis, animals received an i.v. infusion of odronextamab 0.01, 0.1, or 1 mg/kg (n = 6 per cohort, mixture of male and female mice), and blood samples were collected at 5 min, 5 h, and 24 h postdose. Odronextamab was formulated in an aqueous buffered vehicle, pH 5.8, containing 10 mM histidine, 10% (w/v) sucrose, and 0.1% (w/v) polysorbate 80, to provide a nominal protein concentration of either 25 or 100 mg/ml.
Bioanalytical methodology for evaluation of total odronextamab concentration in monkey serum, and cytokine analysis methodology in plasma, are described in Supplementary Methods.
Predictions of odronextamab exposure in humans
The PK of odronextamab in monkeys demonstrated some degree of nonlinearity, likely due to target‐mediated clearance, evidenced by accelerated elimination during the terminal phase in single‐dose PK studies and greater than dose‐proportional increases for exposure (area under the curve) between lower (<0.01 mg/kg) dose levels. However, the observed monkey clearance values (range 7.4–13.0 ml/day/kg, which converts to 0.308–0.542 ml/h/kg) and volume of distribution values (75.4–79.8 ml/kg) for odronextamab in the PK study were within a similar range and consistent with examples of other human IgG1, IgG2, and IgG4 antibody PK in monkeys described in the literature (clearance of 0.14–0.55 ml/h/kg and volume of distribution of 46–71 ml/kg) that were characterized by linear kinetics. 10 , 11 , 12 Thus, for the purpose of predicting odronextamab PK parameters and exposures in humans, no direct allometric scaling was performed, but instead, typical human clearance and volume of distribution values were used with a standardized two‐compartment linear PK model of IgG1, IgG2, and IgG4 monoclonal antibodies. 13 NONMEM software (version 7.4.1; ICON Development Solutions) was used for predicting human exposure. A schematic depiction of a two‐compartment linear model following i.v. administration is provided in Supplementary Table S1.
Odronextamab exposure in humans
Odronextamab serum concentration data were obtained from the dose‐escalation portion of the FIH clinical study R1979‐HM‐1333 (NCT02290951), 5 in which odronextamab was administered intravenously in patients with R/R B‐NHL. A step‐up dosing strategy was implemented during the dose escalation. During the step‐up dosing period, the doses administered were evenly split into two infusions on two consecutive days of each week. 6 Bioanalytical methodology for evaluation of total odronextamab concentration in human serum, and cytokine analysis methodology (including IFN‐γ, IL‐6, and TNF‐α), are described in Supplementary Methods.
The protocol for study R1979‐HM‐1333 was approved by relevant institutional review boards/ethics committees and conducted in accordance with the International Conference on Harmonisation Good Clinical Practice guidelines, and the Declaration of Helsinki for Studies Involving Human Subjects. All participants gave written informed consent.
Utilizing preclinical data to inform design of the odronextamab FIH study
The odronextamab starting dose and dose‐escalation increments for the FIH study (NCT02290951) 5 were informed by the totality of the nonclinical pharmacology, tolerability, and PK data in animals. In mice, data from a Raji tumor‐bearing NSG mouse xenograft model were used to project the effective concentration range in humans. In this mouse xenograft model, complete suppression of tumor growth was demonstrated at a dose range of 0.4–1 mg/kg, and the odronextamab concentration range in mice was used to evaluate the effective concentration range in humans.
In monkeys, a conventional two‐compartment linear PK model of odronextamab was used, with serum concentration data from single‐ and multiple‐dose studies in cynomolgus monkeys in conjunction with typical human antibody values of clearance and volume of distribution, to predict the PK parameters and exposure profiles of odronextamab in humans at predefined dose cohorts of the FIH study for the dose escalation. For data analysis, projected concentrations at week 1 for each cohort were evaluated against the observed concentrations in patients. Additional methodology for the PK analysis of total odronextamab concentrations in cynomolgus monkey serum is described in Supplementary Methods.
To manage CRS during dose escalation in the clinic, an intrapatient step‐up dosing approach with premedication (e.g., steroids) was used for each dose cohort, to control the intensity of cytokine release. Dose ranges to be evaluated were 0.03–1 mg at week 1, 0.1–20 mg at week 2, and 12–320 mg from weeks 3–12 during dose escalation. Selection of the first dose level in humans (i.e., 0.03 mg at week 1 and 0.1 mg at week 2) was based primarily on estimated EC50 values from in vitro cytokine release assays for IL‐6, IFN‐γ, and TNF‐α. Selection of the highest dose tested in patients was based on odronextamab exposures at 1 mg/kg in a 5‐week toxicokinetic study in cynomolgus monkeys, in combination with safety profiles observed during dose escalation in patients. The 1 mg/kg dose was the highest non‐step‐up dose regimen tested, and was well tolerated in monkeys.
RESULTS
Odronextamab‐induced in vitro cytokine release in human whole blood
The in vitro EC50 values and maximal concentrations of IL‐6, TNF‐α, and IFN‐γ elicited by odronextamab or a nonbinding control antibody in whole blood from multiple human donors are summarized in Figure 1. Median EC50 values ranged from 0.3–0.5 nM (or 0.05–0.08 mg/L) for these cytokines. Donor‐to‐donor variability in EC50 values and maximum concentration was observed. Dose‐dependent cytokine profiles for a single representative donor are shown in Figure 2a, demonstrating maximal IL‐6, TNF‐α, and IFN‐γ concentrations observed at odronextamab concentrations greater than 1 nM (or >0.15 mg/L).
FIGURE 1.

Odronextamab‐induced cytokine release in human whole blood samples from multiple donors: EC50 (a) and maximum cytokine release (b). Data points represent individual donors. Box‐and‐whisker plots represent the median (central line), 25/75 percentiles (box), and min/max range (whiskers). Reported LLODs per Meso Scale Diagnostics documentation for Human ProInflammatory 4‐Plex Ultra‐Sensitive Kit: IFN‐γ, 0.40 pg/ml; IL‐6, 0.22 pg/ml; TNF‐α, 0.49 pg/ml. EC50, half‐maximal effective concentration; IFNγ, interferon‐γ; IL‐6, interleukin 6; LLOD, lower limit of detection; TNF‐α, tumor necrosis factor‐α
FIGURE 2.
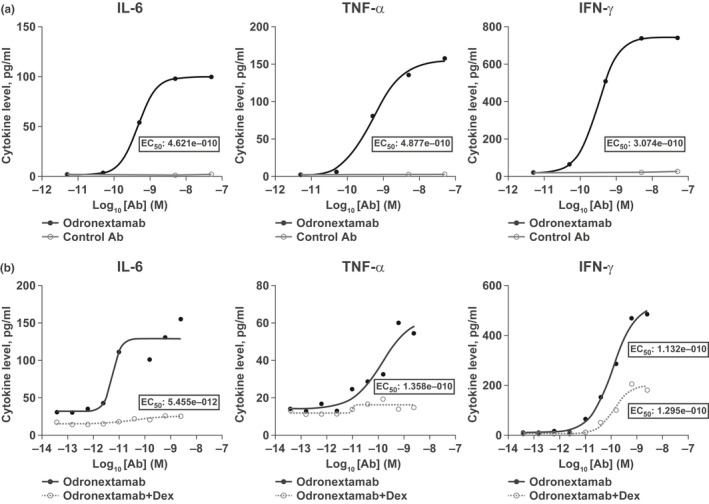
Odronextamab‐induced in vitro cytokine release is reduced in the presence of dexamethasone. In vitro cytokine profiles in (a) human whole blood samples from a healthy donor incubated with odronextamab or control antibody and (b) a 96‐h co‐culture assay with Raji and human PBMCs in the presence or absence of dexamethasone 300 nM. EC50 values for cytokine release were determined using GraphPad PrismTM software, with values calculated using a four‐parameter nonlinear regression analysis. Panel 1a shows representative data from one of 9–10 independent donors evaluated in single wells per condition. In Panel 1b, Raji +/− Dex was performed a single time; cytokines were evaluated from one assay well per condition. Ab, antibody; Dex, dexamethasone; EC50, half‐maximal effective concentration; IFN‐γ, interferon‐γ; IL‐6, interleukin 6; PBMCs, peripheral blood mononuclear cells; TNF‐α, tumor necrosis factor‐α
In a separate whole blood assay that used CD3/CD28 stimulation beads as a positive control, the maximum cytokine release induced by odronextamab was generally lower than that induced by control beads (Supplementary Figure S1).
Effect of dexamethasone on odronextamab‐induced in vitro cytokine release following co‐culture with Raji cells
In 96‐h co‐culture assays with Raji and PBMCs in the presence or absence of 300 nM dexamethasone, in vitro cytokine profiles for release of IL‐6, TNF‐α, and IFN‐γ were observed at odronextamab concentrations ranging from 1 pM to 100 nM (Figure 2b). Dexamethasone reduced odronextamab‐induced elevations in IL‐6, TNF‐α, and IFN‐γ.
Odronextamab in vitro cytotoxicity in lymphoma cell lines
In co‐culture assays with CD20‐expressing lymphoma cells and PBMCs, a low picomolar concentration of odronextamab was capable of mediating cytotoxicity of all CD20‐expressing lymphoma cells tested (Figure 3a–d); EC50 values for cytotoxicity were in a range of 3–25 pM. Across all lymphoma cell lines, maximum cytotoxicity occurred at odronextamab concentrations of 1–10 nM (i.e., 0.15–1.5 mg/L) and the cytotoxicity of odronextamab against the Raji cell line was unaffected by the presence of dexamethasone (Figure 3e).
FIGURE 3.
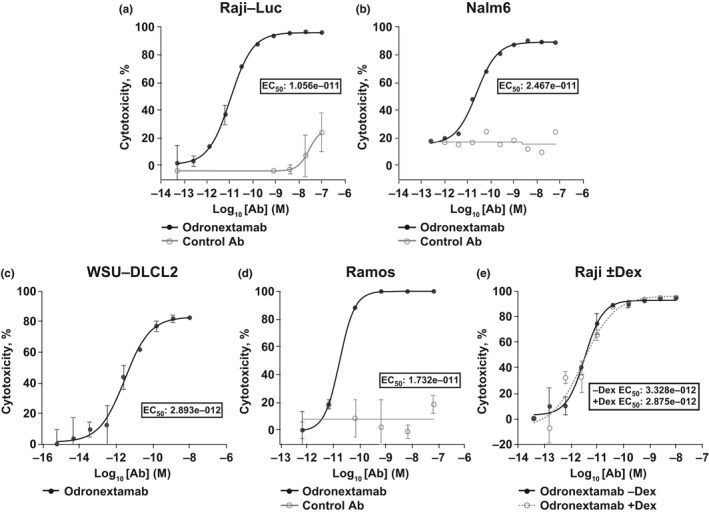
In vitro cytotoxicity of odronextamab against various CD20‐expressing lymphoma cell lines (a–d), and Raji cells in the presence of dexamethasone (e). Each plot shows representative results from independent experiments (Panel 2a: n = 11 experiments; 2b: n = 7 experiments; 2c: n = 5 experiments; 2d: n = 4 experiments; and 2e: n = 1 experiment). EC50 values were determined using GraphPad PrismTM software, with values calculated using a four‐parameter non‐linear regression analysis. Panels 2a, 2c, 2d, and 2e were performed in duplicate, with average values and standard deviations plotted; Panel 2b was performed in a single well per condition. Ab, antibody; Dex, dexamethasone; EC50, half‐maximal effective concentration
Odronextamab exposure and antitumor effect in a mouse tumor model
In the mouse tumor model, odronextamab concentrations in serum were quantified over the 21‐day study period at doses 0.04, 0.1, 0.4, and 1 mg/kg following a single intraperitoneal dose (Figure 4a). The drug concentration increased dose‐dependently and showed apparent target‐mediated elimination at 0.04 mg/kg dose. With odronextamab 0.4 and 1 mg/kg, serum concentrations remained greater than 1 μg/ml throughout the study (Figure 4a).
FIGURE 4.
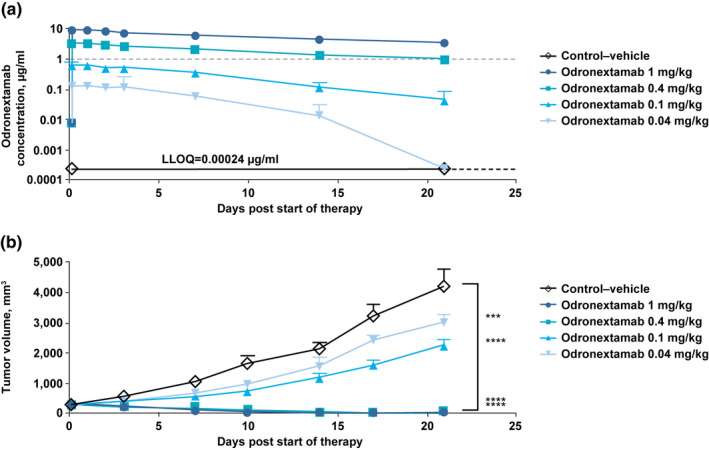
Odronextamab exposure (a) and antitumor effects (b) in immunocompromised nonobese diabetic (NOD) severe combined immunodeficiency (scid) γ mice bearing Raji cell xenografts. In NSG mice bearing Raji tumors co‐implanted with human PBMCs, single‐dose odronextamab (0.04, 0.1, 0.4, and 1.0 mg/kg) was administered intraperitoneally on day 0 when average tumor volume reached 220 mm3. Tumor volume in each treatment group was measured twice weekly and averages (mm3 ± SEM) are plotted. Grouped two‐way ANOVA (day 21) was performed using GraphPad PrismTM software. In Panel 3a, the gray dashed line represents a reference concentration of 1 µg/ml, at which a complete inhibition of tumor growth was achieved. In Panel 3b, asterisks indicate statistically significant differences in average tumor volume on day 21 compared with vehicle control group (***p ≤ 0.001; ****p ≤ 0.0001). ANOVA, analysis of variance; LLOQ, lower limit of quantification; NSG, NOD‐scid IL2Rgammanull; PBMCs, peripheral blood mononuclear cells; SEM, standard error of the mean
Changes in tumor volume over time with odronextamab treatment are shown in Figure 4b. In mice receiving odronextamab 0.4 or 1 mg/kg (drug concentration 1–10 µg/ml), complete tumor suppression was achieved over the observation period. Although tumor growth was slowed in mice receiving odronextamab 0.04–0.1 mg/kg (drug concentration <1 µg/ml over the observation period) compared with control‐treated mice, only the two highest doses tested (odronextamab 0.4 and 1 mg/kg, drug concentration 1–10 µg/ml) resulted in complete suppression (p ≤ 0.001 vs. vehicle control).
Odronextamab pharmacokinetics and cytokine release in cynomolgus monkeys
Following a single i.v. infusion in cynomolgus monkeys, mean concentration–time profiles were characterized by an initial distribution phase followed by a bi‐phasic elimination phase, consisting of a saturating beta‐elimination phase and a terminal target‐mediated elimination phase (Figure 5a). In general, the PK of odronextamab are described by linear kinetics at doses greater than or equal to 0.01 mg/kg. Additional PK analysis of total odronextamab concentrations in cynomolgus monkey serum is provided in Supplementary Table S2.
FIGURE 5.

Mean concentration–time profiles for odronextamab at various dosesa (a) and relationship between mean odronextamab Cmax and mean peak IL‐6 level on day 1 following i.v. infusionb (b) in cynomolgus monkeys. aConcentration versus time profiles were imputed to ½ LLOQ. bIL‐6 production at 5 h following i.v. administration of odronextamab 0.01, 0.1, and 1 mg/kg. Cmax, maximum concentration; IL‐6, interleukin 6; i.v., intravenous; LLOQ, lower limit of quantification
In addition, levels of cytokines produced following i.v. dosing were assessed to understand the pharmacodynamic relationship between peak odronextamab concentrations (Cmax) and peak IL‐6 concentrations. Peak concentrations of IL‐6 increased with odronextamab Cmax following a single dose of 0.01, 0.1, and 1 mg/kg and maximal IL‐6 level was more than 2000 pg/ml (Figure 5b).
Comparison of projected and observed odronextamab concentrations in patients
A standardized two‐compartment linear PK model was used to project odronextamab exposure in humans. The projected and observed exposure data in patients with B‐NHL at week 1 are provided in Table 1. Odronextamab concentration at the 0.03 mg dose was not quantifiable in patients.
TABLE 1.
Predicted and observed odronextamab exposure in patients with B‐cell non‐Hodgkin lymphoma
| Odronextamab dose in week 1 (mg) |
Predicted mean concentration (mg/L) a |
Observed mean (SD) concentration (mg/L) b | ||
|---|---|---|---|---|
| Cmax | Ctrough | Cmax | Ctrough | |
| 0.1 | 0.038 | 0.022 |
0.024 (0.020) (n = 7) |
0.0006 (0.0017) (n = 7) |
| 0.3 | 0.112 | 0.051 |
0.031 (0.037) (n = 7) |
0.0032 (0.0052) (n = 6) |
| 0.5 | 0.187 | 0.113 |
0.081 (0.046) (n = 5) |
0.0009 (0.0020) (n = 5) |
| 1 | 0.375 | 0.225 |
0.196 (0.024) (n = 79) |
0.0212 (0.0191) (n = 76) |
Abbreviations: Cmax, maximum concentration; Ctrough, trough concentration prior to the first dose of week 2; LLOQ, lower limit of quantification; SD, standard deviation.
Predicted exposures are based on a two‐compartment linear pharmacokinetic model using exposure data in cynomolgus monkeys. LLOQ in monkeys: 0.00313 mg/L.
Observed concentration data are based on the odronextamab first‐in‐human study. LLOQ in humans: 0.003 mg/L.
In the dose range of 0.1–1 mg at week 1, the projected human Cmax values for odronextamab were two to fourfold higher than the observed Cmax values in patients. Compared with measured concentration in patients, trough odronextamab concentrations (Ctrough) were not well predicted, as predicted values were greater than 10‐fold higher than observed values.
At odronextamab doses less than or equal to 0.5 mg, a single infusion was administered in patients. The 1 mg dose was the highest tested at week 1 and was split into two infusions (0.5 mg/0.5 mg) on two consecutive days. At the 0.5 mg dose, the mean odronextamab Cmax was 0.081 mg/L, which was at the upper range of the in vitro EC50 (0.05–0.08 mg/L) for cytokine release. On day 2 of week 1, the mean Cmax was 0.196 mg/L following the 1 mg split dose; most cytokines peaked on day 1 of week 1 and returned to baseline prior to the second 0.5 mg dose. 14 These data support the use of a split dosing strategy in the early weeks of treatment.
Following initial dosing of odronextamab, transient cytokine release generally occured in weeks 1–2. 14 Individual Cmax of IL‐6 at week 1 and week 2 versus corresponding Cmax of odronextamab is depicted in Figure 6. Peak IL‐6 concentrations were highly variable. In week 1 and week 2, the mean (coefficient of variation %) was 640 (199%) and 475 (258%) pg/ml, respectively, and the median (range) was 133 (3–7550) and 38 (5–7100) pg/ml, respectively. There was no correlation between peak IL‐6 values and odronextamab Cmax.
FIGURE 6.
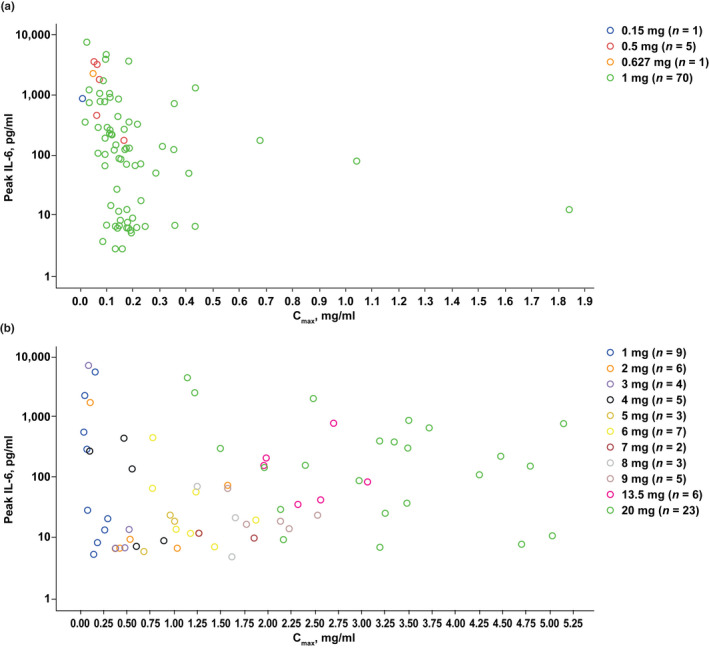
Individual IL‐6 peak concentration versus odronextamab Cmax in week 1 (a) and week 2 (b) of treatment in patients with B‐cell non‐Hodgkin lymphoma. Note: Odronextamab serum concentration data taken from the dose‐escalation portion of the FIH clinical study R1979‐HM‐1333 (NCT02290951). 5 n = number of patients in each dose group; color represents different dose group. Cmax, maximum concentration; FIH, first‐in‐human; IL‐6, interleukin 6
In the FIH study of odronextamab, the maximum tolerated dose was not reached, and 320 mg was the highest dose tested. 6 The efficacious concentration range of 1–10 mg/L observed at doses of 0.4–1 mg/kg in the mouse xenograft model (Figure 4) was similar to the efficacious serum concentration previously reported in patients with follicular lymphoma, 15 given that the antitumor effects of odronextamab are generally observed at greater than or equal to 5 mg in this subgroup. 6
DISCUSSION
Odronextamab is a CD20xCD3‐targeting bsAb currently being evaluated clinically for the treatment of CD20+ B‐cell malignancies. Early clinical experience from the FIH study demonstrates that odronextamab can achieve durable complete responses in heavily pretreated patients with B‐NHL. The overall safety profile favors continued investigation of odronextamab in this setting. 6
In this retrospective analysis, we present key data from preclinical in vitro assays and in vivo animal studies of odronextamab, and summarize observed odronextamab serum concentrations in patients during the early weeks of treatment in the FIH study. Below, we discuss the translational value of various aspects of these preclinical data.
Projecting odronextamab exposures in humans
If a monoclonal antibody demonstrates linear PK properties in cynomolgus monkeys, it has been shown that these data alone can successfully predict clearance within twofold of the starting dose in humans. 16 In monkeys, odronextamab PK profiles at concentrations greater than 0.01 mg/ml generally showed linear kinetics (Figure 5), hence, a linear PK model was used to project odronextamab exposure in humans.
Similarly to other bsAbs, 17 the projected odronextamab Cmax was within two to fourfold of observed data, whereas Ctrough was overestimated (Table 1); there was negligible drug accumulation with a weekly dosing interval. The overestimated Ctrough and lack of accumulation is potentially due to the target‐mediated disposition of odronextamab in patients who had a much higher number of CD20+ B cells than healthy monkeys. Target‐mediated drug clearance appears to predominate at lower doses and odronextamab concentrations, which may explain the overpredicted exposure value at doses less than 1 mg from the linear PK model. Of note, the more than 50‐fold higher binding affinity of odronextamab to CD3 in humans than in cynomolgus monkeys may also contribute to the rapid clearance of odronextamab in patients. 18 In addition, interpatient variability in odronextamab exposure could be greater than 100% at doses less than 1 mg, indicating that the amount of target contributed to variability in drug exposures. Nevertheless, although projected odronextamab Cmax in the first week was two to fourfold higher than the observed data, this provided a conservative Cmax estimation for the first patient cohort.
Estimating odronextamab concentrations associated with cytokine release in humans
In vitro odronextamab EC50 values for cytokine release in whole blood (IL‐6, TNF‐α, and IFN‐γ) were 0.3–0.5 nM (0.05–0.08 mg/L), and maximal cytokine release was achieved at greater than 1 nM (>0.15 mg/L; Figure 2a). In the FIH study, odronextamab mean (standard deviation) Cmax at 0.5 mg and 1 mg split dose (0.5 mg/0.5 mg) was 0.081 (0.046) mg/L and 0.196 (0.024) mg/L, respectively (Table 1). Therefore, EC50 values from the in vitro whole blood cytokine assays provided a reasonable estimate of odronextamab concentrations associated with cytokine release in patients treated with the week 1 day 1 dose (0.5 mg), and could be used for determining the initial dose in the first cohort of a FIH study via a minimum anticipated biological effect level (MABEL)‐based approach. Furthermore, this is a conservative estimation, given that in vitro EC50 values were determined in the absence of dexamethasone (Figure 2a). With the inclusion of dexamethasone, cytokine release is suppressed (Figure 2b) without affecting B‐cell killing (Figure 3e), supporting the clinical use of dexamethasone as premedication for CRS management.
Transient cytokine release is common in the early weeks following initiation of treatment with T‐cell‐engaging bsAbs. 19 , 20 Although multiple cytokines are released, we used IL‐6 as a surrogate for the analysis because it plays a key role in clinical manifestations of CRS, as evidenced by the effectiveness of IL‐6 blockade in CRS management. 20 Despite our in vitro and monkey cytokine data showing a clear relationship between odronextamab concentration and IL‐6 concentration (Figures 2 and 5b), such a relationship was not apparent in the clinical study during the step‐up dosing period (Figure 6). This could be explained by highly variable numbers of B cells (tumor and non‐tumor) and T cells at baseline in individual patients, in contrast to the in vitro experiment (Figure 2b) in which initial cell counts were tightly controlled, as well as large variability in EC50 values for cytokine release across patients, as shown in the experiment with multiple donors (Figure 1). Our observations are consistent with studies of other T‐cell engaging bsAbs. It has been reported that dose‐dependent cytokine elevation occurred in the first week of blinatumomab dosing, 21 and a clear dose–CRS relationship for glofitamab was found from 1.8–25 mg initial doses when step‐up dosing was not implemented. 22 , 23 In contrast, with step‐up dosing of mosunetuzumab, no apparent dose–CRS relationship was found. 24 Collectively, these findings suggest that multiple factors, such as drug concentration, time following the first dose, and the number of and binding affinity to target B cells and T cells in individual patients could affect the intensity and variability of cytokine release. Additionally, cytokine release differs across species; in monkeys, odronextamab was tolerated at 1 mg/kg without step‐up dosing, compared with a dose of 1 mg (0.01 mg/kg) on day 1 of week 1 in humans. This difference could be explained in part by the much higher odronextamab concentrations required for T‐cell activation in monkeys compared with humans, due to different binding affinities to T cells in the two species.
Predicting effective odronextamab concentrations in humans
Accurate prediction of the efficacious dose range in patients can facilitate a fast escalation of dose in the FIH study and reduce the number of dose cohorts required for evaluation. Our data suggest that efficacious concentrations in mice (>1 mg/L), which resulted in 100% inhibition of tumor growth (Figure 4), were useful for the prediction of minimal efficacious concentrations in patients, and to inform the dose‐escalation strategy in the FIH study. In contrast, the maximum cytotoxicity observed in the in vitro cytotoxicity assay (0.015 mg/L or 10−10 nM; Figure 3), which is often used to estimate MABEL, was less predictive for efficacious concentrations in patients. Predicting effective target dose range in patients is particularly challenging, as it is difficult to mimic disease condition and clinical response to a specific treatment in preclinical experiments.
Testing of high odronextamab doses in humans
Odronextamab exposure in cynomolgus monkeys at 1 mg/kg provided supportive information for testing doses up to 80 mg in humans. However, in the FIH study, dose escalation beyond the maximum exposure projected in monkeys was driven by clinical observation and adherence to dose‐limiting toxicity assessment rules; in fact, odronextamab 320 mg (4 mg/kg) was well tolerated by patients following a step‐up dosing strategy. 6
Translating findings to other bispecific antibodies
In summary, the following can be generalized qualitatively to other bsAbs, albeit with several caveats/limitations. Regarding safety, T‐cell‐engaging bsAbs mediate cytokine release during T‐cell activation, and the EC50 values obtained from in vitro cytokine release assays could be used for selecting an FIH starting dose via a MABEL‐based approach. However, the magnitude of cytokine release in patients is dependent upon T‐cell activation status, accessable tumor targets, and disease type. Regarding PK, allometry with inclusion of target‐mediated disposition, as appropriate, can be used for predicting the clinical PK of bsAbs for FIH starting doses. 17 Finally, regarding efficacy, in vivo mouse models can be used to evaluate the antitumor effect of bsAbs. However, the translational value of mouse models to the clinic depends on the patient populations being evaluated. If a treatment‐sensitive tumor cell line was tested in mice, with the patient population being relapsed or refractory to multiple prior lines of treatment, the efficacious concentration from the mouse model may be considered only a minimal effective concentration. If a treatment‐resistant tumor cell line that closely resembles the tumor target in patients was tested in mice, the data will likely be more relevant for the identification of an efficacious concentration in patients. We acknowledge in vitro assay systems cannot completely represent the native immune system, 25 and fast tumor growth in mice may not accurately represent tumor growth rates in patients. 4 The selection of species and relevant disease models for efficacy, pharmacology, and toxicology studies to characterize bsAbs needs to consider the properties of both the target cells and T cells, cross‐species specificity, bsAb functionality, and the expression and function of targets. 25
CONCLUSION
This retrospective analysis indicates that data from in vitro cytokine experiments, in vivo mouse models, and monkey PK and toxicity data are valuable for the design of FIH studies of odronextamab, and potentially other bsAbs, in patients with R/R B‐cell malignancies.
CONFLICT OF INTEREST
Min Zhu, Kara Olson, Jessica R. Kirshner, Masood Khaksar Toroghi, Hong Yan, Lauric Haber, Craig Meagher, Dina M. Flink, Srikanth R. Ambati, John D. Davis, A. Thomas DiCioccio, Eric J. Smith, and Marc W. Retter are employees and shareholders of Regeneron Pharmaceuticals, Inc.
AUTHOR CONTRIBUTIONS
M.Z., K.O., J.R.K., M.K.T., H.Y., L.H., C.M., D.M.F., S.R.A., J.D.D., A.T.D., E.J.S., and M.W.R. wrote the manuscript. M.Z., K.O., J.R.K., M.K.T., L.H., C.M., E.J.S., and M.W.R. designed the research. M.Z., K.O., J.R.K., M.K.T., L.H., C.M., E.J.S., and M.W.R. performed the research. M.Z., K.O., J.R.K., M.K.T., H.Y., L.H., C.M., D.M.F., S.R.A., J.D.D., A.T.D., E.J.S., and M.W.R. analyzed the data.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank Pamela Krueger and her Research PK team for measuring odronextamab concentrations in mice. This study was supported by Regeneron Pharmaceuticals, Inc. Medical writing support was provided by Paul Scutt, PhD, of Arc, a division of Spirit Medical Communications Ltd, funded by Regeneron Pharmaceuticals, Inc. We would also like to thank all the patients, their families, and site personnel who participated in this study.
Zhu M, Olson K, Kirshner JR, et al. Translational findings for odronextamab: From preclinical research to a first‐in‐human study in patients with CD20+ B‐cell malignancies. Clin Transl Sci. 2022;15:954‐966. doi: 10.1111/cts.13212
Funding information
This study was funded by Regeneron Pharmaceuticals, Inc.
REFERENCES
- 1. Brinkmann U, Kontermann RE. The making of bispecific antibodies. mAbs. 2017;9:182‐212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Smith EJ, Olson K, Haber LJ, et al. A novel, native‐format bispecific antibody triggering T‐cell killing of B‐cells is robustly active in mouse tumor models and cynomolgus monkeys. Sci Rep. 2015;5:17943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wang L, Qin W, Huo YJ, et al. Advances in targeted therapy for malignant lymphoma. Signal Transduct Target Ther. 2020;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kamperschroer C, Shenton J, Lebrec H, Leighton JK, Moore PA, Thomas O. Summary of a workshop on preclinical and translational safety assessment of CD3 bispecifics. J Immunotoxicol. 2020;17:67‐85. [DOI] [PubMed] [Google Scholar]
- 5. NIH. U.S. National Library of Medicine ; Clinicaltrials.gov. www.clinicaltrials.gov. Accessed August 10, 2021.
- 6. Bannerji R, Allan JN, Arnason JE, et al. Odronextamab (REGN1979), a human CD20 x CD3 bispecific antibody, induces durable, complete responses in patients with highly refractory B‐cell non‐Hodgkin lymphoma, including patients refractory to CAR T therapy. Blood. 2020;136:42‐43. [Google Scholar]
- 7. Crawford A, Haber L, Kelly MP, et al. A Mucin 16 bispecific T cell‐engaging antibody for the treatment of ovarian cancer. Sci Transl Med. 2019;11:eaau7534. [DOI] [PubMed] [Google Scholar]
- 8. Shultz LD, Brehm MA, Garcia‐Martinez JV, Greiner DL. Humanized mice for immune system investigation: progress, promise and challenges. Nat Rev Immunol. 2012;12:786‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lu H, Zhou Q, Deshmukh V, et al. Targeting human C‐type lectin‐like molecule‐1 (CLL1) with a bispecific antibody for immunotherapy of acute myeloid leukemia. Angew Chem Int Ed Engl. 2014;53:9841‐9845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dong JQ, Salinger DH, Endres CJ, et al. Quantitative prediction of human pharmacokinetics for monoclonal antibodies: retrospective analysis of monkey as a single species for first‐in‐human prediction. Clin Pharmacokinet. 2011;50:131‐142. [DOI] [PubMed] [Google Scholar]
- 11. Ling J, Zhou H, Jiao Q, Davis HM. Interspecies scaling of therapeutic monoclonal antibodies: initial look. J Clin Pharmacol. 2009;49:1382‐1402. [DOI] [PubMed] [Google Scholar]
- 12. Oitate M, Masubuchi N, Ito T, et al. Prediction of human pharmacokinetics of therapeutic monoclonal antibodies from simple allometry of monkey data. Drug Metab Pharmacokinet. 2011;26:423‐430. [DOI] [PubMed] [Google Scholar]
- 13. Ryman JT, Meibohm B. Pharmacokinetics of monoclonal antibodies. CPT Pharmacometrics Syst Pharmacol. 2017;6:576‐588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brouwer‐Visser J, Bannerji R, Allan JN, et al. Effects of REGN1979 (odronextamab) on cytokines and T cells in the circulation of patients with relapsed/refractory B‐cell non‐Hodgkin lymphoma. EP1270. Poster presented at EHA 2020.
- 15. Bannerji R, Arnason JE, Advani R, et al. Emerging clinical activity of REGN1979, an anti‐CD20 x anti‐CD3 bispecific antibody, in patients with relapsed/refractory follicular lymphoma (FL), diffuse large B‐cell lymphoma (DLBCL), and other B‐cell non‐Hodgkin lymphoma (B‐NHL) subtypes. Blood. 2018;132:1690. [Google Scholar]
- 16. Deng R, Iyer S, Theil FP, Mortensen DL, Fielder PJ, Prabhu S. Projecting human pharmacokinetics of therapeutic antibodies from nonclinical data: what have we learned? mAbs. 2011;3:61‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Upreti VV, Yago MR, Kast J, et al. Accurate prediction of clinical pharmacokinetics of three generations of bispecific T‐cell engagers (canonical bite construct; half‐life extended bite construct; bispecific antibody) for MABEL based first‐in‐human starting doses. Clin Pharmacol Ther. 2021;109:PIII‐041. [Google Scholar]
- 18. Haber L, Olson K, Kelly MP, et al. Generation of T‐cell‐redirecting bispecific antibodies with differentiated profiles of cytokine release and biodistribution by CD3 affinity tuning. Sci Rep. 2021;11:14397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hijazi Y, Klinger M, Kratzer A, et al. Pharmacokinetic and pharmacodynamic relationship of blinatumomab in patients with non‐Hodgkin lymphoma. Curr Clin Pharmacol. 2018;13:55‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hosseini I, Gadkar K, Stefanich E, et al. Mitigating the risk of cytokine release syndrome in a Phase I trial of CD20/CD3 bispecific antibody mosunetuzumab in NHL: impact of translational system modeling. NPJ Syst Biol Appl. 2020;6:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhu M, Wu B, Brandl C, et al. Blinatumomab, a Bispecific T‐cell Engager (BiTE®) for CD‐19 targeted cancer immunotherapy: clinical pharmacology and its implications. Clin Pharmacokinet. 2016;55:1271‐1288. [DOI] [PubMed] [Google Scholar]
- 22. Dickinson MJ, Morschhauser F, Iacoboni G, et al. CD20‐TCB (RG6026), a novel “2:1” format T‐cell‐engaging bispecific antibody, induces complete remissions in relapsed/refractory B‐cell non‐Hodgkin's lymphoma. Hematol Oncol. 2019;37:92‐93.31187519 [Google Scholar]
- 23. Hutchings M, Morschhauser F, Iacoboni G, et al. Glofitamab, a novel, bivalent CD20‐targeting T‐cell‐engaging bispecific antibody, induces durable complete remissions in relapsed or refractory B‐cell lymphoma: a Phase I trial. J Clin Oncol. 2021;39:1959‐1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sehn LH, Assouline S, Bartlett NL, et al. Managing cytokine release syndrome (CRS) and neurotoxicity with step‐up dosing of mosunetuzumab in relapsed/refractory (R/R) B‐cell non‐Hodgkin lymphoma (NHL). Hematol Oncol. 2019;37:310‐311.30847943 [Google Scholar]
- 25. Nie S, Wang Z, Moscoso‐Castro M, et al. Biology drives the discovery of bispecific antibodies as innovative therapeutics. Antib Ther. 2020;3:18‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


