Abstract
This paper aims to investigate the efficacy of circularly polarized light smartphones in affecting dry eye symptoms and asthenopia through a comparison with linearly polarized smartphones. One hundred twenty participants were randomly divided into four groups. Dry eye and asthenopia symptoms were evaluated using the Ocular Surface Disease Index (OSDI), Computer Vision Syndrome Scale 17 (CVSS17), Convergence Insufficiency Symptom Survey (CISS), and visual analogue scale (VAS). Objective ocular examinations were assessed by confusion flicker frequency (CFF), tear meniscus height (TMH), noninvasive break‐up time (NIBUT), conjunctiva redness, fluorescein tear break‐up time (FTBUT), corneal fluorescein staining, and the Schirmer I test. Tests were performed before and after a reading task. Subjective evaluations including the OSDI, CVSS17, and CISS were all significantly increased after reading on a linearly polarized smartphone, whereas no change was observed in the circular polarization groups in both light and dark environments. A significantly enlarged VAS was shown in all of the four groups, but a significant increase in ΔVAS only appeared in the linear polarization groups. There were significant decreases in TMH, NIBUT, conjunctiva redness, FTBUT, and CFF after reading on a linearly polarized smartphone but the circularly polarized smartphone had lesser effects on these parameters. Our study indicated that reading on linearly polarized smartphones may cause dry eye disorder, asthenopia, and ocular discomforts, whereas circularly polarized smartphones appears to minimize these adverse effects on eye dryness and visual fatigue in light and dark environments.
Study Highlights.
WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?
Light emissions of the smartphones have polarization and linearly polarized light was currently adopted by most of the smartphones, which will cause significant ocular surface disorders, including dry eye and asthenopia. The circularly polarized light smartphone was designed recently to minimize the hazards above and bring benefits to ocular surface protection.
WHAT QUESTION DID THIS STUDY ADDRESS?
This study aimed to investigate the efficacy of circularly polarized light smartphones in affecting dry eye symptoms and asthenopia through a comparison with linearly polarized smartphones.
WHAT DOES THIS STUDY ADD TO OUR KNOWLEDGE?
Our study indicated that reading on linearly polarized smartphones may cause dry eye disorder, asthenopia, and ocular discomforts, whereas circularly polarized smartphones appear to minimize the adverse effects on eye dryness and visual fatigue in light and dark environments.
HOW MIGHT THIS CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE?
Designing a circularly polarized smartphone and bringing it into use may provide a novel way to minimize the video display terminal‐induced dry eye symptoms and asthenopia. Changes may happen in the industry of digital devices by adopting circularly polarized light to relieve eye‐related problems.
INTRODUCTION
The development of video display terminals (VDTs), especially smartphones, has increased rapidly in the past 2 decades. The number of VDT users has increased from 16 million in 1995 to 4.68 billion in 2019. 1 Young people aged 16–29 years are the most likely to be attracted to VDTs, with nearly 91% owning digital devices. 2 Enthusiasm for VDTs, however, results in widespread visual and ocular discomforts, including eye dryness, eye pain, eye strain, asthenopia, and headaches. 3 A report from the Tear Film and Ocular Surface Dry Eye Workshop II (TFOS DEWS II) suggested that VDT use has been considered as a factor contributing to dry eye disease (DED). 4 A correlation between the ocular discomforts induced by smartphone use and DED has been identified in different regions, such as South Korea, Japan, and Italy. 5 , 6 , 7 , 8 The etiology of these reported symptoms has also led to the consideration that smartphone use may have an impact on blink rate, tear volume, tear film stability, ocular staining, and conjunctiva redness. 9
As daily life functions require a smartphone, it is essential to diminish the associated health hazards to user symptoms and develop better smartphone products to prevent ocular symptoms. The light derivation of a smartphone is polarized, and its polarization state can be simply divided into linear and circular. Linearly and circularly polarized light differs in the direction of propagation and the characteristics of circularly polarization have closer relationship with natural light. 10 A previous study has proved that circular polarized liquid crystal display televisions (LCDTVs) performed better than linear polarized LCDTVs in alleviating visual fatigue. 11 However, the methods of use, interior compositions, and screens of smartphones and televisions are entirely dissimilar.
To determine whether circularly polarized light smartphones perform better than linearly polarized light smartphones on dry eye and asthenopia symptoms, our study aimed to investigate changes in dry eye symptoms and asthenopia before and after reading on a smartphone with circularly or linearly polarized light in both the light and dark environments.
METHODS
Subjects
In total, 120 voluntary participants were involved in this prospective randomized controlled study. The calculation of sample sizes followed the formula of N = Z 2 × (P × (1−P))/E 2. When the confidence was set to be 95%, Z value was relevantly to be 1.96. With a p value of 0.5 and a E value of 0.1, we calculated the sample size N as 96. Considering a maximum sample fall off value of 20%, the sample size was finalized to be 120. The study was conducted at the Eye Center of the Second Affiliated Hospital of Zhejiang University School of Medicine and was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine following the Declaration of Helsinki. This study was registered with the Chinese Clinical Trial Register (https://www.chictr.org.cn/, No. ChiCTR2100043986).
Volunteers were recruited mainly among college students. Concerning the inclusion criterion, participants were required to have basic reading comprehension skills and to be older than 18 years old. The exclusion criterion stated that eligible participants must not have ocular inflammation and disease, not have used topical eye drop within 1 month, not have worn contact lens within 1 month, not have a history of eye surgery within 6 months, not be a lactating or pregnant woman, or not have severe systemic diseases.
Digital devices
Two types of smartphones were mainly involved in this experiment: circularly and linearly polarized light smartphones. The circularly and linearly polarized smartphones had an identical exterior appearance with the only divergence being their light polarization. Detailed information about the smartphones is demonstrated in Table S1.
Study design
The 120 participants were randomly divided into four groups: (1) circularly polarized smartphone in a light condition, (2) linearly polarized smartphone in a light condition, (3) circularly polarized smartphone in a dark condition, and (4) linearly polarized smartphone in a dark condition. Each group was assigned 30 subjects. The study was designed to be double‐blinded. The participants were prevented from knowing the group to which they were assigned, and they could not find clues from the smartphones because the circularly and linearly polarized smartphones used in this research had the same appearance. The examiners were also blinded in the study and finished each examination without knowing to which group each participant belonged. Participants were required to read for two consecutive hours on a smartphone and they could not stop reading for more than 1 minute. The subjects in the light condition performed the reading task in a room with natural light, and the subjects in the dark condition were placed in a closed room without a window, where the smartphone was the only light source. The average light intensities of the two conditions were 71 flux and 0.91 flux, respectively. The brightness intensities of screens were set up to 50% of the maximum in the light environment and 30% of the maximum in the dark environment. The room temperature and humidity were kept at 22–25°C and 40%–60%, respectively. Reading assignments were conducted between 9 a.m. and 11 a.m. each day. To avoid the influence of self‐smartphone use before the study, participants were required to be prevented from using smartphones between 12 a.m. and 9 a.m. on the research day.
Subjective questionnaires and objective ocular measurements for detecting dry eye and asthenopia were adopted before and after the 2‐h reading, following the order of: Four subjective questionnaires, critical flicker fusion frequency (CFF), noninvasive Keratograph 5 M including tear meniscus height (TMH), tear break‐up time (NIBUT) and redness, fluorescein tear break‐up time (FTBUT), corneal fluorescein staining (CFS), and the Schirmer I test. Both the right and left eyes were examined.
Subjective questionnaires
Reliable and standard questionnaires were used to evaluate the subjective feelings of volunteers. Ocular Surface Disease Index (OSDI) was used for assessing typical dry eye symptoms. OSDI is recommended by TFOS DEWS II, an authoritative guideline in the dry eye field, as one of the gold standards in dry eye diagnosis, and its reliability and efficacy have been validated. 12 OSDI contains 12 different questions, each graded from 0–4 where 0 indicates none of the time, 1 indicates some of the time, 2 indicates half of the time; 3 indicates most of the time, and 4 indicates all of the time. The total OSDI score was calculated following the formula: OSDI score = ([sum of scores for all questions answered] × 100)/[total number of questions answered] × 4). Scores over 13 are diagnosed as symptomatic DED. Computer Vision Syndrome Scale 17 (CVSS17) was used for assessing digital devices‐related ocular symptoms. It is a novel and validated scale introduced by Gonzalez‐Perez et al. 13 and was specially designed to evaluate eye‐related symptoms caused by digital device use. Higher CVSS17 scores represents more severe ocular symptoms. Convergence Insufficiency Symptom Survey (CISS) was used for assessing asthenopia and visual fatigue, which was developed by the Convergence Insufficiency and Reading Study Group in 1999. 14 Discomfort and topical fatigue were assessed by the visual analogue scale (VAS), ranging from 0–100, where 0 indicates no discomfort and fatigue and 100 indicates extremely discomfort and fatigue.
Noninvasive measurements
The CFF is recognized as an indicator of asthenopia and its reduction represents the generation of visual fatigue. 15 The CFF was analyzed by Digital Flicker (Takei Scientific Instruments Co. Ltd., Tokyo, Japan). The blinking frequency of CFF descended from 60 Hz to 1 Hz, and participants were required to stop the blink of CFF immediately after they can perceive the flicker. The descending threshold was measured two times, and an average value was obtained for further statistical analysis.
The TMH, NIBUT, and conjunctiva redness of all participants were measured by the Keratograph 5 M (Oculus, Wetzlar, Germany). The ocular images of participants were taken by a single examiner, using the Keratograph 5 M, and the machine will automatically analyze the value of TMH, NIBUT, and redness. The value of TMH represented the volume and the storage capacity of tears. Less volume or lower storage of tears may result in dry eye symptoms. The value of NIBUT shows the break‐up time of the tear film, and a quicker NIBUT represents a less stable tear film and a greater possibility of eye dryness. The first and average values of the NIBUT (NIBUT‐first and NIBUT‐ave) were recorded and analyzed, respectively. Conjunctiva redness was divided into bulbar redness and palpebral redness, each of which was analyzed individually.
Invasive measurements
The FTBUT examination was conducted by a single ophthalmologist with more than 20 years of clinical experience. FTBUT values were measured using sterile fluorescein paper strips (Jinming New Technological Development Co. Ltd., Tianjin, China). Briefly, ~ 5 μl (a drop) of normal saline was instilled in the strip, which was then shaken to remove extra liquid to minimize the volume of fluorescein fluid. The strip was then gently touched with the inferior temporal bulbar conjunctiva for 1 s. Participants were asked to blink three times naturally to facilitate the uniform distribution of fluorescein on the ocular surface. The time from the last blink of the eye to the first dry spot on the tear film was measured under a cobalt‐blue filter. Three consecutive measurements were recorded with a time interval of 30 s.
The CFS assessment was carried out right after the FTBUT testing with the same fluorescein staining strips. Corneal staining was evaluated under a yellow filter, and CFS scores were calculated according to the Oxford scale. 16
The Schirmer I test was performed using a sterile 5 mm × 30 mm strip (Jinming New Technological Development Co. Ltd., Tianjin, China). The strip was gently inserted between the middle and lateral third of each lower lid margin. Participants were then instructed to softly close their eyes. A Schirmer strip was placed for 5 min, and the length of the wetting strip was recorded in millimeters.
Statistical analysis
Statistical analyses were conducted by SPSS 25.0 (SPSS Inc., Chicago, IL, USA), GraphPad Prism 8.0 (GraphPad Software Inc., San Diego, CA, USA) and GPower version 3.1 software. Data comparisons before and after the examination were conducted using the Wilcoxon signed‐rank test. The differences in indicators between the two groups were analyzed using the Mann–Whitney U test. The sample size and power calculations were analyzed by GPower. The statistical test is two‐tailed and the p < 0.05 is considered significantly different.
RESULTS
Baseline information
In total, 120 volunteers, including 37 men and 83 women, completed the study. The mean age of all subjects was 25.86 ± 2.31 years. All participants were of Chinese ethnicity. Table 1 shows the baseline information of all participants before the 2‐h reading and no statistically significant difference was found among the four groups at the baseline. Results after 2 h of reading and the differences before and after reading are demonstrated in Table S2 and Table 2, respectively. The results of the post hoc power analysis are shown in Table S3.
TABLE 1.
Baseline information
| Light | Dark | p value | |||
|---|---|---|---|---|---|
| Circular | Linear | Circular | Linear | ||
| N | 30 | 30 | 30 | 30 | |
| Age | 26.10 ± 2.31 | 25.57 ± 2.20 | 26.07 ± 2.48 | 25.70 ± 2.19 | 0.762 |
| Sex (male:female) | 0.50 | 0.58 | 0.30 | 0.43 | 0.965 |
| OSDI | 24.03 ± 12.75 | 23.47 ± 14.51 | 23.19 ± 11.10 | 22.64 ± 10.15 | 0.978 |
| CVSS17 | 33.50 ± 6.37 | 31.50 ± 6.95 | 32.13 ± 6.30 | 32.20 ± 4.91 | 0.659 |
| CISS | 12.73 ± 6.23 | 11.17 ± 7.00 | 12.03 ± 6.21 | 12.27 ± 6.06 | 0.820 |
| VAS | 47.30 ± 19.84 | 44.23 ± 22.80 | 43.60 ± 20.74 | 43.40 ± 18.54 | 0.878 |
| CFF | 28.77 ± 3.21 | 29.96 ± 3.55 | 28.60 ± 2.58 | 29.31± 3.00 | 0.343 |
| TMH | 0.23 ± 0.05 | 0.25 ± 0.06 | 0.23 ± 0.06 | 0.25 ± 0.06 | 0.203 |
| NIBUT‐first | 6.65 ± 2.97 | 6.94 ± 3.51 | 7.35 ± 3.58 | 8.44 ± 5.33 | 0.539 |
| NIBUT‐ave | 7.57 ± 2.69 | 8.39 ± 2.96 | 9.34 ± 3.62 | 10.29 ± 5.34 | 0.200 |
| Bulbar redness | 0.98 ± 0.24 | 0.91 ± 0.25 | 0.94 ± 0.21 | 0.96 ± 0.28 | 0.479 |
| Palpebral redness | 0.79 ± 0.21 | 0.72 ± 0.24 | 0.74 ± 0.21 | 0.71 ± 0.25 | 0.189 |
| FTBUT | 4.18 ± 1.93 | 4.11 ± 1.79 | 5.30 ± 2.21 | 4.85 ± 2.65 | 0.220 |
| CFS | 1.08 ± 1.45 | 0.38 ± 1.80 | 0.97 ± 1.35 | 0.78 ± 1.46 | 0.002 |
| Schirmer I test | 12.42 ± 9.53 | 13.57 ± 9.34 | 15.67 ± 10.25 | 13.65 ± 8.54 | 0.501 |
Data are presented as mean ± SD.
Abbreviations: CFF, confusion flicker frequency; CFS, corneal fluorescein staining; CISS, Convergence Insufficiency Symptom Survey; CVSS, Computer Vision Syndrome Scale 17; FTBUT, fluorescein tear break‐up time; NIBUT‐ave, noninvasive break‐up time‐average; NIBUT‐first, noninvasive break‐up time‐first; OSDI, Ocular Surface Disease Index; TMH, tear meniscus height; VAS, visual analogue scale.
TABLE 2.
Differences of before and after reading 2 h on a smartphone
| Light | Dark | |||||
|---|---|---|---|---|---|---|
| Circular | Linear | p value | Circular | Linear | p value | |
| OSDI | −0.90 ± 5.15 | 5.00 ± 5.37 | <0.001 | 0.42 ± 3.06 | 4.93 ± 5.37 | <0.001 |
| CVSS17 | 0.20 ± 4.42 | 4.40 ± 3.46 | <0.001 | −0.10 ± 2.41 | 3.10 ± 3.98 | <0.001 |
| CISS | 0.37 ± 2.12 | 2.80 ± 3.32 | <0.001 | 0.07 ± 2.14 | 3.77 ± 4.64 | <0.001 |
| VAS | 9.20 ± 10.08 | 19.43 ± 12.21 | <0.001 | 6.07 ± 9.83 | 19.73± 14.61 | <0.001 |
| CFF | −0.01 ± 0.88 | −1.09 ± 1.70 | 0.003 | 0.37 ± 1.11 | −1.15 ± 1.88 | <0.001 |
| TMH | 0.01 ± 0.06 | −0.06 ± 0.06 | <0.001 | 0.01 ± 0.06 | −0.04 ± 0.05 | <0.001 |
| NIBUT‐first | −0.21 ± 3.05 | −1.98 ± 3.42 | 0.006 | 0.82 ± 4.21 | −2.00 ± 3.73 | <0.001 |
| NIBUT‐ave | −0.20 ± 2.85 | −1.65 ± 2.76 | 0.011 | 0.80 ± 3.63 | −2.18 ± 3.19 | <0.001 |
| Bulbar redness | 0.05 ± 0.23 | 0.10 ± 0.24 | 0.394 | 0.03 ± 0.16 | 0.11 ± 0.22 | 0.009 |
| Palpebral redness | 0.00 ± 0.19 | 0.10 ± 0.21 | 0.034 | 0.06 ± 0.15 | 0.13 ± 0.14 | 0.005 |
| FTBUT | −0.44 ± 1.66 | −0.80 ± 1.36 | 0.165 | −0.60 ± 1.69 | −1.58 ± 2.30 | 0.017 |
| CFS | 0.05 ± 0.38 | 0.08 ± 0.38 | 0.639 | 0.03 ± 0.45 | 0.15 ± 0.40 | 0.078 |
| Schirmer I test | 2.08 ± 7.33 | −2.38 ± 6.44 | 0.007 | 0.19 ± 3.76 | −4.10 ± 7.16 | <0.001 |
Data are presented as mean ± SD.
Abbreviations: CFF, confusion flicker frequency; CFS, corneal fluorescein staining; CISS, Convergence Insufficiency Symptom Survey; CVSS, Computer Vision Syndrome Scale 17; FTBUT, fluorescein tear break‐up time; NIBUT‐ave, noninvasive break‐up time‐average; NIBUT‐first, noninvasive break‐up time‐first; OSDI, Ocular Surface Disease Index; TMH, tear meniscus height; VAS, visual analogue scale.
Subjective assessments of dry eye symptoms and asthenopia
Subjective dry eye symptoms were evaluated by OSDI. The OSDI scores of the light and dark linearly polarized light smartphone groups showed a significant increase when compared to the baseline statistics (p < 0.001 and p < 0.001; Figure 1a), whereas the two circularly polarized groups showed no significant differences (p = 0.353 and p = 0.470; Figure 1a). For ΔOSDI, significant differences were found between the circularly and linearly polarized groups in both of the light and dark environments (p < 0.001 and p < 0.001; Figure 1e). Similar score change trends were identified in the CVSS17 and CISS evaluations, which evaluated computer vision syndrome and degree of asthenopia, respectively (Figure 1b,c,f,g). VAS scores, which reflected the extent of visual fatigue and discomfort, demonstrated significant differences in all the four groups compared to baseline (p < 0.001, p < 0.001, p < 0.01, and p < 0.001; Figure 1d), and ΔVAS differed significantly between the circularly and linearly polarized groups under the light and dark environments (p < 0.001 and p < 0.001; Figure 1h).
FIGURE 1.
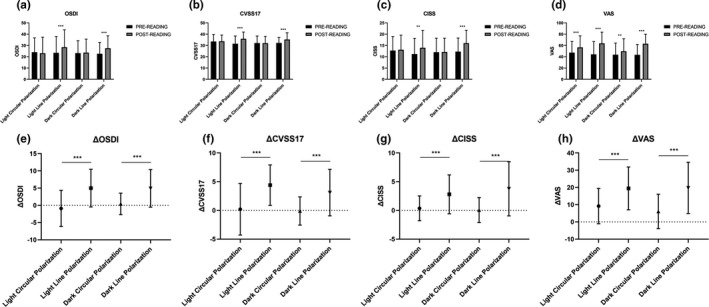
Influence of subjective assessments on dry eye symptoms and asthenopia. (a–d) Shows data presented as mean ± SD. a–d Demonstrated the differences of OSDI, CVSS17, CISS, and VAS between post‐ and pre‐reading, respectively. (e–h) Shows the Δ differences of subjective measurements between circular and linear groups under two separated environments (Δ = post–pre). *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001. CISS, Convergence Insufficiency Symptom Survey; CVSS, Computer Vision Syndrome Scale 17; OSDI, Ocular Surface Disease Index; VAS, visual analogue scale
Influence of circularly and linearly polarized smartphones on tear film stability and tear volume
Typically, ocular stability is assessed using the NIBUT, FTBUT, and CFS. The changing tendency of NIBUT‐first appeared to be consistent with NIBUT‐ave. NIBUT‐first and NIBUT‐ave were significantly decreased after reading on the linearly polarized smartphone (p < 0.001 and p < 0.001; Figure 2a,b), but no significance was found after reading on the circularly polarized smartphone. Significant decreases were also observed in ΔNIBUT‐first and ΔNIBUT‐ave (p < 0.001, p < 0.001, p < 0.05, and p < 0.001; Figure 2g,h). A significant reduction in FTBUT was identified in all four groups (p < 0.05, p < 0.001, p < 0.05, and p < 0.001; Figure 2c), however, the difference in ΔFTBUT was only present between the dark linear and circular polarization groups (p < 0.05; Figure 2i). For CFS, a difference was only found in the dark linear polarization group (p < 0.01; Figure 2d), whereas there was no change in ΔCFS (p > 0.05 and p > 0.05; Figure 2j).
FIGURE 2.
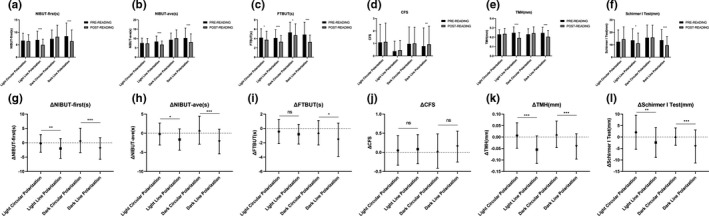
Influence of circularly and linearly polarized smartphone on tear film stability and tear volume. (a–f) Shows data presented as mean ± SD. a–f Demonstrated the differences of NIBUT‐first, NIBUT‐ave, FTBUT, CFS, TMH, and Schirmer I test between post‐ and pre‐reading, respectively. g–l showed the Δ differences of above objective measurements between circular and linear groups under two separated environments (Δ = post–pre). *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001. CFS, corneal fluorescein staining; FTBUT, fluorescein tear break‐up time; NIBUT‐ave, noninvasive break‐up time‐average; NIBUT‐first, noninvasive break‐up time‐first; TMH, tear meniscus height
Tear volume measurements indicated that TMH and ΔTMH were significantly decreased after reading on the linearly polarized smartphone (all p < 0.001; Figure 2e), whereas no changes were found in the circularly polarized groups. Similar changing trends were shown in the Schirmer I test (p < 0.05 and p < 0.001; Figure 2f) and the ΔSchirmer I test (p < 0.01 and p < 0.001; Figure 2l).
Influence of circularly and linearly polarized smartphone on asthenopia examination
As shown in Figure 3a and d, CFF and ΔCFF were significantly lower after reading on the linearly polarized smartphone when compared to the baseline data (p < 0.001, p < 0.01; p < 0.01, and p < 0.001). No difference was observed in the circular polarization groups (p > 0.05 and p > 0.05; Figure 3a). For conjunctiva redness, there were significant differences in bulbar and palpebral redness (p < 0.01 and p < 0.001; Figure 3b; p < 0.01 and p < 0.001; Figure 3c) in the linear polarization groups in light and dark environments. Significant differences were also shown in the bulbar redness of the circular polarization group in the light condition (p < 0.05; Figure 3b), and palpebral redness of circular polarization group in the dark condition (p < 0.01; Figure 3c). There were significant increases in Δbulbar redness between the circular and linear polarization groups in the dark environment (p < 0.01; Figure 3e) and Δpalpebral redness between the circular and linear polarization groups in both the light and dark environments (p < 0.05 and p < 0.01; Figure 3f).
FIGURE 3.
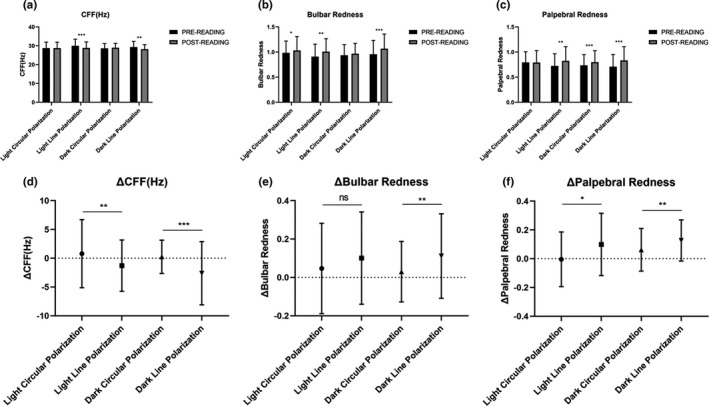
Influence of circularly and linearly polarized smartphone on asthenopia examination. (a–c) Shows data presented as mean ± SD. a–c Demonstrated the differences of CFF, bulbar redness, and palpebral redness between post‐ and pre‐reading, respectively. (d–f) Shows the Δ differences of above objective measurements between circular and linear groups under two separated environments (Δ = post–pre). *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001. CFF, confusion flicker frequency
DISCUSSION
Our study was the first to focus on the influence of the light polarizations of smartphones on eye‐related problems. In this study, we investigated and evaluated the performance of circularly polarized light from a smartphone in affecting dry eye symptoms and asthenopia after 2 h of reading by comparing with a linearly polarized smartphone in both light and dark environments. Our results indicated that reading on a linearly polarized smartphone contributed to inducing dry eye and asthenopia, whereas circularly polarized smartphone tended to reduce and minimize these visual discomforts caused by electronic reading in both of the light and dark conditions.
Previously, several researchers have suggested that the use of a smartphone may disrupt the ocular micro‐environment and lead to a reduction in tear film stability and tear volume. 17 , 18 , 19 Our results showed that FTBUT was significantly reduced after reading tasks, especially for the linearly polarized smartphone, and NIBUT was decreased only in the linearly but not the circularly polarized groups. The TMH and Schirmer I test, which refer to the generation and preservation of tear volume, had a similarly significant reduction after the reading task was performed on the linearly polarized smartphone, but there was no reduction with the circularly polarized smartphone. A number of factors contributed to this difference, and the major one possibly being the polarization characteristics of the light source. Light is known to be an electro‐magnetic wave. The vibration direction of the electro‐vector and forward direction of the light wave form the vibration plane for light. 20 For linearly polarized light, the vibration direction of the electro‐vector is restricted to a certain direction. However, the vibration direction of circularly polarized light forms a rotation circle toward the direction of light propagation. Closely, the electro‐vector of natural light becomes uniformly distributed in all directions, which is more likely consistent with circular polarized light. 21 , 22 Apparently, human eyes might have better compliance with circularly polarized light, as people live in an environment surrounded by natural light. Therefore, our study suggested that an uneven distribution of vibration direction might be harmful to the stability of the tear film, which could lead to DED, resulting in a quicker break in the tear film and reduction in tear volume.
Except for dry eye, asthenopia is another considerable indication of continuous smartphone use. Various studies have confirmed the correlation between asthenopia and hand‐held device use. 21 Yan et al. 11 proposed that circularly polarized LCDTVs had an advantage of relieving asthenopia and reducing blink rates compared to linearly polarized LCDTVs. This was in accordance with our results. Both the CFF and conjunctiva redness results indicated that reading on a linearly polarized smartphone led to more severe visual fatigue. This was partly due to the vibration natures of circular and linear light. Human eyes spontaneously adapt to daily activities and biological rhythms under natural light. Long‐time exposure to different vibration directions may result in an impairment of the self‐regulation mechanism, thereby triggering progressive fatigue of the intraocular muscles and conjunctiva redness. In this way, circularly polarized light, which had similar characteristics to natural light, does not induce extra fatigue and capillary congestion.
Reports from different regions have previously shown that reading on smartphones could typically aggravate subjective feelings of eye dryness and visual fatigue. 5 , 6 , 7 , 8 In our study, we evaluated dry eye and asthenopia symptoms by using the following standard questionnaires: the OSDI, CVSS17, CISS, and VAS. A consistent tendency was found in the changes in the OSDI, CVSS17, and CISS scores in which they were significantly increased after completing the 2‐h reading on the linearly polarized smartphone, but there were no variations when reading on the circularly polarized smartphone. These results of subjective ocular symptoms were agreed with the objective signs mentioned above. Increase in the OSDI and CVSS17 scores after using the linearly polarized smartphone were a result of tear film damage and tear volume lessening. It was confirmed by previous research that a shorter break‐up time and lower TMH had statistical correlations with higher OSDI and CVSS17 scores. 23 , 24 , 25 Likewise, a reduced CFF, which represented heavier degrees of asthenopia and visual sensitivity, was a major factor of increases in CISS and VAS scores. 11 The statistical data of our study indicated that changes in subjective symptoms after reading on different polarized smartphones seemed to be more distinct and susceptible than objective signs.
There are still some limitations in our study. Our study did not adjust for statistical multiplicity, consequently, the analysis appeared weaker because our results eventually demonstrated statistical differences but not clinical differences and such results required further evaluation to confirm its clinical importance. Reading on smartphones for 2 h seemed a short period, therefore, changes in physical signs and symptoms may not be apparent enough. Smartphone use tracking for months and years should be conducted to explore the long‐term influences on dry eye symptoms and asthenopia. Furthermore, the internal mechanisms and potential molecular pathways of circular and linear light polarization on human eyes still remain unclear. Our results simply illustrated the impact of light polarization on dry eye and asthenopia symptoms, but not the reason for it. Further research must be organized and carried out to investigate interior reasons.
In conclusion, our study suggested that reading on linearly polarized smartphones may cause dry eye disorder, asthenopia, and ocular discomforts. On the contrary, circularly polarized smartphones appears to minimize these adverse effects on ocular health and relieve eye dryness and visual fatigue in light and dark environments. Although there are still some advantages of linear polarization technology, circularly polarized smartphones appear to be more suitable for users, especially those with long‐term smartphone operation needs.
CONFLICT OF INTERESTS
The authors declared no competing interests for this work.
AUTHOR CONTRIBUTIONS
Y.M., F.F., and X.J. wrote the manuscript. Y.M., K.Y., and X.J. designed the research. X.S. and K.Y. performed the research. X.W., Y.W., and C.W. analyzed the data. F.F. contributed new reagents.
Supporting information
Tables S1‐S3
ACKNOWLEDGEMENT
Special thanks to TÜV Rheinland (Shanghai) Co., Ltd. for providing the digital devices and technical assistance for our study.
Mou Y, Shen X, Yuan K, et al. Comparison of the influence of light between circularly polarized and linearly polarized smartphones on dry eye symptoms and asthenopia. Clin Transl Sci. 2022;15:994‐1002. doi: 10.1111/cts.13218
Funding information
This work was supported by the Major Science and Technology Projects of Zhejiang Province (grant number 2017C03046) and (grant number 2020C03035) and A Project Supported by Scientific Research Fund of Zhejiang Provincial Education Department (No. Y202045610)
REFERENCES
- 1. Statista.com . Number of mobile phone users worldwide from 2015 to 2020. https://www.statista.com/statistics/274774/forecast‐of‐mobile‐phone‐users‐worldwide Accessed November 2016.
- 2. PEW Research Center . https://www.pewresearch.org/internet/fact‐sheet/mobile. Accessed 2020.
- 3. Talens‐Estarelles C, Garcia‐Marqués JV, Cervino A, Garcia‐Lázaro S. Use of digital displays and ocular surface alterations: a review. Ocul Surf. 2021;2021(19):252‐265. [DOI] [PubMed] [Google Scholar]
- 4. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334‐365. [DOI] [PubMed] [Google Scholar]
- 5. Moon JH, Kim KW, Moon NJ. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: a case control study. BMC Ophthalmol. 2016;16:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children. J Pediatr Ophthalmol Strabismus. 2014;51:87‐92. [DOI] [PubMed] [Google Scholar]
- 7. Hanyuda A, Sawada N, Uchino M, et al. Physical inactivity, prolonged sedentary behaviors, and use of visual display terminals as potential risk factors for dry eye disease: JPHC‐NEXT study. Ocul Surf. 2020;18:56‐63. [DOI] [PubMed] [Google Scholar]
- 8. Rossi GCM, Scudeller L, Bettio F, Pasinetti GM, Bianchi PE. Prevalence of dry eye in video display terminal users: a cross‐sectional Caucasian study in Italy. Int Ophthalmol. 2019;39:1315‐1322. [DOI] [PubMed] [Google Scholar]
- 9. Antona B, Barrio AR, Gascó A, Pinar A, González‐Pérez M, Puell MC. Symptoms associated with reading from a smartphone in conditions of light and dark. Appl Ergon. 2018;68:12‐17. [DOI] [PubMed] [Google Scholar]
- 10. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539‐574. [DOI] [PubMed] [Google Scholar]
- 11. Horváth G. Polarized Light and Polarization Vision in Animal Sciences. Springer; 2014. [Google Scholar]
- 12. Xiaolin Y, Dong F, Changchang Z, et al. Invited paper: the circular polarized LCD‐TV and its advantage over visual fatigue. Sid Symposium Digest Technical Papers. 2009;40:536‐539. [Google Scholar]
- 13. González‐Pérez M, Susi R, Antona B, Barrio A, González E. The Computer‐Vision Symptom Scale (CVSS17): development and initial validation. Invest Ophthalmol Vis Sci. 2014;55:4504‐4511. [DOI] [PubMed] [Google Scholar]
- 14. González‐Pérez M, Pérez‐Garmendia C, Barrio AR, García‐Montero M, Antona B. Spanish cross‐cultural adaptation and Rasch analysis of the convergence insufficiency symptom survey (CISS). Transl Vis Sci Technol. 2020;9:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maeda E, Yoshikawa T, Hayashi N, et al. Radiology reading‐caused fatigue and measurement of eye strain with critical flicker fusion frequency. Jpn J Radiol. 2011;29:483‐487. [DOI] [PubMed] [Google Scholar]
- 16. Bron AJ, Evans VE, Smith JA, et al. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22:640‐650. [DOI] [PubMed] [Google Scholar]
- 17. Horváth G, Barta A, Pomozi I, et al. On the trail of Vikings with polarized skylight: experimental study of the atmospheric optical prerequisites allowing polarimetric navigation by Viking seafarers. Philos Trans R Soc Lond B Biol Sci. 2011;366:772‐782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Golebiowski B, Long J, Harrison K, Lee A, Chidi‐Egboka N, Asper L. Smartphone use and effects on tear film, blinking and binocular vision. Curr Eye Res. 2020;45:428‐434. [DOI] [PubMed] [Google Scholar]
- 19. Prabhasawat P, Pinitpuwadol W, Angsriprasert D, Chonpimai P, Saiman M. Tear film change and ocular symptoms after reading printed book and electronic book: a crossover study. Jpn J Ophthalmol. 2019;63:137‐144. [DOI] [PubMed] [Google Scholar]
- 20. Horváth G, Varjú D. Polarized Light in Animal Vision. Springer; 2004. [Google Scholar]
- 21. Jaiswal S, Asper L, Long J, Lee A, Harrison K, Golebiowski B. Ocular and visual discomfort associated with smartphones, tablets and computers: what we do and do not know. Clin Exp Optom. 2019;102:463‐477. [DOI] [PubMed] [Google Scholar]
- 22. Cronin TW, Marshall J. Patterns and properties of polarized light in air and water. Philos Trans R Soc Lond B Biol Sci. 2011;366:619‐626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Choi JH, Li Y, Kim SH, et al. The influences of smartphone use on the status of the tear film and ocular surface. PLoS One. 2018;13:e0206541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Courtin R, Pereira B, Naughton G, et al. Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta‐analysis. BMJ Open. 2016;6:e009675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sanchez‐Valerio MDR, Mohamed‐Noriega K, Zamora‐Ginez I, Baez Duarte BG, Vallejo‐Ruiz V. Dry eye disease association with computer exposure time among subjects with computer vision syndrome. Clin Ophthalmol. 2020;14:4311‐4317. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1‐S3


