Abstract
Adverse drug reactions (ADRs) of targeted therapy drugs (TTDs) are frequently unexpected and long‐term toxicities detract from exceptional efficacy of new TTDs. In this proof‐of‐concept study, we explored how molecular causation involved in trastuzumab‐induced cardiotoxicity changes when trastuzumab was given in combination with doxorubicin, tamoxifen, paroxetine, or lapatinib. The data analytical platform Molecular Health Effect was utilized to map population ADR data from the US Food and Drug Administration (FDA) Adverse Event Reporting System to chemical and biological databases (such as UniProt and Reactome), for hypothesis generation regarding the underlying molecular mechanisms causing cardiotoxicity. Disproportionality analysis was used to assess the statistical relevance between adverse events of interest and molecular causation. Literature search was performed to compare the established hypotheses to published experimental findings. We found that the combination therapy of trastuzumab and doxorubicin may affect mitochondrial dysfunction in cardiomyocytes through different molecular pathways such as BCL‐X and PGC‐1α proteins, leading to a synergistic effect of cardiotoxicity. We found, on the other hand, that trastuzumab‐induced cardiotoxicity would be diminished by concomitant use of tamoxifen, paroxetine, and/or lapatinib. Tamoxifen and paroxetine may cause less cardiotoxicity through an increase in antioxidant activities, such as glutathione conjugation. Lapatinib may decrease the apoptotic effects in cardiomyocytes by altering the effects of trastuzumab on BCL‐X proteins. This patient‐centered systems‐based approach provides, based on the trastuzumab‐induced ADR cardiotoxicity, an example of how to apply reverse translation to investigate ADRs at the molecular pathway and target level to understand the causality and prevalence during drug development of novel therapeutics.
Study Highlights.
WHAT IS THE CURRENT KNOWLEDGE ON THE TOPIC?
Adverse drug reactions (ADRs) of targeted therapy drugs are frequently unexpected and long‐term toxicities detract from the exceptional efficacy of newly developed targeted therapy drugs.
WHAT QUESTION DID THIS STUDY ADDRESS?
In this proof‐of‐concept study, we explored how the molecular causation involved in trastuzumab‐induced cardiotoxicity changes when trastuzumab is given in combination with other chemotherapeutics.
WHAT DOES THIS STUDY ADD TO OUR KNOWLEDGE?
By mapping pharmacovigilance and molecular descriptor data, several hypotheses were generated regarding the underlying molecular mechanisms causing trastuzumab‐induced cardiotoxicity and how molecular causations alter due to drug‐drug interactions. Disproportionality analysis was used to assess the statistical relevance between adverse events of interest and molecular causation.
HOW MIGHT THIS CHANGE CLINICAL PHARMACOLOGY OR TRANSLATIONAL SCIENCE?
This patient‐centered reverse translational systems‐based approach provides an example of a detailed investigation of ADRs at the molecular pathway and target level to provide a process to better understand and predict drug pair adverse events.
INTRODUCTION
In a systems pharmacology view of drug action, a drug interacts with multiple primary and secondary targets and pathways. These targets exist within a complex network that can mediate the response to the drug leading to both therapeutic and adverse effects. A systems‐based approach can improve drug safety by enabling a more detailed and mechanistic understanding of adverse drug reactions (ADRs). It can provide feedback on how to mitigate future risks by rendering causal hypotheses, identifying biomarkers that can be used to predict ADRs before they occur, delineating a strategy for targeting high‐risk adverse events in clinical or post‐marketing surveillance analysis, and/or stratifying a population at a molecular level to identify risks for a particular ADR. In this proof‐of‐concept study, we present an example of an applied patient‐centered reverse translational systems‐based approach to investigate cardiotoxicity, an ADR caused by the targeted therapy drug (TTD) trastuzumab.
Overall, clinical responses of patients with cancer to TTDs depend on both efficacy and safety variables. However, current drug development strategies for TTDs in oncology mostly focus on the on‐target effects which are related to the efficacy of a drug candidate and its predictable safety concerns. This is the reason why off‐target side effects of TTDs are frequently unexpected and long‐term toxicities detract from exceptional efficacy of new TTDs. 1 , 2 , 3 In addition, efficacy of TTDs is compromised by additional host factors. Above 96% of patients with cancer are concomitantly given one to six additional medications because of their comorbidities on top of the existing complex chemotherapy. This complex therapeutic landscape with overlapping and pleiotropic molecular pathways leads to a high potential of causing serious drug‐drug interactions (DDIs). 4
In the current study, we focus on trastuzumab, which is a monoclonal antibody TTD binding to human epidermal growth factor receptor‐2 (HER2) that is overexpressed in about 25% of all patients with breast cancer. 5 HER2 blockade, however, can cause cardiotoxic side effects because HER2 receptors are present in not only breast cancer cells but also in normal cardiomyocytes, 1 , 2 , 3 as it is essential to their development and function. 1 , 3 , 6 Although trastuzumab‐induced (type II) cardiotoxicity was regarded as less severe and largely reversible (no changes in cardiomyocyte ultrastructures in contrast to anthracycline‐induced (type I) cardiotoxicity), the concerns on immediate and long‐term use of trastuzumab as well as the need for follow‐up have been strongly emphasized, along with increased awareness of trastuzumab‐induced cardiotoxicity and cardiomyopathies. 7
In particular, serious cardiac side effects have been reported due to the addition of trastuzumab to anthracyclines even though the combination therapies of trastuzumab and chemotherapy drugs like doxorubicin are considered as standard treatments according to the National Comprehensive Cancer Network clinical practice guidelines in oncology. 2 , 8 , 9
Interestingly, there are experimental findings showing that a combination therapy of trastuzumab and lapatinib, which is also a TTD targeting HER2, reduces trastuzumab‐induced cardiotoxicity. 1 , 10 In addition, it has been demonstrated that some drugs, such as tamoxifen and paroxetine, which are commonly prescribed with trastuzumab have cardio‐protective effects in combination with other breast cancer drugs or themselves. 11 , 12 , 13 , 14 , 15 , 16 From these facts we can infer that concomitant uses of these drugs during treatment with trastuzumab may reduce trastuzumab‐induced cardiotoxicity.
In this research, we utilized the applied patient‐centered reverse translational systems‐based approach to explore the underlying molecular mechanisms causing cardiotoxicity induced by monotherapy of trastuzumab and how cardiotoxicity may change when trastuzumab is given in combination with doxorubicin, tamoxifen, paroxetine, or lapatinib. To this end, population ADR reports from the US Food and Drug Administration (FDA) Adverse Event Reporting System (FAERS) database 17 mapped to chemical and biological databases were analyzed using the Molecular Health’s Effect (MH Effect) 18 analytical platform in order to frame several hypotheses regarding the changes in molecular mechanisms of cardiotoxicity due to the DDIs. This patient‐centered reverse translational systems‐based approach provides an example for a detailed investigation of ADRs at the pathway and target level to untangle the complex network of ADRs and to create a hypothesis toward drug safety predictions.
METHODS
ADR cases reported in the FAERS database were analyzed using the MH Effect (version 1.7). The following sections describe the FAERS, MH Effect, and our approach in detail as well as how we compared and evaluated our findings with previously published experimental data in PubMed.
FDA adverse event reporting system
FAERS is a postmarket surveillance database of ADRs submitted to the FDA. 17 , 19 It provides a rich source of ADR information submitted voluntarily by drug manufacturers, healthcare professionals, and consumers in the United States. Over 19,750,000 ADR reports were submitted from 1969 to the present, and the number of reports increases every year. 17 The ADR reports are evaluated by clinical reviewers before being publicly released on a quarterly basis by the FDA.
Molecular Health Effect
The MH Effect is a data warehouse platform that contains and maps population ADR data from FAERS with protein information, molecular targets, and pathway data (Figure 1). It enables a comprehensive analysis of molecular targets and mechanisms associated with ADRs to untangle the complexity of the underlying molecular mechanisms of spontaneous ADRs. 20 , 21 The protein and pathway mapping are established based on information of entries from DrugBank, PubChem, UniProt, NCI‐Nature, Reactome, and BioCarta.
FIGURE 1.
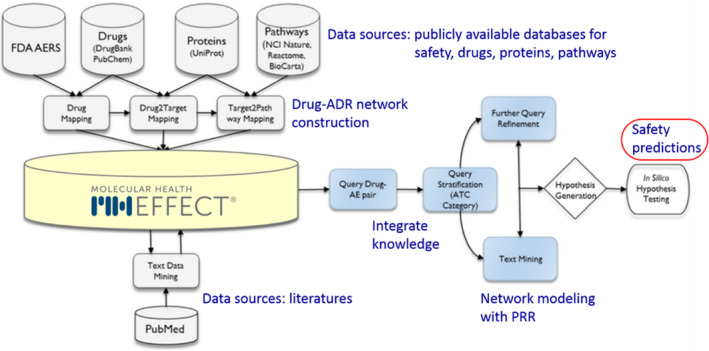
Schematic overview of the data integration process mapping FDA Adverse Event Reporting System (FAERS) data with molecular data using Molecular Health Effect. This figure was adapted from Schotland et al. 42 AE, adverse event; ATC, Anatomic Therapeutic Chemical; FDA, US Food and Drug Administration; NCI, National Cancer Institute; PRR, proportional reporting ratio
In MH Effect version 1.7, used for this proof‐of‐concept study, FAERS data were included up to the fourth quarter (Q4)/2019. Reported ADRs associated with trastuzumab and four other drugs that are typically given in combination with trastuzumab in patients with breast cancer, namely doxorubicin, tamoxifen, paroxetine, and lapatinib, were collected from the first quarter (Q1)/2008 to Q4/2019. Data were collected from approximately a year after the latest approval among the five investigated drugs (i.e., March 13, 2007, for lapatinib) in order to reduce statistical bias driven by the gap before the newest drug was introduced and prescribed.
There are a total of 18 combinations (i.e., cohorts) examined in this analysis (Figure 2). First, ADR cases associated with each of the five investigated drugs were collected. From the ADR cases associated with trastuzumab, four subsets were created, including the cases reported with each of the other four drugs in combination. In order to focus on molecular targets and mechanisms that might be synergistic to increase trastuzumab‐induced cardiotoxicity, we further explored subsets of all nine drug combinations after filtering out cases that do not include cardiotoxicity among reported ADRs (Figure 2: cohort B). As all cases in such subsets were already exposed by effects of cardiotoxicity, we explored the collected cases, including all reported ADRs for possible molecular mechanisms reducing cardiotoxic effects (Figure 2: cohort A). The Preferred Term (PT) named “Cardiotoxicity” was used from the MedDRA hierarchy to define “cardiotoxic” ADRs (MedDRA version 22.1; PT refers to level 4 of the hierarchy).
FIGURE 2.
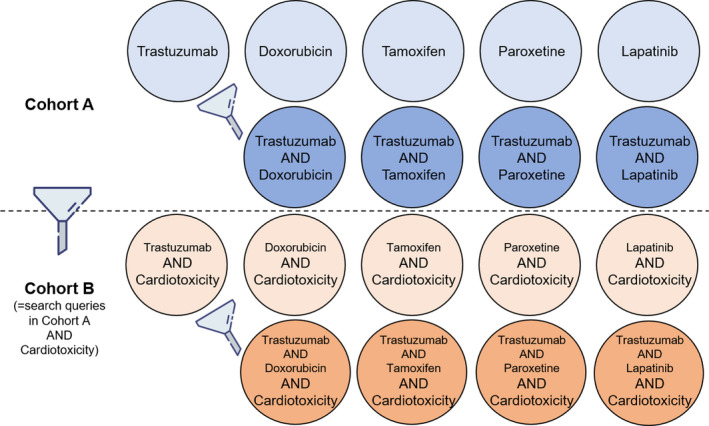
Cohort building. In cohort A, there are nine cohorts collected using drug name(s) in search queries. We collected adverse drug reaction (ADR) cases associated with each of the five investigated drugs (i.e., trastuzumab, doxorubicin, tamoxifen, paroxetine, and lapatinib). In the ADR cases associated with trastuzumab, we made four subsets of the cases reported with each of the other four drugs together. In cohort B, both drug name(s) and cardiotoxicity were used in search queries to filter out cases that do not include cardiotoxicity among reported ADRs from each of the nine cohorts. Data were collected from Q1/2008 to Q4/2019 in all cohorts
Disproportionality analysis
The proportional reporting ratio (PRR) was used to assess the statistical relevance between the query entity and events of interest. 22 The PRR, commonly used in pharmacovigilance (PhVg), is one of the methods of disproportionality analysis that have the advantage of reducing uncertainty from the spontaneously reported data. The MH Effect calculates the PRR according to its definition which is a / (a + b) divided by c / (c + d) where a is the number of cases reported with the query entities and events of interest, b is the number of cases reported with the query entities and all events except the events of interest, c is the number of cases reported with the events of interest and all others in the categories of the query entities in the database except the query entities, and d is the number of cases reported with all events in the database but without the query entities and events of interest. 22 , 23 In addition, we determined if the signal is statistically significant using two traditional PhVg criteria: (i) three or more of the number of the ADR case reports and (ii) two or greater of the lower bound of the 95% confidence interval (CI) of the PRR. 22
Comparison with experimental findings found in PubMed
To examine the hypotheses we established using the MH Effect, we compared our results with findings from previous experimental studies published in PubMed. 1 , 15 , 16 , 22 , 24 , 25 , 26 , 27 , 28 , 29 Synonyms of the biological molecules showing high statistical relevance according to the PRR in the MH Effect were used during the literature search.
RESULTS
Drug combinations and cardiotoxicity
The statistical association between the drugs and cardiotoxicity for the chosen combinations is presented in Table 1. Both trastuzumab and doxorubicin are cardiotoxic drugs that have statistically significant PRRs regarding cardiotoxicity. Trastuzumab showed the highest statistical association with cardiotoxicity followed by doxorubicin out of the investigated drugs. Concomitant use of trastuzumab and doxorubicin led to a more than twofold increase in the PRR of cardiotoxicity, compared to that of trastuzumab alone.
TABLE 1.
Statistical associations between the drug combinations and cardiotoxicity. Listed results are based on reported ADRs in cohort A
| Drug(s) | N of all ADRs |
N including cardiotoxicity |
PRR associated with cardiotoxicity (95% CI) |
|---|---|---|---|
| Trastuzumab | 31,795 | 438 | 46.33 (41.97–51.14) |
| Doxorubicin | 62,792 | 723 | 42.15 (38.89–45.69) |
| Tamoxifen | 12,085 | 31 | 7.72 (5.42–10.98) |
| Paroxetine | 49,088 | 5 | 0.3 (0.13–0.73) |
| Lapatinib | 12,858 | 61 | 14.38 (11.18–18.51) |
| Trastuzumab and doxorubicin | 2049 | 75 | 111.5 (89.09–139.56) |
| Trastuzumab and tamoxifen | 1383 | 27 | 58.72 (40.37–85.43) |
| Trastuzumab and paroxetine | 139 | 0 | n/a (n/a) |
| Trastuzumab and lapatinib | 2881 | 35 | 36.61 (26.3–50.97) |
Data collection period = Q1/2008 to Q4/2019.
Abbreviations: ADR, adverse drug reaction; CI, confidence interval; N, number of case reports; PRR, Proportional Reporting Ratio.
The other drugs for example, tamoxifen (hormonal therapy), paroxetine (antidepressant), and lapatinib, showed much lower numbers of ADR reports, including cardiotoxicity and lower PRRs associated with cardiotoxicity, as compared to trastuzumab and doxorubicin (Table 1). For the reported ADR cases with both tamoxifen and trastuzumab, the PRR associated with cardiotoxicity was slightly higher but the number of such cases was much less compared to those of trastuzumab alone. Paroxetine did not have a statistically significant PRR associated with cardiotoxicity with respect to the applied PhVg criteria. 22 Moreover, there were zero ADR cases of cardiotoxicity reported with the combination therapy of paroxetine and trastuzumab. Although lapatinib is also a TTD targeting HER2‐like trastuzumab, the PRR between lapatinib and cardiotoxicity was threefold lower than that of trastuzumab. Moreover, it is notable that concomitant use of these two TTDs decreased trastuzumab‐induced cardiotoxicity with respect to the PRR. However, the 95% CIs of the PRR of the combination therapies with either tamoxifen or lapatinib overlap with the one of trastuzumab alone.
Trastuzumab‐induced cardiotoxicity
In MH Effect, 746 molecular mechanisms were mapped with cases associated with trastuzumab and cardiotoxicity (Table 2). When ranking them using the PRR, we found that molecular mechanisms of apoptosis regulator proteins of BCL‐2 members have a strong statistical association with trastuzumab‐induced cardiotoxicity. In particular, the PRRs were high with a mechanism of inactivation of anti‐apoptotic BCL‐2 members as well as a mechanism of activation of the pro‐apoptotic BAD protein that is a BCL‐2 associated death promoter. As a result, a molecular mechanism related to mitochondria and increased apoptosis through intrinsic death receptor (BAD) signaling showed a high PRR.
TABLE 2.
Major molecular mechanisms related to trastuzumab‐induced cardiotoxicity
| Ranking (total: 746) | Molecular mechanisms | N (total: 438) | PRR (95% CI) |
|---|---|---|---|
| 1 | Signaling by ERBB2 (HER2) | 438 | 85.83 (85.38–86.29) |
| 4 | Signaling by ERBB4 | 438 | 57.7 (57.45–57.95) |
| 8 | ERBB receptor signaling network | 438 | 50.53 (50.32–50.74) |
| 33 | Bh3‐only proteins associated with and inactivate anti‐apoptotic BCL‐2 members | 209 | 15.93 (14.44–17.58) |
| 35 | Activation of BAD and translocation to mitochondria | 209 | 15.81 (14.33–17.44) |
| 38 | Role of mitochondria in apoptotic signaling | 209 | 15.38 (13.94–16.96) |
The total number of 746 molecular mechanisms, which are associated with the 438 cases reported with trastuzumab and cardiotoxicity together (i.e., cohort B), were ranked by PRR.
Data collection period = Q1/2008 to Q4/2019.
Abbreviations: CI, confidence interval; N, number of case reports; PRR, Proportional Reporting Ratio.
Through literature review, we validated that these mechanisms induce mitochondria dysfunction and caspase activation through BCL‐2 family proteins, leading to cardiotoxicity (Figure 3). 1 In addition, previous experimental findings support that HER2 inhibition by trastuzumab leads to a decrease in an anti‐apoptotic member of the BCL‐2 family, BCL‐xL, and an increase in a pro‐apoptotic member, BCL‐xS. 24 Loss of mitochondrial membrane potential and caspase activation occur as results of the mechanisms. 1 , 24
FIGURE 3.
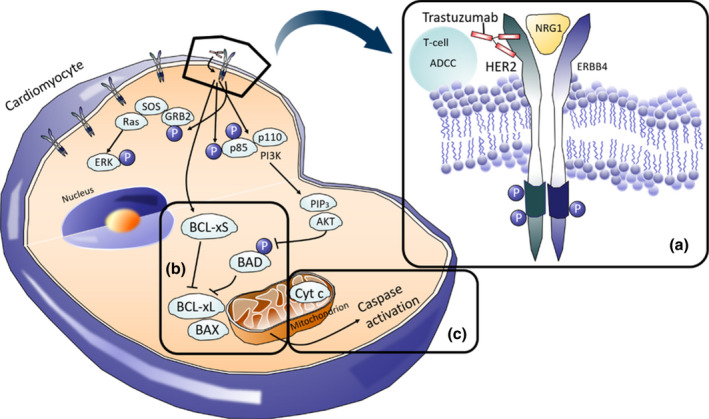
HER2 signaling and mitochondrial dysfunction in cardiomyocytes. Targeting the HER2 receptor (a) may induce mitochondria dysfunction and caspase activation (c) through BCL‐2 family proteins (b), leading to cardiotoxicity. Figure is adapted from reference 1
Drug‐drug interactions increasing trastuzumab‐induced cardiotoxicity
Concomitant use of doxorubicin with trastuzumab increased the PRRs of molecular mechanisms triggering apoptosis through BCL‐2 members, compared to trastuzumab alone (Table 3). Both toxic mechanisms (i.e., inactivation of anti‐apoptotic BCL‐2 members and activation of BAD), showed higher PRRs in the ADR cases, including both drugs included in the search queries. In addition, it has been known that binding doxorubicin to topoisomerase II (top2) in cardiomyocytes downregulates peroxisome proliferator‐activated receptor‐γ coactivator 1‐α (PGC‐1α) and PGC‐1β, which are critical for the mitochondrial biogenesis and function. 30 , 31 , 32 The PRRs of the Peroxisome proliferator activated receptor‐α (PPARα)‐related mechanisms were low (<1.25) in all three cohorts, and the values were statistically insignificant when comparing the quantities. 22 The resultant molecular mechanism (i.e., role of mitochondria in apoptotic signaling), also showed a higher PRR, indicating the increased risk of developing cardiotoxicity. Thus, we hypothesize that the combination therapy of trastuzumab and doxorubicin may induce a synergistic effect of mitochondrial dysfunction in cardiomyocytes through different molecular pathways of the BCL‐2 family and PPAR proteins, leading to an increased risk of developing cardiotoxicity.
TABLE 3.
Molecular mechanisms increasing trastuzumab‐induced cardiotoxicity
| Drug(s) | Molecular mechanisms | N | PRR (95% CI) |
|---|---|---|---|
| Trastuzumab | BH3‐only proteins associated with and inactivate anti apoptotic BCL‐2 members | 209 | 15.93 (14.44–17.58) |
| Doxorubicin | 88 | 4.06 (3.34–4.94) | |
| Trastuzumab and doxorubicin | 57 | 25.37 (22.34–28.81) | |
| Trastuzumab | Activation of BAD and translocation to mitochondria | 209 | 15.81 (14.33–17.44) |
| Doxorubicin | 88 | 4.03 (3.31–4.9) | |
| Trastuzumab and doxorubicin | 57 | 25.17 (22.16–28.59) | |
| Trastuzumab | PPARα activates gene expression | 76 | 0.55 (0.44–0.67) a |
| Doxorubicin | 285 | 1.24 (1.13–1.36) a | |
| Trastuzumab and doxorubicin | 27 | 1.13 (0.84–1.53) a | |
| Trastuzumab | Role of mitochondria in apoptotic signaling | 209 | 15.38 (13.94–16.96) |
| Doxorubicin | 88 | 3.92 (3.22–4.77) | |
| Trastuzumab and doxorubicin | 57 | 24.48 (21.56–27.8) |
The PRR represents the statistical association quantity of how much the molecular mechanism is associated with both the drug(s) and cardiotoxicity in cohort B.
Data collection period = Q1/2008 to Q4/2019.
Abbreviations: CI, confidence interval; N, number of case reports; PRR, Proportional Reporting Ratio.
Statistically insignificant.
Drug‐drug interactions decreasing trastuzumab‐induced cardiotoxicity
Concomitant use of tamoxifen with trastuzumab increased the PRRs of molecular mechanisms involved in protecting cardiomyocytes (Table 4). Two molecular mechanisms describing the calcineurin‐mediated nuclear factor of activated T cells (NFAT) signaling pathways showed higher PRRs when both drugs were included in the search queries, compared to trastuzumab alone. Thus, we inferred that the combination therapy with tamoxifen might enhance calcineurin activity, resulting in cardiac hypertrophy. Although hypertrophy is considered as one of the varieties of pathological conditions of cardiotoxicity, it has been demonstrated that calcineurin‐mediated hypertrophy protects cardiomyocytes from apoptosis as well as the activation of calcineurin itself downregulates apoptosis by increasing anti‐apoptotic BCL‐2 proteins. 25 , 26 , 27 Therefore, we hypothesize that the combination therapy of trastuzumab and tamoxifen may reduce trastuzumab‐induced cardiotoxicity by stimulating the anti‐apoptotic effect through calcineurin‐dependent pathways.
TABLE 4.
Molecular mechanisms decreasing trastuzumab‐induced cardiotoxicity
| Drug(s) | Molecular Mechanisms | N | PRR (95% CI) |
|---|---|---|---|
| Trastuzumab | Role of calcineurin‐dependent NFAT signaling in lymphocytes | 17,725 | 5.76 (5.7–5.81) |
| Tamoxifen | 12,085 | 10.29 (10.27–10.31) | |
| Trastuzumab and tamoxifen | 1383 | 10.2 (10.18–10.22) | |
| Trastuzumab | Calcineurin‐regulated NFAT‐dependent transcription in lymphocytes | 6086 | 0.63 (0.61–0.64) a |
| Tamoxifen | 12,085 | 3.28 (3.27–3.28) | |
| Trastuzumab and tamoxifen | 1383 | 3.27 (3.27–3.27) | |
| Trastuzumab | Glutathione conjugation | 8331 | 2.92 (2.87–2.98) |
| Paroxetine | 2008 | 1.84 (1.77–1.92) a | |
| Trastuzumab and paroxetine | 419 | 3.36 (3.1–3.64) | |
| Trastuzumab | BH3‐only proteins associated with and inactivate anti‐apoptotic BCL‐2 members | 17,001 | 18.72 (18.52–18.93) |
| Lapatinib | 2332 | 6.09 (5.87–6.32) | |
| Trastuzumab and lapatinib | 1600 | 18.62 (18.01–19.24) | |
| Trastuzumab | Activation of BAD and translocation to mitochondria | 17,008 | 18.58 (18.38–18.78) |
| Lapatinib | 2335 | 6.05 (5.83–6.27) | |
| Trastuzumab and lapatinib | 1603 | 18.51 (17.91–19.12) | |
| Trastuzumab | Activated AMPK stimulates fatty‐acid oxidation in muscle | 1289 | 0.52 (0.49–0.55) a |
| Lapatinib | 396 | 0.39 (0.36–0.43) a | |
| Trastuzumab and lapatinib | 112 | 0.5 (0.42–0.6) a |
The PRR represents the statistical association quantity of how much the molecular mechanism is associated with the drug(s) and all reported ADRs in cohort A.
Data collection period = Q1/2008 to Q4/2019.
Abbreviations: ADR, adverse drug reaction; CI, confidence interval; N, number of case reports; PRR, Proportional Reporting Ratio.
Statistically insignificant.
For the concomitant use of paroxetine with trastuzumab, we found that the PRR of the mechanisms of glutathione conjugate increased in the combination cohort (Table 4). Paroxetine reduces oxidative stress by replenishing glutathione and its antihypertensive properties, which may attenuate cardiotoxic effects. 15 , 16 , 28 Therefore, we hypothesize that paroxetine may reduce trastuzumab‐induced cardiotoxicity by promoting the antioxidant activity of glutathione.
Last, the concomitant use of lapatinib with trastuzumab showed slightly less PRRs of the toxic molecular mechanisms related to the BCL‐2 apoptosis regulator proteins (Table 4). In addition, published findings suggest that lapatinib may reduce trastuzumab‐induced cardiotoxicity by activating adenosine monophosphate‐activated protein kinase (AMPK), whereas trastuzumab reduces AMPK. 29 We explored the AMPK‐related molecular mechanisms, but the PRRs were too low to be statistically significant (Table 4). 22 Thus, we hypothesize that lapatinib might alter the effect of trastuzumab on BCL‐2 family proteins to mediate mitochondrial dysfunction in cardiomyocytes.
DISCUSSION
Whereas trastuzumab inhibits HER2 signaling, doxorubicin acts on top2. 30 Acting on different pharmacological targets leads to a reduced death rate of patients with breast cancer by 30% through concomitant use of the drugs. 33 The high risk of cardiotoxic ADRs, however, often terminates the combination therapy of trastuzumab and doxorubicin. The mechanism of cardiotoxicity induced by each one of the two drugs of the combination seems to be distinct from one another as the characteristics of the ADR are different. 1 For example, trastuzumab‐induced cardiotoxicity is not dose‐dependent, and it is not associated with ultrastructural changes so it is at least partially reversible. 1 , 10 On the other hand, doxorubicin‐induced cardiotoxicity correlates with total cumulative dose, and it is associated with changes in myocardial ultrastructure and hence it is irreversible. 1 , 33 In this work, we explored possible changes of molecular cardiotoxic causation when trastuzumab is given in combination with doxorubicin. In addition, we explored how trastuzumab‐induced cardiotoxicity would be reduced when trastuzumab is given in combination with one of the other drugs under investigation in this analysis, such as tamoxifen, paroxetine, and lapatinib. About four out of every five cases of breast cancer are estrogen receptor (ER) positive, which means there are excessive receptors binding the hormone estrogen. 34 The signaling of ER promotes the growth of cancer cells, and tamoxifen inhibits its signaling. 35 It has been suggested that ER and HER2 are inhibited by tamoxifen and trastuzumab, respectively, at the same time based on the rationale that both receptors are therapeutic targets. 35 , 36 Experiments counting cell accumulations during phases of the cell cycle of BT‐474 cells and measuring the percentage of living cells of breast cancer cells demonstrated that the combination therapy of trastuzumab and tamoxifen has better efficacy than monotherapy with either agent. 35 , 37
Our results indicate that the concomitant use of trastuzumab and tamoxifen has the higher PRR associated with cardiotoxicity, compared to each drug alone (Table 1). However, this is based on only 27 cases. For this reason, we tested the hypothesis further by investigating at the molecular level and cross‐examined it with literature. We found that the molecular level analysis supported that the trastuzumab and tamoxifen combination may instead lower the risk of cardiotoxicity (Table 4). Even though it is still ambiguous whether the concomitant use of trastuzumab and tamoxifen has an advantage in reducing cardiac side effects induced by trastuzumab, some studies indicate tamoxifen has cardioprotective effects. 11 , 12 , 13 , 14 In addition, Silva et al. evaluated the recovering effects of tamoxifen after chemotherapy by measuring the left ventricular ejection fraction (LVEF) and a plasma level of NT‐pro‐B‐type natriuretic peptide (NT‐proBNP), which is a biomarker of cardiac dysfunction. 12 Although their study was not directly related to the combination therapy with trastuzumab, it was proven that tamoxifen restored the levels of LVEF and NT‐proBNP that were changed due to chemotherapy to the initial degrees at the beginning of treatment. 12
Paroxetine has been prescribed to be given in combination with anticancer drugs, including trastuzumab to treat depression frequently observed in the majority of patients with cancer; at least 25% of patients with breast cancer experience depressive disorders. 38 , 39 In our analysis, paroxetine showed cardioprotective effects.
Lapatinib is a small molecule inhibitor of the epidermal growth factor receptor and HER2. Targeting distinct sides on the HER2 receptor concomitantly via different mechanisms of action by lapatinib and trastuzumab enhances efficacy versus when either agent is given as monotherapy. 5 , 40 Concomitant use of lapatinib with trastuzumab has a further tactical advantage from a safety perspective because lapatinib has minimal cardiotoxicity and even it reduces the trastuzumab‐induced cardiotoxicity while it targets HER2 as trastuzumab does. 1 , 6
Nevertheless, we acknowledge the limitations of our analysis using FAERS data. One limitation is that similar symptoms of cardiotoxicity could have been reported in FAERS using different terms in MedDRA. 41 In addition, the general definition or threshold of cardiotoxicity is still ambiguous despite attempts to define cardiotoxicity in terms of a reduction in LVEF. 8 Moreover, due to limited information, it was not accounted whether the examined drugs were given in combination at the same time or if one was started after discontinuation of the other. In addition, disease stages (or severity) of cardiotoxicity were not provided in FAERS. Other limitations of this analysis and of FAERS data include (i) the possibility of misstatements of indications, (ii) ADRs attributed to additionally co‐administered medications, (iii) difficulty for risk assessment of over‐the‐counter drugs, and (iv) uncertainty that a given ADR is causally related to the drug product or due to other risk factors, such as patient characteristics, including age, smoking status, and history of coronary artery disease. 42 , 43 , 44 , 45 , 46
Although many questions still remain to develop better methodologies to mechanistically investigate ADRs using spontaneous reporting databases, this systems‐based approach provides an exemplar for a detailed investigation of an ADR (i.e., cardiotoxicity), due to DDIs at the pathway and target levels and provides a process to better understand drug pair adverse events. Mapping real‐world population data to the protein and pathway databases enables mechanistic investigation into the molecular pathways and provides the scientific rationale for potentially mitigating cardiotoxicity of trastuzumab and doxorubicin, as a single agent or in combination. Using this approach, Schotland et al. was able to show improved accuracy of the safety evaluation using postmarket reporting databases. 47
In this work, we investigated the underlying molecular mechanisms of cardiotoxicity induced by trastuzumab, and explored signal alterations caused by DDIs with other drugs typically given in combination with trastuzumab in patients with breast cancer. In the future, once additional ADR events have been reported, an investigation focusing on different types of heart disorders and/or subpopulations could be performed (e.g., for QT prolongation, heart failure, or bradycardia).
We conclude that the combination therapy of trastuzumab and doxorubicin may induce a synergistic effect of mitochondrial dysfunction in cardiomyocytes through different molecular pathways of BCL‐2 and PPARα proteins, whereas other combinations with the hormone therapy tamoxifen, the antidepressant paroxetine, and another TTD lapatinib may reduce trastuzumab‐induced cardiotoxicity by stimulating the anti‐apoptotic effect of calcineurin signaling pathways, by promoting the antioxidant activity of glutathione, and by changing the effects of trastuzumab on BCL‐2 family proteins, respectively. Our findings are consistent with previous experimental results and we anticipate that the systems‐based approach we applied will contribute to the progress made in understanding the mechanisms of trastuzumab‐induced cardiotoxicity. In addition, this methodology provides an example for the detailed mechanistic investigation of ADRs due to monotherapy or DDIs at the molecular pathway and target levels and a process helping to better understand drug pair adverse events. This patient‐centered reverse translational systems‐based approach could be useful to back translate and inform drug development pipelines not only in oncology but also in other disease areas to predict the probability of ADR events already during early stage drug development for a novel therapeutic.
CONFLICT OF INTEREST
The authors declared no competing interests for this work.
AUTHOR CONTRIBUTIONS
S.K., G.L., M.V., D.B.J., T.G.S., L.J.L., and M.N.T. wrote the manuscript. S.K., L.J.L. and M.N.T. designed the research. S.K. and M.N.T. performed the research. S.K., G.L., M.V., D.B.J., T.G.S., L.J.L., and M.N.T. analyzed the data. D.B.J. and T.G.S. provided new reagents/analytical tools.
ACKNOWLEDGEMENTS
The authors would like to acknowledge David Jackson from Molecular Health Effect for his generous support of this research and software access.
Kim S, Lahu G, Vakilynejad M, et al. A case study of a patient‐centered reverse translational systems‐based approach to understand adverse event profiles in drug development. Clin Transl Sci. 2022;15:1003‐1013. doi: 10.1111/cts.13219
Funding information
This work was sponsored by Takeda Pharmaceutical Inc, Cambridge, Massachusetts
REFERENCES
- 1. Force T, Krause DS, Van Etten RA. Molecular mechanisms of cardiotoxicity of tyrosine kinase inhibition. Nat Rev Cancer. 2007;7:332‐344. [DOI] [PubMed] [Google Scholar]
- 2. Popat S, Smith IE. Therapy Insight: anthracyclines and trastuzumab–the optimal management of cardiotoxic side effects. Nat Clin Pract Oncol. 2008;5:324‐335. [DOI] [PubMed] [Google Scholar]
- 3. Gordon LI, Burke MA, Singh AT, et al. Blockade of the erbB2 receptor induces cardiomyocyte death through mitochondrial and reactive oxygen species‐dependent pathways. J Biol Chem. 2009;284:2080‐2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hanigan MH, Dela Cruz BL, Thompson DM, Farmer KC, Medina PJ. Use of prescription and nonprescription medications and supplements by cancer patients during chemotherapy: questionnaire validation. J Oncol Pharm Pract. 2008;14:123‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xia W, Gerard CM, Liu L, Baudson NM, Ory TL, Spector NL. Combining lapatinib (GW572016), a small molecule inhibitor of ErbB1 and ErbB2 tyrosine kinases, with therapeutic anti‐ErbB2 antibodies enhances apoptosis of ErbB2‐overexpressing breast cancer cells. Oncogene. 2005;24:6213‐6221. [DOI] [PubMed] [Google Scholar]
- 6. Spector NL, Yarden Y, Smith B, et al. Activation of AMP‐activated protein kinase by human EGF receptor 2/EGF receptor tyrosine kinase inhibitor protects cardiac cells. Proc Natl Acad Sci USA. 2007;104:10607‐10612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Witteles R. Type I and Type II Cardiomyopathy Classifications Are Complete Nonsense: PRO. American College of Cardiology; 2018. https://www.acc.org/latest‐in‐cardiology/articles/2018/05/04/08/41/type‐i‐and‐type‐ii‐cardiomyopathy‐classifications‐are‐complete‐nonsense‐pro. Accessed April 29, 2021. [Google Scholar]
- 8. Albini A, Pennesi G, Donatelli F, Cammarota R, De Flora S, Noonan DM. Cardiotoxicity of anticancer drugs: the need for cardio‐oncology and cardio‐oncological prevention. J Natl Cancer Inst. 2010;102:14‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. NCCN Clinical Practice Guidelines in Oncology ‐ Breast Cancer (Version 3.2020). 2020. https://www.nccn.org/patients/. Accessed August 3, 2020.
- 10. Adão R, de Keulenaer G, Leite‐Moreira A, Brás‐Silva C. Cardiotoxicity associated with cancer therapy: pathophysiology and prevention strategies. Rev Port Cardiol. 2013;32:395‐409. [DOI] [PubMed] [Google Scholar]
- 11. Ek RO, Yildiz Y, Cecen S, Yenisey C, Kavak T. Effects of tamoxifen on myocardial ischemia‐reperfusion injury model in ovariectomized rats. Mol Cell Biochem. 2008;308:227‐235. [DOI] [PubMed] [Google Scholar]
- 12. Silva FB, Romero WG, Carvalho AL, et al. Hormone therapy with tamoxifen reduces plasma levels of NT‐B‐type natriuretic peptide but does not change ventricular ejection fraction after chemotherapy in women with breast cancer. Braz J Med Biol Res. 2015;48:154‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pedram A, Razandi M, Aitkenhead M, Levin ER. Estrogen inhibits cardiomyocyte hypertrophy in vitro. Antagonism of calcineurin‐related hypertrophy through induction of MCIP1. J Biol Chem. 2005;280:26339‐26348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Day BJ. Catalase and glutathione peroxidase mimics. Biochem Pharmacol. 2009;77:285‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yeragani VK, Pesce V, Jayaraman A, Roose S. Major depression with ischemic heart disease: effects of paroxetine and nortriptyline on long‐term heart rate variability measures. Biol Psychiat. 2002;52:418‐429. [DOI] [PubMed] [Google Scholar]
- 16. Golding M, Kotlyar M, Carson SW, et al. Effects of paroxetine on cardiovascular response to mental stress in subjects with a history of coronary artery disease and no psychiatric diagnoses. Psychopharmacology. 2005;182:321‐326. [DOI] [PubMed] [Google Scholar]
- 17. FDA Adverse Event Reporting System (FAERS) Public Dashboard. U.S. Food & Drug Administration; 2019. https://www.fda.gov/drugs/questions‐and‐answers‐fdas‐adverse‐event‐reporting‐system‐faers/fda‐adverse‐event‐reporting‐system‐faers‐public‐dashboard. Accessed August 3, 2020. [Google Scholar]
- 18. MH Effect . Molecular Health GmbH, 2019. https://www.molecularhealth.com/us/2017/11/17/molecular‐health‐and‐fda‐us/). Accessed August 3, 2020.
- 19. Questions and Answers on FDA's Adverse Event Reporting System (FAERS). U.S. Food & Drug Administration; 2018. https://www.fda.gov/drugs/surveillance/questions‐and‐answers‐fdas‐adverse‐event‐reporting‐system‐faers. Accessed August 3, 2020. [Google Scholar]
- 20. Soldatos TG, Jackson DB. Adverse Event Circumstances and the Case of Drug Interactions. Healthcare; 2019; 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Soldatos TG, Taglang G, Jackson DB. In silico profiling of clinical phenotypes for human targets using adverse event data. High‐Throughput. 2018;7(4):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Evans SJ, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf. 2001;10:483‐486. [DOI] [PubMed] [Google Scholar]
- 23. Bate A, Evans SJ. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf. 2009;18:427‐436. [DOI] [PubMed] [Google Scholar]
- 24. Grazette LP, Boecker W, Matsui T, et al. Inhibition of ErbB2 causes mitochondrial dysfunction in cardiomyocytes: implications for herceptin‐induced cardiomyopathy. J Am Coll Cardiol. 2004;44:2231‐2238. [DOI] [PubMed] [Google Scholar]
- 25. De Windt LJ, Lim HW, Taigen T, et al. Calcineurin‐mediated hypertrophy protects cardiomyocytes from apoptosis in vitro and in vivo: an apoptosis‐independent model of dilated heart failure. Circ Res. 2000;86:255‐263. [DOI] [PubMed] [Google Scholar]
- 26. Molkentin JD. Calcineurin, mitochondrial membrane potential, and cardiomyocyte apoptosis. Circ Res. 2001;88:1220‐1222. [DOI] [PubMed] [Google Scholar]
- 27. Kakita T, Hasegawa K, Iwai‐Kanai E, et al. Calcineurin pathway is required for endothelin‐1‐mediated protection against oxidant stress‐induced apoptosis in cardiac myocytes. Circ Res. 2001;88:1239‐1246. [DOI] [PubMed] [Google Scholar]
- 28. Gero D, Szoleczky P, Suzuki K, et al. Cell‐based screening identifies paroxetine as an inhibitor of diabetic endothelial dysfunction. Diabetes. 2013;62:953‐964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shell SA, Lyass L, Trusk PB, Pry KJ, Wappel RL, Bacus SS. Activation of AMPK is necessary for killing cancer cells and sparing cardiac cells. Cell Cycle (Georgetown, Tex). 2008;7:1769‐1775. [DOI] [PubMed] [Google Scholar]
- 30. Zhang S, Liu X, Bawa‐Khalfe T, et al. Identification of the molecular basis of doxorubicin‐induced cardiotoxicity. Nat Med. 2012;18:1639‐1642. [DOI] [PubMed] [Google Scholar]
- 31. Vejpongsa P, Yeh ET. Prevention of anthracycline‐induced cardiotoxicity: challenges and opportunities. J Am Coll Cardiol. 2014;64:938‐945. [DOI] [PubMed] [Google Scholar]
- 32. Mohan N, Jiang J, Dokmanovic M, Wu WJ. Trastuzumab‐mediated cardiotoxicity: current understanding, challenges, and frontiers. Antib Ther. 2018;1:13‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rochette L, Guenancia C, Gudjoncik A, et al. Anthracyclines/trastuzumab: new aspects of cardiotoxicity and molecular mechanisms. Trends Pharmacol Sci. 2015;36:326‐348. [DOI] [PubMed] [Google Scholar]
- 34. Types of Breast Cancer: ER‐Positive, HER2‐Positive, and Triple Negative. WebMD. http://www.webmd.com/breast‐cancer/guide/breast‐cancer‐types‐er‐positive‐her2‐positive. Accessed August 6, 2020.
- 35. Argiris A, Wang CX, Whalen SG, DiGiovanna MP. Synergistic interactions between tamoxifen and trastuzumab (Herceptin). Clin Cancer Res. 2004;10:1409‐1420. [DOI] [PubMed] [Google Scholar]
- 36. Jones A. Combining trastuzumab (Herceptin) with hormonal therapy in breast cancer: what can be expected and why? Ann Oncol. 2003;14:1697‐1704. [DOI] [PubMed] [Google Scholar]
- 37. Ropero S, Abel Menéndez J, Vázquez‐Martín A, Montero S, Cortés‐Funes H, Colomer R. Trastuzumab plus tamoxifen: anti‐proliferative and molecular interactions in breast carcinoma. Breast Cancer Res Treat. 2004;86:125‐137. [DOI] [PubMed] [Google Scholar]
- 38. Kelly CM, Juurlink DN, Gomes T, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. BMJ. 2010;340:c693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Henry NL, Stearns V, Flockhart DA, Hayes DF, Riba M. Drug interactions and pharmacogenomics in the treatment of breast cancer and depression. Am J Psychiatry. 2008;165:1251‐1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Blackwell KL, Burstein HJ, Storniolo AM, et al. Randomized study of Lapatinib alone or in combination with trastuzumab in women with ErbB2‐positive, trastuzumab‐refractory metastatic breast cancer. J Clin Oncol. 2010;28:1124‐1130. [DOI] [PubMed] [Google Scholar]
- 41. MedDRA: Medical Dictionary for Regulatory Activities. https://www.meddra.org/.
- 42. Schotland P, Bojunga N, Zien A, Trame MN, Lesko LJ. Improving drug safety with a systems pharmacology approach. Eur J Pharm Sci. 2016;94:84‐92. [DOI] [PubMed] [Google Scholar]
- 43. Stephenson WP, Hauben M. Data mining for signals in spontaneous reporting databases: proceed with caution. Pharmacoepidemiol Drug Saf. 2007;16:359‐365. [DOI] [PubMed] [Google Scholar]
- 44. Schotland P, Racz R, Jackson D, Levin R, Strauss DG, Burkhart K. Target‐adverse event profiles to augment pharmacovigilance: a pilot study with six new molecular entities. CPT Pharmacometrics Syst Pharmacol. 2018;7:809‐817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Soldatos TG, Iakovou I, Sachpekidis C. Retrospective toxicological profiling of radium‐223 dichloride for the treatment of bone metastases in prostate cancer using adverse event data. Medicina (Kaunas, Lithuania). 2019;55(5):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sachpekidis C, Jackson DB, Soldatos TG. Radioimmunotherapy in Non‐Hodgkin's Lymphoma: retrospective adverse event profiling of Zevalin and Bexxar. Pharmaceuticals. 2019;12:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Schotland P, Racz R, Jackson DB, et al. Target adverse event profiles for predictive safety in the postmarket setting. Clin Pharmacol Ther. 2021;109:1232‐1243. [DOI] [PMC free article] [PubMed] [Google Scholar]


