Abstract
OBJECTIVE:
To assess the association between usual dietary sodium intake and blood pressure among US children and adolescents, overall and by weight status.
METHODS:
Children and adolescents aged 8 to 18 years (n = 6235) who participated in NHANES 2003–2008 comprised the sample. Subjects’ usual sodium intake was estimated by using multiple 24-hour dietary recalls. Linear or logistic regression was used to examine association between sodium intake and blood pressure or risk for pre-high blood pressure and high blood pressure (pre-HBP/HPB).
RESULTS:
Study subjects consumed an average of 3387 mg/day of sodium, and 37% were overweight/obese. Each 1000 mg per day sodium intake was associated with an increased SD score of 0.097 (95% confidence interval [CI] 0.006–0.188, ~1.0 mm Hg) in systolic blood pressure (SBP) among all subjects and 0.141 (95% CI: −0.010 to 0.298, ~1.5 mm Hg) increase among overweight/obese subjects. Mean adjusted SBP increased progressively with sodium intake quartile, from 106.2 mm Hg (95% CI: 105.1–107.3) to 108.8 mm Hg (95% CI: 107.5–110.1) overall (P = .010) and from 109.0 mm Hg (95% CI: 107.2–110.8) to 112.8 mm Hg (95% CI: 110.7–114.9; P = .037) among those overweight/obese. Adjusted odds ratios comparing risk for pre-HBP/HPB among subjects in the highest versus lowest sodium intake quartile were 2.0 (95% CI: 0.95–4.1, P = .062) overall and 3.5 (95% CI: 1.3–9.2, P = .013) among those overweight/obese. Sodium intake and weight status appeared to have synergistic effects on risk for pre-HBP/HPB (relative excess risk for interaction = 0.29 (95% CI: 0.01–0.90, P < .05).
CONCLUSIONS:
Sodium intake is positively associated with SBP and risk for pre-HBP/HPB among US children and adolescents, and this association may be stronger among those who are overweight/obese.
Keywords: sodium intake, overweight, blood pressure, hypertension, cardiovascular risk factor
High blood pressure (HBP) in childhood not only predisposes people to hypertension in adulthood,1 it also increases their risk for the early development of cardiovascular disease and death.2–9 High sodium intake and overweight/obesity are recognized as risk factors for hypertension in adults as well as in children. Of >20 observational studies on sodium intake and blood pressure (BP) in children, most have shown a positive association.10–12 Results of a meta-analysis from 10 randomized controlled trials showed that a modest reduction in children’s sodium intake was associated with a small but significant reduction in BP.13 Although results of several trials among adults and adolescents have suggested that the effect of sodium reduction on BP might be modified by weight status or presence of metabolic syndrome,14–17 research examining the association between sodium intake and BP by weight status or their joint effect on risk for hypertension among children and adolescents is limited.
Examining risk factors for hypertension among children at the population level, especially among those with high sodium intake18,19 amid a growing epidemic of childhood obesity in the United States,20 is essential for developing and initiating effective interventions that could slow down or even prevent the development of hypertension and related complications later in life.21 In this study, we used NHANES data from 2003 through 2008 to examine the association between usual sodium intake and BP, sodium intake and risk for HBP by weight status, and the joint effect of sodium intake and weight status on risk for HBP among children and adolescents aged 8 to 18.
METHODS
Data Source
We analyzed data from the NHANES (2003–2008), which uses a stratified multistage probability design to obtain a nationally representative sample of the civilian, noninstitutionalized US population and collects data from survey participants via household interviews and physical examinations. Detailed information about NHANES procedures is available elsewhere.22 For our analyses, we used data collected from participants aged 8 to 18 years during 2003–2004, 2005–2006, and 2007–2008. Of 7199 potential study subjects, we excluded 72 who were pregnant, 432 whose data did not meet the minimum dietary recall data quality standards (http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/diet03_04.htm), 289 with missing BP data or height or weight measurements, and 171 who were under-weight (<5th percentile in BMI), leaving 6235 children for analyses.
Estimating Subjects’ Usual Sodium Intake
All subjects provided at least one 24-hour dietary recall at the mobile examination center, and 91% also provided a second recall via telephone interview 3 to 10 days later. NHANES estimated participants’ nutrient intake from foods by using the US Department of Agriculture Food and Nutrient Databases for Dietary Studies for each 2-year NHANES cycle.23
Dietary data from a single 24-hour recall may not represent a respondent’s usual dietary intake because of day-to-day variations in diet, and use of such data may bias estimates of the association between nutrient intake and health outcomes due to the measurement errors.24,25 To limit such possible bias, we used a 2-step method developed by the National Cancer Institute (NCI) to estimate participants’ usual sodium intake.26 Because sodium was consumed daily by nearly every participant, we used only the amount part of the model in the first step. The second step involves calculating the individual’s estimated usual intake with parameters from the first step.27 The NCI method requires that some of the participants have multiple days of nutrient values to estimate the within- and between-individual variations.26,27 The models for estimating usual intake included the following covariates: an indicator of first- versus second-day recall, day of the week recall (weekday vs weekends), race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and others), and age groups (8–12, 13–15, and ≥16 years).28 We used the similar approach to estimate the usual potassium and total energy intakes and estimated these usual intakes for male and female subjects separately.
BP Measurements
NHANES measured participants’ BP up to 3 times during their visits to the mobile examination center. All BP measurements were taken with a sphygmomanometer by certified examiners with a proper cuff size after children rested quietly in a sitting position for 5 minutes.29 The average of 3 (78%), 2 (11%), and 1 (11%) BP measurements per individual were used in the study. The guidelines recommend multiple BP measurements at different times to define persistent prehypertension and hypertension in children and adolescents.30 To differentiate the BP measurements in the current study (up to 3 measurements in a single mobile examination center visit) from the recommended definitions, we used the terms of pre-high BP (pre-HBP) and HBP with the same cutoff points that are used to define prehypertension and hypertension.30,31 We classified children’s (8–17 years) BP as normal, pre-HBP, or HBP on the basis of age-, gender-, and height-specific BP percentiles derived from the reference population for the 2000 Centers for Disease Control and Prevention growth charts.30 Normal BP is defined as systolic blood pressure (SBP) and diastolic blood pressure (DBP) below 90th percentile for their age, gender, and height; pre-HBP as an average SBP or DBP ≥90th but <95th percentile or with observed BP levels ≥120/80 mm Hg; and HBP as an SBP or DBP ≥95th percentile. For adolescents aged 18 years, pre-HBP is defined as either 120<SBP<140 mm Hg or 80 < DBP<90 mm Hg and HBP as either the SBP ≥140 mm Hg, the DBP ≥90 mm Hg, or was taking antihypertensive medication.32 To produce more stable estimates of the association, we combined subjects classified as having pre-HBP or HBP into 1 group, which we defined as having pre-HBP/HBP.
Baseline Covariates and Sensitivity Analysis
Our baseline covariates include age, gender, race-ethnicity, table salt use (never/rarely, sometimes, or often), and BMI calculated as kilograms of weight divided by meters of height squared. To account for variability by age and gender, BMI in children is compared with age- and gender-specific reference values from the 2000 Centers for Disease Control and Prevention growth charts to define the weight status.33 We defined overweight as a BMI-for-age/gender between the 85th and 95th percentiles and obesity as a BMI-for-age/gender ≥95th percentile.34 In our analyses, however, we collapsed the overweight and obese categories into “overweight/obese” to produce more stable estimates.
Apart from the weight status, several studies have suggested that the association between sodium intake and BP among children might be affected by their physical activity level and by family history of hypertension.12,14,35,36 However, NHANES 2003–2008 did not collect family hypertension data from children or physical activity data from children <12. In our sensitivity analyses, we assessed the effect of physical activity (inactive, active but at below recommended levels, and active at or above recommended levels) only among adolescents aged 12 to 18 years (Supplemental Tables 4 and 5). For sensitivity analyses of BP measurements, we restricted our analyses among participants with 3 BP measurements (Supplemental Tables 6 and 7).
Statistical Analysis
We calculated the weighted mean and SE of subjects’ estimated usual sodium and total calorie intakes by the categories described earlier and used the Satterthwaite adjusted F test to assess the differences in mean intakes. We calculated the SD score (SDS) of BP as observed minus expected BP divided by the SD30 and used linear regression to estimate the adjusted β-coefficients of sodium intake (per 1000 mg/day) with SDS of SBP and DBP by weight status (normal weight vs overweight/obese). We calculated the middle value of each quartile of usual sodium intake in total population and by weight status (ie, 12.5th, 37.5th, 62.5th, and 87.5th percentiles), used the linear regression models to estimate the adjusted mean SBP and DBP associated with each of these values, and presented these adjusted means as SBP or DBP level associated with the each quartile of usual sodium intake in population.37,38
We used logistic regression to estimate the adjusted odds ratio (OR) for the association between subjects’ sodium intake quartile and their risk for pre-HBP/HBP by comparing the risk among those in each of the top 3 quartiles with that among those in the lowest quartile (Q4, Q3, and Q2 vs Q1).37,38 In both the linear and logistic regression analyses, we estimated age, gender, race-ethnicity, and total energy adjusted β-coefficient or ORs as well as the estimates adjusted for, in addition, weight status, table salt use, and usual potassium intake.
Many studies have suggested that assessment of interaction on an additive scale is more meaningful than an assessment of interaction on a multiplicative scale (a product term in the regression models) especially from a public health perspective.39,40 We used the relative excess risk due to interaction (RERI) to examine the joint effect of sodium intake and weight status on risk for pre-HBP/HBP.40 The RERI was calculated by using the coefficients from the multivariable logistic regression as follows:
where β1 is the logistic regression coefficient of sodium intake per 1000 mg per day, β2 is the coefficient of the weight status, and β3 is the coefficient of the product term of sodium intake and weight status.41 RERI = 0 indicates exact additivity of 2 exposure variables and no interaction, and RERI >0 indicates the synergistic interaction on additive scale. We used the rescaling bootstrap method that takes into account the complex survey design by changing the sampling weights for each resample.42,43 We generated 1000 rescaled bootstrap weights and reported 2.5th and 97.5th percentile values as 95% CI of RERI. We used SUDAAN (version 9.2) and SAS (version 9.3) for all analyses.44 All tests were 2-sided, and P values <.05 were considered statistically significant.
RESULTS
US children and adolescents aged 8 to 18 years consumed, on average, 3387 mg per day of sodium, and average sodium intake increased with age. Consumption was higher among male than among female subjects, higher among those of normal weight than among those overweight/obese, and highest by race/ethnicity among non-Hispanic whites (Table 1). The prevalence of overweight/obesity in the study population was 37.1% (95% CI: 32.9%–39.3%), and the prevalence of pre-HBP and HBP was 14.9% (95% CI: 12.9%–17.0%).
TABLE 1.
Estimated Usual Intake of Sodium and Calories Among US Children and Adolescents Aged 8 to 18 Years, NHANES 2003–2008
| Characteristicsa | Sample n (%)b | Mean Usual Intake (SE)a | |
|---|---|---|---|
| Sodium (mg/d) | Calories | ||
| All | 6235 | 3387 (18.8) | 2162 (12.5) |
| Age | |||
| 8–12 y | 2508 (43.6) | 3260 (23.9) | 2077 (13.7) |
| 13–18 y | 3727 (56.4) | 3486 (26.2) | 2227 (17.0) |
| P value | <.001 | <.001 | |
| Gender | |||
| Male | 3125 (51.2) | 3801 (24.7) | 2418 (16.7) |
| Female | 3110 (48.8) | 2956 (15.4) | 1895 (9.2) |
| P value | <.001 | <.001 | |
| Race/ethnicity | |||
| Non-Hispanic white (1) | 1744 (62.8) | 3490 (25.5) | 2219 (16.2) |
| Non-Hispanic black (2) | 2007 (14.8) | 3218 (22.2) | 2047 (16.2) |
| Mexican American (3) | 1854 (12.3) | 3204 (22.8) | 2105 (18.1) |
| Other (4) | 630 (10.1) | 3227 (36.9) | 2046 (20.2) |
| P value (1 vs 2) | <0001 | <.001 | |
| P value (1 vs 3) | <.001 | <.001 | |
| P value (1 vs 4) | <.001 | <.001 | |
| Weight statusc | |||
| Normal | 3691 (62.9) | 3459 (20.5) | 2224 (13.2) |
| Overweight | 1133 (18.3) | 3214 (37.6) | 2049 (24.8) |
| Obese | 1411 (18.8) | 3319 (35.0) | 2060 (21.5) |
| P value for trend | .001 | <.001 | |
| Table-salt use | |||
| No/rarely | 1789 (27.8) | 3334 (35.1) | 2127 (23.6) |
| Sometimes | 3734 (61.8) | 3390 (23.6) | 2161 (14.8) |
| Often | 711 (10.4) | 3489 (60.2) | 2226 (27.2) |
| P value for trend | .033 | .004 | |
| BPd | |||
| Normal | 5307 (85.1) | 3358 (19.4) | 2148 (12.3) |
| Pre-HBP | 740 (11.5) | 3641 (55.1) | 2287 (34.6) |
| HBP | 188 (3.4) | 3278 (57.3) | 2080 (40.0) |
| P value for trend | .141 | .084 | |
For categories of the continuous variables in nature (eg, BMI and hypertension,), P values indicate differences across the categories. For categorical variables (eg, race/ethnicity), we presented pairwise P values. All tests were 2-tailed and based on the Satterthwaite adjusted F test.
Mean (SE) and percentage (%) presented by the estimated usual sodium and calorie intakes.
Overweight was defined as a BMI-for-age/gender between the >85th and <95th percentiles and obesity as BMI-for-age/gender ≥95th % percentile based on age- and gender-specific reference values from the 2000 Centers for Disease Control and Prevention growth charts.
For children aged 8–17 years: Subjects’ BP was classified as normal, pre-HBP, or HBP on the basis of age-, sex-, and height-specific blood pressure percentiles derived from the reference population for the 2000 CDC growth charts. For adolescents aged 18 years: subjects’ BP was classified using cut-offs for adults.
Overall, the adjusted SDS of SBP increased by 0.097 (95% CI 0.006–0.188, ~1.0 mm Hg) per 1000 mg per day sodium consumed (sodium intake ranged from 1334 to 8177 mg/day), whereas SDS of DBP was not significantly associated with sodium intake (Table 2). Among normal-weight subjects, the adjusted SDS of SBP increased by 0.022 (95% CI: −0.096 to 0.140, ~0.2 mm Hg) per 1000 mg per day of sodium, and it increased by 0.141 (95% CI: −0.010 to 0.298, ~1.5 mm Hg) among overweight/obese subjects. The mean adjusted SBP of all study subjects ranged from 106.2 mm Hg (95% CI: 105.1–107.3) among those in the lowest quartile of sodium intake to 108.8 mm Hg (95% CI: 107.5–110.1; P = .010) among those in the highest with a mean difference 2.6 mm Hg (95% CI: 1.0–4.2). Among participants who were overweight/obese, it ranged from 109.0 mm Hg (95% CI: 107.2–110.8) to 112.8 mm Hg (95% CI: 110.7–114.9; P = .036) with a mean difference 3.8 mm Hg (95% CI: 1.1–6.5), and among those of normal weight, it increased from 104.8 mm Hg (95% CI: 103.4–106.2) to 106.6 mm Hg (95% CI: 104.8–108.3; P = .186) with a mean difference 1.7 mm Hg (95% CI: −0.5 to 3.9; Fig 1).
TABLE 2.
Adjusted Associations Between Each 1000-mg/d Increase in Sodium Intake and SDS of BP Among US Children and Adolescents, Based on 2 Models, Overall and by Weight Status, NHANES 2003–2008
| Characteristics | SDS of SBP | SDS of DBP | ||
|---|---|---|---|---|
| β-Coefficient (95% CI) | P Value | β-Coefficient (95% CI) | P Value | |
| All | ||||
| Model 1 | 0.121 (0.034 to 0.207) | .008 | −0.072 (−0.182 to 0.0374) | .190 |
| Model 2 | 0.097 (0.006 to 0.188) | .037 | −0.066 (−0.175 to 0.043) | .227 |
| Weight status | ||||
| Normal wt | ||||
| Model 1 | 0.043 (−0.069 to 0.155) | .445 | −0.125 (−0.263 to 0.013) | .074 |
| Model 2 | 0.022 (−0.096 to 0.140) | .710 | −0.120 (−0.258 to 0.019) | .090 |
| Overweight/obese | ||||
| Model 1 | 0.197 (0.036 to 0.357) | .017 | 0.015 (−0.178 to 0.209) | .875 |
| Model 2 | 0.141 (−0.010 to 0.298) | .075 | 0.008 (−0.185 to 0.201) | .936 |
Model 1 adjusted for age, gender, race/ethnicity, and total energy intake. Model 2 adjusted for all factors in Model 1 plus weight status (normal, overweight, and obese except for the weight-stratified analyses for which we included BMI as a continuous variable), table-salt use, and estimated usual intake of potassium. P values for interactions between daily sodium intake and weight classification among normal-weight children were 0.922 for SBP and 0.204 for DBP; all adjusted P values derived from 2-tailed Satterthwaite adjusted F tests.
FIGURE 1.
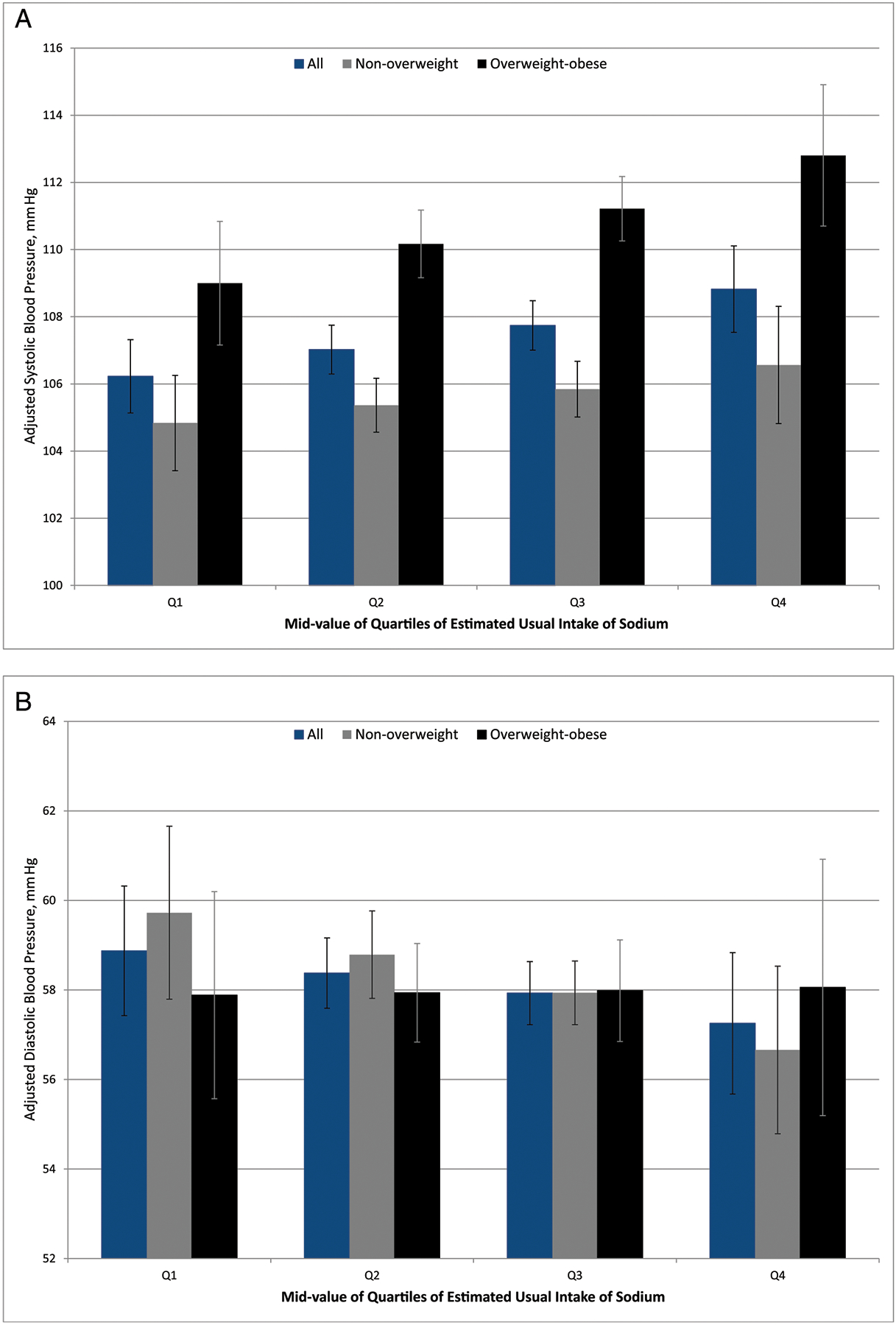
Adjusted mean (95% CI) systolic (A) and diastolic (B) blood pressure values among US children and adolescents aged 8 to18 years, by sodium intake quartile and weight status, NHANES 2003–2008.
The adjusted risk of HBP among all subjects comparing the highest to the lowest quartile of sodium intake was 1.98 (95% CI: 0.95–4.11; P = .062). However, among overweight/obese subjects, it was 3.51 (95% CI: 1.34–9.20; P = .013). For every 1000 mg per day increase in sodium intake, the risk for pre-HBP/HBP increased by 74% among overweight/obese subjects but by only 6% among normal weight subjects. The estimated RERI = 0.29 (95% CI: 0.01–0.90), suggesting synergistic interaction of sodium intake and overweight/obese on risk for pre-HBP/HBP (Table 3).
TABLE 3.
Adjusted ORs for Pre-High Blood Pressure/High Blood Pressure (Pre-HBP/HPB)a Among US Children and Adolescents Aged 8 to 18 Years, by Quartile of Usual Daily Sodium Intake, NHANES 2003–2008
| Sodium Intake Quartile, OR (95% CI) | P Value for Trenda | Overall Increase in Pre-HBP/HPB Risk per 1000 mg/d Increase in Sodium Intake, OR (95% CI)b | RERI (5th–95th percentile) | ||||
|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||||
| Total | |||||||
| Usual daily sodium intake (range: 1334–8177) | 2316 | 3014 | 3642 | 4589 | |||
| Model 1 | Ref | 1.31 (1.03 to 1.67) | 1.68 (1.07 to 2.64) | 2.43 (1.11 to 5.28) | .023 | 1.48 (1.06 to 2.06) | 0.28 (−0.01 to 0.83) |
| Model 2 | Ref | 1.23 (0.98 to 1.54) | 1.49 (0.97 to 2.28) | 1.98 (0.95 to 4.11) | .062 | 1.35 (0.98 to 1.86) | 0.29 (0.01 to 0.90) |
| Weight status | |||||||
| Normal weight | |||||||
| Usual daily sodium intake (range: 1354–8177) | 2315 | 3010 | 3641 | 4587 | |||
| Model 1 | Ref | 1.06 (0.82 to 1.39) | 1.13 (0.68 to 1.87) | 1.23 (0.51 to 2.93) | .635 | 1.09 (0.75 to 1.60) | — |
| Model 2 | Ref | 1.04 (0.79 to 1.38) | 1.08 (0.63 to 1.85) | 1.15 (0.46 to 2.86) | .775 | 1.06 (0.71 to 1.57) | — |
| Overweight/obese | |||||||
| Usual daily sodium intake (range: 1334–6862) | 2319 | 3020 | 3649 | 4601 | |||
| Model 1 | Ref | 1.64 (1.17 to 2.31) | 2.57 (1.35 to 4.89) | 5.05 (1.68 to 15.22) | .005 | 2.03 (1.26 to 3.26) | — |
| Model 2 | Ref | 1.47 (1.09 to 1.98) | 2.08 (1.18 to 3.65) | 3.51 (1.34 to 9.20) | .013 | 1.74 (1.13 to 2.68) | — |
Model 1 adjusted for age, gender, race/ethnicity, and total energy intake. Model 2 adjusted for age, gender, race/ethnicity, weight status (normal, overweight, and obese except for the weight-stratified analyses for which we included BMI as a continuous variable), table-salt use, and estimated usual intakes of potassium.
P value for trend across percentiles of estimated usual intake of sodium based on Satterthwaite adjusted F test; all tests are 2-tailed.
ORs are for 1000 mg/d of estimated usual intake of sodium.
DISCUSSION
In this nationally representative sample of US children and adolescents, sodium intake was associated with SBP and risk for pre-HBP/HBP, consistent with findings of other epidemiologic studies.11–13,45 However, by examining the joint effect of usual sodium intake and weight status on risk for pre-HBP/HBP, our results suggested that high sodium intake may have a greater effect on risk for pre-HBP/HBP for overweight/obese children than for normal-weight children. The patterns of association remained consistent when further adjusting physical activity among children aged 12 to 18 years (Supplemental Tables 4 and 5). In a 1989 study, Rocchini et al found that the BP of obese adolescents was particularly sensitive to changes in sodium intake and that this sensitivity may be related to the effects of hyperinsulinemia and hyperaldosteronism and to relatively high activity of the sympathetic nervous system among obese adolescents.14 Other studies among adults also demonstrated that the association between sodium intake and BP tended to be more pronounced among those classified as overweight or in the presence of metabolic syndrome.15–17,36 The significant synergistic interaction between sodium intake and weight status on risk for pre-HBP/HBP observed in our study may have important clinical and public health implications in that reducing sodium intake or weight reduction among children and adolescents in the United States may lead to a greater than expected reduction in HBP. Although we observed a non-significant association between sodium intake and BP or risk for pre-HBP/HBP among normal-weight children, it should not be interpreted as indicating a null effect of high sodium intake on BP. Many controlled trials and observational studies provided strong evidence that high sodium intake and overweight/obesity are risk factors for hypertension in children.10–13,46,47
On average, US children and adolescents consumed ~3400 mg/day sodium, which is nearly the same average consumption as that for adults aged ≥20 years48; 37% of these children were overweight or obese, and ~15% had pre-HBP or HBP. Such a high rate of pre-HBP or HBP is worrisome given that HBP among children and adolescents often remains undiagnosed, in part because the diagnosis requires that their BP be taken with an age-appropriate cuff size and their BP status assessed by gender, age, and height.49–51 HBP, especially untreated, may accelerate atherosclerosis and result in organ damage, primarily left ventricular hypertrophy.49 However, HBP can be managed through healthy lifestyle practices such as the Dietary Approaches to Stop Hypertension diet, as well as weight reduction, regular exercise, and smoking cessation.49 According to the 2010 Dietary Guidelines for Americans, children aged ≥2 should consume ≤2300 mg/day sodium, and some groups, including African Americans and children with hypertension, diabetes, or chronic kidney disease, should consume ≤1500 mg.52 However, reducing the sodium intake of US children remains difficult, in part because ≥75% of sodium in the average American diet comes from packaged, processed, or restaurant food.53 Nevertheless, people can control their sodium intake and manage their weight by controlling portion sizes, not skipping meals, minimizing consumption of processed foods, paying attention to energy and sodium data on food labels, and not adding salt to foods.49 Other research results have shown that school- and community-based interventions can contribute to healthier dietary choices and increased levels of physical activity among school-aged children.54,55
Study Strengths and Limitations
Strengths of our study included our analysis of dietary sodium intake data based on the multiple days of 24-hour recalls. Nutrient intake data based on a single 24-hour dietary recall are not reliable indicators of subjects’ usual nutrient intake because of large day-to-day variations in intake, which may bias the association between nutrient intake and disease.25,37,56 We used a measurement error model developed by NCI to estimate subjects’ usual sodium intake for associations between sodium intake and both BP and risk for pre-HBP/HBP.26,27,38 Several studies have indicated that the estimated usual intakes provided significant improvements in assessments of nutrient-disease associations.37,38
Our study also had some notable limitations. First, our estimates of subjects’ “usual sodium intake” were based on self-reported dietary recalls rather than on the 24-hr urine collection, which is considered to be the most reliable method. Although studies suggested that 24-hr dietary recalls may underestimate the usual sodium intake,57 sodium intake from the repeated dietary recalls correlated significantly with the 24-hr urinary excretion and provided a valid method for previous association studies.57,58 Approximately 9% of subjects had no second-day dietary recalls in our study; however, the patterns of association remained unchanged by excluding those subjects (results not shown). Second, the 24-hr dietary recall underestimated total energy intake by ~11% in NHANES and likely underestimated sodium intake as well because the total energy and sodium intakes are highly correlated. Non-differential recall bias in total energy and sodium intakes by weight status (Table 1) may underestimate the effect of sodium intake on BP and risk for pre-HBP/HBP.59 To assess the extent to which any underestimate of sodium intake may have affected our results, we calculated the total energy-adjusted sodium intake by the residual method60 and found the patterns of association to be largely unchanged from those in our primary analyses. The adjusted β-coefficients of SDS for SBP per 1000 mg per day sodium intake were 0.078 (95% CI: −0.006 to 0.163), 0.028 (95% CI: −0.091 to 0.147), and 0.160 (95% CI: 0.006 to 0.315) for all, normal-weight and overweight/obese children, respectively. The corresponding adjusted ORs were 1.36 (95% CI: 1.00–1.89), 1.02 (95% CI: 0.67–1.55), and 1.72 (95% CI: 1.13–2.63), respectively. Third, because of underreporting of total energy and sodium intakes, the effect of weight status, which reflects several lifestyle factors such as physical activity and healthy diets, on BP or risk for pre-HBP/HBP may be overestimated. In the sensitivity analyses for children aged 12 to 18 years, we also adjusted for physical activity, and the patterns of association remain largely unchanged (Supplemental Tables 4 and 5). Fourth, we restricted our analyses to the 78% of children and adolescents with 3 BP measurements, and the patterns of association remained largely unchanged (Supplemental Tables 6 and 7). Finally, because our study data came from a cross-sectional survey, the associations we found should be interpreted with caution. A large randomized controlled trial would be needed to confirm our findings.
CONCLUSIONS
The average sodium consumption among US children and adolescents aged 8 to 18 years is as high as that of adults. The higher sodium intake is associated with increased SBP and risk for pre-HBP/HBP, and these associations may be stronger among those who are overweight or obese than among those who are not. Evidence-based interventions that help participants reduce their sodium intake, increase their physical activity, and attain or maintain a healthy weight may help reduce the greater than expected prevalence of HBP and other cardiovascular disease risk factors among children and adolescents.
Supplementary Material
WHAT’S KNOWN ON THIS SUBJECT:
High blood pressure in childhood predisposes people to hypertension in adulthood and is associated with early development of cardiovascular disease and risk for premature death. High sodium intake and overweight/obesity are recognized as risk factors for hypertension in children.
WHAT THIS STUDY ADDS:
These results show that usual sodium intake was positively associated with systolic blood pressure and risk for pre-high blood pressure and high blood pressure among US children. The data indicate a synergistic interaction between sodium intake and weight status on risk for high blood pressure.
ABBREVIATIONS
- BP
blood pressure
- CI
confidence interval
- DBP
diastolic blood pressure
- HBP
high blood pressure
- NCI
National Cancer Institute
- OR
odds ratio
- RERI
relative excess risk due to interaction
- SBP
systolic blood pressure
- SDS
standard deviation score
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171–3180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berenson GS. Childhood risk factors predict adult risk associated with subclinical cardiovascular disease. The Bogalusa Heart Study. Am J Cardiol. 2002;90(10C):3L–7L [DOI] [PubMed] [Google Scholar]
- 3.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juonala M, Järvisalo MJ, Mäki-Torkko N, Kähönen M, Viikari JS, Raitakari OT. Risk factors identified in childhood and decreased carotid artery elasticity in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2005;112(10):1486–1493 [DOI] [PubMed] [Google Scholar]
- 5.Lauer RM, Clarke WR. Childhood risk factors for high adult blood pressure: the Muscatine Study. Pediatrics. 1989;84(4): 633–641 [PubMed] [Google Scholar]
- 6.Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290(17):2271–2276 [DOI] [PubMed] [Google Scholar]
- 7.Raitakari OT, Juonala M, Kähönen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290(17): 2277–2283 [DOI] [PubMed] [Google Scholar]
- 8.Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119(2):237–246 [DOI] [PubMed] [Google Scholar]
- 9.Sundström J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010; 52(5):363–382 [DOI] [PubMed] [Google Scholar]
- 11.He FJ, Marrero NM, Macgregor GA. Salt and blood pressure in children and adolescents. J Hum Hypertens. 2008;22(1):4–11 [DOI] [PubMed] [Google Scholar]
- 12.Sugiyama T, Xie D, Graham-Maar RC, Inoue K, Kobayashi Y, Stettler N. Dietary and lifestyle factors associated with blood pressure among U.S. adolescents. J Adolesc Health. 2007;40(2):166–172 [DOI] [PubMed] [Google Scholar]
- 13.He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48(5):861–869 [DOI] [PubMed] [Google Scholar]
- 14.Rocchini AP, Key J, Bondie D, et al. The effect of weight loss on the sensitivity of blood pressure to sodium in obese adolescents. N Engl J Med. 1989;321(9):580–585 [DOI] [PubMed] [Google Scholar]
- 15.The Trials of Hypertension Prevention Collaborative Research Group. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. Arch Intern Med. 1997;157(6):657–667 [PubMed] [Google Scholar]
- 16.The Trials of Hypertension Prevention Collaborative Research Group. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267(9): 1213–1220 [DOI] [PubMed] [Google Scholar]
- 17.Chen J, Gu D, Huang J, et al. ; GenSalt Collaborative Research Group. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: a dietary intervention study. Lancet. 2009; 373(9666):829–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ervin RB, Wang CY, Wright JD, Kennedy-Stephenson J. Dietary intake of selected minerals for the United States population: 1999–2000. Adv Data. 2004; (341):1–5 [PubMed] [Google Scholar]
- 19.Institute of Medicine, Committee on Strategies to Reduce Sodium Intake. Strategies to reduce sodium intake in the United States. Washington, DC: National Academies Press; 2010. Available at: www.iom.edu/reports/2010/strategies-to-reduce-sodium-intake-in-the-united-states.aspx. Accessed December 5, 2011 [Google Scholar]
- 20.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Juonala M, Viikari JS, Kähönen M, et al. Life-time risk factors and progression of carotid atherosclerosis in young adults: the Cardiovascular Risk in Young Finns study. Eur Heart J. 2010;31(14):1745–1751 [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. National Health and Nutrition Examination Survey. Questionnaires, datasets, and related documentation. Available at: www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed January 2012
- 23.US Department of Agriculture. Food and nutrient database for dietary studies. Beltsville, MD: Agricultural Research Service, Food Surveys Research Group. Available at: www.ars.usda.gov/Services/docs.htm?docid=12089. Accessed October 2011 [Google Scholar]
- 24.Carriquiry AL. Estimation of usual intake distributions of nutrients and foods. J Nutr. 2003;133(2):601S–608S [DOI] [PubMed] [Google Scholar]
- 25.Willett W Nutritional Epidemiology. New York, NY: Oxford University Press; 1998 [Google Scholar]
- 26.Tooze JA, Midthune D, Dodd KW, et al. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106(10):1575–1587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Cancer Institute. Usual dietary intakes: the NCI method. Available at: http://riskfactor.cancer.gov/diet/usualintakes/method.html. Accessed May 2010
- 28.Institute of Medicine (US), Panel on Dietary Reference Intakes for Electrolytes and Water. DRI, Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: National Academies Press; 2005 [Google Scholar]
- 29.National Center for Health Statistics. National Health and Nutrition Examination Survey. Blood pressure section of the physician examination, NHANES 2003–2008. Available at: www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed August 2011
- 30.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(suppl 2, 4th report):555–576 [PubMed] [Google Scholar]
- 31.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116(13):1488–1496 [DOI] [PubMed] [Google Scholar]
- 32.Chobanian AV, Bakris GL, Black HR, et al. ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572 [DOI] [PubMed] [Google Scholar]
- 33.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002; (246):1–190 [PubMed] [Google Scholar]
- 34.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010;(25):1–5 [PubMed] [Google Scholar]
- 35.Falkner B, Michel S. Blood pressure response to sodium in children and adolescents. Am J Clin Nutr. 1997;65(suppl 2): 618S–621S [DOI] [PubMed] [Google Scholar]
- 36.Stabouli S, Papakatsika S, Kotsis V. The role of obesity, salt and exercise on blood pressure in children and adolescents. Expert Rev Cardiovasc Ther. 2011;9(6):753–761 [DOI] [PubMed] [Google Scholar]
- 37.Kipnis V, Midthune D, Buckman DW, et al. Modeling data with excess zeros and measurement error: application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics. 2009; 65(4):1003–1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tooze JA, Kipnis V, Buckman DW, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010; 29(27):2857–2868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blot WJ, Day NE. Synergism and interaction: are they equivalent? Am J Epidemiol. 1979; 110(1):99–100 [DOI] [PubMed] [Google Scholar]
- 40.Rothman KJ, Greenland S. Modern Epidemiology. Philadelphia, PA: Lippincott-Raven; 1998 [Google Scholar]
- 41.Knol MJ, van der Tweel I, Grobbee DE, Numans ME, Geerlings MI. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int J Epidemiol. 2007;36(5): 1111–1118 [DOI] [PubMed] [Google Scholar]
- 42.Cheng NF, Han PZ, Gansky SA. Methods and software for estimating health disparities: the case of children’s oral health. Am J Epidemiol. 2008;168(8):906–914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rao JNK, Wu CFJ, Yue K. Some recent work on resampling methods for complex surveys. Surv Methodol. 1992;18(2):209–217 [Google Scholar]
- 44.Shah VBBB, Bieler GS. SUDAAN User’s Manual, Release 9. Research Triangle Park, NC: Research Triangle Institute; 2005 [Google Scholar]
- 45.Cooper R, Soltero I, Liu K, Berkson D, Levinson S, Stamler J. The association between urinary sodium excretion and blood pressure in children. Circulation. 1980;62(1): 97–104 [DOI] [PubMed] [Google Scholar]
- 46.Sorof J, Daniels S. Obesity hypertension in children: a problem of epidemic proportions. Hypertension. 2002;40(4):441–447 [DOI] [PubMed] [Google Scholar]
- 47.Torrance B, McGuire KA, Lewanczuk R, McGavock J. Overweight, physical activity and high blood pressure in children: a review of the literature. Vasc Health Risk Manag. 2007;3(1):139–149 [PMC free article] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. Sodium intake among adults—United States, 2005–2006. MMWR Morb Mortal Wkly Rep. 2010;59(24):746–749 [PubMed] [Google Scholar]
- 49.McCrindle BW. Assessment and management of hypertension in children and adolescents. Nat Rev Cardiol. 2010;7(3): 155–163 [DOI] [PubMed] [Google Scholar]
- 50.Brady TM, Solomon BS, Neu AM, Siberry GK, Parekh RS. Patient-, provider-, and clinic-level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125(6). Available at: www.pediatrics.org/cgi/content/full/125/6/e1286 [DOI] [PubMed] [Google Scholar]
- 51.Hansen ML, Gunn PW, Kaelber DC. Under-diagnosis of hypertension in children and adolescents. JAMA. 2007;298(8):874–879 [DOI] [PubMed] [Google Scholar]
- 52.Dalaker J, Proctor BD. Poverty in the United States: 1999. Current Population Reports Series P60, No. 210. Washington, DC: US Census Bureau; 2000. Available at: www.census.gov/hhes/www/poverty/publications/p60-210.pdf. Accessed June 2011 [Google Scholar]
- 53.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10(4):383–393 [DOI] [PubMed] [Google Scholar]
- 54.Pate RR, Davis MG, Robinson TN, Stone EJ, McKenzie TL, Young JC; American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Physical Activity Committee); Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing. Promoting physical activity in children and youth: a leadership role for schools: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Physical Activity Committee) in collaboration with the Councils on Cardiovascular Disease in the Young and Cardiovascular Nursing. Circulation. 2006;114 (11):1214–1224 [DOI] [PubMed] [Google Scholar]
- 55.Kumanyika SK, Obarzanek E, Stettler N, et al. ; American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation. 2008;118(4): 428–464 [DOI] [PubMed] [Google Scholar]
- 56.Dodd KW, Guenther PM, Freedman LS, et al. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc. 2006;106(10): 1640–1650 [DOI] [PubMed] [Google Scholar]
- 57.Espeland MA, Kumanyika S, Wilson AC, et al. ; TONE Cooperative Research Group. Statistical issues in analyzing 24-hour dietary recall and 24-hour urine collection data for sodium and potassium intakes. Am J Epidemiol. 2001;153(10):996–1006 [DOI] [PubMed] [Google Scholar]
- 58.Reinivuo H, Valsta LM, Laatikainen T, Tuomilehto J, Pietinen P. Sodium in the Finnish diet: II trends in dietary sodium intake and comparison between intake and 24-h excretion of sodium. Eur J Clin Nutr. 2006;60(10):1160–1167 [DOI] [PubMed] [Google Scholar]
- 59.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–332 [DOI] [PubMed] [Google Scholar]
- 60.Poslusna K, Ruprich J, de Vries JH, Jakubikova M, van’t Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 hour recalls, control and adjustment methods in practice. Br J Nutr. 2009;101(suppl 2):S73–S85 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


