Summary
Objective
This study was undertaken to investigate the COVID‐19 vaccine uptake rate and possible postvaccination effects in adults with epilepsy.
Methods
We invited adults with epilepsy attending three centers in China from July 24 to August 31, 2021 to participate in this study. We also asked age‐ and sex‐matched controls among people attending for other chronic neuropsychiatric conditions and healthy controls accompanying people with illness attending the hospitals to participate. We excluded people who, under the national guidelines, had evident contradictions to vaccination. Participants were interviewed face‐to‐face using questionnaires. Vaccine uptake and postvaccine adverse events among the people with epilepsy were compared with those with neuropsychiatric conditions and controls. We also compared the willingness and reasons for hesitancy among unvaccinated participants.
Results
We enrolled 981 people, of whom 491 had epilepsy, 217 had other neuropsychiatric conditions, and 273 were controls. Forty‐two percent of those with epilepsy had had the first dose of a vaccine, compared with 93% of controls and 84% of the people with neuropsychiatric conditions (p < .0001). The majority (93.8%) of those immunized had inactivated vaccines. Among the unvaccinated people with epilepsy, 59.6% were willing to have the vaccine. Their main reasons for hesitation were potential adverse effects (53.3%) and concerns about losing seizure control (47.0%). The incidence of adverse events in the epilepsy group was similar to controls. Nineteen people with epilepsy reported an increase in seizure frequency. No episode of status epilepticus or prolonged seizures was reported. Two controls had their first‐ever seizure, which was unlikely related to the vaccine.
Significance
The vaccine uptake rate in people with epilepsy was lower than in their same‐age controls. The postvaccination effect was no higher than in controls. We found no evidence suggesting worsening seizures after vaccination. Measurement and education focused on increasing the vaccination rate in epilepsy are warranted.
Keywords: real‐world investigation, SARS‐CoV‐2, seizure, vaccine
Key Points.
Adults with epilepsy had a much lower vaccine uptake than their age‐matched controls
Vaccines were well tolerated in adults with epilepsy, and postvaccination effects were no worse than in controls
Postvaccination increase in seizures was rare
Evidence‐based recommendations and detailed individual education are required to facilitate the best vaccine decision‐making
1. INTRODUCTION
With the ongoing COVID‐19 pandemic, the only hope for reestablishing prepandemic routines is deploying effective vaccines with high take‐up rates worldwide. In December 2020, the US Food and Drug Administration authorized the emergency use of two mRNA vaccines, 1 , 2 starting the first‐ever vaccination program in adults. Since then, the World Health Organization has evaluated six vaccines meeting the criteria for safety and efficacy. 3 These are the mRNA vaccines from Moderna and Pfizer/BioNTech, the viral vector vaccines from Johnson & Johnson and Oxford/AstraZeneca, and the inactivated vaccines from Sinopharm and Sinovac.
The safety and efficacy of the COVID‐19 vaccines have raised concerns among people with epilepsy. In guidelines for other vaccines 4 such as diphtheria–tetanus‐pertussis and measles–mumps–rubella, epilepsy is not a contraindication. Specific evidence about the COVID‐19 vaccines in epilepsy is, however, still lacking. Reports from Germany 5 and Kuwait 6 based on relatively small cohorts suggest good tolerance of COVID‐19 vaccines. Based on the current evidence, the International League Against Epilepsy (ILAE) stated that no available evidence suggested that having epilepsy was associated with a higher risk of side effects from a COVID‐19 vaccine. Conversely, in China, the early national guidelines listed severe neurological disorders, including uncontrolled epilepsy, as contraindications. 7
We assessed whether there was a difference in the vaccination rate and postvaccination adverse effects between people with epilepsy and controls or people with other neuropsychiatric conditions. We also explored seizure‐related changes after vaccination in people with epilepsy.
2. MATERIALS AND METHODS
The ethics committee of West China Hospital, Sichuan University (2020[100]) approved this cross‐sectional multicenter study. All participants provided written consent.
The study was conducted in three tertiary hospitals (West China Hospital [Sichuan University], Henan Provincial People's Hospital, and Chongqing University Three Gorges Hospital) from July 24 to August 31, 2021. We invited people 18 years or older previously diagnosed with epilepsy attending neurological clinics to participate. We also invited other visitors to the hospital to participate; they were divided into two groups: people with other neuropsychiatric conditions and healthy controls (recruited among healthy visitors). We excluded people if any conditions listed as contraindications in the national vaccination guidelines, including pregnancy, allergy to vaccine products or severe allergy history, severe neurological disorders, and febrile illness, were present.
We gathered data through face‐to‐face interviews. We designed a questionnaire (Supplementary Material) to acquire demographic data, diagnosis, medication, history of febrile convulsions, and vaccine‐related information such as contraindications and willingness to be vaccinated. We asked about vaccine type and related adverse effects for those who had had a vaccine. We used a different questionnaire for people with epilepsy to include information about epilepsy, seizure frequency data, and seizure‐related changes after vaccination. Seizure frequency was measured in two ways. The first was a grading variable, with the options of 1 year seizure‐free, at least once per year, once every 6 months, once every 3 months, once every month, once every week, and once every day. Participants were asked to choose the frequency ranking that best fit. The second was the seizure‐free interval between vaccination and the previous seizure. Seizure frequency change was recorded from the first injection to 1 week afterward. According to national guidelines, complete vaccination was defined as having had full immunization according to the schedule required by the corresponding vaccine. The subunit vaccine requires three doses, the inactivated platforms require two injections, and the viral vector vaccine requires only one injection. Postvaccine fever was defined as a temperature > 38.5°C within the 7 days after the vaccination. Drug‐resistant epilepsy was defined as people not seizure‐free in the previous 12 months despite having had treatment trials of two or more antiseizure medications (ASMs). 8
Analysis of variance test and chi‐squared test were used based on the variables. We used IBM SPSS Statistics (v25.0, 64‐digital) for the analysis. Results were considered statistically significant at a p‐value of <.05.
3. RESULTS
We enrolled 981 individuals, including 491 people with epilepsy, 273 healthy controls, and 217 people with other neuropsychiatric conditions. None of the participants had a COVID‐19 infection by the study endpoint. None in the epilepsy group had an epileptic encephalopathy. The cumulative first dose rate among the three groups from December 2020 to study end is shown in Figure 1.
FIGURE 1.
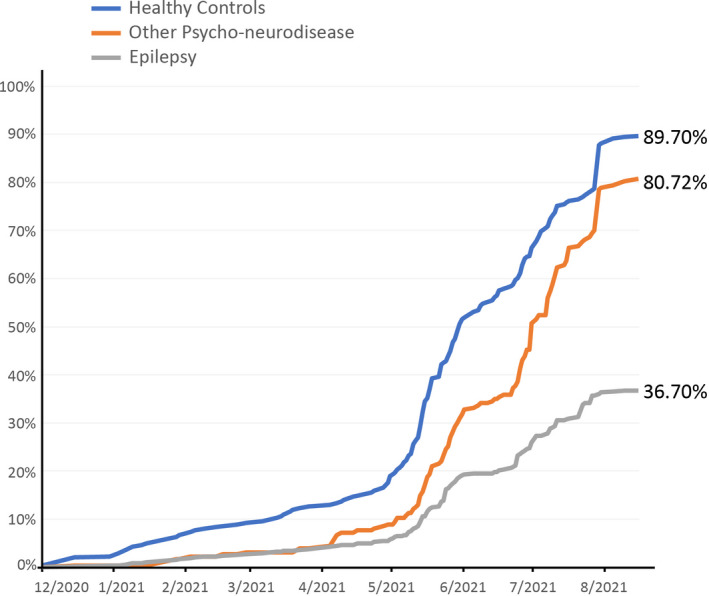
The COVID‐19 vaccine program started in December 2020. The first injection rate among people with epilepsy (in gray) is lower than in the other two control groups throughout the whole period
Table 1 shows the demographics, febrile seizure history, vaccination rate, and willingness to be inoculated in the unvaccinated population. In the unvaccinated population, vaccination willingness was similar between those with epilepsy and those with neuropsychiatric conditions, but controls reported a higher willingness rate. The main reasons for vaccine hesitancy in people with epilepsy and other neuropsychiatric disorders are provided in Table 2. Despite fewer concerns about disease‐vaccine interaction in those who were unvaccinated in the healthy group (n = 20), their main reasons were concerns of potential adverse events (n = 6) and scheduling conflicts at the time of the vaccine appointment (n = 11).
TABLE 1.
Demographics and vaccination details among the three groups.
| Characteristic | Healthy, n = 273 | Neuropsychiatric conditions, n = 217 | Epilepsy, n = 491 | p |
|---|---|---|---|---|
| Gender, n male (%) | 128 (46.9) | 105 (48.4) | 243 (49.5) | .78 |
| Ethnicity, n Han (%) | 255 (93.4) | 205 (94.5) | 466 (94.9) | .90 |
| Age, years, mean ± SD | 31.12 ± 8.12 | 33.2 ± 12.37 | 30.4 ± 10.90 | .78 |
| History of febrile convulsions, n (%) | 7 (2.56%) | 6 (2.76%) | 89 (18.13%) | <.0001 |
| 1st injection, n (%) | 253 (92.7%) | 183 (84.3%) | 204 (41.6%) | <.0001 |
| 2nd injection, N2/N1 (%) a | 196 (77.5%) | 129 (70.5%) | 139 (68.1%) | .07 |
| Completed vaccine course, n (%) | 196 (71.8%) | 131 (60.4%) | 155 (31.6%) | <.0001 |
| Vaccine platforms, N1/N2 b | ||||
| Inactivated vaccine, 2 doses required | 236 (93.3) | 177 (96.7) | 187 (92.2) | .31 |
| Subunit vaccine, 3 doses required | 15 (5.9) | 4 (2.2) | 14 (6.9) | |
| Viral‐vector vaccine, 1 dose required | 2 (.8) | 2 (1.1) | 2 (.9) | |
| Willing to be vaccinated, N4/N5 c | 70.00 | 58.82 | 59.58 | <.0001 |
N1 is the number of participants who had the first vaccine. N2 is the number who had the second vaccine, excluding those who had viral vector vaccine, which requires only one injection.
N1 is the number of participants injected with the indicated vaccine. N2 is the number of participants injected with the first vaccine. One participant from the epilepsy group received an mRNA vaccine.
N1 is the number of uninjected participants who would be willing to have any kind of vaccine. N2 is the number of uninjected participants.
TABLE 2.
Willingness for vaccination among unvaccinated participants with epilepsy or neuropsychiatric conditions
| Neuropsychiatric conditions, n = 34 | People with epilepsy, n = 287 | p | |
|---|---|---|---|
| Willingness, n (%) | 20 (58.8%) | 171 (59.6%) | .93 |
| Reason for hesitation, n (%) | |||
| Worried about the potential adverse effects | 8 (23.5%) | 153 (53.3%) | <.0001 |
| Unsatisfied with seizure/disease control | 17 (50.0%) | 135 (47.0%) | .63 |
| Worried about the interaction between current medication and the vaccine | 5 (14.7%) | 16 (5.6%) | .04 |
| Other comorbidity | 2 (5.9%) | 42 (14.6%) | .18 |
| Local administration suggested delaying the injection | 1 (2.9%) | 12 (4.2%) | .75 |
| Others | 8 (23.5%) | 15 (5.2%) | <.0001 |
For people with epilepsy, the clinical features of those vaccinated and those not vaccinated are shown in Table 3.
TABLE 3.
Clinical characteristics in people with epilepsy
| Characteristic | Vaccinated, n = 204 a | Unvaccinated, n = 286 | p |
|---|---|---|---|
| Age, years, mean ± SD | 30.9 ± 11.5 | 29.9 ± 10.1 | .93 |
| Course of disease, months, mean ± SD | 96.6 ± 99.8 | 109.3 ± 97.0 | <.0001 |
| Current ASMs, n, mean ± SD | 1.46 ± .80 | 1.83 ± .89 | .63 |
| Drug‐resistant epilepsy, n (%) b | 58 (28.0%) | 146 (50.5%) | .04 |
| Seizure classification, n (%) | |||
| Focal onset | 107 (52.5%) | 138 (48.1%) | .18 |
| Generalized onset | 51 (25.0%) | 73 (25.4%) | .75 |
| Unknown onset | 35 (17.2%) | 57 (19.9%) | <.0001 |
| Unclassified | 11 (5.4%) | 19 (6.6%) | .93 |
| Seizure frequency ranking, n (%) | |||
| Over 1 year seizure‐free | 80 (39.2%) | 65 (22.7%) | <.0001 |
| Once per year | 42 (20.6%) | 35 (12.2%) | .01 |
| Once every 6 months | 17 (8.3%) | 30 (10.5%) | .43 |
| Once every 3 months | 23 (11.3%) | 38 (13.2%) | .52 |
| Once every month | 27 (13.2%) | 70 (24.4%) | .02 |
| Once every week | 12 (5.9%) | 41 (14.3%) | .003 |
| Once every day | 3 (1.5%) | 8 (2.8%) | .331 |
Abbreviation: ASM, antiseizure medication.
All participants had the first injection.
Excluding newly diagnosed people with epilepsy (course of the disease < 3 months).
Adverse events reported by people with epilepsy and controls are provided in Table 4. Fever was only reported by two subjects after the first injection, and none had a fever after subsequent injections. Only the subunit vaccine required three injections; there were 17 people among the controls, seven in the other neurological group, and eight participants in the epilepsy group who had the third injection. Three reported local reactions and two reported muscle pain.
TABLE 4.
General adverse events among three groups
| Healthy | Neuropsychiatric conditions | Epilepsy | p | |
|---|---|---|---|---|
| Participants who had 1st injection, n | 253 | 184 | 204 | |
| Adverse event after 1st injection, n (%) | 46 (18.2%) | 26 (14.1%) | 33 (16.2%) | .53 |
| Local injection site skin adverse events | 18 (7.1%) | 5 (2.7%) | 12 (5.9%) | .13 |
| Muscle pain | 18 (4.7%) | 5 (4.9%) | 12 (2.9%) | .55 |
| Fatigue | 10 (4.0%) | 8 (4.4%) | 4 (2.0%) | .37 |
| Headache | 3 (1.2%) | 4 (2.2%) | 4 (2.0%) | .70 |
| Drowsiness | 5 (2.0%) | 8 (4.4%) | 1 (.5%) | .03 |
| Fever | 0 | 1 (.5%) | 1 (.5%) | .52 |
| Others | 3 (1.2%) | 2 (1.1%) | 9 (4.4%) | .03 |
| Participants who had the 2nd injection, n | 196 | 123 | 139 | |
| Adverse event after 2nd injection, n (%) | 36 (18.4%) | 9 (7.3%) | 19 (13.7%) | .02 |
| Local injection site skin adverse events | 13 (6.6%) | 3 (2.4%) | 5 (3.6%) | .18 |
| Muscle pain | 13 (6.6%) | 1 (.8%) | 3(2.2%) | .01 |
| Fatigue | 5 (2.6%) | 2 (1.6%) | 2 (1.4%) | .73 |
| Headache | 0 | 1 (.8%) | 4 (2.9%) | .04 |
| Drowsiness | 4 (2.0%) | 1 (.8%) | 1 (.7%) | .49 |
| Others | 3 (1.5%) | 2 (1.6%) | 9 (6.5%) | .02 |
Adverse event rates were defined as the number of events divided by the number of people who had the 1st/2nd injection of vaccines.
Among controls, two participants visited the clinic for postvaccine seizurelike symptoms. The first was a 29‐year‐old female with no specific history who reported one seizure after her second inactivated vaccine injection. The other was a 37‐year‐old male who reported a seizure while playing mah‐jongg 5 days after vaccination. He was diagnosed with reflex epilepsy after a subsequent seizure also when playing mah‐jongg. After an investigation by the disease control and prevention administration, neither of the seizure incidences was considered vaccine‐induced. No status epilepticus or prolonged seizures were reported.
During the vaccination period, 19 participants with epilepsy reported increased seizure frequency after vaccination; two experienced seizure recurrence after >2 years seizure‐free. Two participants had a first‐ever convulsive seizure. Six withdrew medication, whereas two had add‐on ASMs during the vaccination for seizure control. The median seizure‐free interval for them was 3 months. The most prolonged interval was 58 months.
4. DISCUSSION
We report a dramatically lower first dose coverage of COVID‐19 vaccination in adults with epilepsy than people with other neuropsychiatric conditions and healthy controls. The general adverse effects were no higher in the epilepsy group, and no evidence of seizure worsening or status epilepticus was seen.
We found a significantly lower vaccination rate and hesitancy in people with epilepsy compared to nonepilepsy groups. We could not find data from other regions addressing this issue, apart from two uncontrolled cross‐sectional studies. One report from Germany suggested that fewer than one fifth of people with epilepsy had at least one dose, and a Kuwaiti report was similar. 5 , 6
The difference might be multifactorial. First, access and the population priority of vaccination might be significantly different due to the limited availability of vaccines. To date, three quarters of the world population has not yet been fully vaccinated, despite the unprecedented worldwide vaccination campaign. 9 The recommendation from ILAE suggests that the risk of COVID‐19 infection far outweighs the risk of adverse effects from vaccines. 10 Different countries have announced widely differing regulations, however, adapted to the local situation and culture. For example, people with epilepsy were listed as a priority group in the UK and other European countries, but in the United States and Thailand, epilepsy was not on the priority lists. 5 , 11 , 12 , 13 In China, with almost no new domestic cases since last May, severe neurological diseases, including people with “uncontrolled seizures,” were listed as contraindications in the guidelines during the study period. 7 As the primary readers of the guidelines were health professionals, this is unlikely to have affected the willingness of people with epilepsy to get vaccinated; however, this could have led to some clinicians not being willing to provide immunization. Uncontrolled epilepsy was also not clearly defined, nor was the minimal seizure frequency threshold set, so the guidance may have been overinterpreted. This uncertainty and ambiguity might harm promoting vaccinations in people with epilepsy.
Second, fear of seizure worsening was another factor. Our study suggests that compared to people with other chronic neuropsychiatric conditions such as depression, people with epilepsy had more concerns about safety and were worried about seizure exacerbation. This agrees with a previous study about vaccination safety, where efficacy and fear of epilepsy worsening were the two most common causes of vaccination hesitancy. 14
Third, in these two studies, data acquisition was 4–5 months previously, so rates may have changed since. 5 , 6
The potential for adverse effects was another critical issue influencing vaccination coverage. Thus far, no report has provided data comparing the vaccination rate among people with epilepsy and controls. The premarketing data of the currently used vaccines suggest good tolerance in the general population. Until recently, no real‐world data were available, but now two single‐center reports exist, with generally similar results from relatively small groups of epilepsy. 5 , 6 Our data also showed an equal distribution and prevalence of general adverse effects in epilepsy and nonepilepsy groups, other than a slightly higher rate of postvaccination headache in the epilepsy group. The most common adverse effects were pain at the injection site, myalgia, and fatigue, consistent with the previous two studies. 5 , 6 In the earlier studies, most had mRNA or adenoviral vector‐based vaccines, whereas most had inactivated vaccines in our study.
Interestingly, one healthy control reported a seizurelike event with no fever or other provoking factors and another one was diagnosed with reflex epilepsy after vaccination. A case report from India stated that a healthy older male had a first‐ever seizure following the first dose of the vaccine. 15 Investigations after the event showed normal electroencephalography for age, but ASM was started, as mild periventricular leukoaraiosis was seen on brain magnetic resonance imaging. No further seizure was reported at the subsequent 1‐month follow‐up. Only one person with new onset seizures among vaccinated individuals was reported in the premarketing phase of Chinese vaccines. We reported the second case of a seizure and the first case of reflex epilepsy in healthy subjects. Long‐term follow‐up and larger cohorts are warranted to test causality.
For people with epilepsy, whether the vaccination will trigger a seizure or cause other epilepsy‐specific side effects was a frequently asked question. No case of status epilepticus was reported after vaccination. Fewer than 10% reported seizure increase after vaccination, which might have been coincidental or within the natural variation of seizures. There was no evidence of seizure exacerbation in the group, and it is impossible to interpret the causality given the absence of control data. Nearly one third of those reporting an increase had stopped or reduced their ASM, fearing potential interaction with vaccinations. The reasons for the rise in seizures in the others remain unclear. Previous reports also reported a few people with seizure increases or status epilepticus for unknown reasons after vaccination. 5 Although the safety of vaccines requires long‐term studies, current evidence suggests they are likely to be safe. Intensive education programs are urgently needed to improve the coverage of the vaccine.
Our study has several limitations. First, the questionnaires were retrospective and self‐reported, introducing bias. Second, participating hospitals were tertiary centers, which might not represent the general population of people with epilepsy. We only enrolled adults, and most had inactivated vaccines. Third, our results are not generalizable, as vaccines used, guidelines, and local conditions vary. Our results, for instance, do not reflect the tolerability of mRNA vaccines. Lastly, our study had a relatively large population, but we did not actively monitor or perform further analysis on seizure worsening. Even though only a small number of people reported worsening seizures, given the lack of control data among people with epilepsy who are not vaccinated, we cannot draw definitive conclusions. In the future, studies with a larger cohort focusing on particular groups such as children or people with comorbidities are warranted to provide a clearer picture of vaccination safety in people with epilepsy.
5. CONCLUSIONS
Our data from a multicenter study in China suggest that the take‐up rate of vaccines in people with epilepsy was far behind their age‐matched counterparts. The general postvaccination effect, including painful injection site, muscle pain, and fatigue, was no higher than in controls, and there were no suggestions of seizure exacerbation due to the vaccination. The generalization of our results to other populations with different vaccine types and guidelines is, however, not possible. Education focused on increasing the vaccine coverage in people with epilepsy is warranted.
CONFLICT OF INTEREST
None of the authors has any conflict of interest to disclose. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Supporting information
Supplementary Material
ACKNOWLEDGMENTS
We are grateful to all the medical centers and their staff who took part in the project. We are also thankful to all the participants. We thank Dr. G. S. Bell for critically reviewing a previous version of the manuscript. This work was supported by grants from the National Natural Science Foundation of China (81801294, 81871017), the International Science and Technology Innovation Cooperation Project of Sichuan (2021YFH0141, 2019YFH0196), the Science and Technology Application Demonstration Project of the Chengdu Science and Technology Bureau (2019‐YF09‐00215‐SN), the 1.3.5 Project for Disciplines of Excellence, and the Brain Science Project of West China Hospital, Sichuan University (ZY2017305, ZYGD20011, ZYJC21001). J.W.S. is supported by the University College London Hospitals Biomedical Research Centre, which receives a proportion of funding from the UK Department of Health’s National Institute for Health Research; he also receives research support from the Dr Marvin Weil Epilepsy Research Fund, UK Epilepsy Society, and Christelijke Vereniging voor de Verplegingvan Lijders aan Epilepsie (the Netherlands).
Lu L, Zhang Q, Xiao J, Zhang Y, Peng W, Han X, et al. COVID‐19 vaccine take‐up rate and safety in adults with epilepsy: Data from a multicenter study in China. Epilepsia. 2022;63:244–251. doi: 10.1111/epi.17138
Contributor Information
Qi Zhang, Email: 1306914045@qq.com.
Dong Zhou, Email: zhoudong66@yahoo.de.
Weixi Xiong, Email: 502216168@qq.com, Email: zhoudong66@yahoo.de.
REFERENCES
- 1. US Food and Drug Administration . Comirnaty and Pfizer‐BioNTech COVID‐19 vaccine. https://www.fda.gov/emergency‐preparedness‐and‐response/coronavirus‐disease‐2019‐covid‐19/pfizer‐biontech‐covid‐19‐vaccine. Accessed 21 Aug 2021.
- 2. US Food and Drug Administration . Moderna COVID‐19 vaccine. https://www.fda.gov/emergency‐preparedness‐and‐response/coronavirus‐disease‐2019‐covid‐19/moderna‐covid‐19‐vaccine. Accessed 21 Aug 2021.
- 3. World Health Organization . COVID‐19 advice for the public: getting vaccinated . https://www.who.int/emergencies/diseases/novel‐coronavirus‐2019/covid‐19‐vaccines/advice. Accessed 21 Aug 2021.
- 4. Pruna D, Balestri P, Zamponi N, Grosso S, Gobbi G, Romeo A, et al. Epilepsy and vaccinations: Italian guidelines. Epilepsia. 2013;54(Suppl 7):13–22. [DOI] [PubMed] [Google Scholar]
- 5. von Wrede R, Pukropski J, Moskau‐Hartmann S, Surges R, Baumgartner T. COVID‐19 vaccination in patients with epilepsy: first experiences in a German tertiary epilepsy center. Epilepsy Behav. 2021;122:108160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Massoud F, Ahmad SF, Hassan AM, Alexander KJ, Al‐Hashel J, Arabi M. Safety and tolerability of the novel 2019 coronavirus disease (COVID‐19) vaccines among people with epilepsy (PwE): a cross‐sectional study. Seizure. 2021;92:2–9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chinese Center for Disease Control and Prevention . Technical guidelines for COVID‐19 vaccination (first edition). http://www.nhc.gov.cn/xcs/yqfkdt/202103/c2febfd04fc5498f916b1be080905771.shtml. Accessed 24 Aug 2021.
- 8. Kwan P, Schachter SC, Brodie MJ. Drug‐resistant epilepsy. N Engl J Med. 2011;365(10):919–26. [DOI] [PubMed] [Google Scholar]
- 9. Our World in Data. Coronavirus (COVID‐19) vaccinations. https://ourworldindata.org/covid‐vaccinations?country=OWID_WRL. Accessed 24 Aug 2021.
- 10. International League Against Epilepsy . COVID‐19 vaccines and people with epilepsy. https://www.ilae.org/patient‐care/covid‐19‐and‐epilepsy/covid‐19‐vaccines‐and‐people‐with‐epilepsy. Accessed 24 Aug 2021.
- 11. Department of Disease Control Covid vaccination guideline. bangkok: The Department of Disease Control, Ministration of Public Health of Thiland;(updated August 2021). 2021. [Google Scholar]
- 12. COVID‐19 vaccination first phase priority groups. https://www.gov.uk/government/publications/covid‐19‐vaccination‐care‐home‐and‐healthcare‐settings‐posters/covid‐19‐vaccination‐first‐phase‐priority‐groups. Accessed 24 Aug 2021.
- 13. Vaccines for COVID‐19 . https://www.cdc.gov/coronavirus/2019‐ncov/vaccines/index.html. Accessed 24 Aug 2021.
- 14. Puteikis K, Mameniskiene R. Factors associated with COVID‐19 vaccine hesitancy among people with epilepsy in Lithuania. Int J Environ Res Public Health. 2021;18(8):4374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ghosh R, Dubey S, Roy D, Mandal A, Naga D, Benito‐Leon J. Focal onset non‐motor seizure following COVID‐19 vaccination: a mere coincidence? Diabetes Metab Syndr. 2021;15(3):1023–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


