Abstract
Background
The term “orbital complication” does not designate an independent nosological entity, but is rather a collective designation for diseases or disease effects that involve the orbit and its internal structures by extension from outside. In general, their most prominent manifestation is swelling of the orbital soft tissues, usually unilaterally. The incidence of sinogenic orbital complications is approximately 1.6 per 100 000 children and 0.1 per 100 000 adults per year.
Methods
This review is based on publications retrieved by a selective search of the literature on the epidemiology, diagnosis, and treatment of sinogenic orbital complications.
Results
Acute sinusitis is the most common cause of orbital complications. These are diseases of the orbit with potentially serious consequences for the eye and the risk of intracranial complications such as cavernous sinus thrombosis, meningitis, or brain abscess. Aside from acute sinusitis, many other infectious and non-infectious diseases can extend to and involve the orbit. Because of the complexity and severity of the condition, its diagnosis and treatment are always an interdisciplinary matter. The treatment is primarily conservative, under observation in a hospital, and generally consists of the treatment of acute sinusitis with measures to combat edema along with the administration of broad-spectrum antibiotics. Surgical intervention is needed in severe cases or if there is an abscess. An endonasal approach is usually used for drainage.
Conclusion
In 95–98% of cases in stages I–IV, healing is complete and without further sequelae. Even if vision is affected preoperatively, it usually recovers fully when therapy is appropriate. Approximately 15% of the patients who undergo surgery need more than one operative procedure.
cme plus
This article has been certified by the North Rhine Academy for Continuing Medical Education. Participation in the CME certification program is possible only over the internet: cme.aerzteblatt.de. The deadline for submissions is 20 January 2023.
The term “orbital complication” does not designate an independent nosological entity but is rather a collective designation for diseases or disease effects that involve the orbit and its internal structures by extension from outside (1). Their cardinal symptom is unilateral swelling of the orbital soft tissues.
The most common cause of orbital complications is an acute sinusitis, with children being more commonly affected than adults (2). Between 4 and 20% of acute sinusitis cases develop complications, of which between 74 and 85% involve the orbit (2). The more frequent occurrence in children is partly due to the fact that their bone growth is not yet complete and the still open cranial sutures are predilection sites for inflammatory spread (3). The ethmoid cells are already present at birth, so sinusitis can also occur in infancy (4).
Apart from acute sinusitis, a number of other diseases may also invade the orbit. Depending on their cause, orbital complications can lead to further disturbances within a very short time, such as reduction or loss of visual acuity, restricted ocular motility, or intracranial complications. Accurate case history and examination, knowledge of pathogenesis and therapy, and interdisciplinary collaboration, especially between otolaryngology, ophthalmology, pediatrics, oral and maxillofacial surgery, and radiology, are crucial for correct diagnosis and successful cure.
The present review covers sinogenic orbital complications, their diagnosis, differential diagnosis, and therapy.
Basic anatomical principles
The orbit is a bony compartment. Rises in pressure, for example after hemorrhage or secondary to inflammation, can only be transmitted anteriorly to a limited extent (5).
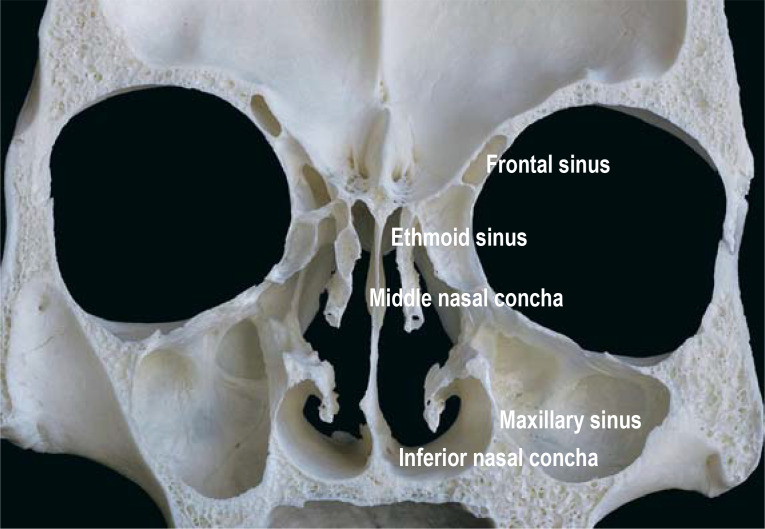
Topographically, the orbit is divided into an extraconal and an intraconal space. The intraconal space comprises the region between/within the extraocular muscles. The extraconal space is situated outside the musculofascial cone and is divided into a preseptal and a postseptal region. In adults, more than 60% of the orbital wall area is adjacent to the paranasal sinuses (5) (Figure 1).
Figure 1:
Proximity of the orbit to the paranasal sinuses (taken from [5], reprinted with kind permission of © Thieme Group)
Pathogenesis of sinogenic orbital complications
Inflammatory sinogenic orbital complications usually arise from an ethmoid or maxillary, less commonly from a frontal, sinusitis (6, 7). In children, too, the ethmoid cells are usually the starting point. The disease is milder in children under two years of age than in older ones (8, 9).
Few data are available regarding incidence. This is due to the fact that it is not a separate and clearly defined nosological entity. According to information obtained from the Federal Statistical Office (D-Statis; www.destatis.de, request 04. 10. 2021), 6647 patients were hospitalized in Germany in 2016 for acute sinusitis (ICD group J01) and 1905 patients for acute affection of the orbit (ICD group H05), of whom 670 (35%) were children under 15 years of age. According to a study of hospitalized cases in Scotland, the incidence of sinogenic orbital complications is 1.6/100 000 in children and 0.1/100 000 in adults (10). Analysis of cases identified in the Kids’ Inpatient Database revealed that 15 260 children were hospitalized with orbital sinogenic complications in the United States between 2003 and 2012 (11). An analysis from the same source showed a decrease in children hospitalized for acute rhinosinusitis from 8312 to 5592 between 2006 and 2016, but orbital complications increased from 8.9% to 19.3% in these children (12). A cohort study conducted in Sweden reported an incidence of acute rhinosinusitis in children under 18 years of age of 7.8/100 000 (9.2 in boys and 6.2 in girls). Thirty-four percent of these children had an orbital complication (13). Zhao et al. report similar figures after a systematic review of the literature (14).
Streptococcus species are among the most commonly detected pathogens, followed by Hemophilus influenzae and Staphylococcus strains (14– 17, e1– e3). Anaerobic and alpha-hemolytic streptococci are the pathogens usually identified in odontogenic sinusitis with a subsequent orbital complication (18).
Bony sites of predilection for inflammatory spread are the lamina papyracea and the floor of the frontal sinus. Anatomic variants can promote inflammatory spread (8, 18).
Inflammation in the paranasal sinuses increases pressure in the venous anastomoses between the ethmoid veins and the superior ophthalmic vein (valveless veins of Brechet). Venous blood flow increases towards the orbit. Bacterial toxins may lead to direct damage of the optic nerve, or there may be a spread of inflammation toward the cavernous sinus (e4, e5). In addition, activation of an inflammatory cascade leads to an increase in pressure, resulting in exophthalmos and facultative optic neuropathy (19). And finally, large parts of the orbital contents consist of relatively loose adipose tissue that does not present a barrier to the spread of inflammatory changes.
Classification
As regards inflammatory causes, sinogenic orbital complications must be distinguished from other inflammatory diseases. The latter may spread to the orbit (e.g., odontogenic focus), originate in the orbit itself (e.g., dacryocystitis), or be the result of facial trauma with or without a foreign body (20). Unilateral orbital swelling is the cardinal symptom. The case history is often already suggestive, revealing whether the process developed gradually, whether sinusitis, rhinitis, or an inflammatory disease of the teeth or jaw was present, or whether a trauma or an operation preceded it.
Sinogenic orbital complications progress in various phases. A number of classifications have been published (4, 20– 22). The term “orbital cellulitis”, often used in clinical terminology for all inflammations involving the orbit, is misleading. First, a distinction must be made between preseptal (approximately 70% of cases) and postseptal inflammation (approximately 25% of cases). Preseptal inflammation involves the eyelid region and does not affect internal structures of the orbit. Postseptal inflammation is considerably more serious. If left untreated, preseptal inflammation can also spread to the postseptal parts of the orbit (23) (table 1).
Table 1. Clinical characteristics of preseptal and postseptal orbital inflammation (taken from 20).
| Clinical symptom | Preseptal inflammation | Postseptal inflammation |
| Eyelid swelling | yes | yes |
| Periorbital erythema | yes | yes |
| Globe protrusion | no | incipient |
| Ocular motility / diplopia | normal/no | restricted/possibly yes |
| Painful reduced eye movements | no | yes |
| Orbital pain / pressure | no | yes |
| Visual acuity | perserved | possibly reduced |
| Pupillary reaction | normal | possibly pathological (relative afferent pupillary defect) |
| Chemosis: edema and hyperemia of the conjunctiva | rare | common |
| Corneal sensation | normal | possibly restricted |
| Fundoscopy | normal | possible pathological findings, e.g., congestion of retinal veins; blurred optic disc margins |
| Systemic symptoms (e.g., fever; general weakness) | mild to absent | common |
Because the cavernous sinus belongs anatomically to the intracranial structures, sinus cavernosus thrombosis is an intracranial complication and not an orbital complication in its strict sense (5, e6). Therefore, and for clinical practicality, existing classifications have been modified to a certain extent (1, 20) (table 2).
Table 2. Clinical symptoms of the individual stages of orbital complications of sinusitis.
| Stage | Description | Clinical symptoms |
| I | Preseptal edema/ eyelid edema | unilateral upper and/or lower eyelid swelling; confined to the preseptal region; unrestricted ocular motility, not painful; preserved visual acuity, normal pupillary reaction; active eye opening usually possible; no globe protrusion; only mild or moderate chemosis |
| II | Orbital periostitis | unilateral upper and/or lower eyelid swelling; erythema; ocular motility painful and restricted, but possible; exophthalmos; only passive opening of eyelids possible; significant chemosis; pupillary reaction and visual acuity still preserved |
| III | Subperiosteal abscess | unilateral upper and/or lower eyelid swelling; erythema; painful restriction of ocular motility; diplopia; exophthalmos; only passive opening of eyelids possible; pupillary reaction and visual acuity still preserved; significant chemosis |
| IV | Orbital abscess | unilateral, progressively taut, upper and/or lower eyelid swelling; erythema; painful restriction of ocular motility; incipient reduction of visual acuity; exophthalmos; only passive opening of eyelids possible; diplopia; pupillary reaction still preserved |
| V | Orbital cellulitis/ orbital apex syndrome | unilateral taut upper and/or lower eyelid swelling; loss of ocular motility due to paralysis of cranial nerves III, IV and VI (internal and external ophthalmoplegia); reduction of visual acuity to the point of amaurosis; pupillary response (light reflex and convergence reaction) usually absent; considerable chemosis; exophthalmos |
Stages I and II account for approximately 75–80% of sinogenic orbital complications (24) (figure 2). The location of a subperiosteal abscess provides an indication of which paranasal sinus can be considered its point of origin (e7). It is usually not possible clinically to distinguish between periostitis and a subperiosteal abscess. Computed tomography (CT) or magnetic resonance imaging (MRI) is required here.
Figure 2.
Patient with an orbital complication secondary to acute right ethmoid sinusitis associated with considerable swelling of the orbital soft tissues.
A staging classification for children is more difficult than for adults. In stage I the eye is often already swollen shut and can only be opened passively, while in stage III reduced visual acuity and double vision may also occur.
An orbital abscess or subperiosteal abscess may progress to orbital cellulitis. Pus may breach the abscess membrane and cause diffuse infiltration of the internal orbital structures with spread to the adipose tissue, intraorbital muscles, and nerve structures. This can result in neuritis of cranial nerves II, III, IV, and VI with subsequent ophthalmoplegia and reduced visual acuity, progressing even to amaurosis (orbital apex syndrome). Due to the obstruction of venous outflow, the bulb clinically appears taut, with significant exophthalmos and chemosis. The eye can only be opened passively under pain, ocular motility is absent, and the pupillary light reaction and convergence response can no longer be elicited (25). According to meta-analyses, intracranial complications occur in approximately 10% of all patients with an orbital complication, and amaurosis develops in 2–12%, with the risk of loss of visual acuity increasing with progression of stage (6, 26– 28, e7– e9).
Diagnostic investigations
The diagnostic work-up is an interdisciplinary task involving otolaryngology (ENT), ophthalmology, pediatrics, oral and maxillofacial surgery, radiology, and possibly other specialties. The parents should be involved where children are concerned. The first clue is a medical history of acute rhinitis in the past. The cardinal symptom of an orbital complication is unilateral swelling of the orbital soft tissues with proptosis.
In a case-control study of 43 patients, multivariate logistic regression showed a positive association of ethmoid sinusitis with orbital complications (odds ratio [OR] 31.1; 95% confidence interval: [2.3; 430.6]) (26). In this study, a shorter duration of symptoms was associated with a higher risk of orbital complications (OR 0.9 [0.8; 0.9]). In a retrospective study of 83 patients, ethmoid sinusitis was diagnosed as the source of infection in 75.6% and maxillary sinusitis in 81.7% (28).
Loss of visual acuity to initially <20/200 and an afferent defect are considered prognostically unfavorable with respect to recovery of visual acuity (27, 29), as is inflammation-related central retinal artery occlusion (30).
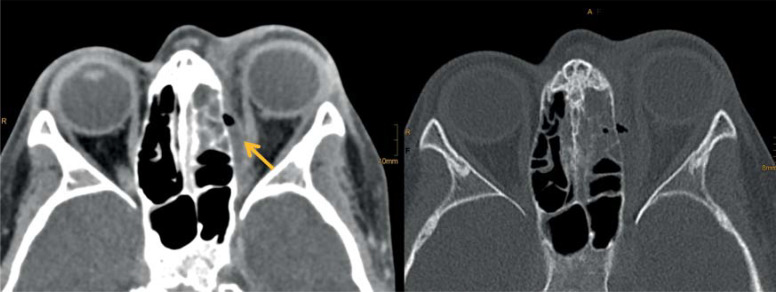
CT is considered the gold standard in the diagnostic workup and for determining the extent of orbital complication (6, e10). This also allows an abscess to be detected and its size estimated (e11) (Figure 3). A meta-analysis involving more than 1100 patients aged up to 18 years showed that restricted ocular motility occurred in about 46% of cases, proptosis in 44%, and fever in 35% (16). Staphylococcus aureus was the most commonly isolated pathogen. These findings are considered indicative of a sinogenic orbital complication (16, 28). Fatal courses have also been reported in isolated cases (31). Apart from acute sinusitis, odontogenic infection is the most common cause, usually originating from the roots of the first molars (18, 32). A skin infection is the cause of an orbital complication in 15.2% (27) and dacryocystitis in 13.6% of cases (27).
Figure 3a.
Computed tomography depicting a right subperiosteal abscess, originating from an ethmoid sinusitis in a 7-year-old child. Gas inclusions are evident within the abscess.
In an analysis of data from 125 children with unilateral swelling of the orbital soft tissues in our own patient population, a sinogenic orbital complication was found in 38.4%, followed by skin infections (16.8%), dacryocystitis (12%), conjunctivitis (9.6%), and odontogenic causes (5%). These findings confirm the results of previous studies (33).
Based on the presented studies and clinical experience, the following recommendations for diagnostic measures are presented:
Examination by an ENT specialist with endoscopy of the nasal cavity
-
Examination by an ophthalmologist with
assessment of visual acuity
examination of pupillomotor function
examination of the anterior and posterior segments of the eye
assessment of the field of vision, of exophthalmos using the Hertel method, intraocular pressure and eye motility
CT or digital volume tomography (DVT) of the paranasal sinuses and the orbit, consider ultrasound
Blood sampling to determine inflammatory parameters, including C-reactive protein and possibly procalcitonin (fever, elevated CRP levels and pus in the middle nasal passage are indicative of a sinogenic focus, especially in children [33])
A swab sample should be taken for microbiological examination in the presence of pus in the nasal cavity.
Treatment
No randomized controlled trials of therapy have been published to date. The literature usually contains case-control studies or meta-analyses with level of evidence grades between IIa and IV. Inpatient management is indicated for sinogenic orbital complications. The question of whether a conservative or surgical course of action is indicated is significantly determined by the clinical symptoms, the type of previous treatment, and the stage of the disease (24). According to a meta-analysis by Zhao et al (14), the proportion of pediatric patients requiring surgery has decreased from 45.2% in studies published before 2010 to 21.7% in subsequent years.
Conservative therapy is largely the same as for acute sinusitis, i.e., involving decongestant measures, for example, with nasal sprays containing 0.1% xylometazoline to reduce edematous obstruction of the sinus ostia (e12, e13).
Broad-spectrum penicillins, such as ampicillin and sulbactam, are drugs of first choice; alternatively, a third-generation cephalosporin may be given in combination with metronidazole (34, e13), and clindamycin may be given in cases of penicillin allergy (34).
Antibiotic therapy should be administered intravenously because of the better and faster bioavailability of antibiotics in the walls of the paranasal sinuses and in the orbital soft tissues (35).
In stage I (= periseptal edema) and II (= periostitis) disease without previous antibiotic treatment, conservative therapy with close monitoring of the patient is usually sufficient (2, 35). If progression occurs within 24 hours of therapy (loss of visual acuity; restricted ocular motility; exophthalmos), CT or digital volumetric tomography (DVT) of the paranasal sinuses followed by surgical intervention is indicated (6). In children, the indication for CT is particularly restrictive because of radiation exposure with subsequent potential complications. The latest generation of CT scanners and DVT are associated with significantly lower radiation exposure (e14– e17).
In stages III (= subperiosteal abscess), IV (= orbital abscess), and V (= orbital cellulitis with orbital apex syndrome), immediate surgical intervention is indicated in addition to the administration of antibiotics. The indication for surgery is also based on abscess size (2, 16, 27, e9, e11), with extensive abscesses with a volume of >1500 mm3 or an extension of >4 mm always requiring surgical drainage (OR: 3.66 [2.40; 5.44]) (16, 27, e9). Proptosis and gaze restriction were also predictors of surgery (OR: 1.65 [1.29; 2.12] and relative risk [RR] 1.9 [1.2; 3], respectively) (16). In a meta-analysis by Adil et al, half of the included patients required surgical drainage (16).
In 55 children and adolescents with orbital complications secondary to acute rhinosinusitis, retrospective evaluation showed that pharmacologic intervention alone was sufficient in 60% of cases, whereas drainage was required in 40%. Seven patients developed complications, which healed uneventfully in six. The average stay in hospital was 8±5 days. Six patients developed recurrence of infection (around 11%) (6).
Additional subcutaneous administration of heparin (for example, enoxaparin, based on body weight) is recommended in adults for prevention of sinus vein thrombosis, with the possible administration of glucocorticoids (for example, prednisolone 100 mg/die) for several days (1, 20).
Surgical procedures center on endonasal access routes involving minimally invasive endonasal endoscopic surgical approaches (24, 36). They have been shown to be effective, safe, and have a low complication rate (36, 37). The initial step involves endonasal ethmoid surgery. The lamina papyracea is removed and the periorbita incised. In the presence of a subperiosteal abscess, pus now discharges into the ethmoid (e9). In the case of an intraorbital abscess, the orbital soft tissues are further dissected until the abscess can be drained. If the abscess is located in the cranial and lateral regions, external drainage may also be necessary via an anterior orbitotomy or via a lateral orbitotomy (24, 36, e7, e12). The external approaches have the disadvantage of scarring with possible persistent paresthesia. The use of a computerized navigation system is useful for precise localization. Complications of the endonasal approach are rare, occurring in 0.36–3% of cases (e18), of which postoperative bleeding and loss of smell are the most common (approx. 1% of cases). Injury to the base of the skull with subsequent CSF leakage (<1%) and blindness from iatrogenic optic nerve injury have been reported (0.15%) (38, e18– e20). In addition, recurrent abscess formation in the orbital soft tissues may occur in up to 17% of cases, requiring multiple surgical procedures (11, 15, e19).
The differential diagnoses are numerous (3, e21– e25) and demonstrate the complexity of unilateral orbital swelling, the diagnosis and therapy of which are always interdisciplinary (table 3).
Table 3. Common differential diagnoses of unilateral orbital swelling.
| Description | Diseases |
|
Infectious causes (in the orbit itself or spread to the orbit) |
● orbital complication of acute sinusitis (most common cause at approx. 35–40%) ● odontogenic causes (approx 20%; second most common cause) ● dacryocystitis (third most common cause) − acute − chronic ● infected insect bite ● mycosis in particular mucormycosis in patients with severe general diseases and immunosuppression) ● hordeolum/chalazion ● infections of the skin ● conjunctivitis |
| Non-infectious diseases of the orbit | ● orbital emphysema ● endocrine orbitopathy ● idiopathic orbital inflammatory disease (orbital pseudotumor) ● IgG4-associated orbital disease ● lymphoid hyperplasia of the orbit ● orbital myositis ● granulomatous diseases (granulomatosis with polyangiitis; Tolosa-Hunt syndrome; sarcoidosis) ● vasculitis ● allergic diseases |
| Cystic and tumorous lesions | ● dermoid cysts ● mucocele of the paranasal sinuses ● encephalocele ● vascular tumors (hemangiomas) ● vascular malformations ● lacrimal gland adenomas (pleomorphic adenomas) ● lacrimal gland carcinomas ● optic nerve glioma ● optic nerve sheath meningioma ● secondary meningioma ● plexiform neurofibroma ● malignant lymphomas ● sarcomas ● metastases ● tumors of the paranasal sinuses with orbital infiltration |
Recommendations for clinical practice
Orbital complications are diseases with potentially serious consequences for the eye, even to the extent of blindness and the risk of intracranial complications with thrombosis of the cavernous sinus, meningitis or brain abscess. Unilateral orbital swelling is the cardinal symptom. Approximately one third of orbital swellings are due to a sinogenic orbital complication. Any suspected sinogenic orbital complication requires hospital admission and treatment to be able to react immediately in the event of deterioration.
In 95–98% of cases, complete and uncomplicated healing is to be expected in stages I–IV. Even preoperative impairment of visual acuity usually recovers (24, 39). However, prognosis in terms of function is worse with orbital apex syndrome, preoperative visual acuity of <20/200, intracranial spread of inflammation, and afferent defect (27, 28, 40). Approximately 15% of patients who undergo surgical management require more than one surgical procedure (11, 15). A few studies reported long-term effects with neurological complications (e26).
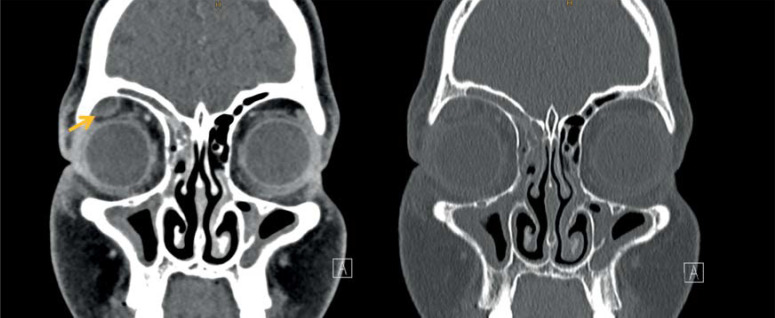
Figure 3b.
Coronal computed tomography section of a 10-year-old boy with an abscess located in the cranio-lateral orbit, originating from a right frontal sinusitis. (Reprint of the two images with kind permission of Dr. J. Weidemann, Department for Pediatric Radiology and Ultrasound of the Pediatric Hospital auf der Bult, Hanover, Germany).
Questions on the article in issue 3/2022:
Sinogenic Orbital Complications
The submission deadline is 20 January 2023. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What is the incidence of sinogenic orbital complications in children?
0.01/100 000
0.6/100 000
1.6/100 000
5.3/100 000
16.1/100 000
Question 2
What is the most common cause of orbital complications?
Acute sinusitis
Acute conjunctivitis
Active labial herpes
Acne vulgaris
Erysipelas
Question 3
What is the term for the space within the orbit that is outside the extraocular muscles?
Intraconal space
Peribulbar space
Interconal space
Extraconal space
Extrabulbar space
Question 4
Which sinuses are most often the origin of sinogenic orbital complications in the adult patient?
Frontal and maxillary sinuses
Sphenoid and maxillary sinuses
Frontal and sphenoid sinuses
Ethmoid or maxillary sinus
Ethmoid and frontal sinuses
Question 5
What clinical symptom typically occurs in preseptal inflammation?
Impairment of visual acuity
Reduced pupillary reaction
Orbital pain
Globe protrusion
Eyelid swelling
Question 6
Which cerebral sinus is particularly susceptible to disseminated inflammation from the orbital area?
Inferior petrosal sinus
Cavernous sinus
Transverse sinus
Straight sinus
Superior sagittal sinus
Question 7
Orbital complications can have dental root inflammation as a starting point. Which tooth is then usually the point of origin?
Canine
First premolar
Second premolar
First molar
Second molar
Question 8
What is the medication of first choice for conservative management of orbital complications?
Oral clindamycin
Intravenous broad-spectrum penicillin
Broad-spectrum penicillin as a nasal spray
Clindamycin as a nasal spray
Oral metronidazole
Question 9
In what percentage of cases can complete and uneventful healing be expected in stages I-IV of orbital complications of sinusitis?
25–37%
48–53%
65–73%
75–85%
95–98%
Question 10
Approximately what percentage of patients operated on for orbital complications must undergo at least one additional surgical procedure?
1%
5%
10%
15%
25%
Acknowledgments
Translated from the original German by Dr. Grahame Larkin, MD
Footnotes
Conflict of interest statement
Prof. Welkoborsky, Dr. Grass and Prof. Wiechens received editor‘s royalties for publications related to the topic from Thieme medical publishers, Prof. Welkoborsky and Prof. Wiechens also from Science Press.
The other authors declare that no conflict of interest exists.
References
- 1.Graß SK, Welkoborsky HJ. Welkoborsky HJ, Wiechens H, Hinni ML, editors. Orbitale Komplikationen. Orbita. Thieme Verlag. 2016:112–124. [Google Scholar]
- 2.Wong SJ, Levi J. Management of pediatric orbital cellulitis: a systematic review. Int J Pediatr Otorhinolaryngol. 2018;110:123–129. doi: 10.1016/j.ijporl.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Santos JC, Pinto S, Ferreira S, Maia S, Alves S, da Silva V. Pediatric preseptal and orbital cellulitis: a 10-year experience. Int J Pediatr Otorhinolaryngol. 2019;120:82–88. doi: 10.1016/j.ijporl.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Stammberger H. Komplikationen der Entzündungen der Nasennebenhöhlen und des Oberkiefers. Europ Arch Otolaryngol, Suppl. I, 1993:14–15. [Google Scholar]
- 5.Schmiedl A. Welkoborsky HJ, Wiechens B, Hinni ML, editors. Topographische Anatomie der Orbita. Orbita. Thieme Verlag. 2016:5–42. [Google Scholar]
- 6.Martins M, Martins SP, Pinto-Moura C, Leal V, Spratley J. Management of post-septal complications of acute rhinosinusitis in children: a 14-year experience in a tertiary hospital. Int J Pediatr Otorhinolaryngol. 2021;151 doi: 10.1016/j.ijporl.2021.110925. 110925. [DOI] [PubMed] [Google Scholar]
- 7.Mekhitarian Neto L, Pignatari S, Mitsuda S, Fava AS, Stamm A. Acute sinusitis in children: a retrospective study of orbital complications. Braz J Otorhinolaryngol. 2007;73:75–79. doi: 10.1016/S1808-8694(15)31126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jabarin B, Marom T, Gavriel H, Eviatar E, Pitaro J. Orbital complications secondary to acute rhinosinusitis in toddlers: a unique age group. Int J Pediatr Otorhinolaryngol. 2019;121:46–49. doi: 10.1016/j.ijporl.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Trivić A, Cevik M, Folić M, et al. Management of orbital complications of acute rhinosinusitis in pediatric patients: a 15-year single-center experience. Pediatr Infect Dis J. 2019;38:994–998. doi: 10.1097/INF.0000000000002414. [DOI] [PubMed] [Google Scholar]
- 10.Murphy C, Livingstone I, Foot B, Murgatroyd H, MacEwen CJ. Orbital cellulitis in Scotland: current incidence, aetiology, management and outcomes. Br J Ophthalmol. 2014;98:1575–1578. doi: 10.1136/bjophthalmol-2014-305222. [DOI] [PubMed] [Google Scholar]
- 11.Villwock MR, Villwock JA. Incidence and extent of sinus procedures in treatment of pediatric orbital cellulitis. Int J Pediatr Otorhinolaryngol. 2020;135 doi: 10.1016/j.ijporl.2020.110086. 110086. [DOI] [PubMed] [Google Scholar]
- 12.Levy DA, Nguyen SA, Harvey R, Hopkins C, Schlosser RJ. Hospital utilization for orbital and intracranial complications of pediatric acute rhinosinusitis. Int J Pediatr Otorhinolaryngol. 2020;128 doi: 10.1016/j.ijporl.2019.109696. 109696. [DOI] [PubMed] [Google Scholar]
- 13.Hultman Dennison S, Hertting O, Bennet R, et al. A Swedish population-based study of complications due to acute rhinosinusitis in children 5-18 years old. Int J Pediatr Otorhinolaryngol. 2021;150 doi: 10.1016/j.ijporl.2021.110866. 110866. [DOI] [PubMed] [Google Scholar]
- 14.Zhao EE, Koochakzadeh S, Nguyen SA, Yoo F, Pecha P, Schlosser RJ. Orbital complications of acute bacterial rhinosinusitis in the pediatric population: a systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol. 2020;135 doi: 10.1016/j.ijporl.2020.110078. 110078. [DOI] [PubMed] [Google Scholar]
- 15.Chorney SR, Buzi A, Rizzi ND. The role of endoscopic sinus surgery in children undergoing external drainage of non-medial subperiosteal orbital abscess. Am J Rhinol Allergy. 2021;35:288–295. doi: 10.1177/1945892420953790. [DOI] [PubMed] [Google Scholar]
- 16.Adil EA, Muir ME, Kawai K, Dombrowski ND, Cunningham MJ. Pediatric subperiosteal abscess secondary to acute sinusitis: a systematic review and meta-analysis. Laryngoscope. 2020;130:2906–2912. doi: 10.1002/lary.28570. [DOI] [PubMed] [Google Scholar]
- 17.Peña MT, Preciado D, Orestes M, Choi S. Orbital complications of acute sinusitis: changes in the post-pneumococcal vaccine era. JAMA Otolaryngol Head Neck Surg. 2013;139:223–227. doi: 10.1001/jamaoto.2013.1703. [DOI] [PubMed] [Google Scholar]
- 18.Craig JR, Cheema AJ, Dunn RT, Vemuri S, Peterson E. Extrasinus complications from odontogenic sinusitis: a systematic review. Otolaryngol Head Neck Surg. 2021;13 doi: 10.1177/01945998211026268. 1945998211026268. [DOI] [PubMed] [Google Scholar]
- 19.Welkoborsky HJ, Kraft T. Welkoborsky HJ, Wiechens B, Hinni ML, editors. Pathophysiologische Aspekte der Orbita. Orbita. Thieme Verlag. 2016:35–43. [Google Scholar]
- 20.Graß SK, Welkoborsky HJ, Glien A, Plontke S. Orbitale Komplikationen. HNO. 2018;66:800–811. doi: 10.1007/s00106-018-0569-3. [DOI] [PubMed] [Google Scholar]
- 21.Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414–1428. doi: 10.1288/00005537-197009000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Kastenbauer E. Naumann HH, Helms J, Herberhold C, Kastenbauer E, editors. Komplikationen der Entzündungen der Nasennebenhöhlen und des Oberkiefers. Oto-Rhino-Laryngologie in Klinik und Praxis, Band 2, Thieme, Stuttgart. 1992:234–246. [Google Scholar]
- 23.Dennison SH, Aks LS, Eriksson M, et al. Serious complications due to acute rhinosinusitis in children up to five years old in Stockholm, Sweden—still a challenge in the pneumococcal conjugate vaccine era. Int J Pediatr Otorhinolaryngol. 2019;121:50–54. doi: 10.1016/j.ijporl.2019.02.034. [DOI] [PubMed] [Google Scholar]
- 24.Chrobok V, Pellant A, Mandysova P, Mejzlik J, Dedkova J, Celakovsky P. Rhinogenic orbital inflammation—what has changed over the past 50 years? Acta Medica (Hradec Kralove) 2019;62:94–98. doi: 10.14712/18059694.2019.131. [DOI] [PubMed] [Google Scholar]
- 25.Huang Y, Gui L. Cavernous sinus-orbital apex aspergillus infection in a diabetic patient: a case report. Medicine (Baltimore) 2019;98 doi: 10.1097/MD.0000000000015041. e15041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snidvongs K, Chitsuthipakorn W, Akarapas C, et al. Risk factors of orbital complications in outpatients presenting with severe rhinosinusitis: a case-control study. Clin Otolaryngol. 2021;46:587–593. doi: 10.1111/coa.13718. [DOI] [PubMed] [Google Scholar]
- 27.Aryasit O, Aunruan S, Sanghan N. Predictors of surgical intervention and visual outcome in bacterial orbital cellulitis. Medicine (Baltimore) 2021;100 doi: 10.1097/MD.0000000000026166. e26166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chang Y-S, Chen P-L, Hung J-H, et al. Orbital complications of paranasal sinusitis in Taiwan, 1988 through 2015: acute ophthalmological manifestations, diagnosis, and management. PLoS One. 2017;12 doi: 10.1371/journal.pone.0184477. e0184477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tomaç S, Turgut S. Orbital cellulitis and irreversible visual loss owing to acute sinusitis. Ann Ophthalmol (Skokie) 2006;38:131–133. doi: 10.1385/ao:38:2:131. [DOI] [PubMed] [Google Scholar]
- 30.Chen X, Man X, Dong L, Luan J, Li Y, Song X. Central artery occlusion due to subperiosteal orbital abscess caused by acute sinusitis in a child: a case report. Ear Nose Throat J. 2021;12 doi: 10.1177/01455613211016731. 1455613211016731. [DOI] [PubMed] [Google Scholar]
- 31.Sharma S, Josephson GD. Orbital complications of acute sinusitis in infants: a systematic review and report of a case. JAMA Otolaryngol Head Neck Surg. 2014;140:1070–1073. doi: 10.1001/jamaoto.2014.2326. [DOI] [PubMed] [Google Scholar]
- 32.Arunkumar KV. Orbital infection threatening blindness due to carious primary molars: an interesting case report. J Maxillofac Oral Surg. 2016;15:72–75. doi: 10.1007/s12663-015-0801-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Welkoborsky HJ, Graß S, Deichmüller C, Bertram O, Hinni ML. Orbital complications in children: differential diagnosis of a challenging disease. Europ. Arch. Otolaryngol. 2015;272:1157–1163. doi: 10.1007/s00405-014-3195-z. [DOI] [PubMed] [Google Scholar]
- 34.Cushen R, Francis NA. Antibiotic use and serious complications following acute otitis media and acute sinusitis: a retrospective cohort study. Br J Gen Pract. 2020;26 doi: 10.3399/bjgp20X708821. 70: e255–e263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El Mograbi A, Ritter A, Najjar E, Soudry E. Orbital complications of rhinosinusitis in the adult population: analysis of cases presenting to a tertiary medical center over a 13-year period. Ann Otol Rhinol Laryngol. 2019;128:563–568. doi: 10.1177/0003489419832624. [DOI] [PubMed] [Google Scholar]
- 36.Sekhar V, Ao J, Iqbal I, Ooi EH, Munn Z. Effectiveness of endoscopic versus external surgical approaches in the treatment of orbital complications of rhinosinusitis: a systematic review protocol. JBI Database System Rev Implement Rep. 2019;17:2378–2389. doi: 10.11124/JBISRIR-2017-003972. [DOI] [PubMed] [Google Scholar]
- 37.Zoli M, Sollini G, Milanese L, et al. Endoscopic approaches to orbital lesions: case series and systematic literature review. J Neurosurg. 2020;3:1–13. doi: 10.3171/2019.10.JNS192138. [DOI] [PubMed] [Google Scholar]
- 38.Seredyka-Burduk M, Burduk PK, Wierzchowska M, Kaluzny B, Malukiewicz G. Ophthalmic complications of endoscopic sinus surgery. Braz J Otorhinolaryngol. 2017;83:318–323. doi: 10.1016/j.bjorl.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta S, Goyal R, Gupta RK. Clinical presentation and outcome of the orbital complications due to acute infective rhino sinusitis. Indian J Otolaryngol Head Neck Surg. 2013;65 (Suppl 2):431–434. doi: 10.1007/s12070-013-0646-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh M, Negi A, Zadeng Z, Verma R, Gupta P. Long-term ophthalmic outcomes in pediatric orbital cellulitis: a prospective, multidisciplinary study from a tertiary-care referral institute. J Pediatr Ophthalmol Strabismus. 2019;56:333–339. doi: 10.3928/01913913-20190807-01. [DOI] [PubMed] [Google Scholar]
- E1.Aring AM, Chan MM. Acute rhinosinusitis in adults. Am Fam Physician. 2011;83:1057–1063. [PubMed] [Google Scholar]
- E2.Danishyar A, Sergent SR. Orbital cellulitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2020 [PubMed] [Google Scholar]
- E3.Levy DA, Pecha PP, Nguyen SA, Schlosser RJ. Trends in complications of pediatric rhinosinusitis in the United States from 2006-2016. Int J Pediatr Otorhinolaryngol. 2020;128 doi: 10.1016/j.ijporl.2019.109695. 109695. [DOI] [PubMed] [Google Scholar]
- E4.Sotoudeh H, Shafaat O, Aboueldahab N, Vaphiades M, Sotoudeh E, Bernstock J. Superior ophthalmic vein thrombosis: what radiologist and clinician must know? Eur J Radiol Open. 2019;6:258–264. doi: 10.1016/j.ejro.2019.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Chen MC, Ho YH, Chong PN, Chen JH. A rare case of septic cavernous sinus thrombosis as a complication of sphenoid sinusitis. Ci Ji Yi Xue Za Zhi. 2019;31:63–65. doi: 10.4103/tcmj.tcmj_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Bhatia H, Kaur R, Bedi R. MR imaging of cavernous sinus thrombosis. Eur J Radiol Open. 2020;7 doi: 10.1016/j.ejro.2020.100226. 100226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Linton S, Pearman A, Joganathan V, Karagama Y. Orbital abscess as a complication of Pott´s puffy tumor in an adolescent male. BMJ Case Rep. 2019;12 doi: 10.1136/bcr-2019-229664. pii:e229664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.De Melo WM, Sonoda CK, Hochuli-Vieira E, Gabrielli MA, Gabrielli MF. Paranasal sinus infection causing orbital subperiosteal abscess: surgical management of this devastating entity. Oral Maxillofac Surg. 2013;17:131–135. doi: 10.1007/s10006-012-0343-8. [DOI] [PubMed] [Google Scholar]
- E9.Sansa-Perna A, Gras-Cabrerizo JR, Montserrat-Gili JR, Rodríguez-Álvarez F, Massegur-Solench H, Casasayas-Plass M. Our experience in the management of orbital complications in acute rhinosinusitis. Acta Otorrinolaringol Esp (Engl Ed) 2020;71:296–302. doi: 10.1016/j.otorri.2019.11.005. [DOI] [PubMed] [Google Scholar]
- E10.Mabrouk AB, Wannes S, Hasnaoui M, et al. Orbital complication of acute ethmoiditis: a Tunisian paediatric cross sectional study. Am J Otolaryngol. 2020;41 doi: 10.1016/j.amjoto.2019.102320. 102320. [DOI] [PubMed] [Google Scholar]
- E11.Sussman SM, Sharbel DD, Momin A, Prosser JD, Carroll WW. Cost comparison between surgical and conservative management for pediatric sinogenic subperiosteal abscesses. Int J Pediatr Otorhinolaryngol. 2021;140 doi: 10.1016/j.ijporl.2020.110542. 110542. [DOI] [PubMed] [Google Scholar]
- E12.Sciarretta V, Demattè M, Farneti P, et al. Management of orbital cellulitis and subperiosteal orbital abscess in pediatric patients: a ten-year review. Int J Pediatr Otorhinolaryngol. 2017;96:72–76. doi: 10.1016/j.ijporl.2017.02.031. [DOI] [PubMed] [Google Scholar]
- E13.Mahalingam S, Hone R, Lloyd G, et al. The management of periorbital cellulitis secondary to sinonasal infection: a multicenter prospective study in the United Kingdom. Int Forum Allergy Rhinol. 2020;10:726–737. doi: 10.1002/alr.22535. [DOI] [PubMed] [Google Scholar]
- E14.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E15.Bernier M-O, Rehel J-L, Brisse HJ, et al. Radiation exposure from CT in early childhood: a French large scale multicentre study. Br J Radiol. 2012;85:53–60. doi: 10.1259/bjr/90758403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Meulepas JM, Ronckers CM, Smets AMJB, et al. Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst. 2019;111:256–263. doi: 10.1093/jnci/djy104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Gaudreau K, Thome C, Weaver B, Boreham DR. Cataract formation and low-dose radiation exposure from head computed tomography (CT) scans in Ontario, Canada, 1994-2015. Radiat Res. 2020;193:322–330. doi: 10.1667/RR15504.1. [DOI] [PubMed] [Google Scholar]
- E18.Halderman AA, Sindwani R, Woodard TD. Hemorrhagic complications of endoscopic sinus surgery. Otolaryngol Clin North Am. 2015;48:783–793. doi: 10.1016/j.otc.2015.05.006. [DOI] [PubMed] [Google Scholar]
- E19.Teinzer F, Stammberger H, Tomazic PV. Transnasal endoscopic treatment of orbital complications of acute sinusitis: the Graz concept. Ann Otol Rhinol Laryngol. 2015;124:368–373. doi: 10.1177/0003489414558110. [DOI] [PubMed] [Google Scholar]
- E20.Humphreys IM, Hwang PH. Avoiding complications in endoscopic Sinus Surgery. Otolaryngol Clin North Am. 2015;48:871–881. doi: 10.1016/j.otc.2015.05.013. [DOI] [PubMed] [Google Scholar]
- E21.Hwang K, Kim DH, Lee HS. Orbital fracture due to high-pressure air injection. J Craniofac Surg. 2011;22:1506–1507. doi: 10.1097/SCS.0b013e31821d4c3a. [DOI] [PubMed] [Google Scholar]
- E22.Chang JR, Rajaii F, McCulley TJ. Delayed orbital emphysema mimicking orbital cellulitis: an uncommon complication of dental surgery. Middle East Afr J Ophthalmol. 2019;26:175–177. doi: 10.4103/meajo.MEAJO_241_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E23.Pitz S. Orbital inflammation: current trends. Klin Monbl Augenheilkd. 2020;23:353–367. doi: 10.1055/a-1090-3167. [DOI] [PubMed] [Google Scholar]
- E24.Farooq AV, Patel RM, Lin AY, Setabutr P, Sartori J, Aakalu VK. Fungal orbital cellulitis: presenting features, management and outcomes at a referral center. Orbit. 2015;34:152–159. doi: 10.3109/01676830.2015.1014512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E25.Zayet S, Zaghdoudi A, Ammari L, Kilani B, Benaissa HT. Cerebro-rhino-orbital mucormycosis and aspergillosis coinfection in a patient with diabetes mellitus: a case report. IDCases. 2020;23 doi: 10.1016/j.idcr.2020.e01022. e01022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E26.Ziegler A, Patadia M, Stankiewicz J. Neurological complications of acute and chronic sinusitis. Curr Neurol Neurosci Rep. 2018;18 doi: 10.1007/s11910-018-0816-8. [DOI] [PubMed] [Google Scholar]