Abstract
Meteorological factors have been confirmed to affect the COVID-19 transmission, but current studied conclusions varied greatly. The underlying causes of the variance remain unclear. Here, we proposed two scientific questions: (1) whether meteorological factors have a consistent influence on virus transmission after combining all the data from the studies; (2) whether the impact of meteorological factors on the COVID-19 transmission can be influenced by season, geospatial scale and latitude. We employed a meta-analysis to address these two questions using results from 2813 published articles. Our results showed that, the influence of meteorological factors on the newly-confirmed COVID-19 cases varied greatly among existing studies, and no consistent conclusion can be drawn. After grouping outbreak time into cold and warm seasons, we found daily maximum and daily minimum temperatures have significant positive influences on the newly-confirmed COVID-19 cases in cold season, while significant negative influences in warm season. After dividing the scope of the outbreak into national and urban scales, relative humidity significantly inhibited the COVID-19 transmission at the national scale, but no effect on the urban scale. The negative impact of relative humidity, and the positive impacts of maximum temperatures and wind speed on the newly-confirmed COVID-19 cases increased with latitude. The relationship of maximum and minimum temperatures with the newly-confirmed COVID-19 cases were more susceptible to season, while relative humidity's relationship was more affected by latitude and geospatial scale. Our results suggested that relationship between meteorological factors and the COVID-19 transmission can be affected by season, geospatial scale and latitude. A rise in temperature would promote virus transmission in cold seasons. We suggested that the formulation and implementation of epidemic prevention and control should mainly refer to studies at the urban scale. The control measures should be developed according to local meteorological properties for individual city.
Keywords: SARS-CoV-2, COVID-19 spread, Cold and warm seasons, National and urban scales, GLMs
1. Introduction
Coronavirus disease (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (WHO, 2021a). The virus is highly contagious through human-to-human transmission (Ge et al., 2020). After the COVID-19 was first diagnosed in Wuhan of Hubei province, China, in late December 2019 (Zhu et al., 2020), it has been prevailed around the world in the past for two years, causing a large number of casualties, property losses, and a series of social problems, such as unemployment and economic downturn (Chen et al., 2020b; Lu et al., 2020). To some extent, the use of vaccines and the implementation of effective preventive measures hinder the spread of the COVID-19 while decrease mortality rate in the past year (WHO, 2021b). However, a recent variant, Omicron, has been suspected to be a more transmissible variant of the SARS-COV-2 virus (Callaway and Ledford, 2021). The World Health Organization (WHO) designated Omicron as a ‘variant of Concern’, triggering panic reactions from people across the world (WHO, 2021b). The COVID-19 once again poses a serious threat to people's health and socio-economic security, remains a dark cloud over the world's people (WHO, 2021c).
Numerous studies have found that the spread of the COVID-19 has been affected by meteorological factors, such as temperature, humidity, precipitation and wind speed (Chen et al., 2020a; Huang et al., 2020b; Liu et al., 2020b; Yang et al., 2021c). However, contradictory conclusions were found in the available studies (Álvaro, 2020). For example, Liu et al. (2020b) and Zhang et al. (2020b) found that the reduction of temperature and humidity was conducive to the spread of the COVID-19 in several cities in China. Bashir et al. (2020) indicated that the increase of temperature promoted the COVID-19 transmission in New York, USA. Yao et al. (2020) suggested that high temperature have small influences on the transmission of coronavirus in China's cities. Lélis da Silva et al. (2021) and Sangkham et al. (2021) found that the increase of high temperature facilitated community circulation of the COVID-19, while the opposite pattern were confirmed in Wuhan (Cai et al., 2020). Sarkodie and Owusu (2020) affirmed a positive relationship between relative humidity and the transmission of the COVID-19 in 20 countries, whereas Gunthe et al. (2020) and Jamil et al. (2020) found no correlation between them. Coşkun et al. (2021) indicated that wind speed promoted the increase of the newly-confirmed COVID-19 cases, but Rendana (2020) found an opposite pattern. According to explanation of Liu et al. (2020b), the inconsistent results about the relationship between meteorological factors and the COVID-19 transmission among these studies may be related to the different data sources used in their analysis. It is necessary to integrate all existing data sources for analysis to confirm whether a consistent effect of meteorological factors on the spread of the COVID-19 can be found.
The impact of meteorological factors on the spread of the COVID-19 may also change with season, geospatial scale and latitude (Chen et al., 2020a). This is because many meteorological factors change with spatial-temporal scales, especially for temperature, precipitation and light intensity (Hartmann, 1994). A decrease in temperature from low to high latitudes will increase the survival time of novel coronavirus in the environment, because lower temperature can enhance the structural order of lipids of virus envelope and improve stability (Audi et al., 2020; Moriyama et al., 2020; WMO, 2021). Variations in sunshine duration and intensity among different latitudes would affect not only temperature but also the amount of ultraviolet radiation (Rendana, 2020; Shokouhi et al., 2020; Rhodes et al., 2021). Changes in the intensity and timing of ultraviolet light affect the spread of the COVID-19 due to its bactericidal power (Sabino et al., 2020). The differences in precipitation among latitudes would cause the change of relative humidity (Hartmann, 1994). As novel coronavirus spreads in the air mainly depending on droplets, an increase in relative humidity would reduce the transmission distance of virus (Yang et al., 2021c). Similarly, impact of meteorological factors on the spread of the COVID-19 also differs obviously from season to season due to its properties of seasonal variations. For example, Yin et al. (2022) discovered that the effect of meteorological factors on the COVID-19 show seasonality in Brazil. Merow and Urban (2020) found that the COVID-19 decrease temporarily during summer, but increase in the autumn and peak in winter. The geospatial scale could influence the relationship between meteorological factors and the spread of the COVID-19 is because the change in meteorological factors are more obviously in large scale compared with small scale (Holton, 1973). However, at present, only a small number of scholars, including Yang et al. (2021c) and Méndez-Arriaga (2020), have verified the impact of meteorological factors on the spread of the COVID-19 varies with latitude and season by using data from China and Mexico, respectively. Liu et al. (2021) found that novel coronavirus infections and fatality rate were higher in colder climates than in warmer seasons by analysing the relationship between COVID-19 data and meteorological factors in 10 countries., Whether the results from these studies can be applied to other regions needs to be further validated as they are only examples in discrete parts of the world (Méndez-Arriaga, 2020; Liu et al., 2021; Yang et al., 2021c). Besides, it is still unclear whether geospatial scale affect the relationship between meteorological factors and the spread of the COVID-19.
In this study, we focus on to address two scientific questions: (1) whether meteorological factors have a consistent influence on virus transmission after integrating all existing data sources? (2) Do the impacts of meteorological factors on the spread of the COVID-19 vary with season, latitude and geospatial scale? In this study, we compiled 2813 articles from global databases (Google Scholar, Web of Science and PubMed databases) and conducted a meta-analysis. The results will help epidemiologists understand the relationship between meteorological factors and coronavirus transmission, and provide a new scientific basis for the development of effective control measures.
2. Data sources and methods
2.1. Data collection
We conducted a systematic search of all published articles related to relationship between meteorological factors and the COVID-19. The retrieval keywords used for COVID-19 included COVID, COVID-19, 2019-nCoV and SARS-CoV-2, while meteorological factors include temperature (daily maximum temperature, daily minimum temperature, and daily mean temperature), relative humidity, precipitation and average wind speed. After categorizing the keywords, we used two combinations [(COVID or COVID-19 or 2019-nCoV or SARS-CoV-2) and (Meteorological or Meteorology or Climate or Climatic or Weather or Atmosphere or Atmospheric or Temperature or Rain or Precipitation or Humidity or Wind or Rainfall)], to search all articles about the relationship between spread of the COVID-19 and meteorological factors since 2019 from Google Scholar, Web of Science and PubMed databases. The changes in the newly-confirmed COVID-19 cases and the COVID-19-related deaths were usually used to evaluate the strength of novel coronavirus transmission (Huang et al., 2020a; Wang et al., 2020b; Wu et al., 2020a). However, we found that most of the articles didn't focus on the COVID-19-related deaths in the process of data collection. This may be because the deaths did not effectively reflected changes in the COVID-19 transmission due to the intervention of medical treatment. Therefore, we did not use this indicator in subsequent analysis.
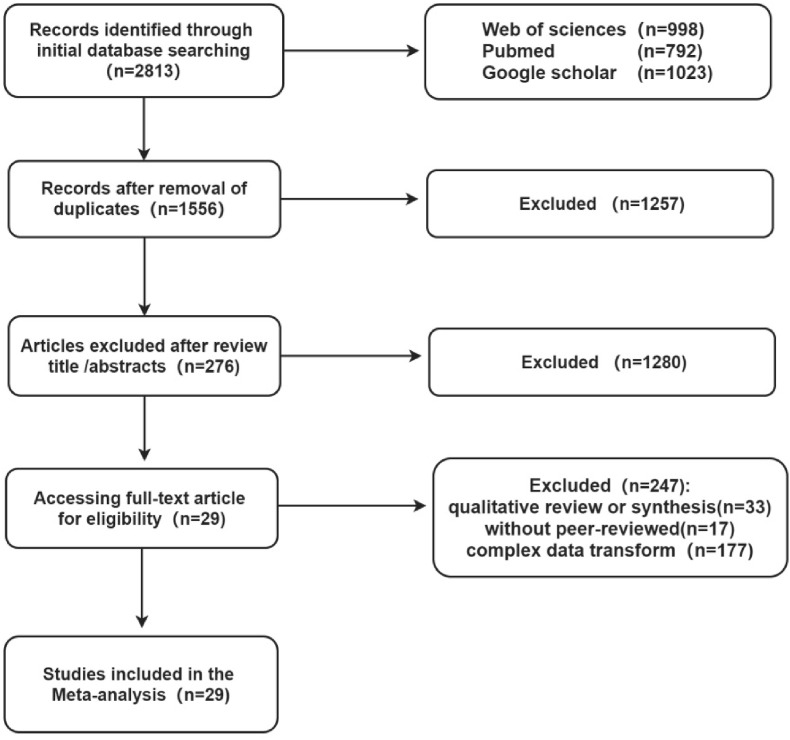
Both the inclusion and exclusion criterion were considered for article screening in this study. The inclusion criteria included: (1) The article collection period was from December 2019 to November 2021; (2) The correlation coefficient between meteorological factors and newly-confirmed COVID-19 cases was calculated in the article; (3) The articles have been peer reviewed; (4) The articles were journal published in English. The exclusion criteria included: (1) duplicate articles and the retention of articles with good quality and complete information; (2) articles without or were difficult to obtain the correlation coefficients; (3) articles with only one meteorological factor associated with the COVID-19; (4) review articles; (5) articles with the study length less than 15 days; (6) articles using only one city to represent one country in order to ensure that the area at the national scale was larger than that at the urban scale. Finally, 29 articles were obtained for further analysis (Fig. 1 and supporting information Table S1).
Fig. 1.
Flow diagram of article screening.
The information from published articles were extracted, including the article title, the first author, the published time, study period and length, study area, geographical latitude, meteorological factors and their correlation coefficients with the newly-confirmed COVID-19 cases. The geographical latitude was obtained using the Google Earth 6.2 software.
2.2. Statistical analysis
2.2.1. Transformation of effect values
The correlation coefficients was used as effect values to quantify the impact of meteorological factors on the spread of the COVID-19. In meta-analysis, the magnitude of the effect value was used as a standardized measure of the influence of the dependent variables on the independent variable. Harrison (2011) had proved that the correlation coefficient can be used as the effect value to effectively compare the statistical results of different studies without any transformation, because it represented the tightness between dependent and independent variables.
Both the Spearman or Pearson correlation coefficients between meteorological factors and the newly-confirmed COVID-19 cases from the screened articles were compiled in this study. All Spearman coefficients were then converted into Pearson coefficients according to the method proposed by Borenstein et al. (2009) in order to compare among different studies. In addition, all Pearson coefficients were transformed into Fisher's Z based on Fisher's transform to eliminate the influence of study length or sample size on the credibility of statistical results of meta-analysis. Each of the summary Z values were then converted back to CORs (summary r) (Equation (1), Equation (2), Equation (3), Equation (4)) (Hedges and Olkin, 1985). Where, r was the Pearson coefficients obtained from a given literature; n was the number of samples (Field, 2001).
| Equation (1) |
| Equation (2) |
| Equation (3) |
| Equation (4) |
2.2.2. Test of publication bias
The quality of literature retrieval will affect the credibility of the meta-analysis due to the publication bias (Peters et al., 2006). Articles with statistical significant results are more likely to be accepted and published, which results in fewer articles associated with statistically insignificant results in the database. As a result, the Meta-analysis results may be biased (Peters et al., 2006). Our study used the funnel plot to judge whether there are publication bias in the screened articles. If the funnel plot was basically symmetrical along the central axis, it is indicating that there was no publication bias in the screened articles, and the meta-analysis results were credible (Egger et al., 1997).
2.2.3. Heterogeneity test and subgroup analysis
Heterogeneity test was an effective method to evaluate whether the Summary r between meteorological factors and the spread of the COVID-19 of the screened articles was independent from each other. Heterogeneity among different articles suggested that the relationship of meteorological factors with the newly-confirmed COVID-19 cases was influenced by the geospatial scale, season and latitudes involved in this study, or other factors (Greenland, 1987). As suggested by Cochran (1954), Q statistic were used to test the heterogeneity among the screened articles. If parameter I 2 >50% and p-value ≤ 0.05 in Q statistical test, it was considered that heterogeneity existed among the screened articles (Lipsey and Wilson, 2001). After that, the sampling random effects model was used to analyze the impact of meteorological factors on the relationship of meteorological factors with the newly-confirmed COVID-19 cases based on all data. In contrast, if there was no heterogeneity, the fixed effects model was used. Then, in order to further verify whether the heterogeneity among articles is caused by geospatial scale, season and latitudes, the subgroup analysis in the meta-analysis were used. The geospatial scale included two subgroups: national and urban scales, while the seasons were also grouped into two subgroups: cold (Winter and Spring) and warm seasons (Summer and Autumn). This is due to the similarity in meteorological factors between winter and spring, and between autumn and summer. Additionally, the influencing mechanism of meteorological factors on the spread of respiratory virus was significantly different between winter and summer (Liu et al., 2021; Yang et al., 2021c; Yin et al., 2022). If the Summary r between meteorological factors and the newly-confirmed COVID-19 cases was significant differed among subgroups, it indicates that geospatial scale or season significantly could affect the relationship of meteorological factors with the newly-confirmed COVID-19 cases (Shi et al., 2019).
2.2.4. Meta-regression and generalized linear models
The meta-regression was used to analyze the impact of latitude on relationship between meteorological factors and the newly-confirmed COVID-19 cases (Equation (5)). In meta-regression, Summary r was the dependent variable while latitude was the independent variable. β i and β 0 were regression parameters. ε was the error. Larger R 2 and p-value ≤0.1 in regression indicated that latitude has the significant influence on the relationship of meteorological factors with the newly-confirmed COVID-19 cases. In this study, the reason of why we set the confidence level at 0.1 instead of 0.05 is that a higher confidence level can meet the requirements of meta-analysis because of the diversity and complexity of the research objects. It was worth noting that the latitude of a country was represented by a range. In the analysis, we divided the country into several latitude bands with 10°, and the Summary r of each latitude band was set to the same value, which was equal to the Summary r of this country.
| Equation (5) |
Additionally, the generalized linear models (GLMs) was used to analyze the synthetic effects of season, geospatial scale and latitude on the relationship between meteorological factors and the newly-confirmed COVID-19 cases. Heterogeneity test and meta-subgroup analysis were performed in Stata16.0 statistical software. Publication bias, Meta-regression and GLMs was conducted using ‘metafor’, ‘tidyverse’ and ‘leaps’ packages of R4.1.2 software, respectively (Viechtbauer, 2010; Lumley and Lumley, 2013; Wickham et al., 2019).
3. Results
3.1. Impacts of geospatial scale and season on the relationship between meteorological factors and the newly-confirmed COVID-19 cases
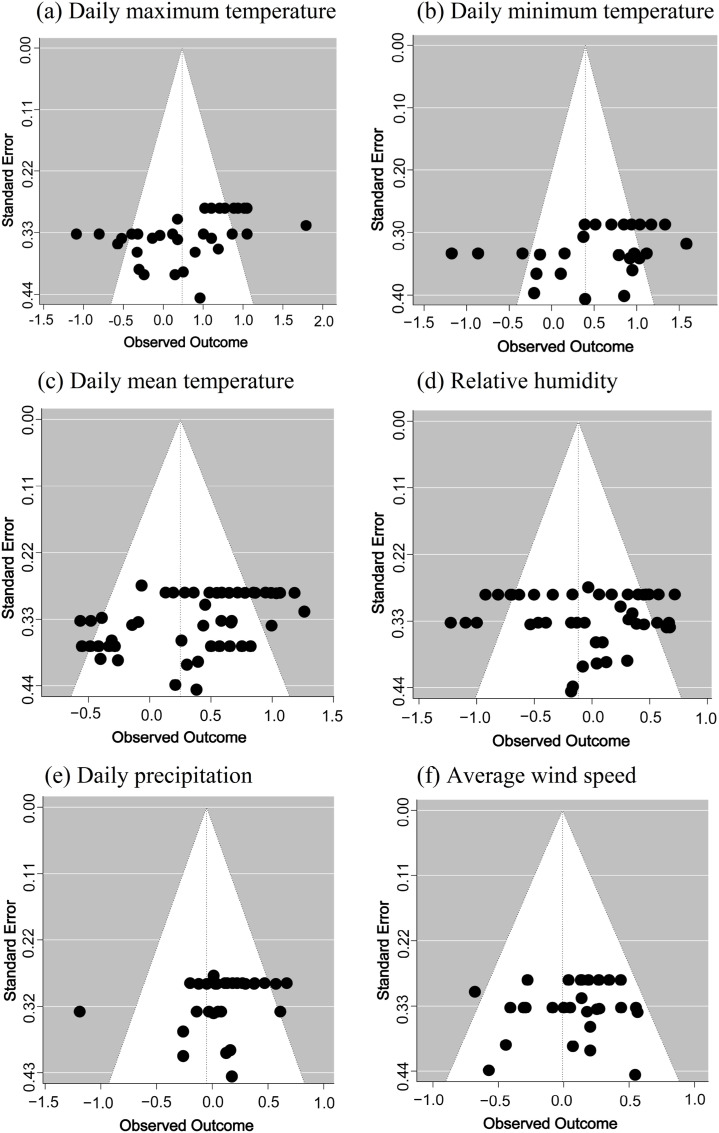
As showed in the funnel plot, the correlation coefficient between meteorological factors and the newly-confirmed COVID-19 cases (Summary r) was basically symmetric around the central axis, indicating that there was no obvious publication bias in the screened articles (Fig. 2 ). This suggested that the subsequent meta-analysis results in our study were credible.
Fig. 2.
Funnel plots of the screened articles about the relationship between meteorological factors and the newly-confirmed COVID-19 cases.
Heterogeneity test conformed that the Summary r of six meteorological factors were differed significantly among the screened articles (I 2 > 50%, p < 0.01) (Table 1 ). These suggested that the relationship between meteorological factors and the newly-confirmed COVID-19 cases may be affected by some factors (perhaps latitude, geospatial scale and season). The sampling random effects model showed that meteorological factors (daily maximum temperature, daily minimum temperature, daily mean temperature, daily precipitation, relative humidity and average wind speed) have no consistent influences on the newly-confirmed COVID-19 cases across all published articles (the absolute value of COR ≤ 0.07; p > 0.1) (Table 1).
Table 1.
Heterogeneity test for the relationship between meteorological factors and the newly-confirmed COVID-19 cases across all the screened articles. COR was the correlation coefficient between meteorological factors and the newly-confirmed COVID-19 cases by using the sampling random effects model based on all articles.
| Meteorological factors | Sampling random effects model |
Q statistical test |
Sample size (n) | |||
|---|---|---|---|---|---|---|
| COR | p-values | I2 (%) | Q | Qp-values | ||
| Daily maximum temperature | −0.07 | 0.46 | 94.68 | 593.01 | <0.001 | 29 |
| Daily minimum temperature | 0.07 | 0.64 | 96.88 | 792.13 | <0.001 | 23 |
| Daily mean temperature | 0.05 | 0.48 | 94.28 | 741.41 | <0.001 | 51 |
| Daily precipitation | −0.03 | 0.64 | 88.31 | 20.3.32 | <0.001 | 28 |
| Relative humidity | −0.02 | 0.75 | 94.62 | 717.05 | <0.001 | 43 |
| Average wind speed | 0.04 | 0.49 | 87.65 | 266.36 | <0.001 | 38 |
After the subgroup analysis of all meteorological factors, our results found that, unlike the analysis based on all data, several factors had the consistent influences on the newly-confirmed COVID-19 cases (Table 2 and Table 3 ). However, the direction of the effects (positive or negative) varied among subgroups. To be specific, in terms of the two seasonal subgroups (cold and warm seasons), heterogeneity test and sampling random effect model showed that the impacts of the daily maximum temperature and the daily minimum temperature on the newly-confirmed COVID-19 cases were completely different between cold and warm seasons. The increases of maximum temperature (COR = 0.13) and minimum temperature (COR = 0.39) increased the newly-confirmed COVID-19 cases in cold season, while the decreases of them were beneficial to the spread of the COVID-19 in warm season (the COR of maximum temperature = −0.27; the COR of minimum temperature = −0.36) (Table 2). No consistent influences were identified for the rest meteorological factors on the newly-confirmed COVID-19 cases between the two subgroups, indicating that their influences on the spread of the COVID-19 had not been affected by season (Table 2). Additionally, the absolute value of COR of these factors were not high, while their significance (p-values) were larger than 0.1 (Table 2). These suggested that these meteorological factors had no different impact on the newly-confirmed COVID-19 cases between cold and warm seasons.
Table 2.
Impact of season on relationship between meteorological factors newly-confirmed COVID-19 cases tested using the subgroup analysis. *p ≤ 0.1, **p ≤ 0.05, ***p ≤ 0.01.
| Meteorological factor | Cold season |
Warm season |
Heterogeneity test between the subgroup |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Sample size (n) | Heterogeneity test within the subgroup |
Sampling random effects model |
Sample size (n) | Heterogeneity test within the subgroup |
Sampling random effects model |
||||
| I2 (%)(p-value) | COR (95%CI) | p-value | I2 (%)(p-value) | COR (95%CI) | p-value | Q (p-value) | |||
| Daily maximum temperature | 14 | 94.57 (p < 0.01) | 0.13 (−0.13 to 0.39) | 0.32 | 15 | 93.05 (p < 0.01) | −0.27 (−0.52 to −0.02) | <0.05 | 4.85 (p<0.05) |
| Daily minimum temperature | 13 | 95.98 (p < 0.01) | 0.39 (0.08–0.70) | <0.01 | 10 | 95.02 (p < 0.01) | −0.36 (−0.74 to 0.01) | <0.1 | 9.17 (p<0.01) |
| Daily mean temperature | 26 | 93.99 (p < 0.01) | 0.08 (−0.13 to 0.28) | 0.48 | 25 | 93.88 (p < 0.01) | 0.02 (−0.14 to 0.18) | 0.83 | 0.19 (p = 0.67) |
| Relative humidity | 16 | 93.05 (p < 0.01) | −0.01 (−0.22 to 0.23) | 0.97 | 27 | 95.41 (p < 0.01) | −0.04 (−0.22 to 0.14) | 0.67 | 0.09 (p = 0.77) |
| Daily precipitation | 10 | 91.84 (p < 0.01) | −0.18 (−0.44 to 0.08) | 0.18 | 18 | 67.14 (p < 0.01) | 0.05 (−0.03 to 0.14) | 0.20 | 2.72 (p = 0.10) |
| Average wind speed | 15 | 84.95 (p < 0.01) | 0.10(-0.07 to 0.27) | 0.25 | 23 | 88.42 (p < 0.01) | −0.01 (−0.13 to 0.12) | 0.94 | 0.96 (p = 0.33) |
Table 3.
Impact of geospatial scale on relationship between meteorological factors and the newly-confirmed COVID-19 cases tested using the subgroup analysis. *p ≤ 0.1, **p ≤ 0.05, ***p ≤ 0.01.
| Meteorological factor | National scale |
Urban scale |
Heterogeneity test between the subgroup |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Sample size (n) | Heterogeneity test within the subgroup |
Sampling random effects model |
Sample size (n) | Heterogeneity test within the subgroup |
Sampling random effects model |
||||
| I2 (%)(p-value) | COR (95%CI) | p-value | I2 (%)(p-value) | COR (95%CI) | p-value | Q (p-value) | |||
| Daily maximum temperature | 12 | 97.49 (p < 0.01) | −0.08 (−0.48 to 0.33) | 0.71 | 17 | 87.02 (p < 0.01) | −0.07 (−0.24 to 0.10) | 0.43 | 0.01 (p = 0.97) |
| Daily minimum temperature | 10 | 98.56 (p < 0.01) | 0.08 (−0.47 to 0.63) | 0.78 | 13 | 92.78 (p < 0.01) | 0.06 (−0.22 to 0.34) | 0.67 | 0.01 (p = 0.96) |
| Daily mean temperature | 8 | 95.26 (p < 0.01) | 0.06 (−0.31 to 0.43) | 0.76 | 43 | 94.15 (p < 0.01) | 0.05 (−0.10 to 0.19) | 0.53 | 0.01 (p = 0.95) |
| Relative humidity | 11 | 96.90 (p < 0.01) | −0.33 (−0.69 to 0.03) | <0.1 | 32 | 89.33 (p < 0.01) | 0.09 (−0.02 to 0.21) | 0.11 | 4.77 (p < 0.05) |
| Daily precipitation | 9 | 95.05 (p < 0.01) | −0.13 (−0.44 to 0.18) | 0.42 | 19 | 42.03 (p < 0.05) | 0.02 (−0.04 to 0.09) | 0.46 | 0.89 (p = 0.34) |
| Average wind speed | 9 | 92.69 (p < 0.01) | 0.14 (−0.15 to 0.43) | 0.35 | 29 | 81.45 (p < 0.01) | −0.01 (−0.09 to 0.10) | 0.93 | 0.75 (p = 0.39) |
In terms of the two subgroups of the geospatial scale (national and urban scales), our results showed that the impact of the relative humidity on the newly-confirmed COVID-19 cases was significantly different between national and urban scales (p < 0.05) (Table 3). Relative humidity had a significant negative correlation with the spread of the COVID-19 at the national scale (COR = −0.33), while had no impact at the urban scale (COR = 0.09). The rest of relationships between meteorological factors and newly-confirmed COVID-19 cases have no significant difference between the two subgroups, indicating that their influences had not been affected by geospatial scale (Table 3).
3.2. Relationship between meteorological factors and the newly-confirmed COVID-19 cases varied among latitudes
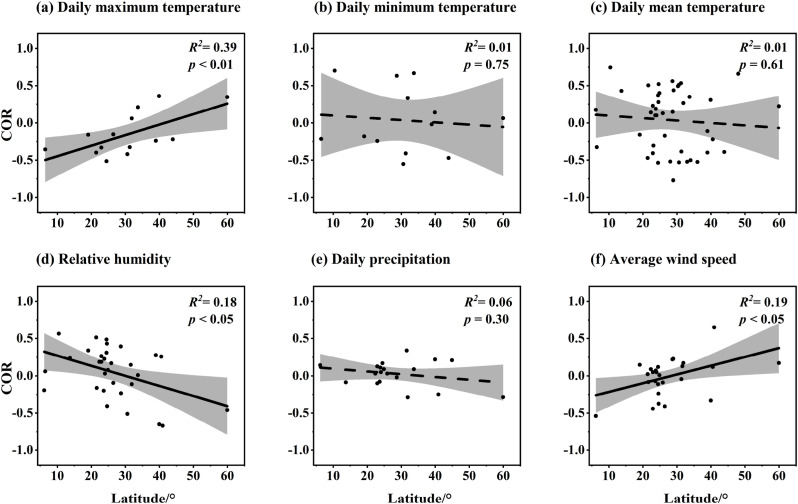
The meta-regression results showed that the positive effects of daily maximum temperature (R 2 = 0.39; p < 0.01) and wind speed (R 2 = 0.19; p < 0.05) on the newly-confirmed COVID-19 cases were significantly increased with the latitude, while the negative effect of relative humidity was decreased (R 2 = 0.18; p < 0.05). The impacts of other meteorological factors on the spread of the COVID-19 were not affected by latitude (Fig. 3 ).
Fig. 3.
Change in the relationship between meteorological factors and the newly-confirmed COVID-19 cases along the latitudes.
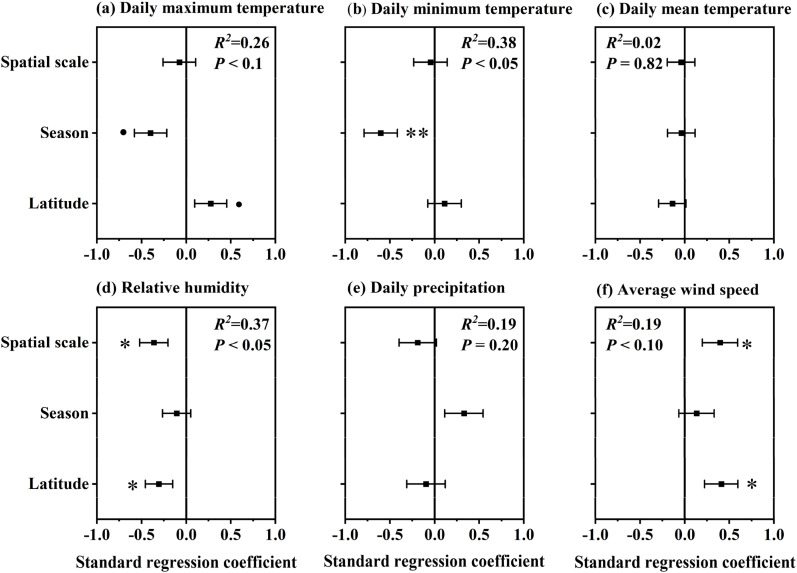
3.3. The synthetic effect of season, geospatial scale and latitude on the relationship between meteorological factors and the newly-confirmed COVID-19 cases
GLMs results showed that the synthetic effect of season, geospatial scale and latitude on the relationship between meteorological factors and the newly-confirmed COVID-19 cases were varied (Fig. 4 ). Specifically, they affected the relationship of the daily maximum temperature (R 2 = 0.26), daily minimum temperature (R 2 = 0.38), relative humidity (R 2 = 0.37) and the average wind speed (R 2 = 0.19) with the newly-confirmed COVID-19 cases (p < 0.1), while had not contributed on the impacts’ of daily mean temperature and precipitation (p > 0.1). Additionally, influences of these three variables on the relationship between meteorological factors and the newly-confirmed COVID-19 cases were not equalized (Fig. 4). The impact of daily maximum temperature on the spread of the COVID-19 were mainly affected by season and latitude, while the impact of daily minimum temperature was mainly affected by season, but the influences of relative humidity (p < 0.01) and wind speed were both mainly determined by geospatial scale and latitude (p < 0.05). Geospatial scale has greater influence on the relationship of relative humidity and wind speed with the newly-confirmed COVID-19 cases than latitude and season.
Fig. 4.
The synthetic effect of season, geospatial scale and latitude on the relationship between meteorological factors and the newly-confirmed COVID-19 cases, which was tested using GLMs. •p < 0.1, *p < 0.05, **p < 0.01.
4. Discussion
4.1. Existing studies are inconsistent on the impact of meteorological factors on the COVID-19 transmission
Our results showed that, none of the six meteorological factors had a consistent influence on the newly-confirmed COVID-19 cases across all selected articles. This was inconsistent with the many proven conclusions that meteorological factors can play a role in the spread of the epidemic in a certain period of time or in a certain city or country (He et al., 2020; Jamshidi et al., 2020; Sarkodie and Owusu, 2020; Yang et al., 2021c). Our results suggested the influence of meteorological factors on the newly-confirmed COVID-19 cases confirmed COVID-19 cases varied greatly among existing studies, and there was no consistent conclusion, which was probably because the novel coronavirus was a very intelligent living organism (Almeida et al., 2018; Méndez-Arriaga, 2020; Yang et al., 2021c). The strong environmental adaptability of novel coronavirus make the main meteorological determinants on their survival or transmission to vary among different period or different regions (Merow and Urban, 2020; Yang et al.,2021a, 2021c). For example, in arid environments, an increase in relative humidity promoted novel coronavirus transmission, but limited it in humid region (Merow and Urban, 2020; Yang et al., 2021c). The reason for this difference was that the increase in relative humidity allowed virus-carrying droplets to rapidly fuse with other droplets into larger droplets in humid regions, which then quickly settle to the ground under the influence of gravity and air resistance, limiting the spread of the COVID-19 (Seminara et al., 2020; WMO, 2021). In contrast, the intense evaporation and high temperatures negatively affected viral surface protein and lipid membranes through water loss in arid regions. The increased humidity in the atmosphere would mitigate the water loss, thereby increasing the likelihood of survival and transmission of the COVID-19 (Audi et al., 2020; Moriyama et al., 2020).
On the other hand, our results suggested that the impact of meteorological factors on the COVID-19 transmission might be influenced by other factors, such as season, geospatial scale, latitude, non-pharmacological interventions and vaccine cultivation (Baniasad et al., 2021; Yin et al., 2022). For examples, non-pharmacological interventions, including social distancing, stay-home order, etc., may have weakened the relationship between meteorological factors and COVID-19 spread (Badr et al., 2020; Kraemer et al., 2020; Duhon et al., 2021). Besides, some studies have argued the influence of meteorological factors on COVID-19 transmission was changing over the course of the epidemic (WMO, 2021). The influence was limited in the early stage of the pandemic because almost everyone is susceptible (Baker et al., 2020). These factors may to some extent lead to inconsistencies across the literature between the relationship between meteorological factors and the spread of the COVID-19. Direct analysis of the relationship between meteorological factors and the spread of the COVID-19 without considering these influencing factors may lead to biased results. As shown in this study, we analyzed all selected articles and found there were no consistent relationships of the six meteorological factors with the newly-confirmed COVID-19 cases. These conclusions, if used without considering other factors (e.g. non-pharmacological interventions and vaccine cultivation), may mislead the government and epidemic control authorities to formulate less effective prevention and control measures.
4.2. Relationships of daily maximum temperature and daily minimum temperature with the newly-confirmed COVID-19 cases were affected by season
The daily maximum temperature and daily minimum temperature showed completely opposite effects on the newly-confirmed COVID-19 cases between the two seasons after grouping the selected articles into cold and warm seasons by study period. The increases of daily maximum temperature and daily minimum temperature during cold season were conducive to promoting the spread of the COVID-19. This is probably because, in cold season, the novel coronavirus change lipids on envelope from liquid to solid under low temperature conditions, which subsequently made the virus less susceptible to water loss or other environmental stresses to causing death (Yao et al., 2020). The virus can survive longer at lower temperatures (Merow and Urban, 2020). At the cold season, a small increase of temperature will extend the transmission distance of the virus due to speed up the activity of small particles in the atmosphere, resulting in a rise of the infectious rate (Audi et al., 2020; Gupta and Pradhan, 2020; Yang et al., 2021c). Besides, many studies have found that the rising temperatures promoted the spread of the COVID-19 may be related to increased human outdoor activities (Merow and Urban, 2020; Xie and Zhu, 2020; Bourdrel et al., 2021). At the cold season, days with high temperature usually means it was the shining bright days, which would induce people to increase their outdoor activities. This subsequently increased the probability of novel coronavirus infection between humans (Bashir et al., 2020; Xie and Zhu, 2020). Conversely, the transmission and infection abilities of virus in the warm seasons decreased mainly due to higher temperature, especially the maximum temperature can cause rapid dehydration and death of viruses due to their simple structure and lack of hardened protective tissues (Demongeot et al., 2020; Guo et al., 2021). According to Chin et al. (2020) study, the survival time of the novel coronavirus had not exceeded 24 h in an environment with temperatures above 37 °C. This in turn resulted in a negative relationship between temperature and virus transmission (Casanova et al., 2010).
Except for daily maximum temperature and daily minimum temperature, the impacts of other meteorological factors on novel coronavirus transmission were not affected by season. Numerous studies have shown that viruses were more sensitive to ambient temperature than other meteorological factors, especially maximum and minimum temperatures (Marr et al., 2019; Pani et al., 2020; Zhang et al., 2020a), because these two factors reflected the temperature extremes that could affect more on the activity of viral proteins (Lowen et al., 2007). The mean temperature was included in these two extreme temperatures, the variation of it would not significantly affect the spread of COVID-19 (Marr et al., 2019; Zhang et al., 2020a). The influences of relative humidity, precipitation and wind speed on the spread of COVID-19 had not differed significantly between the cold and warm seasons, which may be because these factors have not varied significantly between the two seasons on a global scale (Barry and Chorley, 2009). Specifically, in a certain region, they changed between the two seasons. But globally, they were higher in winter than in summer in some areas, such as the Mediterranean climate zones. In some areas like monsoon regions or continental climate zones, however, they showed an opposite pattern (Summer > Winter). When all data were gathered together to analyze the relationship between meteorological factors and the spread of the COVID-19, the countervailing among different data sources would result in no variations about relationship between cold and warm seasons (Shokouhi et al., 2020; Byun et al., 2021; Liu et al., 2021).
4.3. Only the relationship between relative humidity and the newly-confirmed COVID-19 cases was affected by geospatial scale
Among the six meteorological factors, only relationship of relative humidity with the newly-confirmed COVID-19 cases was affected by geospatial scale. The relative humidity had no effect on the spread of the COVID-19 at the urban scale, whereas the increase of relative humidity limited coronavirus transmission at the national scale. This result was similar to the conclusion of many studies in a given country (Jamshidi et al., 2020; Wu et al., 2020b; Byun et al., 2021). For example, Wang et al. (2021) and Ward et al. (2020) confirmed that the increase of relative humidity were hampering the spread of the COVID-19 in China, America and Australia, respectively. This result may be due to the fact that relative humidity played more roles in limitation to coronavirus transmission than that in promotion (Lowen et al., 2007; Chan et al., 2011). This limitation would become more apparent with the increases of the geospatial scale (Wu et al., 2020b). On the contrary, the impacts of other meteorological factors on the COVID-19 transmission had not changed with geospatial scale, which may be related to the differentiated contribution of these factors to virus survival or transmission among different regions or periods (Merow and Urban, 2020). Many studies have shown that the impacts of temperature, precipitation and wind speed on the spread of the COVID-19 varied from city to city, or among different times (Byun et al., 2021; Guo et al., 2021; Yang et al., 2021c; Yin et al., 2022). For example, Yang et al. (2021c) found that low temperature in coastal cities was conducive to the spread of the COVID-19, while had no significant impact in inland cities. The most important reason of that the impact of meteorological factors on the coronavirus transmission was not affected by spatial scale may be caused by the strong environmental adaptation of the virus (Holland and Domingo, 1998; Álvaro, 2020; Yang et al., 2021c). Existing studies have proved that novel coronavirus had higher variability than MERS and SARS (Chen, 2020; Liu et al., 2020a; Méndez-Arriaga, 2020). The number of genome sequence of novel coronavirus had changed more than 8 million times since it was diagnosed (https://www.gisaid.org/). The higher variability of the novel coronavirus indicated that its environmental adaptation might vary among different regions and across different times (Chen, 2020). This would lead to inconsistent results from different studies about the relationship between meteorological factors and the spread of the COVID-19. Therefore, in the process of meta-analysis, the inconsistent relationship between different studies would cause that the impact of meteorological factors on the spread of the COVID-19 have not been affected by geospatial scale due to the mutual cancellation.
Another reason for the impacts of most meteorological factors on coronavirus transmission were independent from geospatial scale may be related to effective human control of the epidemic (Ficetola and Rubolini, 2021). In the past two years of epidemic management, most countries have adopted strict measures when the COVID-19 has been diagnosed in a city, such as the community lockdown, home quarantine, and traffic control, to contain it within a small geographical space (Hellewell et al., 2020). For example, China has even managed to contain the epidemic within a community or township through community lockdown (Lin et al., 2020; Liu et al., 2020b; Wang et al., 2020a). These processes have resulted in much of the current published research on the epidemic focusing on the urban scale (Bashir et al., 2020; He et al., 2020; Méndez-Arriaga, 2020; Ward et al., 2020; Xie and Zhu, 2020; Yao et al., 2020; Zhang et al., 2020a; Yang et al., 2021a). Few articles have been published at the national scale (Gupta and Pradhan, 2020; Sarkodie and Owusu, 2020; Wu et al., 2020b; Zhu et al., 2020). In the meta-analysis, such bias in the number of published articles may also lead to the relationship concerned in this study not changing with geographical scale.
4.4. Influences of daily maximum temperature, relative humidity and wind speed on the newly-confirmed COVID-19 cases increased with latitude
The role of daily maximum temperature in promoting the COVID-19 transmission increased with latitude. This finding is consistent with the research results of many scholars (Laird et al., 2020; Liu et al., 2021; Rhodes et al., 2021). This may be related to the temperature range that is favorable for novel coronavirus. According to Bukhari et al. (2020) reports, the favorite temperature range for survival and transmission of the novel coronavirus ranged from 0 to 17 °C. Especially in winter when the COVID-19 pandemic was widespread around world, the annual mean maximum temperature in low latitude areas (20°–30° N as an example) was about 20 °C, which was much higher than that in high latitude areas (30°–40° N as an example) (0 °C) (Peel et al., 2007). The maximum temperatures at low and high latitudes lied on both sides of the virus's favorite temperature range, respectively. The increase of maximum temperature at low latitudes will push the ambient temperature away from virus' favorite range, while that at high latitudes will drew the ambient temperature closer to virus' favorite range. This process will become more pronounced with latitude, and as a result caused the increasing positive relationship between daily maximum temperature and coronavirus transmission with latitude (Lin et al., 2020; Yang et al., 2021c).
Our results showed that the inhibitory effect of relative humidity on COVID-19 transmission increased with latitude. This was probably because an increase in relative humidity reduced the transmission distance of virus in atmosphere (Tamerius et al., 2013; Deyle et al., 2016). Especially during the cold season, the high latitudes have higher relative humidity than the low latitudes due to lower temperatures, less evaporation, and higher snow cover. Under the condition of the same increase of relative humidity, the respiratory droplet carrying the virus had a fast settlement rate in high latitudes compared with low latitudes, thus preventing the transmission of novel coronavirus (Chan et al., 2011; Tamerius et al., 2011). In addition, as suggested by Lowen et al. (2007), low relative humidity can increase respiratory infections of virus. Breathing dry air can lead to epithelial damage and reduced the clearance of mucociliary, leading to more susceptible hosts to respiratory viruses (Wang et al., 2021; Yang et al., 2021c; Yin et al., 2022). Therefore, a dry environment has a higher transmission rate than a humid environment (Chan et al., 2011; Gustin et al., 2015). The role of wind speed in promoting COVID-19 transmission increased with latitude. This finding was consistent with the opinions of many scholars (Rios et al., 2020; Cao et al., 2021; Hridoy et al., 2021). Controlled by the continental climate, the average wind speed at high latitudes was higher than that at low latitudes, especially in winter and spring when the epidemic was at its peak (Tokumaru et al., 2010). The increase in wind speed was conducive to the spread of viruses in the air over a longer distance, further promoting transmission (Coccia, 2021).
4.5. Season, geospatial scale and latitude had unbalanced influences on relationship between meteorological factors and the newly-confirmed COVID-19 cases
Compared with mean temperature and precipitation, the impacts of the daily maximum temperature, daily minimum temperature, relative humidity and the average wind speed on the spread of the COVID-19 were more likely to be affected by the synthetic effects of season, geospatial scale and latitude. This result was similar with most previous studies (Almeida et al., 2018; Jamshidi et al., 2020; Merow and Urban, 2020; Shokouhi et al., 2020). This could be due to that daily mean temperature had not affected the survival time or mortality of the virus relative to maximum and minimum temperatures (Gupta and Pradhan, 2020). Precipitation only contributed indirectly to the transmission or survival of the coronavirus via changing relative humidity, maximum or minimum temperature (Sarkodie and Owusu, 2020).
In terms of the three meteorological factors that are more closely related to the spread of the COVID-19: relative humidity, maximum and minimum temperatures (Wu et al., 2020b), our results showed that the relationship of maximum and minimum temperatures with the COVID-19 transmission were more susceptible to season, while relative humidity's was more affected by latitude and geospatial scale. This result indicated that the magnitude of impacts of season, geospatial scale and latitude on relationship of meteorological factors with virus transmission were not unevenly distributed. The seasonal variations of maximum and minimum temperatures were much higher than that of latitude and spatial scale (Tamerius et al., 2013; Dave and Lee, 2019). Although temperature varied widely from equator to the north or south poles, the epidemic had been more concentrated between 20° and 60° north-south latitude band in the past two years because the vast majority of planet's people live in these bands (Shokouhi et al., 2020). The changes in temperature within this range did not vary as much as that between cold and warm seasons. However, the latitude variation was greater than the seasonal variation for relative humidity, especially in winter and spring when epidemic outbreaks were more concentrated. The increase in relative humidity with latitude will help prevent the transmission of novel coronavirus in the atmosphere (Tamerius et al., 2013).
5. Conclusions and remarking
Our results showed that the novel coronavirus had a strong environmental adaptability, and can always adapt to adverse meteorological condition to sustain transmission. The daily maximum temperatures and minimum temperatures promoted the spread of the COVID-19 in the cold season, but suppressed the transmission in the warm season. The effect of relative humidity on the virus transmission has been influenced by geospatial scales. The constraints of relative humidity and the promotions of maximum temperatures and wind speed on the spread of the COVID-19 increased with latitude, respectively. In addition, we found that the impacts of season, geospatial scale and latitude on the relationship of meteorological factors with the COVID-19 transmission were not unevenly distributed. However, at present, many studies have proved that meteorological factors, especially maximum temperature, minimum temperature, relative humidity and wind speed, have obviously influences on the novel coronavirus transmission (Chen et al., 2020a; Liu et al., 2020b; Pani et al., 2020). However, in most cases, the results obtained by such studies were contradictory, because they were mostly drawn on a specific region, such as a city or a country (Almeida et al., 2018; Méndez-Arriaga, 2020; Yang et al., 2021c). When formulating the urban level preventive measures, it was very accurate to rely on local research results, because it did not take into account the spatial-temporal validity of relationship between meteorological factors and the COVID-19 transmission. We are very fortunate in that the vast majority of countries and cities are operating in this way.
There are few limitations in this study. The effects of different strains (Alpha, Beta, Gamma, Delta and Omicron mutants), vaccine type, vaccination rates, socio-economic determinants and air pollutants etc. were not considered in this study when determining the relationship between meteorological factors and newly-confirmed COVID-19 cases Existing studies have found that the impacts of meteorological factors, such as temperature and relative humidity, on the survival and reproduction varied among different mutants (Seligmann et al., 2020; Kulkarni et al., 2021; Sharif et al., 2021). People's immunity to different mutants varied after vaccination (Koirala et al., 2020), which may attenuate the impact of meteorological factors on the spread of the COVID-19. Socio-economic determinants, such as government interventions, local health system capacity, demographic structure, GDP, transport infrastructure and educational qualifications, may affect the impact of meteorological factors on virus transmission by influencing the awareness of epidemic prevention and control, virus expansion and treatment of COVID-19 patients (Dowd et al., 2020; Huang et al., 2020a; Legido-Quigley et al., 2020; Lian et al., 2020; Yang et al., 2021b; Liang et al., 2022). Air pollution can promote novel coronavirus transmission as it can enhance respiratory infections due to the prolongation of the aerosol transmission of viruses, and also to enhance the ability of viruses to invade airway epithelial cells (Domingo and Rovira, 2020; Woodby et al., 2021; Marquès and Domingo, 2022). The small atmospheric particulate matters might act as a medium for novel coronavirus transmission (Morawska and Milton, 2020; Setti et al., 2020). Additionally air pollution can also affect the spread of novel coronavirus by changing the meteorological environment, such as increasing near-surface temperature while reducing ultraviolet radiation (Bourdrel et al., 2021; WMO, 2021).
Moreover, the peer-reviewed 2800 records were initially screened in our study, but only 29 studies were eventually selected and introduced in the meta-analysis. As these final studies were distributed in 19 countries and 41 areas, covered many parts of the globe including China, America, Russia, India, Brazil et al., the meta-analysis results can reveal the relationship between meteorological factors and novel coronavirus transmission. However, according to statistical standards, 29 studies represented only 1/100 of the initial peer-reviewed records, which was a small sample. Using these to analyze the connection between the virus transmission and meteorological factors across the global scale may reduce the reliability and objectivity of the conclusion.
At the same time, although data points in cold and warm seasons were evenly distributed in 29 studies, they were mostly concentrated in latitude 20–40° N and mainly distributed at urban scale. These biases may also affect the reliability and objectivity of the conclusion. Much more research efforts are required to fully uncover the relationship between meteorological factors and coronavirus transmission. In addition, our results found that a slight rise of temperatures in cold season increased coronavirus transmission. This was contrary to some current studies which suggested that cooler temperatures in winter were more conducive to novel coronavirus transmission and reproduction (Liu et al., 2020b; Méndez-Arriaga, 2020; Sarkodie and Owusu, 2020). On the premise that virus can survive for a long time in the winter, the large number of the COVID-19 outbreaks may be partly caused by that a small rise in temperature increased the transmission capacity of the virus in the atmosphere. Therefore, we suggest that in winter, especially on sunny days, people should reduce outdoor activities or wear masks when outside to reduce the infection risk.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was supported by National Natural Science Foundation of China (No. 41871031 and 31860111), and General Scientific Research Project of Zhejiang Provincial Department of Education (Y202146266). We thank Dr. Yanju Liu at the Newcastle University for the assistance with English language and grammatical editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2022.113297.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Almeida A., Codeço C., Luz P.M. Seasonal dynamics of influenza in Brazil: the latitude effect. BMC Infect. Dis. 2018;18(1):1–9. doi: 10.1186/s12879-018-3484-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Álvaro B.-R. The effect of climate on the spread of the COVID-19 pandemic: a review of findings, and statistical and modelling techniques. Prog. Phys. Geogr. 2020;44(5):591–604. [Google Scholar]
- Audi A., AlIbrahim M., Kaddoura M., Hijazi G., Yassine H.M., Zaraket H. Seasonality of respiratory viral infections: will COVID-19 follow suit? Front. Public Health. 2020;8:576. doi: 10.3389/fpubh.2020.567184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H.S., Du H., Marshall M., Dong E., Squire M.M., Gardner L.M. Association between mobility patterns and COVID-19 transmission in the USA: a mathematical modelling study. Lancet Infect. Dis. 2020;20(11):1247–1254. doi: 10.1016/S1473-3099(20)30553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker R.E., Yang W., Vecchi G.A., Metcalf C.J.E., Grenfell B.T. Susceptible supply limits the role of climate in the early SARS-CoV-2 pandemic. Science. 2020;369(6501):315–319. doi: 10.1126/science.abc2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baniasad M., Mofrad M.G., Bahmanabadi B., Jamshidi S. COVID-19 in Asia: transmission factors, re-opening policies, and vaccination simulation. Environ. Res. 2021;202:111657. doi: 10.1016/j.envres.2021.111657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry R.G., Chorley R.J. Routledge; London: 2009. Atmosphere, Weather and Climate. [Google Scholar]
- Bashir M.F., Ma B., Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728:138835. doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M., Hedges L.V., Higgins J.P., Rothstein H.R. Wiley; Chichester: 2009. Introduction to Meta-Analysis. [Google Scholar]
- Bourdrel T., Annesi-Maesano I., Alahmad B., Maesano C.N., Bind M.-A. The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies. Eur. Respir. Rev. 2021;30(159) doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukhari Q., Massaro J.M., D’agostino R.B., Khan S. Effects of weather on coronavirus pandemic. Int. J. Environ. Res. Publ. Health. 2020;17(15):5399. doi: 10.3390/ijerph17155399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byun W.S., Heo S.W., Jo G., Kim J.W., Kim S., Lee S., Park H.E., Baek J.-H. Is coronavirus disease (COVID-19) seasonal? A critical analysis of empirical and epidemiological studies at global and local scales. Environ. Res. 2021;196:110972. doi: 10.1016/j.envres.2021.110972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Y., Huang T., Liu X., Xu G. The effects of “Fangcang, Huoshenshan, and Leishenshan” hospitals and environmental factors on the mortality of COVID-19. PeerJ. 2020;8 doi: 10.7717/peerj.9578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaway E., Ledford H. How bad is Omicron? What scientists know so far. Nature. 2021;600(7888):197–199. doi: 10.1038/d41586-021-03614-z. [DOI] [PubMed] [Google Scholar]
- Cao W., Chen C., Li M., Nie R., Lu Q., Song D., Li S., Yang T., Liu Y., Du B. Important factors affecting COVID-19 transmission and fatality in metropolises. Publ. Health. 2021;190:e21. doi: 10.1016/j.puhe.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76(9):2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan K.-H., Peiris J.M., Lam S., Poon L., Yuen K., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv. Virol. 2011;2011:7. doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B., Liang H., Yuan X., Hu Y., Xu M., Zhao Y., Zhang B., Tian F., Zhu X. 2020. Roles of Meteorological Conditions in COVID-19 Transmission on a Worldwide Scale. MedRxiv. [Google Scholar]
- Chen J. Pathogenicity and transmissibility of 2019-nCoV—a quick overview and comparison with other emerging viruses. Microb. Infect. 2020;22(2):69–71. doi: 10.1016/j.micinf.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin A.W., Chu J.T., Perera M.R., Hui K.P., Yen H.-L., Chan M.C., Peiris M., Poon L.L. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microb. 2020;1(1):e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. The effects of atmospheric stability with low wind speed and of air pollution on the accelerated transmission dynamics of COVID-19. Int. J. Environ. Stud. 2021;78(1):1–27. [Google Scholar]
- Cochran W.G. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–129. [Google Scholar]
- Coşkun H., Yıldırım N., Gündüz S. The spread of COVID-19 virus through population density and wind in Turkey cities. Sci. Total Environ. 2021;751:141663. doi: 10.1016/j.scitotenv.2020.141663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dave K., Lee P.C. Global geographical and temporal patterns of seasonal influenza and associated climatic factors. Epidemiol. Rev. 2019;41(1):51–68. doi: 10.1093/epirev/mxz008. [DOI] [PubMed] [Google Scholar]
- Demongeot J., Flet-Berliac Y., Seligmann H. Temperature decreases spread parameters of the new covid-19 case dynamics. Biology. 2020;9(5):94. doi: 10.3390/biology9050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deyle E.R., Maher M.C., Hernandez R.D., Basu S., Sugihara G. Global environmental drivers of influenza. Proc. Natl. Acad. Sci. Unit. States Am. 2016;113(46):13081–13086. doi: 10.1073/pnas.1607747113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domingo J.L., Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020;187:109650. doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd J.B., Andriano L., Brazel D.M., Rotondi V., Block P., Ding X., Liu Y., Mills M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(18):9696–9698. doi: 10.1073/pnas.2004911117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhon J., Bragazzi N., Kong J.D. The impact of non-pharmaceutical interventions, demographic, social, and climatic factors on the initial growth rate of COVID-19: a cross-country study. Sci. Total Environ. 2021;760:144325. doi: 10.1016/j.scitotenv.2020.144325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ficetola G.F., Rubolini D. Containment measures limit environmental effects on COVID-19 early outbreak dynamics. Sci. Total Environ. 2021;761:144432. doi: 10.1016/j.scitotenv.2020.144432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A.P. Meta-analysis of correlation coefficients: a Monte Carlo comparison of fixed-and random-effects methods. Psychol. Methods. 2001;6(2):161. doi: 10.1037/1082-989x.6.2.161. [DOI] [PubMed] [Google Scholar]
- Ge H., Wang X., Yuan X., Xiao G., Wang C., Deng T., Yuan Q., Xiao X. The epidemiology and clinical information about COVID-19. Eur. J. Clin. Microbiol. Infect. Dis. 2020;39(6):1011–1019. doi: 10.1007/s10096-020-03874-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Quantitative methods in the review of epidemiologic literature. Epidemiol. Rev. 1987;9(1):1–30. doi: 10.1093/oxfordjournals.epirev.a036298. [DOI] [PubMed] [Google Scholar]
- Gunthe S.S., Swain B., Patra S.S., Amte A. On the global trends and spread of the COVID-19 outbreak: preliminary assessment of the potential relation between location-specific temperature and UV index. J. Public Health. 2020:1–10. doi: 10.1007/s10389-020-01279-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo C., Bo Y., Lin C., Li H.B., Zeng Y., Zhang Y., Hossain M.S., Chan J.W., Yeung D.W., Kwok K.-O. Meteorological factors and COVID-19 incidence in 190 countries: an observational study. Sci. Total Environ. 2021;757:143783. doi: 10.1016/j.scitotenv.2020.143783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A., Pradhan B. 2020. Impact of Daily Weather on COVID-19 Outbreak in India. MedRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustin K.M., Belser J.A., Veguilla V., Zeng H., Katz J.M., Tumpey T.M., Maines T.R. Environmental conditions affect exhalation of H3N2 seasonal and variant influenza viruses and respiratory droplet transmission in ferrets. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0125874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison F. Getting started with meta-analysis. Methods Ecol. Evol. 2011;2(1):1–10. [Google Scholar]
- Hartmann D.L. Academic press; San Diego: 1994. Global Physical Climatology. [Google Scholar]
- He Z., Chin Y., Huang J., He Y., Akinwunmi B.O., Yu S., Zhang C.J., Ming W.-k. MedRxiv; 2020. Meteorological Factors and Domestic New Cases of Coronavirus Disease (COVID-19) in Nine Asian Cities: A Time-Series Analysis. [Google Scholar]
- Hedges L.V., Olkin I. Academic press; San Diego: 1985. Statistical Methods for Meta-Analysis. [Google Scholar]
- Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., Munday J.D., Kucharski A.J., Edmunds W.J., Sun F. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Global Health. 2020;8(4):e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holland J., Domingo E. Origin and evolution of viruses. Virus Gene. 1998;16(1):13–21. doi: 10.1023/a:1007989407305. [DOI] [PubMed] [Google Scholar]
- Holton J.R. An introduction to dynamic meteorology. Am. J. Phys. 1973;41(5):752–754. [Google Scholar]
- Hridoy A.-E.E., Mohiman M., Tusher S.M., Hasan S., Nowraj S.Z.A., Rahman M.A. Impact of meteorological parameters on COVID-19 transmission in Bangladesh: a spatiotemporal approach. ThApC. 2021;144(1):273–285. doi: 10.1007/s00704-021-03535-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Zhang L., Liu X., Wei Y., Liu C., Lian X., Huang Z., Chou J., Liu X., Li X. Global prediction system for COVID-19 pandemic. Sci. Bull. 2020;65(22):1884. doi: 10.1016/j.scib.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Z., Huang J., Gu Q., Du P., Liang H., Dong Q. Optimal temperature zone for the dispersal of COVID-19. Sci. Total Environ. 2020;736:139487. doi: 10.1016/j.scitotenv.2020.139487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamil T., Alam I., Gojobori T., Duarte C.M. No evidence for temperature-dependence of the COVID-19 epidemic. Front. Public Health. 2020;8:436. doi: 10.3389/fpubh.2020.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamshidi S., Baniasad M., Niyogi D. Global to USA county scale analysis of weather, urban density, mobility, homestay, and mask use on COVID-19. Int. J. Environ. Res. Publ. Health. 2020;17(21):7847. doi: 10.3390/ijerph17217847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koirala A., Joo Y.J., Khatami A., Chiu C., Britton P.N. Vaccines for COVID-19: the current state of play. Paediatr. Respir. Rev. 2020;35:43–49. doi: 10.1016/j.prrv.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer M.U., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M., Group O.C.-D.W., du Plessis L., Faria N.R., Li R. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni H., Khandait H., Narlawar U.W., Rathod P., Mamtani M. Independent association of meteorological characteristics with initial spread of Covid-19 in India. Sci. Total Environ. 2021;764:142801. doi: 10.1016/j.scitotenv.2020.142801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird E., Rhodes J., Kenny R.A. Vitamin D and inflammation: potential implications for severity of Covid-19. Ir. Med. J. 2020;113(5):81. [PubMed] [Google Scholar]
- Legido-Quigley H., Asgari N., Teo Y.Y., Leung G.M., Oshitani H., Fukuda K., Cook A.R., Hsu L.Y., Shibuya K., Heymann D. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395(10227):848–850. doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lélis da Silva F.L., Pita J.D., Gomes M.D.A., da Silva A.P.L., da Silva G.L.P. Intraregional propagation of Covid-19 cases in Pará, Brazil: assessment of isolation regime to lockdown. Epidemiol. Infect. 2021;149 doi: 10.1017/S095026882100039X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian X., Huang J., Huang R., Liu C., Wang L., Zhang T. Impact of city lockdown on the air quality of COVID-19-hit of Wuhan city. Sci. Total Environ. 2020;742:140556. doi: 10.1016/j.scitotenv.2020.140556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang X., Ma R., Cheng Y., Gong Q., Li J., Zhu B. The right to accessible COVID-19 testing in the post-epidemic period under the urban–rural integration: Haishu District, Ningbo city, China. Sustainability. 2022;14(3):1636. [Google Scholar]
- Lin C., Lau A.K., Fung J.C., Guo C., Chan J.W., Yeung D.W., Zhang Y., Bo Y., Hossain M.S., Zeng Y. A mechanism-based parameterisation scheme to investigate the association between transmission rate of COVID-19 and meteorological factors on plains in China. Sci. Total Environ. 2020;737:140348. doi: 10.1016/j.scitotenv.2020.140348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey M.W., Wilson D.B. Sage Publications; Thousand Oaks, CA: 2001. Practical Meta-Analysis. [Google Scholar]
- Liu J., Xie W., Wang Y., Xiong Y., Chen S., Han J., Wu Q. A comparative overview of COVID-19, MERS and SARS. Int. J. Surg. 2020;81:1–8. doi: 10.1016/j.ijsu.2020.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Huang J., Li C., Zhao Y., Wang D., Huang Z., Yang K. The role of seasonality in the spread of COVID-19 pandemic. Environ. Res. 2021;195:110874. doi: 10.1016/j.envres.2021.110874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C., Mubareka S., Steel J., Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3(10):e151. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T., Lumley M.T. Package ‘leaps’. 2013. https://cran.r-project.org/web/packages/leaps/leaps.pdf
- Marquès M., Domingo J.L. Positive association between outdoor air pollution and the incidence and severity of COVID-19. A review of the recent scientific evidences. Environ. Res. 2022;203:111930. doi: 10.1016/j.envres.2021.111930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marr L.C., Tang J.W., Van Mullekom J., Lakdawala S.S. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface. 2019;16(150):20180298. doi: 10.1098/rsif.2018.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Méndez-Arriaga F. The temperature and regional climate effects on communitarian COVID-19 contagion in Mexico throughout phase 1. Sci. Total Environ. 2020;735:139560. doi: 10.1016/j.scitotenv.2020.139560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merow C., Urban M.C. Seasonality and uncertainty in global COVID-19 growth rates. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(44):27456. doi: 10.1073/pnas.2008590117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Milton D.K. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19) Clin. Infect. Dis. 2020;71(9):2311–2313. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Ann. Rev. Virol. 2020;7:83–101. doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- Pani S.K., Lin N.-H., RavindraBabu S.t. Association of COVID-19 pandemic with meteorological parameters over Singapore. Sci. Total Environ. 2020;740:140112. doi: 10.1016/j.scitotenv.2020.140112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peel M.C., Finlayson B.L., McMahon T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 2007;11(5):1633–1644. [Google Scholar]
- Peters J.L., Sutton A.J., Jones D.R., Abrams K.R., Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- Rendana M. Impact of the wind conditions on COVID-19 pandemic: a new insight for direction of the spread of the virus. Urban Clim. 2020;34:100680. doi: 10.1016/j.uclim.2020.100680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes J.M., Subramanian S., Laird E., Griffin G., Kenny R.A. Perspective: vitamin D deficiency and COVID-19 severity–plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis. J. Intern. Med. 2021;289(1):97–115. doi: 10.1111/joim.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rios G., Fratti J.D.C., Castillo E., Soto A., Castillo W., Choc M. Meteorological factors associated with the spread of the COVID-19 virus. Chest. 2020;158(4):A338. [Google Scholar]
- Sabino C.P., Ball A.R., Baptista M.S., Dai T., Hamblin M.R., Ribeiro M.S., Santos A.L., Sellera F.P., Tegos G.P., Wainwright M. Light-based technologies for management of COVID-19 pandemic crisis. J. Photochem. Photobiol. B Biol. 2020;212:111999. doi: 10.1016/j.jphotobiol.2020.111999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sangkham S., Thongtip S., Vongruang P. Influence of air pollution and meteorological factors on the spread of COVID-19 in the Bangkok Metropolitan Region and air quality during the outbreak. Environ. Res. 2021;197:111104. doi: 10.1016/j.envres.2021.111104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkodie S.A., Owusu P.A. Impact of meteorological factors on COVID-19 pandemic: evidence from top 20 countries with confirmed cases. Environ. Res. 2020;191:110101. doi: 10.1016/j.envres.2020.110101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligmann H., Iggui S., Rachdi M., Vuillerme N., Demongeot J. Inverted covariate effects for first versus mutated second wave Covid-19: high temperature spread biased for young. Biology. 2020;9(8):226. doi: 10.3390/biology9080226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seminara G., Carli B., Forni G., Fuzzi S., Mazzino A., Rinaldo A. Biological fluid dynamics of airborne COVID-19 infection. Rendiconti Lincei. Sci. Fis. Nat. 2020;31(3):505–537. doi: 10.1007/s12210-020-00938-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Licen S., Perrone M.G., Piazzalunga A., Borelli M., Palmisani J., Di Gilio A. Potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first observational study based on initial epidemic diffusion. BMJ Open. 2020;10(9) doi: 10.1136/bmjopen-2020-039338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharif N., Ahmed S.N., Opu R.R., Daullah M.U., Khan S., Talukder A.A., Okitsu S., Ushijima H., Zhang M., Dey S.K. Impact of meteorological parameters and population density on variants of SARS-CoV-2 and outcome of COVID-19 pandemic in Japan. Epidemiol. Infect. 2021;149:e103. doi: 10.1017/S095026882100100X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi T., Min M., Ye P., Wang Y., Qu G., Zhang Y., Liang M., Sun Y., Duan L., Bi P. Meteorological variables and the risk of fractures: a systematic review and meta-analysis. Sci. Total Environ. 2019;685:1030–1041. doi: 10.1016/j.scitotenv.2019.06.281. [DOI] [PubMed] [Google Scholar]
- Shokouhi M., Miralles-Wilhelm F., Amoroso M.A., Sajadi M.M. 2020. Temperature, Humidity, and Latitude Analysis to Predict Potential Spread and Seasonality for COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamerius J., Nelson M.I., Zhou S.Z., Viboud C., Miller M.A., Alonso W.J. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ. Health Perspect. 2011;119(4):439–445. doi: 10.1289/ehp.1002383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamerius J.D., Shaman J., Alonso W.J., Bloom-Feshbach K., Uejio C.K., Comrie A., Viboud C. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9(3) doi: 10.1371/journal.ppat.1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokumaru M., Kojima M., Fujiki K.i. Solar cycle evolution of the solar wind speed distribution from 1985 to 2008. J. Geophys. Res. 2010;115(A4) [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010;36(3):1–48. [Google Scholar]
- Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tang K., Feng K., Lin X., Lv W., Chen K., Wang F. Impact of temperature and relative humidity on the transmission of COVID-19: a modelling study in China and the United States. BMJ Open. 2021;11(2) doi: 10.1136/bmjopen-2020-043863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J. Med. Virol. 2020;92(6):568–576. doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M.P., Xiao S., Zhang Z. The role of climate during the COVID-19 epidemic in New South Wales, Australia. Transbound. Emerg. Dis. 2020;67(6):2313–2317. doi: 10.1111/tbed.13631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2021. WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020.https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 Available at: [Google Scholar]
- WHO . 2021. WHO Coronavirus(COVID-19) Dashboard.https://covid19.who.int/ Available at: [Google Scholar]
- WHO . 2021. WHO Coronavirus (COVID-19) Dashboard.https://covid19.who.int/table Available at: [Google Scholar]
- Wickham H., Averick M., Bryan J., Chang W., McGowan L.D.A., François R., Grolemund G., Hayes A., Henry L., Hester J. Welcome to the tidyverse. J. Open. Source. Softw. 2019;4(43):1686. [Google Scholar]
- WMO . 2021. First Report of the WMO COVID-19 Task Team: Review on Meteorological and Air Quality Factors Affecting the COVID-19 Pandemic. NO.1262. [Google Scholar]
- Woodby B., Arnold M.M., Valacchi G. SARS-CoV-2 infection, COVID-19 pathogenesis, and exposure to air pollution: what is the connection? Ann. N. Y. Acad. Sci. 2021;1486(1):15–38. doi: 10.1111/nyas.14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.T., Leung K., Bushman M., Kishore N., Niehus R., de Salazar P.M., Cowling B.J., Lipsitch M., Leung G.M. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat. Med. 2020;26(4):506–510. doi: 10.1038/s41591-020-0822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., Du M., Liu M. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S.-q., Fang Z.-g., Lv C.-x., An S.-y., Guan P., Huang D.-s., Wu W. Spatiotemporal cluster analysis of COVID-19 and its relationship with environmental factors at the city level in mainland China. Environ. Sci. Pollut. Res. 2021:1–10. doi: 10.1007/s11356-021-16600-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X.-D., Su X.-Y., Li H.-L., Ma R.-F., Qi F.-J., Cao Y.-E. Impacts of socio-economic determinants, spatial distance and climate factors on the confirmed cases and deaths of COVID-19 in China. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0255229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X., Li H., Cao Y. Influence of meteorological factors on the COVID-19 transmission with season and geographic location. Int. J. Environ. Res. Publ. Health. 2021;18(2):484. doi: 10.3390/ijerph18020484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., Wang W. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55(5) doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin C., Zhao W., Pereira P. Meteorological factors' effects on COVID-19 show seasonality and spatiality in Brazil. Environ. Res. 2022;208:112690. doi: 10.1016/j.envres.2022.112690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ye C., Yu J., Zhu W., Wang Y., Li Z., Xu Z., Cheng J., Wang N., Hao L. The complex associations of climate variability with seasonal influenza A and B virus transmission in subtropical Shanghai, China. Sci. Total Environ. 2020;701:134607. doi: 10.1016/j.scitotenv.2019.134607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Xue T., Jin X. Effects of meteorological conditions and air pollution on COVID-19 transmission: evidence from 219 Chinese cities. Sci. Total Environ. 2020;741:140244. doi: 10.1016/j.scitotenv.2020.140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.