Abstract
Background
Breast leiomyoma is a rare benign mesenchymal tumor, accounting for less than 1% of all breast neoplasms. Cases of breast atypical leiomyoma is even more rarely reported and its diagnostic criteria together with its clinical courses is not cleared defined.
Case presentation
We described two patients with breast leiomyomas. One has unilateral benign breast leiomyoma, the other one has bilateral breast leiomyomas. For the bilateral case, the left-side tumor was diagnosed as benign leiomyoma while the right-side tumor was diagnosed as atypical leiomyoma. The morphological features that lead to the diagnosis of atypical leiomyoma are its invasive growth pattern, mild nuclear atypia, and mitotic figures up to 3mitoses/10HPF.
Conclusions
Atypical breast leiomyoma appears to behave like benign leiomyoma without recurrence in our study with nine-year follow-up. Due to the limited experience, cases presented as atypical intraparenchymal breast leiomyoma should be closely followed.
Keywords: Breast leiomyoma, Atypical leiomyoma, Case report
Background
Breast leiomyoma is a rare breast parenchymal tumor, accounting for less than 1% of all breast neoplasms [1]. It usually occurs in middle-aged women with an average age of 47.6 years [2]. Breast leiomyoma share the same histology and immunophenotype with leiomyoma of other sites. A reliable diagnosis is better achieved on excisional specimens with characteristic morphology and immunohistochemical (IHC) staining pattern that are the same with leiomyoma from other organ origins. It is well established that there are atypical smooth muscle tumors of the uterus [3, 4]. However, due to its rarity in the breast, no definitive diagnostic criteria have been proposed for atypical breast leiomyoma [5, 6]. Here, we present two cases of breast leiomyoma and for one of them a diagnosis of atypical leiomyoma should be considered based on its infiltrating growth pattern, mild nuclear atypia and increased mitotic figures.
Case presentation
Case 1
A 46-year-old woman presented with a 3 cm left breast lump detected ten days ago in March 2019. Lumpectomy was performed with all margins clean. Pathology examination revealed a well-circumscribed dense tan mass in breast parenchyma. Histologic examination showed monotonous spindle cell proliferation without nuclear atypia, necrosis or mitotic figures found (Fig. 1A–C). These cells are uniformly positive for smooth muscle actin (SMA), desmin, and caldesmon in IHC staining, and the Ki-67 index was smaller than 1%. The diagnosis of intraparenchymal breast leiomyoma was made. There is no recurrence after 2.5 years of follow-up.
Fig. 1.
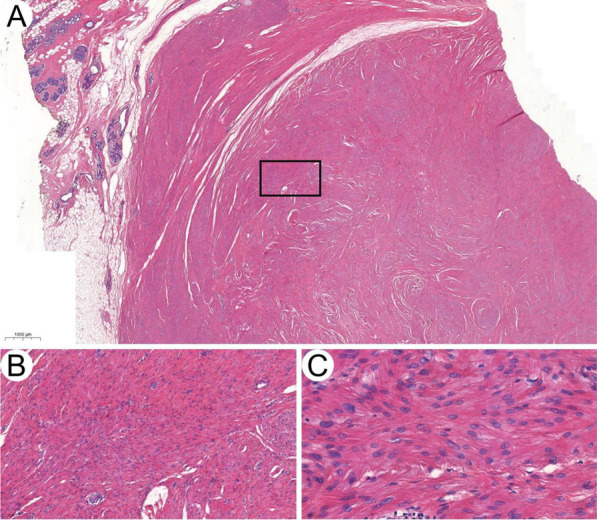
Benign intraparenchymal breast leiomyoma. A–C Histologic image of leiomyoma in case 1 (H&E × 10, × 100 and × 400)
Case 2
A 43-year-old woman presented with relapsed bilateral breast lumps for six months in September 2012. Ultrasound revealed a 1 cm mass in the right breast and a 3 cm one in the left. She had a history of bilateral breast masses in 2010, which were excised by lumpectomies and pathology diagnosis was spindle cell tumor without further classification.
Bilateral lumpectomies were performed this time with all margins clean. No further treatment was applied. The histopathology of the left breast mass displayed an infiltrating growth pattern with mild nuclear atypia and mitotic figures up to 3/10 HPF (Fig. 2A–C), which have exceeded the diagnostic criteria for typical benign leiomyoma but fall short of the threshold for leiomyosarcoma. Therefore, the diagnosis of atypical leiomyoma was made. The simultaneous right breast tumor has similar histopathological features with the left side but without apparent infiltration or increased mitosis (Fig. 2F). A diagnosis of intraparenchymal breast leiomyoma was made for the right-side mass. Both tumors share the same IHC staining pattern with positive SMA and desmin. The Ki-67 index is about 5% in atypical leiomyoma (Fig. 2D, E). The patient has no recurrence until the last follow-up in July 2021.
Fig. 2.
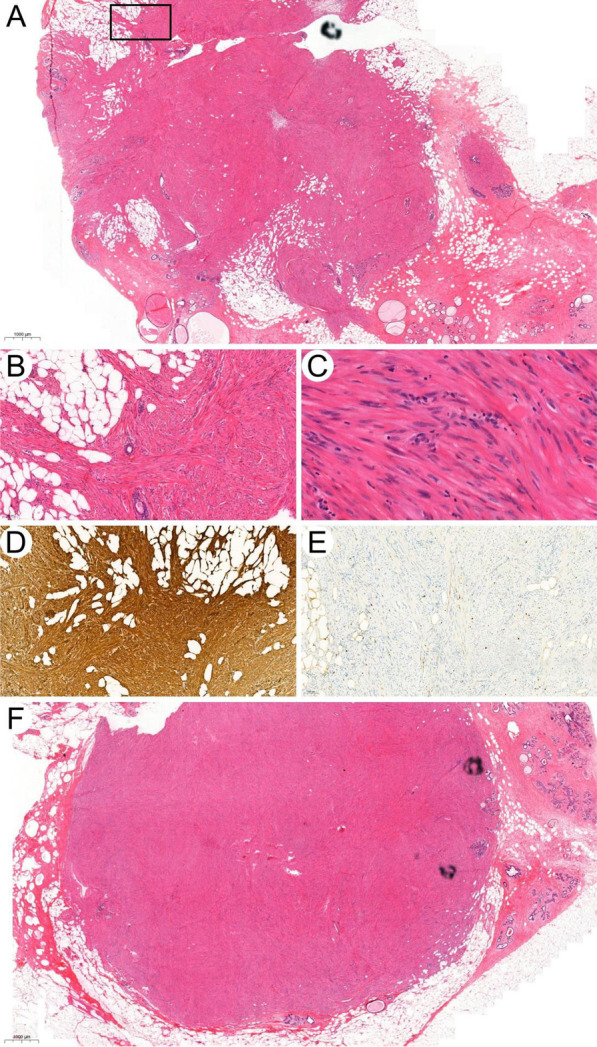
Bilateral leiomyoma of breast. A Leiomyoma of left breast. Noted the invasive growth pattern of this tumor including its infiltrative margin and the packed normal mammary glands in it. The infiltrative margin indicated by the black square is magnified in B (H&E, × 10). B Noted the infiltration of this tumor into adipose tissue (H&E, × 200). C Nuclei of tumor cells in high magnificent view showed typical spindle morphology with blunt end which is characteristics for leiomyoma (H&E, × 400). D, E Immunohistochemical stain of SMA and Ki-67 in leiomyoma of left breast. F Leiomyoma of right breast (H&E, × 10)
Discussion and conclusion
Leiomyoma of the breast is rare and atypical breast leiomyoma is even rarer. To the best of our knowledge, no case of atypical breast leiomyoma has been reported in the English-based literature. Thus, the biological behavior, recurrence rate or diagnostic criteria of atypical breast leiomyoma is unclear. In our reported case of atypical leiomyoma, the patient has no recurrence after lumpectomy by nine years of follow-up, indicating a potential benign behavior of atypical breast leiomyoma. The most common treatment for breast leiomyoma is resection with clean margins [7, 8]. In our experience with atypical leiomyoma, patients achieved favorable prognosis with wide excision only. On account of the limited experience, cases presented as atypical intraparenchymal breast leiomyoma should still be closely followed after surgery.
Due to its rarity, atypical breast leiomyoma has no diagnostic consensus. In uterine, atypical leiomyoma is termed as Uterine Smooth Muscle Tumor of Uncertain Malignant Potential (STUMP) which is also rare. The diagnosis criteria of STUMPs include focal/multifocal or diffuse nuclear atypia and 6–9 mitoses/10HPF; more than 15 mitoses/10HPF without cytological atypia or necrosis; tumor with diffuse nuclear atypia and uncertain mitoses which is often due to brisk karyorrhexis [9–13].
The diagnostic criteria of breast leiomyosarcoma are similar to other parts of the body based on the degree of infiltration, nuclear atypia, and mitotic activity [14–16]. The morphology of atypical leiomyoma falls between leiomyoma and leiomyosarcoma. In multiple or recurrent breast leiomyoma, hereditary leiomyomatosis and renal cell cancer (HLRCC) due to germline mutation of fumarate hydratase should be excluded [17], although our patient had no such family history. The differential diagnosis of breast leiomyoma includes fibroblastic and myofibroblastic tumor, spindle cell lipoma, nodular fasciitis, and nerve sheath tumor [18]. Usually, positive IHC stains for SMA and desmin would confirm the smooth muscle origin. The cell origin of breast parenchymal leiomyoma is not entirely clear; several hypotheses including smooth muscle metaplasia of myoepithelial cell, from smooth muscle cells of the blood vessel or derived from differentiation of multipotent mesenchymal cells has been proposed [19].
Acknowledgements
None.
Abbreviations
- HLRCC
Hereditary leiomyomatosis and renal cell cancer
- HPF
High power field
- IHC
Immunohistochemistry
- SMA
Smooth muscle actin
- STUMP
Uterine smooth muscle tumor of uncertain malignant potential
Author contributions
ML and TH selected the cases; ML, XH and YL review the slides; ML, YL and TH wrote the manuscript. GZ contributed the discussion. All authors read and approved the final manuscript.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Natural Science Foundation of China (Grant No. 82002979), Scientific Research and Development Funds of Peking University People's Hospital (Grant No. RDY2020-16, RDX2021-05) and the Young Investigator Program of Peking University Health Science Center (Grant No. BMU2021PYB013). The funders of the study had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Peking University Cancer Hospital ethics committee (Reference number: 2020KT113). Written consents were obtained from both patients who participated in this study.
Consent for publication
Written consents have been obtained from both patients to use their samples for research and publication of the findings. The patients provided full written, informed consent to publish any identifying images or other personal or clinical details in this manuscript.
Competing interests
The authors declare no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mengping Long, Email: mplong@connect.ust.hk.
Xuejiao Lina Hu, Email: nini114@gmail.com.
Guiyang Zhao, Email: 18611002258@163.com.
Yiqiang Liu, Email: victor.liu76@163.com.
Taobo Hu, Email: thuac@connect.ust.hk.
References
- 1.Ende L, Mercado C, Axelrod D, Darvishian F, Levine P, Cangiarella J. Intraparenchymal leiomyoma of the breast: a case report and review of the literature. Ann Clin Lab Sci. 2007;37(3):268–273. [PubMed] [Google Scholar]
- 2.Diaz-Arias AA, Hurt MA, Loy TS, Seeger RM, Bickel JT. Leiomyoma of the breast. Hum Pathol. 1989;20(4):396–399. doi: 10.1016/0046-8177(89)90052-X. [DOI] [PubMed] [Google Scholar]
- 3.Sabry M, Al-Hendy A. Medical treatment of uterine leiomyoma. Reprod Sci. 2012;19(4):339–353. doi: 10.1177/1933719111432867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ly A, Mills AM, McKenney JK, Balzer BL, Kempson RL, Hendrickson MR, Longacre TA. Atypical leiomyomas of the uterus: a clinicopathologic study of 51 cases. Am J Surg Pathol. 2013;37(5):643–649. doi: 10.1097/PAS.0b013e3182893f36. [DOI] [PubMed] [Google Scholar]
- 5.Kotsuma Y, Wakasa K, Yayoi E, Kishibuchi M, Kishibuchi M, Sakamoto G. A case of leiomyoma of the breast. Breast Cancer. 2001;8(2):166–169. doi: 10.1007/BF02967498. [DOI] [PubMed] [Google Scholar]
- 6.Kafadar MT, Yalcin M, Gok MA, Aktas A, Yurekli TS, Arslan AI. Intraparenchymal leiomyoma of the breast: a rare location for an infrequent tumor. Eur J Breast Health. 2017;13(3):156–158. doi: 10.5152/ejbh.2017.3472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brandao RG, Elias S, Pinto Nazario AC, Alcoforado Assuncao M, Esposito Papa CC, Facina G. Leiomyoma of the breast parenchyma: a case report and review of the literature. Sao Paulo Med J. 2018;136(2):177–181. doi: 10.1590/1516-3180.2016.0253040117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pourbagher A, Pourbagher MA, Bal N, Oguzkurt L, Ezer A. Leiomyoma of the breast parenchyma. AJR Am J Roentgenol. 2005;185(6):1595–1597. doi: 10.2214/AJR.04.1453. [DOI] [PubMed] [Google Scholar]
- 9.Atkins KA, Arronte N, Darus CJ, Rice LW. The Use of p16 in enhancing the histologic classification of uterine smooth muscle tumors. Am J Surg Pathol. 2008;32(1):98–102. doi: 10.1097/PAS.0b013e3181574d1e. [DOI] [PubMed] [Google Scholar]
- 10.Bell SW, Kempson RL, Hendrickson MR. Problematic uterine smooth muscle neoplasms. A clinicopathologic study of 213 cases. Am J Surg Pathol. 1994;18(6):535–558. doi: 10.1097/00000478-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Ip PP, Cheung AN, Clement PB. Uterine smooth muscle tumors of uncertain malignant potential (STUMP): a clinicopathologic analysis of 16 cases. Am J Surg Pathol. 2009;33(7):992–1005. doi: 10.1097/PAS.0b013e3181a02d1c. [DOI] [PubMed] [Google Scholar]
- 12.Gupta M, Laury AL, Nucci MR, Quade BJ. Predictors of adverse outcome in uterine smooth muscle tumours of uncertain malignant potential (STUMP): a clinicopathological analysis of 22 cases with a proposal for the inclusion of additional histological parameters. Histopathology. 2018;73(2):284–298. doi: 10.1111/his.13515. [DOI] [PubMed] [Google Scholar]
- 13.Kalogiannidis I, Stavrakis T, Dagklis T, Petousis S, Nikolaidou C, Venizelos I, Rousso D. A clinicopathological study of atypical leiomyomas: Benign variant leiomyoma or smooth-muscle tumor of uncertain malignant potential. Oncol Lett. 2016;11(2):1425–1428. doi: 10.3892/ol.2015.4062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amaadour L, Benbrahim Z, Moumna K, Boudahna L, Amarti A, Arifi S, Mellas N, El Mesbahi O. Primary breast leiomyosarcoma. Case Rep Oncol Med. 2013;2013:732730. doi: 10.1155/2013/732730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karabulut Z, Akkaya H, Moray G. Primary leiomyosarcoma of the breast: a case report. J Breast Cancer. 2012;15(1):124–127. doi: 10.4048/jbc.2012.15.1.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oktay Y, Fikret A. Leiomyosarcoma of the breast. J Surg Case Rep. 2011;2011(7):1. doi: 10.1093/jscr/2011.7.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Menko FH, Maher ER, Schmidt LS, Middelton LA, Aittomaki K, Tomlinson I, Richard S, Linehan WM. Hereditary leiomyomatosis and renal cell cancer (HLRCC): renal cancer risk, surveillance and treatment. Fam Cancer. 2014;13(4):637–644. doi: 10.1007/s10689-014-9735-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abd el-All HS Breast spindle cell tumours: about eight cases. Diagn Pathol. 2006;1:13. doi: 10.1186/1746-1596-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sidoni A, Luthy L, Bellezza G, Consiglio MA, Bucciarelli E. Leiomyoma of the breast: case report and review of the literature. Breast. 1999;8(5):289–290. doi: 10.1054/brst.1999.0061. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the current study available from the corresponding author on reasonable request.


