Abstract
Data from the 2014 Native Hawaiian and Pacific Islander (NHPI) National Health Interview Survey were used to examine associations between food security and individual chronic diseases, total number of chronic diseases, and general health status among 637 NHPI adults with income below 200 percent federal poverty level. Very low food security was associated with hypertension, diabetes, and asthma. Very low food security and marginal food security were associated with having any chronic disease and with having a higher number of chronic diseases. Risk for food insecurity increased as health status decreased. These associations had not previously been documented for NHPI.
Keywords: Pacific Islander, Chronic Disease, Food Insecurity, Minority Health
INTRODUCTION
In 2018, 11.1% of U.S. households were food insecure, affecting 37.2 million people and particularly those who are low-income.(1) Food insecurity is associated with a variety of chronic diseases, including diabetes, hypertension, and asthma, among many others.(2–5) Food insecurity is also associated with a variety of behaviors—including tobacco and alcohol use,(6, 7) low physical activity,(8–10) and poor dietary quality(11, 12)—associated with development and exacerbation of chronic diseases.(13–16)
Chronic diseases make up 7 of the 10 leading causes of death in the United States.(17) Adults with chronic diseases experience decreased health-related quality of life, which is exacerbated in communities of a lower socioeconomic status.(18) A 2017 US Department of Agriculture (USDA) report documented positive associations between 10 chronic diseases and food insecurity.(5) The report also showed that the probability of excellent self-reported health was much lower in food insecure households, which is consistent with findings from other studies.(5, 19–21)
Native Hawaiians and Pacific Islanders (NHPI) in the US have a high prevalence of food insecurity and a high prevalence of many chronic diseases, including type 2 diabetes, hypertension, and obesity.(22–31) Food insecurity has been observed in 20.5% of NHPI households, higher than in Asian, non-Hispanic White, and Hispanic households.(30) Also, self-reported excellent or very good health has been observed at lower rates among NHPI (61.4%) compared to the overall US population (67.3%).(31) However, no nationally representative study has explored the association between chronic disease prevalence, food insecurity, and general health status among NHPI in the US. Given the high prevalence of chronic diseases and their lifelong impacts, it is important for researchers and policy-makers working with NHPI communities to understand the relationships between chronic disease, food insecurity, and general health status in this population.
This study aimed to examine associations between 10 chronic diseases—both individually and collectively—and food security status among a sample of NHPI households likely to face economic constraints. Extending the findings from other populations,(5) we hypothesized a positive association between these chronic diseases and food insecurity. This study’s second aim was to examine associations between food security status and general health status among NHPI households. Extending the findings from other populations,(5, 19–21) we hypothesized a significant association between general health status and food insecurity.
METHODS
Data Source
This study used data from the 2014 Native Hawaiian and Pacific Islanders National Health Interview Survey (NHPI NHIS).(32) The NHPI NHIS was sponsored by the CDC’s National Center for Health Statistics (NCHS). This was the first survey to be nationally representative of NHPI living in the continental US. It gathered self-reported health information about randomly selected persons living in sampled households. Surveys were conducted in person, and items assessed household-level, family-level, adult-level, and child-level information. This study employed adult-, household-, and family-level items.
Study Population
Out of the 2,590 adult respondents aged 18 years and older, 51% self-identified as NHPI alone, and 49% as NHPI in combination with one or more other racial identities. Adults who did not report NHPI as their primary race were not categorized as NHPI for the purposes of this study and were not included in the analytic sample (n=2,172). Similar to procedures used in USDA’s report on food security and chronic disease,(5) we excluded pregnant women (n=18), who may experience ephemeral chronic diseases (e.g., gestational diabetes).
We also excluded respondents who live in households that reported income more than 200 percent of the Federal poverty line (FPL) (n=1,517). Consistent with past USDA methods, this cutoff was selected to exceed the mean income-to-povery ratio (165% FPL) for adults who responded affirmatively to at least one of the 10 Adult Food Security Survey Module items on the 2011–2015 NHIS, while also being low enough that most members included in the analytic sample were likely to experience economic constraints.(5) The final analytic sample comprised 637 adults. Since the NHPH NHIS has a complex sample design, we did not exclude any observations. Rather, we created a subpopulation with the criteria mentioned above to specify the estimation sample.(33)
Measures
Chronic Diseases
The primary outcomes of interest were chronic diseases, which have been defined as illnesses that last at least a year and that result in limitations (to mobility or functioning) and/or require ongoing medical treatment.(5) We examined whether, and the extent to which, food insecurity was associated with 10 chronic diseases.(34) The 10 chronic diseases examined were: (1) Hypertension/high blood pressure; (2) Coronary heart disease (CHD); (3) Hepatitis; (4) Stroke; (5) Cancer; (6) Asthma; (7) Diabetes; (8) Arthritis; (9) Chronic obstructive pulmonary disease (COPD); and (10) Chronic kidney disease. These 10 diseases were selected because the US Centers for Disease Control and Prevention (CDC) identified them as research priorities due to their societal impacts as well as preventability.(34) In the NHPI NHIS, they were captured by the question: “Have you ever been told by a doctor or other health professional that you had […]?”, and self-reported as “Yes”/“No”/“Refused”/“Don’t know”. In the present study, responses of “Refused” and “Don’t know” were recoded as missing. The 10 dichotomous variables were examined individually, and they were summed to create a score ranging from 0 to 10 diseases. From this score, we created an indicator variable (0/1) that captured all respondents with at least one chronic disease.
General Health Status
The secondary outcome was self-reported general health status captured by the question: “Would you say your health in general is excellent, very good, good, fair, or poor?” Because of small numbers, responses of “fair” or “poor” were combined. The categories “Refused”/“Don’t know/“Not ascertained” were recoded as missing.
Food Security Status
Household food security status was the primary predictor of interest. Food security status was assessed at the family level based on responses from an adult household member. This variable was measured using USDA’s 10-item Adult Food Security Survey Module.(35) Responses to all 10 items were dichotomized (yes/no). Following procedures used by NCHS and USDA, answers of “Often true,” “Sometimes true,” and “Yes” were considered affirmative responses.(36, 37) For the two items assessing the frequency of occurrence of food insecurity in the past 30 days, responses were considered affirmative if the respondent’s answer was greater than or equal to 3 days. A food security score (0–10) was created to represent the number of affirmative responses to the food security items. The food security summative score was categorized as: High food security (score=0); Marginal food security (score=1–2); Low food security (score=3–5); and Very low food security (score=6–10).(35)
Covariates
Additional variables included in the analysis were: age (continuous), sex, health insurance, marital status, employment status, educational level of the adult with the highest education in the family, number of children, family size, and household income as ratio of FPL.(38–41)
Analyses
Descriptive Statistics
We conducted statistical analyses using Stata/SE 15.1.(42) We described the sample by calculating percentages and means for categorical and continuous variables. Percentages of adults with each chronic disease were stratified by food security status (high, marginal, low, very low), and Rao-Scott Chi-square tests were conducted to examine the degree of association between them.(43) Per NCHS standards,(44) weighted percentages with a relative standard error >30% were considered unstable (i.e., should be used with caution as they do not meet standards for adequate reliability or precision) and flagged when reported. For continuous, weighted means (standard errors) were computed and the equality of the means was tested.
Adjusted Associations
Because of sample size limitations and minimal variance for some of the chronic disease variables, we individually estimated logistic regressions to determine the association of food security status with the four most prevalent chronic diseases in the analytic sample: diabetes, hypertension, asthma, and arthritis. The corresponding relative standard error for each of these four variables was less than 30%. We also estimated a logistic regression of the association of food insecurity with the presence of any chronic diseases.
For the association of food security status and general health status, we used multinomial logistic regression in lieu of ordinal logistic regression. Ordinal logistic regression is based on the proportional odds model, which assumes that each predictor has the same effects across the categories of the ordinal outcome variable. To test whether the proportional odds assumption was met, the Brant test(45) was applied after running ordinal regression. The Brant test of the suitability of the data for an ordinal regression model suggested that this outcome should be treated as unordered; thus, multinomial logistic regression was used.(46, 47) Estimates for the associations were presented as odds ratios (OR) and their 95% confidence intervals (95% CI).
For the association of food security status with the number of chronic diseases, we used a negative binomial regression. This generalized linear model was chosen in lieu of Poisson regression because the conditional variance of this outcome variable was greater than the conditional mean (i.e., overdispersion).(46) Estimates were incidence rate ratios (IRR) and their 95% CIs.
We refitted all regression models with food security status measured on a continuous scale (Ranging from 0–10), computed marginal effects, and graphically depicted the predictive margins to illustrate the probability of having a chronic disease along the continuum of food security.
All descriptive and regression analyses accounted for the survey’s complex sampling design and were conducted on complete cases. Variance inflator indicator was computed to examine multicollinearity among independent variables. Variance inflator factor revealed multicollinearity between number of children and family size (VIF: 2.87; correlation: 0.81). Since these two variables were controls and not multicollinear with the primary predictor of interest (food insecurity), multicollinearity was ignored. Statistical significance was determined at α=0.05.
RESULTS
Descriptive Analysis
Table 1 shows descriptive statistics categorized by food security status for NHPI adults from households that earn less than 200% FPL. Compared to the other food security categories, NHPI adults in very low food security households were the oldest (mean age=39.0 years; se:2.7); had the lowest proportions of females (43.2%); had the highest proportion of unemployed (50.2%); and had the highest proportion of respondents from households that earn less than 100% FPL (56.6%).
Table 1.
Socio-demographic Characteristics of the Study Population (<200% FPL) by Food Security Status
| Food Security Status | |||||
|---|---|---|---|---|---|
| All | High | Marginal | Low | Very low | |
| N=637 | n=315 | n=89 | n=130 | n=103 | |
| Weighted percent (standard error) | |||||
| Characteristics of NHPI adults | |||||
| Age (years) * | 36.7 (0.7) | 36.5 (1.6) | 34.9 (2.6) | 36.6 (1.4) | 39.0 (2.7) |
| Female | 50.8 (3.4) | 50.1 (4.8) | 57.0 (8.5) | 53.7 (6.8) | 43.2 (6.1) |
| Employed | 54.5 (4.1) | 53.8 (4.1) | 66.5 (9.0) | 51.4 (7.5) | 49.8 (6.5) |
| Married | 51.8 (3.3) | 55.2 (5.9) | 53.1 (9.2) | 45.5 (7.3) | 49.1 (7.6) |
| Insured | 89.7 (1.7) | 88.1 (3.0) | 94.3 (3.2) | 90.7 (4.0) | 89.7 (5.8) |
| Characteristics of NHPI households | |||||
| Educational level † | |||||
| Less than HS/GED | 15.6 (2.4) | 13.4 (2.3) | 17.8 (6.0) | 23.8 (6.3) | 8.8 (3.3) |
| HS/GED | 51.1 (3.2) | 48.9 (6.4) | 41.3 (10.3) | 52.6 (7.8) | 64.6 (7.8) |
| Above HS/GED | 33.3 (2.9) | 37.7 (6.3) | 40.9 (10.1) | 23.6 (4.5) | 26.6 (5.5) |
| Number of children * | 1.7 (0.2) | 1.6 (0.2) | 1.9 (0.4) | 2.2 (0.3) | 1.5 (0.3) |
| Family size * | 4.1 (0.3) | 3.7 (0.3) | 4.9 (0.8) | 4.5 (0.4) | 4.0 (0.6) |
| Poverty: <100% FPL | 39.8 (3.8) | 27.5 (4.8) | 49.6 (11.3) | 47.4 (6.9) | 56.6 (7.9) |
Data Source: NCHS, Native Hawaiian and Pacific Islander National Health Interview Survey, 2014.
Note: Study population includes only those who reported household incomes <200% FPL. All estimates account for complex survey design.
N=number of unweighted observations. HS=High school; GED=General Education Development, FPL=federal poverty level.
Mean (se).
Educational level refers to the level of education of the adult with the highest education in the household.
Table 2 shows the proportions of respondents reporting the 10 chronic diseases overall and by food security status. Prevalence of any chronic diseases (versus none) was associated with food security status (p=0.035), ranging from 38.6% of respondents from high food security households to 61.6% of respondents from very low food security households. Prevalence of hypertension was associated with food security status (p=0.034), ranging from 18.8% of respondents from high food security households to 36.6% of respondents from very low food security households. Prevalence of diabetes was associated with food security status (p=0.002), ranging from 9.7% in high food security households to 28.3% in very low food security households. Prevalence of COPD was associated with food security status (p<0.001), ranging from 0.5% in high food security households to 7.3% in very low food security households. The mean number of chronic diseases per respondent was highest among those from very low food security households (1.4 versus 0.7 from high food security households; p=0.007).
Table 2.
Proportions of the Study Population (<200% FPL) Reporting Chronic Diseases by Subpopulation
| Chronic Diseases | <200% FPL n=637 |
High FS† n=315 |
Marginal FS† n=89 |
Low FS† n=130 |
Very Low FS† n=103 |
p ‡ |
|---|---|---|---|---|---|---|
| Weighted percent (standard error) | ||||||
| Any chronic disease | 47.1 (3.3) | 38.6 (3.9) | 53.2 (8.8) | 50.2 (5.7) | 61.6 (6.7) | 0.035* |
| Number of chronic diseases: mean (se) § | 0.9 (0.0) | 0.7 (0.1) | 0.8 (0.1) | 0.9 (0.1) | 1.4 (0.2) | <0.001*** |
| Hypertension | 25.4 (2.0) | 18.8 (2.4) | 20.5 (5.4) | 34.7 (6.0) | 36.6 (7.6) | 0.034* |
| Coronary Heart Disease | 3.7 (1.0) | 3.2 (1.0) | 1.6 (0.6) | 3.8 (1.7) | 6.8 (3.0) | 0.111 |
| Hepatitis | 2.6 (0.8) | 3.0 (1.4) | 3.6 (1.7) | 2.2 (1.8) | 1.1 (0.6) | 0.668 |
| Stroke | 3.3 (0.7) | 2.6 (0.7) | 4.4 (1.9) | 4.2 (1.9) | 3.5 (1.5) | 0.652 |
| Cancer | 2.5 (0.4) | 1.9 (0.8) | 2.7 (1.8) | 1.8 (0.8) | 4.9 (2.0) | 0.373 |
| Asthma | 19.0 (2.6) | 13.7 (3.2) | 29.0 (10.8) | 14.7 (4.0) | 31.9 (6.9) | 0.088 |
| Diabetes | 12.7 (1.6) | 9.7 (2.0) | 7.0 (3.0) | 12.3 (3.0) | 28.3 (6.9) | 0.002** |
| Arthritis | 15.7 (1.6) | 17.3 (3.5) | 11.2 (3.9) | 13.0 (2.8) | 18.8 (5.2) | 0.569 |
| COPD | 1.8 (0.4) | 0.5 (0.2) | 1.3 (0.7) | 0.9 (0.6) | 7.3 (1.5) | <0.001*** |
| Kidney Disease | 2.5 (0.4) | 2.1 (0.6) | 1.0 (0.6) | 2.2 (1.4) | 5.5 (2.0) | 0.135 |
Data Source: NCHS, Native Hawaiian and Pacific Islander National Health Interview Survey, 2014.
Note: Estimates with relative standard errors >30% are bolded and are considered unstable (i.e., should be used with caution as they do not meet standards for adequate reliability or precision). All estimates account for complex survey design. FS=food security; FPL=federal poverty level; COPD=chronic obstructive pulmonary disease.
Includes only those respondents who reported household income <200% of the federal poverty level.
Results of Rao-Scott Chi-square tests. The Rao-Scott Chi-square tests whether each chronic disease is associated with food security status not accounting for the influence of confounders.
For continuous variable (number of chronic condition), weighted means (Standard errors) were computed and the equality of the means was tested.
p<0.001
p<0.01
p<0.05
Adjusted Associations between Household Food Security Status and Chronic Diseases
Table 3 shows the regression parameters for each of the four most prevalent chronic diseases in the analytic sample (hypertension, diabetes, asthma, and arthritis) as well as for any chronic diseases using logistic regression. Very low food security status was strongly associated with hypertension (OR:2.79, 95% CI:1.26–6.19), diabetes (OR:3.56, 95% CI:1.12–11.39), asthma (OR:3.76, 95% CI:1.33–10.60), or having any chronic diseases (OR:3.31, 95% CI:1.32–8.30), relative to high food security. Marginal or low food security were not significantly associated with the four chronic diseases individually. However, having marginal food security —relative to high food security— was associated with having at least one of the ten chronic diseases (OR: 3.74, 95% CI:1.24–11.33). No food security category was associated with having arthritis in the study population.
Table 3.
Associations between Food Security Status and Chronic Diseases in the Study Population (<200% FPL): Results of multivariable logistic regression and negative binomial regression models
| Characteristics | Multivariable Logistic Regression | Negative Binomial Regression | ||||
|---|---|---|---|---|---|---|
| Hypertension n=533 |
Diabetes n=506 |
Asthma n=533 |
Arthritis n=532 |
Any Chronic Diseases† n=533 |
Number of Chronic Diseases‡ n=533 |
|
| Odds Ratio (standard error) | Incidence Rate Ratio (standard error) | |||||
| Marginal Food Security | 2.14 (0.93) | 0.99 (0.53) | 2.84 (1.72) | 1.06 (0.61) | 3.74* (2.02) | 1.54* (0.25) |
| Low Food Security | 1.78 (0.67) | 1.17 (0.58) | 1.32 (0.46) | 0.96 (0.39) | 1.46 (0.45) | 1.27 (0.15) |
| Very Low Food Security | 2.79* (1.08) | 3.56* (2.02) | 3.76* (1.90) | 1.20 (0.56) | 3.31* (1.48) | 1.76*** (0.20) |
| Age | 1.11*** (0.01) | 1.08*** (0.02) | 0.98 (0.01) | 1.08*** (0.01) | 1.06*** (0.01) | 1.04*** (0.01) |
| Females | 0.94 (0.37) | 0.67 (0.31) | 4.10*** (1.32) | 0.92 (0.39) | 1.48 (0.52) | 1.04 (0.15) |
| Employed/recently employed | 0.54 (0.20) | 0.56 (0.20) | 0.78 (0.22) | 0.67 (0.18) | 0.58* (0.14) | 0.71* (0.09) |
| Insured | 0.66 (0.37) | 0.42 (0.25) | 0.80 (0.43) | 0.57 (0.25) | 0.40 (0.20) | 0.79 (0.12) |
| Educational level § | ||||||
| HS/GED | 1.70 (0.91) | 1.14 (0.51) | 0.70 (0.33) | 1.45 (0.76) | 1.17 (0.45) | 1.14 (0.20) |
| Above HS | 2.40 (1.07) | 1.19 (0.51) | 0.79 (0.37) | 2.05 (1.24) | 1.38 (0.47) | 1.43* (0.21) |
| Number of children | 0.93 (0.14) | 0.91 (0.17) | 0.65* (0.11) | 1.29 (0.26) | 0.78 (0.11) | 0.93 (0.06) |
| Family size | 1.14 (0.13) | 1.05 (0.14) | 1.13 (0.10) | 0.94 (0.17) | 1.20 (0.13) | 1.05 (0.05) |
| Poverty: less than 100% FPL | 1.73 (0.53) | 1.53 (0.71) | 1.47 (0.35) | 1.07 (0.46) | 1.31 (0.41) | 1.12 (0.15) |
Data Source: NCHS, Native Hawaiian and Pacific Islander National Health Interview Survey, 2014.
Note: Due to missing data, N ranged from 506 to 533 for these regressions. Standard errors (se) are in parentheses. All estimates account for complex survey design. Diabetes, hypertension, asthma, and arthritis are the four most prevalent chronic diseases in the analytic sample.
Reference groups: High food security; males; not employed; uninsured; less than HS/GED, Poverty: 100%–199% FPL. HS=High school; GED=General Education Development; FPL=federal poverty level.
Presence of at least one of the following ten chronic diseases: hypertension/high blood pressure, coronary heart disease, hepatitis, stroke, cancer, asthma, diabetes, arthritis, chronic obstructive pulmonary disease, and chronic kidney disease.
Number of chronic diseases present out of the ten chronic diseases assessed.
Educational level refers to the level of education of the adult with the highest education in the household.
p<0.001
p<0.01
p<0.05
Being employed or recently employed—relative to not employed—was associated with lower risk of having at least one of the ten chronic diseases (OR:0.58, 95% CI:0.35–0.95).
The estimated IRR from the negative binomial regression suggest that among NHPI adults with less than 200% FPL, those with very low food security —relative to those with high food security— have significantly higher numbers of chronic diseases (IRR:1.76, 95% CI:1.40–2.23). Similarly, those with marginal food security had significantly higher numbers of chronic diseases than those with high food security (IRR:1.54, 95% CI:1.10–2.15).
Those who were employed or recently employed—relative to not employed—had significantly fewer numbers of chronic diseases than those not employed (IRR:0.71, 95% CI:0.55–0.92).
Figure 1 displays the probability of having each of the most prevalent chronic diseases, the probability of having at least one chronic disease, and the number of chronic diseases along the continuum of food security ranging from 0 to 10. There is a positive association between the probability of having diabetes, hypertension, asthma, or any chronic diseases and food insecurity: the more household food insecurity increases, the higher the probability of NHPI adults to have a chronic disease. However, this relationship does not hold for arthritis, where the curve is relatively flat.
Figure 1.
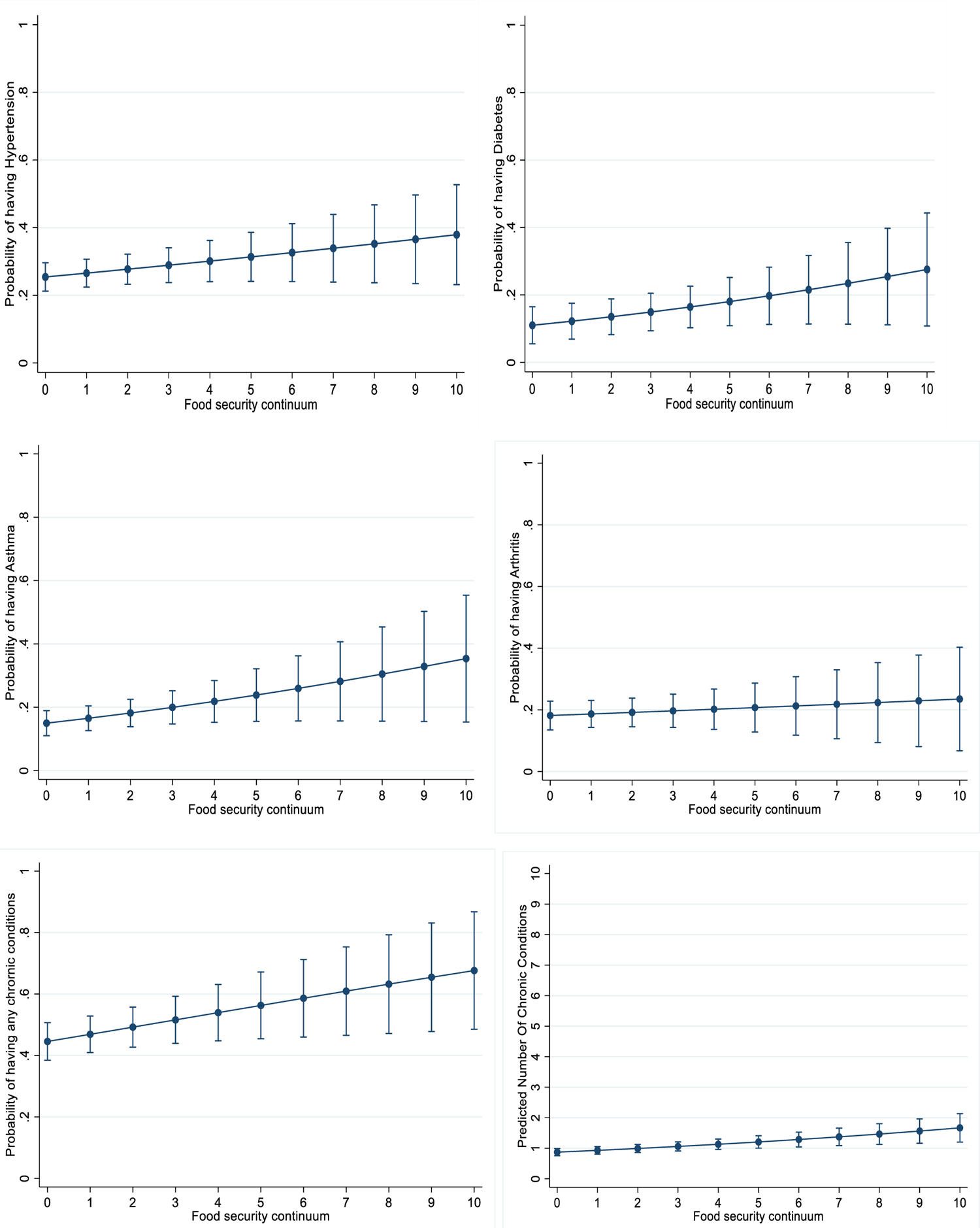
Probability of Chronic Diseases in the Study Population (<200% FPL) along the Continuum of Affirmative Responses to 10 Food Security Items
Data Source: NCHS, Native Hawaiian and Pacific Islander National Health Interview Survey, 2014.
Note: Marginal effects displayed show adjusted predicted probabilities of having chronic diseases, with 95% confidence intervals. Horizontal axis represents the number of affirmative responses (0–10) to USDA’s 10-item Adult Food Security Survey Module.(1)
Results from the multinomial regression for the secondary outcome are presented in Table 4. We found significant differences in food security status across levels of general health status. NHPI adults with excellent health —relative to those with good health— are less likely to experience low food security (OR:0.35, 95% CI:0.13–0.93), and very low food security (OR:0.05, 95% CI:0.01–0.28). On the other hand, NHPI adults with fair or poor health are at greater odds of experiencing low food security (OR:2.88, 95% CI:1.42–5.82) and very low food security (OR:3.65, 95% CI: 1.81–7.36) compared with high food security.
Table 4.
Associations between Food Security Status and General Health Status in the Study Population (<200% FPL): Results of a multinomial logistic regression model, N=637
| Food Security Status | General Health Status |
|||
|---|---|---|---|---|
| Excellent | Very Good | Good (ref) | Fair/Poor | |
|
| ||||
| Odds Ratio (standard error) | ||||
|
| ||||
| High Food Security (ref) | — | — | — | — |
| Marginal Food Security | 1.00 (0.60) | 0.71 (0.41) | — | 0.67 (0.31) |
| Low Food Security | 0.35* (0.17) | 0.73 (0.22) | — | 2.88** (0.99) |
| Very Low Food Security | 0.05** (0.04) | 0.63 (0.33) | — | 3.65** (1.25) |
Data Source: NCHS, Native Hawaiian and Pacific Islander National Health Interview Survey, 2014.
Note: ‘High food security’ and ‘Good’ are reference groups for Food Security Status and General Health Status, respectively. All estimates account for complex survey design. Odds ratios adjusted for age, sex, work, education, marital status, health insurance, number of children, family size, and poverty level. Estimates for these controls are not shown.
p<0.001
p<0.01
p<0.05
DISCUSSION
The present study examines potential associations between 10 high-priority chronic diseases and food security among NHPI households at <200% FPL, showing that hypertension, diabetes, and asthma were associated with very low food security. NHPI from households with very low food security were more likely to report at least one of the 10 chronic diseases and more likely to report a higher number of chronic diseases. NHPI showed increased risk for food insecurity as their general health status decreased. These findings had not previously been documented for NHPI, but are consistent with reported associations between food insecurity and chronic disease in the US general population and in other race/ethnicity groups.(5, 29, 48–50)
To our knowledge, the present study is the first to document associations between food security status, chronic diseases, and general health status in a representative sample of NHPI in the US. Its results demonstrate the importance of examining associations between chronic diseases and food insecurity within each race and ethnicity group in the US. While associations between food insecurity and hypertension, diabetes, asthma, total number of chronic diseases, and general health status found in this study are consistent with findings for the general US population,(5) associations for NHPI related to arthritis differed from previous findings for the general US population.
The present study found no association between arthritis and food insecurity, which contrasts with previous findings where the general population of US working-age adults showed an over 100% increase in arthritis prevalence among adults from households with very low food security (versus high food security).(5) The present study did find unexpected associations between marginal food security and having any chronic disease and with having a higher number of chronic diseases. These associations between chronic disease may be worthy of future investigation, particularly given that these associations were not present for low food security.
NHPI are among the fastest growing populations in the US,(51) and they are at relatively high risk for food insecurity and several chronic diseases.(22–28, 30, 31) Because food insecurity can be a stronger predictor of chronic disease than income or other socioeconomic variables,(5) these findings can guide public health interventions to maximize health outcomes for NHPI. For example, clinical-community partnerships to manage chronic disease in the context of food insecurity are becoming increasingly common, including increased emphasis on screening patients for food insecurity, providing help with applications for federal nutrition programs, providing patient education, and otherwise increasing patient access to healthy foods (e.g., by partnering with food pantries or farmers markets).(52–57) Given the high prevalence of food insecurity and chronic disease among NHPI, cultural adaptation of these interventions for NHPI may be a worthwhile effort.(58) Cultural adaptation has been a key component of effective chronic disease interventions among NHPI,(59–62) and it could increase participant retention, which has been a barrier to scalability of existing interventions focused on chronic disease management in the context of food insecurity.(53)
Limitations
This study’s results must be interpreted with respect to several limitations. First, the NHPI-NHIS relies upon cross-sectional data to assess respondents’ food security status and health information. These data cannot be used to explore changes over time or the extent to which food insecurity preceded the onset of chronic disease or vice versa. Also, sample size limitations (i.e., once the analytic sample was limited to households <200% FPL) and minimal variance for some of the chronic diseases variables limited analyses of the associations of food security status to only the four most prevalent chronic diseases. In addition, NHPI-NHIS data were collected in 2014 and may not fully reflect current conditions. However, the NHPI-NHIS offers the first and only nationally representative data that include a large enough sample of NHPI respondents to explore associations between food insecurity and chronic disease.
Conclusions
This study adds important new information about the associations between chronic diseases and food insecurity among NHPI households. Given the high rates of food insecurity and health disparities experienced by NHPI with respect to diet-sensitive chronic diseases,(23, 24, 26, 31, 63–67) future research should use this study’s findings to develop and evaluate interventions with NHPI that include food security with chronic disease prevention and management. Within NHPI communities and in the general US population, associations among food insecurity, chronic disease, and general health status suggest that improvements in any one of these factors may require addressing the others.
Acknowledgements:
Financial Support:
Support for this study was provided by a Translational Research Institute award under grant No. 1U54TR001629–01A1 from the National Center for Translational Sciences of the National Institutes of Health. The writing of this article was partially supported by the National Institute of General Medical Sciences of the National Institutes of Health under grant No. P20GM109096. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the funders. Any analysis, interpretation, and/or conclusion based on 2014 NHIS and/or 2014 NHPI-NHIS data is solely that of the authors. Opinions, conclusions, and recommendations expressed herein do not necessarily represent those of the NCHS or CDC, which are responsible for the data. NIH had no role in the design, analysis or writing of this article
Footnotes
Conflict of Interest: None
Ethical Standards Disclosure: This study was ruled exempt as non-human subject research by the University of Arkansas for Medical Sciences Institutional Review Board (IRB #206591).
REFERENCES
- 1.Coleman-Jensen A, Rabbitt MP, Gregory CA et al. (2019) Household Food Security in the United States in 2018.
- 2.Gucciardi E, Vahabi M, Norris N et al. (2014) The Intersection between Food Insecurity and Diabetes: A Review. Curr Nutr Rep 3, 324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seligman HK, Laraia BA Kushel MB (2010) Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 140, 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laraia BA (2013) Food insecurity and chronic disease. Adv Nutr 4, 203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gregory CA & Coleman-Jensen A (2017) Food Insecurity, Chronic Disease, and Health Among Working-Age Adults. Washington, DC: United States Department of Agriculture, Economic Research Service. [Google Scholar]
- 6.Kim JE & Tsoh JY (2016) Cigarette Smoking Among Socioeconomically Disadvantaged Young Adults in Association With Food Insecurity and Other Factors. Prev Chronic Dis 13, E08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cutler-Triggs C, Fryer GE, Miyoshi TJ et al. (2008) Increased rates and severity of child and adult food insecurity in households with adult smokers. Arch Pediatr Adolesc Med 162, 1056–1062. [DOI] [PubMed] [Google Scholar]
- 8.To QG, Frongillo EA, Gallegos D et al. (2014) Household food insecurity is associated with less physical activity among children and adults in the U.S. population. J Nutr 144, 1797–1802. [DOI] [PubMed] [Google Scholar]
- 9.Jeon CY, Lokken RP, Hu FB et al. (2007) Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 30, 744–752. [DOI] [PubMed] [Google Scholar]
- 10.Kyu HH, Bachman VF, Alexander LT et al. (2016) Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 354, i3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanson KL & Connor LM (2014) Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr 100, 684–692. [DOI] [PubMed] [Google Scholar]
- 12.Schwingshackl L, Bogensberger B Hoffmann G (2018) Diet Quality as Assessed by the Healthy Eating Index, Alternate Healthy Eating Index, Dietary Approaches to Stop Hypertension Score, and Health Outcomes: An Updated Systematic Review and Meta-Analysis of Cohort Studies. J Acad Nutr Diet 118, 74–100.e111. [DOI] [PubMed] [Google Scholar]
- 13.González K, Fuentes J Márquez JL (2017) Physical Inactivity, Sedentary Behavior and Chronic Diseases. Korean J Fam Med 38, 111–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts CK & Barnard RJ (2005) Effects of exercise and diet on chronic disease. J Appl Physiol (1985) 98, 3–30. [DOI] [PubMed] [Google Scholar]
- 15.McCullough ML, Feskanich D, Stampfer MJ et al. (2002) Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. Am J Clin Nutr 76, 1261–1271. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health (2014) The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General.
- 17.Murphy SL, Xu J, Kochanek KD et al. (2018) Mortality in the United States, 2017. NCHS Data Brief, 1–8. [PubMed]
- 18.Mielck A, Vogelmann M, Leidl R (2014) Health-related quality of life and socioeconomic status: inequalities among adults with a chronic disease. Health and Quality of Life Outcomes 12, 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stuff JE, Casey PH, Szeto KL et al. (2004) Household food insecurity is associated with adult health status. J Nutr 134, 2330–2335. [DOI] [PubMed] [Google Scholar]
- 20.Pheley AM, Holben DH, Graham AS et al. (2002) Food security and perceptions of health status: a preliminary study in rural Appalachia. J Rural Health 18, 447–454. [DOI] [PubMed] [Google Scholar]
- 21.Lee JS & Frongillo EA (2001) Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr 131, 1503–1509. [DOI] [PubMed] [Google Scholar]
- 22.Galinsky A, Zelaya C, Barnes P et al. (2017) Selected health conditions among Native Hawaiian and Pacific Islander adults: United States, 2014. NCHS Data Brief, No. 277. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- 23.McElfish P, Rowland B, Long C et al. (2017) Diabetes and hypertension in Marshallese adults: Results from faith-based health screenings. Journal of Racial and Ethnic Health Disparities 4, 1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karter AJ, Schillinger D, Adams AS et al. (2013) Elevated rates of diabetes in Pacific Islanders and Asian subgroups The Diabetes Study of Northern California (DISTANCE). Diabetes Care 36, 574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aluli N, Jones K, Reyes P et al. (2009) Diabetes and cardiovascular risk factors in Native Hawaiians. Hawaii Med J 68, 152–157. [PMC free article] [PubMed] [Google Scholar]
- 26.Aluli NE, Reyes PW, Brady SK et al. (2010) All-cause and CVD mortality in Native Hawaiians. Diabetes Res Clin Pract 89, 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mau MK, Sinclair K, Saito EP et al. (2009) Cardiometabolic health disparities in Native Hawaiians and other Pacific Islanders. Epidemiol Rev 31, 113–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller BA, Chu KC, Hankey BF et al. (2008) Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control 19, 227–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stupplebeen DA (2019) Housing and Food Insecurity and Chronic Disease Among Three Racial Groups in Hawai’i. Prev Chronic Dis 16, E13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Long CR, Rowland B, McElfish PA et al. (2020) Food Security Status of Native Hawaiians and Pacific Islanders in the US: Analysis of a National Survey. J Nutr Educ Behav. [DOI] [PMC free article] [PubMed]
- 31.Galinsky A, Zelaya C, Simile C et al. (2017) Health conditions and behaviors of Native Hawaiian and Pacific Islander persons in the United States, 2014. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- 32.National Center for Health Statistics (2017) Survey Description, Native Hawaiian and Pacific Islander National Health Interview Survey, 2014. Hyattsville, MD: Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- 33.West BT, Berglund P Herringa S (2008) A Closer Examination of Subpopulation Analysis of Complex-Sample Survey Data. The Stat Journal 8, 520–531. [Google Scholar]
- 34.Goodman RA, Posner SF, Huang ES et al. (2013) Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis 10, E66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.United States Department of Agriculture (2012) U.S. Adult Food Security Survey Module: Three-Stage Design, with Screeners. Washington, DC: USDA, Economic Research Service. [Google Scholar]
- 36.Centers for Disease Control and Prevention; National Center for Health Statistics (2015) 2014 National Health Interview Survey (NHIS) - Public Use Data Release Hyattsville, Maryland: Division of Health Interview Statistics. National Center for Health Statistics. [Google Scholar]
- 37.Bickel G; Nord M; Price C; Hamilton W; Cook J (2000) Guide to measuring household food security, revised 2000. Alexandria, VA: Office of Analysis, Nutrition, and Evaluation. U.S. Department of Agriculture. [Google Scholar]
- 38.Goldberg SL & Mawn BE (2015) Predictors of Food Insecurity among Older Adults in the United States. Public Health Nurs 32, 397–407. [DOI] [PubMed] [Google Scholar]
- 39.Broussard NH (2019) What explains gender differences in food insecurity? Food Policy 83, 180–194. [Google Scholar]
- 40.Hanson KL, Sobal J Frongillo EA (2007) Gender and marital status clarify associations between food insecurity and body weight. J Nutr 137, 1460–1465. [DOI] [PubMed] [Google Scholar]
- 41.Tarasuk V, Fafard St-Germain AA Mitchell A (2019) Geographic and socio-demographic predictors of household food insecurity in Canada, 2011–12. BMC Public Health 19, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.(2019) STATA, 15 ed. College Station, TX: StataCorp LLC. [Google Scholar]
- 43.Rao JNK & Scott AJ (1984) On chi-square test for multiway contingency tables with cell proportions estimated from survey data. Annals of Statistics 12, 40–60. [Google Scholar]
- 44.National Center for Health Statistics National Health and Nutrition Examination Survey: Survey methods and analytical guidelines. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm
- 45.Brant R (1990) Assessing proportionality in the proportional odds model for ordinal logistic regression. Biometrics 46, 1171–1178. [PubMed] [Google Scholar]
- 46.Long JS & Freese J (2014) Regression models for categorical dependent variables using Stata, Third edition. ed. College Station, Texas: Stata Press Publication, StataCorp LP. [Google Scholar]
- 47.Liu X (2016) Applied ordinal logistic regression using Stata : from single-level to multilevel modeling. Los Angeles: Sage. [Google Scholar]
- 48.Vaccaro JA & Huffman FG (2017) Sex and Race/Ethnic Disparities in Food Security and Chronic Diseases in U.S. Older Adults. Gerontol Geriatr Med 3, 2333721417718344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seligman HK & Schillinger D (2010) Hunger and Socioeconomic Disparities in Chronic Disease. New England Journal of Medicine 363, 6–9. [DOI] [PubMed] [Google Scholar]
- 50.Hernandez DC, Reesor LM, Murillo R (2017) Food insecurity and adult overweight/obesity: Gender and race/ethnic disparities. Appetite 117, 373–378. [DOI] [PubMed] [Google Scholar]
- 51.Hixson L, Hepler B Kim M (2012) The Native Hawaiian and Other Pacific Islander population 2010. Washington, DC: United States Census Bureau. [Google Scholar]
- 52.Lundeen EA, Siegel KR, Calhoun H et al. (2017) Clinical-Community Partnerships to Identify Patients With Food Insecurity and Address Food Needs. Prev Chronic Dis 14, E113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Long CR, Rowland B, Steelman SC et al. (2019) Outcomes of disease prevention and management interventions in food pantries and food banks: a scoping review. BMJ Open 9, e029236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.An R, Wang J, Liu J et al. (2019) A systematic review of food pantry-based interventions in the USA. Public Health Nutr 22, 1704–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Trapl ES, Smith S, Joshi K et al. (2018) Dietary Impact of Produce Prescriptions for Patients With Hypertension. Prev Chronic Dis 15, E138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cheyne K, Smith M, Felter EM et al. (2020) Food Bank-Based Diabetes Prevention Intervention to Address Food Security, Dietary Intake, and Physical Activity in a Food-Insecure Cohort at High Risk for Diabetes. Prev Chronic Dis 17, E04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.National Academies of Sciences, Engineering and Medicine (2019) Investing in Interventions That Address Non-Medical, Health-Related Social Needs: Proceedings of a Workshop. [PubMed] [Google Scholar]
- 58.McElfish PA, Yeary KHK, Kaholokula JK et al. (2019) Best practices for community-engaged participatory research with Pacific Islander communities in the US and USAPI: a scoping review. J Health Care Poor Underserved 30, 1302–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kaholokula JK, Ing CT, Look MA et al. (2018) Culturally responsive approaches to health promotion for Native Hawaiians and Pacific Islanders. Ann Hum Biol 45, 249–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yeary K, Aitaoto N, Sparks K et al. (2017) Cultural adaptation of diabetes self-management education for Marshallese residing in the United States: Lessons learned in curriculum development. Progress in Community Health Partnerships: Research, Education and Action 11, 253–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McElfish PA, Long CR, Kohler PO et al. (2019) Comparative Effectiveness and Maintenance of Diabetes Self-Management Education Interventions for Marshallese Patients With Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Care 42, 849–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kaholokula JKa, Look M, Mabellos T et al. (2017) Cultural dance program improves hypertension management for Native Hawaiians and Pacific Islanders: A pilot randomized trial. Journal of racial and ethnic health disparities 4, 35–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Panapasa SV, McNally JW, Heeringa SG et al. (2015) Impacts of Long-Term Obesity on the Health Status of Samoan and Tongan Men in the United States: Results from the Pacific Islander Health Study. Ethn Dis 25, 279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bacong AM, Holub C Porotesano L (2016) Comparing Obesity-Related Health Disparities among Native Hawaiians/Pacific Islanders, Asians, and Whites in California: Reinforcing the Need for Data Disaggregation and Operationalization. Hawaii J Med Public Health 75, 337–344. [PMC free article] [PubMed] [Google Scholar]
- 65.Torre LA, Sauer AM, Chen MS Jr. et al. (2016) Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA Cancer J Clin 66, 182–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.International Diabetes Federation (2017) IDF Diabetes Atlas, 8th edition. Brussels, Belguim: International Diabetes Federation. [Google Scholar]
- 67.NCD Risk Factor Collaboration (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390, 2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]


