Abstract
Purpose:
This study aimed to compare the efficiency of placement technique on internal adaptation, gap formation and microshear bond strength (SBS) of bulk-fill composite resin materials.
Materials and methods:
Standardized class V cavities were prepared for microcomputed tomography (mCT) test and divided into four groups (n=12) as follows: Group SDR: Smart Dentin Replacement system/bulk fill; Group SF2: Sonic-Fill system/bulk fill sonic-activated composite placement system; Group CHU: Herculite-XRV-Ultra composite resin inserted with Compothixo/sonic-vibrated composite resin placement system; Group HIT: Herculite-XRV-Ultra composite resin applied with incremental technique. Self-etch adhesive (Optibond-XTR) was used for bonding in all groups. After 10000 thermocycling, mCT scans were taken to reveal gap formation at the toothrestoration interface and universal testing machine was used to test microshear bond strength SBS values (n=10). ANOVA, post-hoc Bonferroni and Tukey HSD tests were used for evaluating the gap formation and SBS values p=0.05.
Results:
SF2 and CHU showed the best adaptability compared with both SDR and HIT. The difference between groups SDR and HIT was statistically significant (p<0.05).SBS values were found to be the highest for SF2, and the lowest for HIT groups (p>0.05).
Conclusion:
Bulk-fill composite resins placed either with sonic-activated or sonic-vibrated instrument demonstrated better adaptability, less gap formation and higher bond strength than both the bulk-fill flowable composite and conventional incremental techniques.
Keywords: Bulk-fill composite, microcomputed tomography, gap formation, bond strength, sonic instrumentation
Introduction
The use of resin-based composite (RBC) materials has been increasing enormously for nearly a decade. Due to the esthetic appearance and mechanically adequate properties, RBCs are the choice of materials. On the other hand, the performance of RBCs is influenced by several factors, including the design and size of the restoration, placement technique and material itself (1). Although most RBCs meet basic expectations of dentists in terms of adhesion, sealing, wear resistance, fracture toughness and biocompatibility, the main deficiencies of RBCs, such as polymerization shrinkage and internal stress, still exist (2, 3). Polymerization shrinkage leads to voids, microleakage and debonding of RBCs, generates internal stresses due to contraction, and results in a series of challenges starting with voids, leading to gaps, contamination of composite layers, bond failures between increments and tooth-restoration surfaces (4). Moreover, the presence of voids within the final restoration may cause drawbacks like discoloration due to marginal leakage (5, 6). Furthermore, increased wear and microfractures can occur depending on the stress concentration around the voids (7, 8, 9). Ultimately, a decrease in bond strength leads to secondary caries and postoperative sensitivity, leading to failure in the final restoration (10).
Various attempts have been made to solve these problems, including increasing the percentage of the filler content in the composite matrix and reducing the size of filler particles (11, 12). Several studies have shown that heavier filler loading or decreasing the viscosity of the material would result in an increased bond strength of the material, while others concluded that the percentage of the filler content plays a minor role in adhesion (13, 14, 15, 16). However, most studies agreed on the effect of placement techniques, either incremental or bulk-fill, playing a major role in adaptation and polymerization (7,17, 18). These techniques are faciolingual layering (vertical), gingiva-occlusal layering (horizontal), the three-site technique, wedge-shaped layering (oblique), the successive cusp build-up technique, the bulk technique, and centripetal build-up (19).
To reduce clinical steps by filling the cavity with a single increment, bulk-fill composite resins and sonic-activated/ vibrated placement techniques were recently introduced (12,20). Bulk-fill composite resins can be used as a posterior restorative material, an underlining or a base material under suitable RBCs. These materials can be placed up to 4-mm bulk due to their high viscosity and reactivity to light curing, minimizing the voids, reducing porosity and improving the quality of the final restoration (6,21).
Several techniques have been used to evaluate the gap formation and microleakage at the composite-dentin interface, but most of the results vary due to semiquantitative scoring according to the degree of dye penetration, subjective determination of the visual documents or theoretical characterization of each composite that could not simulate the real shrinkage behavior of in vivo conditions (22, 23). Additionally, it is almost impossible to determine and measure the voids within the bulk of the material using conventional methods (17,24). Therefore, a nondestructive and quantitative assessment method, X-ray microcomputed tomography (mCT), was used in this study to quantify and measure the interfacial gaps and voids and also reconstruct the materials and the surrounding tissues three dimensionally (3D), as well as to distinguish the different components into a range of grayscale values, based on the ability to absorb the X-ray to evaluate properly (25).
echniques’ efficiency in internal adaptation and gap formation using mCT; 2) test the microshear bond strength (mSBS) of bulk-fill composite resin materials; 3) compare the effect of gaps and mSBS values and reveal whether any positive correlations exist. Although there are former studies focused on these factors, none evaluated the gaps in the RBCs and investigated the correlation between the rate of adaptation and mSBS of the bulk-fill and conventional RBCs.
The hypotheses of the study were as follows: 1) the shear bond strength will be higher in the sonic-activated/vibrated groups than the incremental placement technique groups, 2) the adaptability and subsequent gap formation will be a statistically different between the bulk-fill and incremental placement technique.
Materials and methods
Ethical statement
Gap formation and shear bond strength were assessed in human molars that were extracted for periodontal reasons; The study protocol has been reviewed and approved by the Ege University Medical Research Ethics Committee (21- 5T/66). 96 extracted caries-free human third molars (48 for mSBS and; 48 for mCT test) were selected to create a pool of teeth for randomization. The teeth were stored in a 2% chloramine solution for a month.
Specimen preparation for the micro-ct test
Forty-eight double-sided standardized class V cavities were prepared using a cylindrical medium-grit diamond bur (835 314 010; Komet, Lemgo, Germany) mounted in a highspeed air turbine (650; KaVo, Biberach, Germany) under water cooling. Cavities were prepared in the approximal surfaces to achieve similar enamel and dentin thickness at occlusal and gingival margins of the cavity using these dimensions: width, 3 mm; length, 3 mm; depth, 4 mm. A two-step selfetch adhesive (Optibond-XTR, Kerr Co, CA, USA) was used for bonding in all the groups.The primer was scrubbed with a brushing motion for 20 s on dentine, air thinned for 5 s, subjected to adhesive application for 15 s and was light-cured for 10 s (Demi Ultra; Kerr Corp, Orange Co, CA, USA). The teeth were randomly divided into four groups (n=12): three experimental and one control. The placement techniques were explained below:
Group - I (SDR)
Smart Dentin Replacement (Dentsply, Konstanz, Germany), is a bulk-fill resin composite placed using the bulk-fill method.
Group - II (SF2)
SonicFill2 (Kerr, Sybron Endo, CA, USA), is a bulk-fill resin composite placed using the sonic-activated composite resin placement method. For this group, the SonicFill compule (compatible with the SonicFill Handpiece) was used.
Group - III (CHU)
Herculite Ultra XRV (Kerr, CA, USA) is a conventional resin composite inserted using Compothixo (a portable sonic vibration instrument).
Group - IV (HIT)
Herculite XRV Ultra (Kerr, CA, USA) is inserted using the Incremental Technique (Control group).
The materials used in the study, their composition, mode of application and manufacturer information are shown in Table 1. The specimens were subjected to a thermocycling regimen of 10000 cycles, at 5-55 ± 8°C with a dwell time of 2 min using a thermocycling machine (Delta Tpo2, Nemo, Mashhad, Iran). High-resolution m-CT (mCT 40; SCANCO Medical, Switzerland) was used to evaluate the adaptation by measuring the overall gap formation percentage and void dimensions at the cavity floors (occlusal, pulpal, cervical and; overall) as well as in the bulk. The imaging settings were as follows: dual-source at 70 kVp; resolution, 8 μm; nominal isotropic pixel area, 72 μm.
Table 1.
Materials used in the study, composition and manufacturer information.
| Material Category | Brand Name | Manufacturer | Filler Concentration | Composition |
|---|---|---|---|---|
| Nanohybrid Composite | SonicFill2 TM | Kerr Co. USA | 81 wt | 2,2'-ethylenedioxydiethyl dimethacrylate, silicon dioxide, titanium dioxide, zinc-oxide, kaolin |
| Kavo, Germany | 63 vol | |||
| Flowable Composite | Surefill SDR | Dentsply. Konstanz. Germany | 78 wt | Urethane di-methacrylate resin, di-methacrylate, di-functional diluents, stronsium amd barium alumino-fluoro-silicate |
| 45 vol | ||||
| Microhybrid Composite | Herculite Ultra XRV | Kerr Co. USA | 79 wt | Hexamethylene diacrylate, hexane-1,6-diol diacrylate, titanium dioxide, methacrylate ester monomer, zinc oxide |
| 59 vol | ||||
| Self-Etch Adhesive | Optibond XTR | Kerr Co. USA | None | Ethanol, esters with acrylic acid, propylidynetrimethanol, 2-hydroxyethyl methacrylate ethoxylated, trimethylsilyl, propanediylbismethacrylate, silanamine, alkalifluorosilicate |
To minimize the changes in the specimen’s position during repeated processes, each specimen was mounted on a special template. 2D sagittal images of each specimen were obtained from the mesial to distal surfaces of the tooth (Figure 1). Nine hundred sagittal cross-sectional images with an interval of 20 mm from the coronal part of the specimens were taken. One hundred slices corresponding to the restoration area (composite-tooth interface) for each specimen at an interval of 30 μm were chosen for the measurements.
Figure 1.
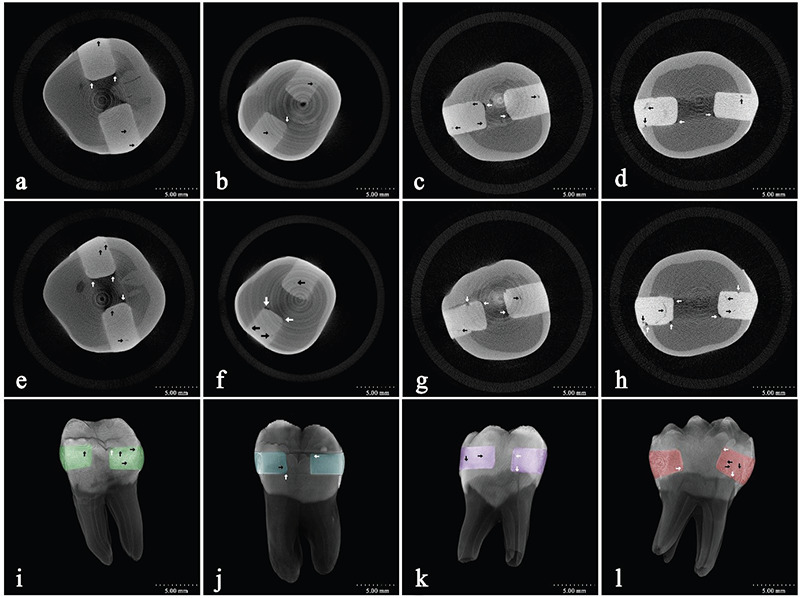
2D micro-CT images and 3D volumetric display for all the groups showing maximum voids within the material and gap formations are as follows: (a,e,i) SDR, (b,f,j), SonicFill2.
To analyze the distribution of gaps at the composite-tooth interface at the occlusal margin, gingival margin and voids within the bulk of the material surface rendered specimen obtained (Figure 1).The 3D images were analyzed using image analysis software (ImageJ ver. 1.46; National Institutes of Health, Bethesda, MD, USA). The percentage, distribution, cluster form and volumetric quantity of the dark pixels (voids and;gaps) as well as the light pixels (tested material and dental hard tissues) were calculated using image analysis software.
Specimen preparation for msbs test and analysis
Twelve teeth for each group were sectioned parallel to the occlusal surface from the upper middle coronal region (~ 1.0-mm thick) and perpendicular to the long axis of the root at one side of the specimen to reach both dentin surfaces, using a water-cooled diamond saw (Isomet, Buehler, IL, USA). The resulting dentin specimens were embedded with the coronal surface exposed in polyvinyl chloride tubes using epoxy resin, both occlusal and polished using wet 400- 600-800 grit silicon carbide paper for 60 seconds to create standardized surfaces.
Twenty resin composite cylinders (1.5 mm. diameter and; 6.0 mm. length) were constructed on the dentin surfaces (two for each teeth) targeting the center of the dentin while avoiding the pulpal horns and enamel residues. After applying the same adhesive system used in mCT tests, composite cyclinders were created with a bonding jig (Ultradent Inc., UT, USA) and cured for 20 s using the same light-emitting diode unit. One of the cyclinders on each specimen was constructed parallel to long axis of the tooth to measure the occlusal dentin shear bond strength, while the other cyclinder was constructed perpendicular to the long axis of the tooth to measure the axial-pulpal dentin shear bond strength. Two random specimens were excluded prior to the mSBS test due to the technical reasons during composite cylinder construction phase. After thermocycling procedure, cross-sectional radiographs and mCT images were taken from each sample prior to the mSBS test to ensure the adaptation was optimal with no gaps (Figure 2). mSBS was tested using the Universal Testing Machine (Instron Inc., MA, USA) at a crosshead speed of 1.0 mm/min and 50 kg of load cell using a 0.5-mm-wide chisel.mSBS values were calculated in MPa by dividing the peak load at failure to the specimen’s surface area (10).
Figure 2.
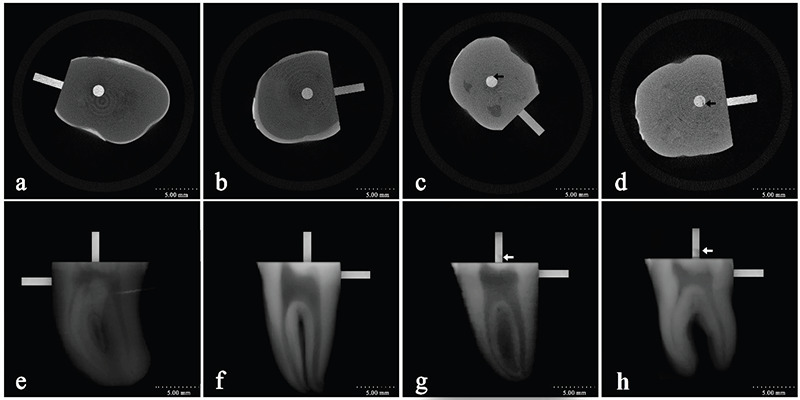
Cross-sectional radiographs and mCT images prior to the bond strength test. (Arrows represent voids within the material).
Statistical analysis
mSBS (Mpa), gap formation (%) and maximum void (mm2) scores obtained from mCT scans were statistically analyzed using SPSS version 23.0 (IBM Corp, IL, USA). One-way analysis of variance and post hoc Bonferroni test were used for evaluating the gap formation scores and post hoc Tukey HSD test was used for comparing the mSBS values amongst the groups. Spearman rank correlation test was chosen to determine the correlation relationship between gap formation and mSBS results (p=0.05).
Results
The mean mSBS for each group is presented in Table 2. The highest mean mSBS value was observed in the SF2 group (17.62 Mpa). A statistically significant difference in mSBS was found between the test groups and control group (p=0.035). The results of the post hoc Tukey test showed that SDR and CHU demonstrated similar results (p=0.872). Therefore, first hypothesis related to shear bond strength is confirmed. Adhesive failures were observed in all samples in the SF2 and SDR groups, while 2 specimens in each CHU and HIT groups exhibited cohesive failures (p=0.677) (Figure 2).
Table 2.
Mean microshear bond strength values (MPa) (with SD*) of each group. Standard deviation values presented in parenthesis. Significant differences between group were given on table using different superscript letters.
| Groups | Minimum mSBS Value | Maximum mSBS Values | Occlusal Dentin mSBS Values | Axio-Pulpal Dentin mSBS Values | Mean mSBS Values |
|---|---|---|---|---|---|
| Gr-1: SDR | 11.902a | 23.351a | 19.785 (2.42) | 13.150 (4.51)a | 16.468 (3.41)a |
| Gr-2: SF2 | 9.556b | 24.575a | 19.982 (3.15) | 15.247 (3.99)a | 17.615 (3.83)a |
| Gr-3: CHU | 8.326b | 22.821a | 17.878 (2.78) | 13.084 (4.05)a | 15.481 (4.50)a |
| Gr-4: HIT | 4.855c | 16.426b | 15.142 (3.02) | 6.376 (4.21)b | 10.759 (3.42)b |
Total restoration volume for each group were similar (35.75 mm3), void and gap percentages (‰107) were be calculated for each group separately according to the bulk volume of the composites. Occlusal, cervical, pulpal and overall mean values (SD) of the maximum void dimensions (mm3×10-8) and overall gap formation percentages observed under mCT for each group are presented in Table 3 and Figure 3. mCT images showed that voids within the bulk of the material were observed commonly close to the pulpal walls in all groups (Figure 1), but the distribution of the voids in the bulk of the material between SDR, SF2, CHU groups was statistically insignificant (p=0.632). Additionally, most of the voids occurred close to the pulpal walls (p=0.044), and gap formation occurred at pulpal regions (p=0.039), with the exception of the SF2 group (p=0.231).
Table 3.
Total restoration volume (mean - mm3), mean void dimensions (mm3) observed in occlusal, cervical, pulpal, in the bulk of the material and the percentage of voids (10-8) acquired from mCT data. Significant differences between group were given on table using different superscript letters.
| Groups | TOTAL (Mean) | Occl. | Cerv. | Pulp. | Bulk | Overall |
|---|---|---|---|---|---|---|
| Gr-1: SDR | 35.62 mm3 | 2.06a | 2.21a | 2.28a | 2.85a | 7.41 mm3 [2.08%]a |
| Gr-2: SF2 | 35.87 mm3 | 1.17b | 1.32b | 1.34b | 2.08a | 4.92 mm3 [1.37%]a |
| Gr-3: CHU | 35.39 mm3 | 1.45b | 1.44b | 1.76b | 2.43a | 5.76 mm3 [1.62%]a |
| Gr-4: HIT | 36.21 mm3 | 4.39c | 4.47b | 4.90c | 6.48b | 14.85 mm3 [4.11%]b |
Figure 3.
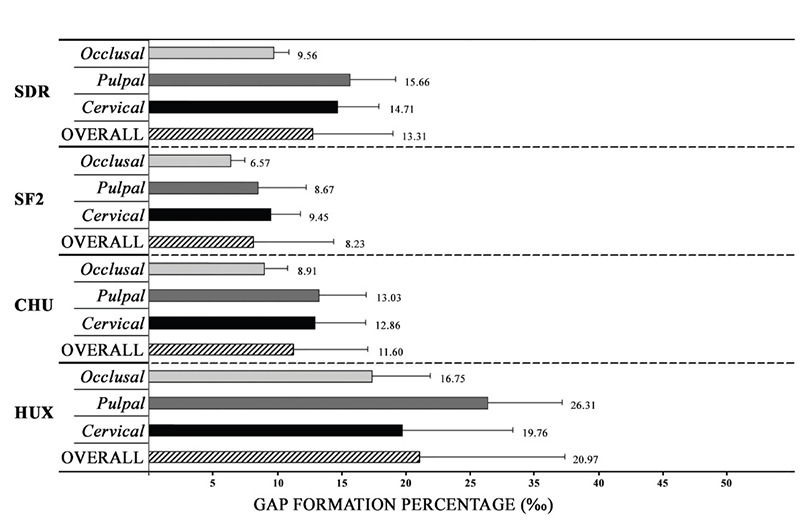
Gap formation percentage (‰) observed in occlusal, cervical and pulpal walls.
The largest void dimensions were observed in “the bulk” of the material for all of the groups, followed by the pulpal and cervical interfaces (p=0.003). The pulpal cavity walls exhibited the largest gap formations, but the differences were statistically insignificant compared with the other interfaces (p=0.462). The mCT images showed that SF2 has the best adaptability, smallest void dimensions (1.17 μm3) and least gap formation (% 1,37 x10-8) (Figure 3). Although CHU showed similar void dimensions in the bulk of material (2,43 mm3) as SF2 (2,08 mm3), the differences in the overall void dimensions between CHU vs. SF2 (p=0.125) and CHU vs. HIT (p=0.348) were statistically insignificant. Therefore, second hypothesis related to gap formation is partially accepted.
The correlation significance scores between mSBS and gap formation obtained from Spearman’s rho test showed that sonically placed composites SF2 (r=0.020), CHU (r=0.045) and microhybrid RBC (HIT) (r=0.010) presented a negative correlation between gap formation and the mSBS scores (p=0.001). On the other hand, no correlation was found between mSBS and gap formation for the SDR group (r=0.127).
Discussion
Although many RBC placement techniques are described, success was not achieved in certain cases, especially in class V cavities, which are susceptible to abfraction forces and leakage of gingival sulcus fluid (4,26). Bulk-fill materials, which have self-levelling features, decreased viscosity and polymerization stress, have been developed to enhance the quality of adaptability to the cavity walls (27). However, the filler content and concentration of the bulkfill materials are associated with some limitations such as microgaps and internal stresses within the material. Therefore, sonic vibrational placement techniques have been developed as an alternative to overcome these challenges (28). In this study, both the microtomographic images and bond strength test results of four materials from each category were investigated to explain the challenges and outcomes of these methods.
Restoration with an RBC involves a rigorous and time-consuming technique that is susceptible to the mechanical properties and chemical composition of the material, as well as the experience of the operator. Both the Bulk-fill SDR and Sonicfill techniques allow condensation of resin composites that can be cured up to a depth of 4-5 mm and at least 20% reduction of the working time compared with the traditional techniques (29, 30). Sampaio et al., (31) suggested that SDR is a type of flowable composite, which can be used as a bulkfill base material and provide better shrinkage and microleakage scores than other flowable RBCs. According to Kapoor et al., (19) SDR is a specially designed RBC and can be used as dentine replacement. Moreover, it showed comparable results to SonicFill when packed in shallow Class I cavities. Contrary to these results, Benetti et al., (8) showed that in “deep” Class II cavities with a gingival cavosurface margin below the cement-enamel junction, high microleakage values were recorded for SDR when compared with SF2. In our case, SDR showed significantly comparable mSBS results (16.47 Mpa) to SF2, but lesser adaptability and increased gap formation (13.31%) compared with Sonicfill2. Decreased filler concentration (both weight and volume) and faster application time of the bulk-fill material SDR could be the main reasons for these differences. Even if all precautions have been taken in the placement stage of this study, increased flowability of the SDR may have caused the application to be performed rapidly, resulting in residual air bubbles in the material and close to the internal surfaces.
The restoration technique and precision in application are the most critical factors in determining the mechanical and physical properties of in vitro conditions because all restorative materials contain defects. Voids in RBCs are unavoidable flaws that contribute to make them prone to wear and fracture (32). To minimize the voids within the restorations, every effort was made to place the RBCs as close as possible to the cavity walls by one operator.
In this study, SF2 presented the least gap formation (8.23%) and mean void dimension of 4.92 mm3, which corroborate with the study of Furness et al.(33), in which the SF2 system achieved a mean value of 10% in gap formation and SDR and conventional RBC presented similar results. Additionally, the results of a study conducted by Swapna et al., (34) demonstrated that most of the gap formation occurred at the cervical and pulpal cavity walls, followed by the occlusal walls, a finding that was consistent with our findings. This study also proved that the voids within the bulk of RBCs comprised most of the defects. These results can be explained by the working principle of the SF2 system. The composite resin used in this system is a combination of both flowable and universal composite resin that incorporates a highly filled proprietary resin with special modifiers that react to sonic energy. Because sonic energy is applied through the hand piece, the modifier causes the viscosity to drop (up to 87%), increasing the flowability of the composite resin until the sonic energy is stopped and then the viscosity turns into a solid and nonslumping phase (35). In accordance with these results, a study conducted by Rengo et al., (26) showed that low-viscosity restorative materials provide satisfactory bond strengths and reasonable microleakage scores compared with conventional RBCs when “deep” Class V cavities were restored.
Another sonically placed composite resin technique evaluated in this study was Compothixo, which is a vibration condensation instrument. The main difference between the two sonically activated placement techniques (SF2 vs. CHU) lies in the incrementation and bulk-filling of the RBCs that change the polymerization stress by slowing the radical polymerization rate (36). In this study, CHU showed comparable mSBS results (15.481 Mpa) with SDR and SF2, while gap formation and void dimensions were relatively better than SDR (11.6%). According to Tolidis et al., (37) conventional RBC packed with the Compothixo System presented better microleakage scores than Sonicfill2 and bulk-fill composites. By contrast, Ortiz et al., (28) compared the adaptation of a fluidized composite resin with a system that modifies its viscosity (Compothixo and SonicFill2) and found a statistically significant difference, showing susceptibility to the formation of the voids at the margins. However, they only measured the cavo-superficial margin using adhesion capability of the selected materials that did not allow evaluation of the degree of total adaptation of a composite resin. Therefore, it is not feasible to evaluate the possible faults that can occur both in the internal margins and within the bulk of the material.
According to our observations, voids commonly occur at internal angles and within material close to the external surfaces of the cavity. In both sonically placed RBCs, an average of 8% (SF2) to 11% (CHU) gap formation was observed; in the bulk-fill placement technique, 13.31% (SDR) gap formation was found. In all groups, the least gap formation was found in the occlusal margins and most of the occlusal gaps were observed at the internal angles. The formation of gaps in the pulpal walls was found to be highest among all groups except for SF2 with a high probability that the unpolymerized RBCs remained in these deeper areas, lost its flowability fast and caused dimensional changes and debonding of the material.
In our study, we evaluated the adaptability of the internal walls as 91% in both sonic-activated placement techniques, a value that is considered satisfactory according to Orlowski et al. (27). Regarding the localization of the gaps, it is important to elucidate whether these are the consequences of the placement technique’s shortage or polymerization shrinkage generated by viscosity changes or poor adaptation of the RBC. mCT analysis of our results demonstrated that the sonic-activated-placed high-viscosity bulk-fill resin composite with reduced polymerization contraction (SF2) and sonic- vibrated high-viscosity microhybrid RBC (CHU) resulted in similar void formation and mSBS to the conventional RBC. In Group CHU and HIT, voids in the transversal mCT images were consistent with lower mSBS values.
We acknowledge that polymerization shrinkage is the major factor involved in the development of contraction stresses and gap formation around cavity margins. In this study, a positive correlation was observed between voids and gap formation for all tested materials consonant to the literature (17,38). The most likely causes are polymerization shrinkage and less likely air bubbles trapped in the material would be the relevant factors affecting the debonding of the material from the cavity walls and decreases the bond strength (33,39). This fact was also confirmed when a negative correlation was observed between gap formation and mSBS values. Bonding to different dentin regions proved to be an important effect factor on mSBS values on bond strength and gap formation values indicating that the internal adaptation performance may not be similar inside the cavity walls (40). The negative correlation between bond strength and gap formation may be explained by the influence of tubule orientation and depth of dentin, positively affecting monomeric infiltration when the tubules are wider, as on the depth dentin and perpendicularly configured, as on the pulpal wall (41). In this study, the occlusal surface showed higher bond strength and lower gap formation than the proximal surface in consisted with the literature (39, 40, 41).
Conclusion
Sonic-activated insertion technique of bulk-fill composites can serve as an alternative choice in restoration of deep cavities to minimize voids because they have enhanced flowability, leading to good adaptation and increased bond strength.
Footnotes
Ethics committee approval: The study protocol has been reviewed and approved by the Ege University Medical Research Ethics Committee (21-5T/66).
Informed consent:Participants provided informed consent.
Peer review: Externally peer-reviewed.
Author contributions: CP, DR participated in designing the study. CP, DR participated in generating the data for the study. CP, DR participated in gathering the data for the study. DR, HK participated in the analysis of the data. CP, DR wrote the majority of the original draft of the paper. HK participated in writing the paper. CP has had access to all of the raw data of the study. CP has reviewed the pertinent raw data on which the results and conclusions of this study are based. CP, DR, HK have approved the final version of this paper. CP guarantees that all individuals who meet the Journal’s authorship criteria are included as authors of this paper.
Conflict of interest:The authors declared no conflict of interest.
Financial disclosure:The authors declared that they have received no financial support.
References
- 1.Ferracane JL. Resin-based composite performance: are there some things we can’t predict? Dent Mater. 2013. Jan;29(1):51–8. 10.1016/j.dental.2012.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaisarly D, Gezawi ME. Polymerization shrinkage assessment of dental resin composites: a literature review. Odontology. 2016. Sep;104(3):257–70. 10.1007/s10266-016-0264-3 [DOI] [PubMed] [Google Scholar]
- 3.Boaro LC, Fróes-Salgado NR, Gajewski VE, Bicalho AA, Valdivia AD, Soares CJ, et al. Correlation between polymerization stress and interfacial integrity of composites restorations assessed by different in vitro tests. Dent Mater. 2014. Sep;30(9):984–92. 10.1016/j.dental.2014.05.011 [DOI] [PubMed] [Google Scholar]
- 4.Ferracane JL, Mitchem JC. Relationship between composite contraction stress and leakage in Class V cavities. Am J Dent. 2003. Aug;16(4):239–43. [PubMed] [Google Scholar]
- 5.Drummond JL. Degradation, fatigue, and failure of resin dental composite materials. J Dent Res. 2008. Aug;87(8):710–9. 10.1177/154405910808700802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim HJ, Park SH. Measurement of the internal adaptation of resin composites using micro-CT and its correlation with polymerization shrinkage. Oper Dent. 2014. Mar-Apr;39(2):E57–70. 10.2341/12-378-L [DOI] [PubMed] [Google Scholar]
- 7.Moharam LM, El-Hoshy AZ, Abou-Elenein K. The effect of different insertion techniques on the depth of cure and vickers surface micro-hardness of two bulk-fill resin composite materials. J Clin Exp Dent. 2017. Feb;9(2):e266–71. 10.4317/jced.53356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benetti AR, Havndrup-Pedersen C, Honoré D, Pedersen MK, Pallesen U. Bulk-fill resin composites: polymerization contraction, depth of cure, and gap formation. Oper Dent. 2015. Mar-Apr;40(2):190–200. 10.2341/13-324-L [DOI] [PubMed] [Google Scholar]
- 9.Leevailoj C, Chaidarun S. Evaluation of voids in class II restorations restored with bulk-fill and conventional nanohybrid resin composite. J Dent Assoc Thai. 2018;68:132–43. [Google Scholar]
- 10.Gupta S, Vellanki VK, Shetty VK, Kushwah S, Goyal G, Chandra SM. In vitro evaluation of shear bond strength of nanocomposites to dentin. J Clin Diagn Res. 2015. Jan;9(1):ZC09–11. 10.7860/JCDR/2015/11463.5386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agarwal RS, Hiremath H, Agarwal J, Garg A. Evaluation of cervical marginal and internal adaptation using newer bulk fill composites: an in vitro study. J Conserv Dent. 2015. Jan-Feb;18(1):56–61. 10.4103/0972-0707.148897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Satterthwaite JD, Vogel K, Watts DC. Effect of resin-composite filler particle size and shape on shrinkage-strain. Dent Mater. 2009. Dec;25(12):1612–5. 10.1016/j.dental.2009.08.012 [DOI] [PubMed] [Google Scholar]
- 13.Kavrik F, Kucukyilmaz E. The effect of different ratios of nano-sized hydroxyapatite fillers on the micro-tensile bond strength of an adhesive resin. Microsc Res Tech. 2019. May;82(5):538–43. 10.1002/jemt.23197 [DOI] [PubMed] [Google Scholar]
- 14.Bociong K, Szczesio A, Krasowski M, Sokolowski J. The influence of filler amount on selected properties of new experimental resin dental composite. Open Chem. 2018;16(1):905–11. 10.1515/chem-2018-0090 [DOI] [Google Scholar]
- 15.Sagsoz O, Ilday NO, Karatas O, Cayabatmaz M, Parlak H, Olmez MH, et al. The bond strength of highly filled flowable composites placed in two different configuration factors. J Conserv Dent. 2016. Jan-Feb;19(1):21–5. 10.4103/0972-0707.173188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cerda-Rizo ER, de Paula Rodrigues M, Vilela A, Braga S, Oliveira L, Garcia-Silva TC, et al. Bonding interaction and shrinkage stress of low-viscosity bulk fill resin composites with high-viscosity bulk fill or conventional resin composites. Oper Dent. 2019. Nov/Dec;44(6):625–36. 10.2341/18-163-L [DOI] [PubMed] [Google Scholar]
- 17.Kim HJ, Park SH. Measurement of the internal adaptation of resin composites using micro-CT and its correlation with polymerization shrinkage. Oper Dent. 2014. Mar-Apr;39(2):E57–70. 10.2341/12-378-L [DOI] [PubMed] [Google Scholar]
- 18.Sun J, Eidelman N, Lin-Gibson S. 3D mapping of polymerization shrinkage using X-ray micro-computed tomography to predict microleakage. Dent Mater. 2009. Mar;25(3):314–20. 10.1016/j.dental.2008.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kapoor N, Bahuguna N, Anand S. Influence of composite insertion technique on gap formation. J Conserv Dent. 2016. Jan-Feb;19(1):77–81. 10.4103/0972-0707.173205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hany SM, Yousry MM, Naguib EA. Evaluation of adaptation of resin composite restorations packed using ultrasonic vibration techniques: A systematic review. Ind J Sci Tech. 2016;9:1–9. [Google Scholar]
- 21.van Dijken JW, Pallesen U. A randomized controlled three year evaluation of “bulk-filled” posterior resin restorations based on stress decreasing resin technology. Dent Mater. 2014. Sep;30(9):e245–51. 10.1016/j.dental.2014.05.028 [DOI] [PubMed] [Google Scholar]
- 22.Kusunoki M, Itoh K, Takahashi Y, Hisamitsu H. Contraction gap versus shear bond strength of dentin adhesive in sound and sclerotic dentins. Dent Mater J. 2006. Sep;25(3):576–83. 10.4012/dmj.25.576 [DOI] [PubMed] [Google Scholar]
- 23.Sun J, Fang R, Lin N, Eidelman N, Lin-Gibson S. Nondestructive quantification of leakage at the tooth-composite interface and its correlation with material performance parameters. Biomaterials. 2009. Sep;30(27):4457–62. 10.1016/j.biomaterials.2009.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sampaio CS, Garcés GA, Kolakarnprasert N, Atria PJ, Giannini M, Hirata R. External marginal gap evaluation of different resin-filling techniques for class II restorations: a micro-ct and sem analysis. Oper Dent. 2020. Jul;45(4):E167–75. 10.2341/19-053-L [DOI] [PubMed] [Google Scholar]
- 25.Takemura Y, Hanaoka K, Kawamata R, Sakurai T, Teranaka T. Three-dimensional X-ray micro-computed tomography analysis of polymerization shrinkage vectors in flowable composite. Dent Mater J. 2014;33(4):476–83. 10.4012/dmj.2013-288 [DOI] [PubMed] [Google Scholar]
- 26.Rengo C, Goracci C, Ametrano G, Chieffi N, Spagnuolo G, Rengo S, et al. Marginal leakage of class V composite restorations assessed using microcomputed tomography and scanning electron microscope. Oper Dent. 2015. Jul-Aug;40(4):440–8. 10.2341/14-022-L [DOI] [PubMed] [Google Scholar]
- 27.Orłowski M, Tarczydło B, Chałas R. Evaluation of marginal integrity of four bulk-fill dental composite materials: in vitro study. ScientificWorldJournal. 2015;2015:701262. 10.1155/2015/701262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han SH, Lee IB. Effect of vibration on adaptation of dental composites in simulated tooth cavities. Korea-Australia Rheol J. 2018;30(4):241–8. 10.1007/s13367-018-0023-9 [DOI] [Google Scholar]
- 29.Vianna-de-Pinho MG, Rego GF, Vidal ML, Alonso RC, Schneider LF, Cavalcante LM. Clinical time required and internal adaptation in cavities restored with bulk-fill composites. J Contemp Dent Pract. 2017. Dec;18(12):1107–11. 10.5005/jp-journals-10024-2184 [DOI] [PubMed] [Google Scholar]
- 30.Penha KS, Souza AF, Dos Santos MJ, Júnior LD, Tavarez RJ, Firoozmand LM. Could sonic delivery of bulk-fill resins improve the bond strength and cure depth in extended size class I cavities? J Clin Exp Dent. 2020. Dec;12(12):e1131–8. 10.4317/jced.57310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sampaio CS, Chiu KJ, Farrokhmanesh E, Janal M, Puppin-Rontani RM, Giannini M, et al. Microcomputed tomography evaluation of polymerization shrinkage of class I flowable resin composite restorations. Oper Dent. 2017. Jan/Feb;42(1):E16–23. 10.2341/15-296-L [DOI] [PubMed] [Google Scholar]
- 32.Han SH, Park SH. Comparison of internal adaptation in class II bulk-fill composite restorations using micro-ct. Oper Dent. 2017. Mar/Apr;42(2):203–14. 10.2341/16-023-L [DOI] [PubMed] [Google Scholar]
- 33.Furness A, Tadros MY, Looney SW, Rueggeberg FA. Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J Dent. 2014. Apr;42(4):439–49. 10.1016/j.jdent.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 34.Swapna MU, Koshy S, Kumar A, Nanjappa N, Benjamin S, Nainan MT. Comparing marginal microleakage of three Bulk Fill composites in Class II cavities using confocal microscope: an in vitro study. J Conserv Dent. 2015. Sep-Oct;18(5):409–13. 10.4103/0972-0707.164058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taneja S, Kumar P, Kumar A. Comparative evaluation of the microtensile bond strength of bulk fill and low shrinkage composite for different depths of Class II cavities with the cervical margin in cementum: An in vitro study. J Conserv Dent. 2016. Nov-Dec;19(6):532–5. 10.4103/0972-0707.194023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mehesen R, Amin LE, Montaser M. The influence of bulk and sonic placement techniques on microleakage of class ii cavities restored with different resin composites. Egypt Dent J. 2020;66(3):1845–53. 10.21608/edj.2020.29011.1117 [DOI] [Google Scholar]
- 37.Tolidis K, Boutsiouki C, Gerasimou P, Panagiotidou E. Microleakage evaluation between higher viscosity and flowable bulk composite resins. Dent Mater. 2014;30:48–57. 10.1016/j.dental.2014.08.096 [DOI] [Google Scholar]
- 38.Hirata R, Clozza E, Giannini M, Farrokhmanesh E, Janal M, Tovar N, et al. Shrinkage assessment of low shrinkage composites using micro-computed tomography. J Biomed Mater Res B Appl Biomater. 2015. May;103(4):798–806. 10.1002/jbm.b.33258 [DOI] [PubMed] [Google Scholar]
- 39.Penha KS, Souza AF, Dos Santos MJ, Júnior LD, Tavarez RJ, Firoozmand LM. Could sonic delivery of bulk-fill resins improve the bond strength and cure depth in extended size class I cavities? J Clin Exp Dent. 2020. Dec;12(12):e1131–8. 10.4317/jced.57310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meriç G, Taşar S, Orhan K. Bonding strategies of resin cement to Er,Cr:YSGG lased dentin: micro-CT evaluation and microshear bond strength testing. Int J Artif Organs. 2016. Feb;39(2):72–6. 10.5301/ijao.5000483 [DOI] [PubMed] [Google Scholar]
- 41.Montagner AF, Carvalho MP, Susin AH. Microshear bonding effectiveness of different dentin regions. Indian J Dent Res. 2015. Mar-Apr;26(2):131–5. 10.4103/0970-9290.159137 [DOI] [PubMed] [Google Scholar]


