Abstract
Background:
The association between illness perceptions and the effectiveness of patients’ illness-management strategies has been supported across a range of medical and psychiatric disorders. Few studies have examined these variables or their association in bipolar disorder (BD). This study examined the main and interactive associations between illness perceptions and one important illness management strategy - social rhythms stability on mood symptom severity in adults with BD.
Methods:
A cross-sectional study with 131 patients with BD in Taiwan was conducted using clinician- and patient-rated mood symptoms, self-reported illness perceptions, and a measure of daily and nightly social rhythms.
Results:
Illness perceptions were associated with mood symptom severity, but social rhythms were not. Unfavorable illness perceptions (e.g., beliefs of experiencing more BD symptoms, having stronger emotional responses to the illness) were associated with more severe mood symptoms. Favorable illness perceptions (e.g., beliefs of being able to understand and control the illness) were associated with less severe mood symptoms, with personal control as the strongest correlate of mood symptom severity. Finally, social rhythm stability moderated the relationship between unfavorable illness perceptions and clinician-rated manic symptoms.
Limitations:
The cross-sectional design limits our ability to make causal conclusions. Also, the effects pertain to patients in remission and may not generalize to more severely ill or hospitalized bipolar patients.
Conclusions:
This study indicates that in patients with BD, illness perceptions are associated with symptom severity. Interventions to enhance favorable IPs and reduce unfavorable IPs may improve mood outcomes, particularly when patients have adopted regular social rhythms.
Keywords: Bipolar disorder, Illness perception, Social rhythm, Depression, Mania
1. Introduction
Illness perception (IP) refers to patients’ beliefs about their health problem(s). The concept of IP was derived from Leventhal’s self-regulatory model, which proposes that people develop both cognitive and emotional representations to actively understand and overcome the impact of their health challenges and, in turn, generate problem-based and emotion-focused coping strategies (Leventhal et al., 1997; H. 2001). Patients’ beliefs about their illness can be favorable or unfavorable, which are associated with better or poorer health outcomes, respectively (Sawyer et al., 2019). Favorable IPs include beliefs that the individual can understand and control the illness by their personal effort or by engaging in treatments that manage their illness (Miceli et al., 2019; Sawyer et al., 2019; Wisting et al., 2019). Unfavorable IPs include beliefs about having a deleterious symptom course, or that the illness or illness label will have irreversible functional consequences.
IPs are associated with patients’ illness management strategies in a range of different conditions, including hypertension (Yang et al., 2018), diabetes (Wisting et al., 2019), heart disease (Mosleh and Almalik, 2016), rheumatoid arthritis (Berner et al., 2018), cancer (Miceli et al., 2019), chronic obstructive and pulmonary disease (Tiemensma et al., 2016), schizophrenia (Lobban et al., 2004), and other mental illnesses or problems (Scerri et al., 2019; Subramaniam et al., 2018). These studies have indicated that IPs play a critical role in approaches to treatment and disease outcomes, including treatment adherence, symptom control, perceived stress, and quality of life. For example, patients’ beliefs about their ability to control the illness may affect their adherence to pharmacological and psychosocial treatments, which then affect treatment outcomes.
Illness beliefs and perceptions have not been adequately explored in patients with mood disorders. Subramaniam et al. (2018) surveyed the IPs among patients with a range of mental illnesses using a multi-ethnic Asian sample (N = 400), and concluded that age, education, and knowledge about illness were positively associated with favorable IPs. Only two studies have examined IPs in bipolar disorder (BD). Averous et al. (2018) found that patients with BD with more favorable IPs and fewer unfavorable IPs showed better adherence to medications. In a study of group psychoeducation, improvements in patients’ IPs, rather than knowledge of the illness or medication adherence, mediated treatment-related improvements in social functioning (Etain et al., 2018). However, the relationship between IPs and mood symptoms in BD is unknown.
Elucidating the associations of IPs, and specifically what beliefs are associated with mood symptoms in BD can have important implications for treatment in this population. For example, favorable IPs about one’s personal understanding of an illness and its controllability might be associated with better mood outcomes, while unfavorable IPs about illness chronicity might be associated with worse mood outcomes. This evidence would have important implications for how treatments that target IPs, such as cognitive-behavioral therapy or psychoeducation, could be improved to provide greater clinical benefits.
In addition to cognitive factors (like IPs), there is considerable evidence that behavioral characteristics, such as disturbances in social rhythms (habitual patterns of sleeping, waking, eating, exercising, and socializing), are associated with the severity of mood symptoms in BD (Alloy et al., 2015; Grandin et al., 2006; Harvey, 2008; Jones et al., 2005; Malkoff-Schwartz et al., 1998, 2000; Shen et al., 2008). The social zeitgeber theory proposes that life events trigger mood episodes and vulnerability to bipolar spectrum disorders by causing disruptions in a person’s social routines, which in turn affect circadian rhythms (e.g., physical or behavioral changes that following daily light/dark cycles; Ehlers et al., 1988). Increasing evidence suggests that circadian dysregulation, activity patterns, and disrupted social rhythms characterize individuals with or at risk for BD (Melo et al., 2017; Murray and Harvey, 2010; Nováková et al., 2015). Patients diagnosed with cyclothymic or bipolar II disorder report significantly more irregular daily routines than healthy controls (Shen et al., 2008). In college students at risk for BD, social rhythm regularity significantly predicts time to first prospective onset of major depressive, hypomanic and manic episodes (Alloy et al., 2015). Two reviews of this literature concluded that both endogenous irregularities in the biological clock’s pacemaking function and external disruptions in circadian rhythms caused by physical and social cues are associated with the onset and course of bipolar spectrum disorders (Abreu and Braganca, 2015; Alloy et al., 2017).
Thus, current theories regarding psychological factors that affect the onset of BD symptoms have emphasized the role of negative cognitions that become activated by stress or reward hypersensitivity (Alloy et al., 2006, 2015; Lima et al., 2018) and social rhythms as predictors of symptom severity and potential targets for psychosocial interventions (Abreu and Braganca, 2015; Alloy et al., 2017; Kato, 2019). There is support for the use of cognitive-behavioral therapy in BD, which focuses on modifying cognitions and behaviors to improve symptom severity (Gonzalez-Isasi et al., 2014; Jones et al., 2015; Lauder et al., 2015). Furthermore, according to the Leventhal’s self-regulatory model, in the context of life stressors, negative IPs may interact with certain personal traits (e.g., circadian rhythm regularity) and specific coping strategies (e.g., ability to challenge beliefs or life styles) could moderate the effects of the IPs on concurrent illness states or outcomes (Hagger et al., 2017; Krok et al., 2019; H. Leventhal et al., 2001). For example, individuals with negative illness beliefs may have a lower probability of depressed mood if they are maintaining stable sleep schedules. A patient who has both negative beliefs (e.g., ‘I cannot control my illness”) and poor sleep/wake regularity may be particularly vulnerable to manic episodes when stressful events disrupt his/her routines. Better understanding of the interplay between such cognitive and behavioral characteristics would support more personalized treatment efforts for patients with BD (Haynes et al., 2016). No study to date has investigated the interaction between IPs, and social rhythm stability on manic and depressive symptoms in adults with BD. In the present study, we examined the main effects and interactions of IPs and social rhythm stability on manic and depressive symptoms in patients with BD. We hypothesized that both favorable IPs and lower social rhythm disturbances would be associated with lower clinician- and patient-rated mood symptoms among patients with BD, while unfavorable IPs and greater social rhythm disturbances would be associated with more severe mood symptoms. Additionally, we hypothesized that better social rhythms would buffer against the negative effects of unfavorable IPs on mood symptoms.
2. Material and methods
2.1. Research design, setting, and procedures
We used a cross-sectional research design to recruit patients in the psychiatric department of a 1200-bed medical center in southern Taiwan. The human rights protection protocols and all other ethics protocols were approved by the hospital’s Institutional Review Board [IRB #: B-ER-103–222] before any patients were recruited. Eligible participants were given written and oral explanations of the study’s details, including the purpose of the study and their right to withdraw at any time without affecting their treatment. We obtained signed written consent from all participants. Participants were provided instructions for how to use the self-reported daily Social Rhythm Metric-5 (SRM-5) and asked to record their daily and nightly activities for one week. After one week, participants returned the completed SRM-5. We then conducted structured interviews to assess their mood symptoms, and patients completed questionnaires concerning their IPs and mood symptoms (see below).
2.2. Participants
Psychiatrists used the following inclusion criteria to refer participants: > 18 years old, able to speak and read Taiwanese (Hoklo) or Taiwanese Mandarin Chinese, and agreed to accept the following medication therapy as needed during the study: a mood stabilizer (valproic acid or lithium salts), an antidepressant, second generation antipsychotics, anxiolytics (lorazepam [< 8 mg/day]), and medicines to counteract side effects. Potential participants who were current alcohol or drug abusers or had been in the previous year, or who had been diagnosed with an organic psychosis, a neurodegenerative disease, a personality disorder, or impaired cognitive abilities were excluded.
Each patient was assessed using the Chinese version of the Modified Schedule of Affective Disorder and Schizophrenia-Lifetime (SADS-L) (Endicott and Spitzer, 1978) to confirm that they met the DSM-IV criteria for a primary diagnosis of BD. The SADS-L has been widely used in clinical research, and its validity and reliability are considered adequate (Hsiao et al., 2009; Rogers et al., 2003).
2.3. Instruments
2.3.1. Brief illness perception questionnaire (BIPQ)
We used the 8-item BIPQ (Broadbent et al., 2006) to assess patients’ IPs, excluding the open-ended question pertaining to beliefs about causal factors. Five items assess cognitive illness representations: consequences (“How much does your illness affect your life?”), timeline (“How long do you think your illness will continue?”), personal control (“How much control do you feel you have over your illness?”), treatment control (“How much do you think your treatment can help your illness?”), and identity (“How much do you experience symptoms from your illness?”). Two items assess emotional representations: concern (“How concerned are you about your illness?”) and emotion (“How much does your illness affect you emotionally?”). One item assesses illness comprehensibility (“How well do you feel you understand your illness?”). All of the items are self-rated using a 0-to-10 response scale. Unfavorable IPs are calculated as the mean of the consequences, timeline, identity, concern, and emotion items, with higher scores indicating more unfavorable IPs. Favorable IPs are calculated as the mean of the personal control, treatment control, and illness comprehension items, with higher scores indicating more favorable IPs.
The psychometric quality of the BIPQ has been tested and found to be internally reliable (Broadbent et al., 2006). The Chinese version of the BIPQ has been assessed with adequate reliability and construct validity in patients with breast cancer (Zhang et al., 2017) and coronary heart disease (Lin et al., 2011). The instrument showed acceptable internal consistency in the current study (Cronbach’s α = 0.66).
2.3.2. Social rhythm metric (SRM)
The self-reported SRM-17 was originally developed to quantify a person’s daily social rhythm pattern (Monk et al., 1990). Bipolar spectrum patients have been found to have lower SRM regularity scores – meaning less consistency in daily and nightly routines- than healthy controls (Jones et al., 2005; Shen et al., 2008). Further, lower scores are associated with higher frequencies of recurrence of mood episodes in bipolar spectrum individuals (Shen et al., 2008). A brief-version, the SRM-5, was developed to minimize participant burden (Monk et al., 2002). The SRM-5 has demonstrated strong sensitivity and specificity compared to the SRM-17 (sensitivity = 74%; specificity = 95%; overall κ = 0.7), and is highly correlated with the SRM-17 in both between-subject and within-subject comparisons over time (Monk et al., 2002).
The SRM-5 is a diary-like instrument with one page per day; the seven sheets constituting one week are then scored as a unit. In the present study, we used the SRM-5 to capture the frequency and timing of five activities that are part of a person’s daily routine by recording the time that these activities occurred: getting out of bed, going to bed, mealtimes, first social contact of the day, and starting work or school (Monk et al., 2002). The habitual time for each activity is calculated, and then the number of activities that occur within 45 min of the habitual time in the week is counted. Activities counted three times in one week are scored 1, and those that occur < 3 times are scored 0. The total scores range from 0 to 5; the higher the score, the more regulated the social rhythms. Subjects who completed less than 5 days of SRM tracking (n = 8) were not included in the analyses.
2.3.3. Assessments for mood symptoms
a). Hamilton Depression Rating Scale (HDRS)
The 17-item HDRS is a widely used clinician-rated depression assessment scale, assessing symptoms during the previous week (Hamilton, 1960). The total score is 52 and is divided into four levels (Keck, 2004): 0–7 means remission, 8–13 means mild severe, 14–22 means moderate severe, and > 23 means very severe. The HDRS has been translated into Chinese and has adequate psychometric quality (Zheng et al., 1988). The inter-rater reliability of the HDRS in the present study was adequate (κ = 0.85).
a). Depression, Anxiety, and Stress Scale (DASS)
The DASS-21 (Henry and Crawford, 2005) is a 21-item self-report measure of depression, anxiety, and stress. It has translated for use as a valid and reliable instrument in Chinese (Moussa et al., 2001). Items are measured on a 4-point Likert scale with higher scores indicating greater severity of symptoms. Only the depression subscale was used in this study. The depression subscale showed good internal consistency (Cronbach’s α= 0.90) and moderate correlation with the HDRS (r = 0.48) in this study.
a). Young Mania Rating Scale (YMRS)
The 11-item YMRS is a clinician-rated assessment of manic symptoms experienced during the previous week (Young et al., 1978). The total score is 60; patients with a total score of 0 to 12 are usually in remission; 13 to 19 are moderate, and scores > 20 usually indicate a full manic episode by DSM-IV criteria (Lukasiewicz et al., 2013). The YMRS has been translated into Chinese and has adequate inter-rater reliability (κ = 0.93) and concurrent validity (significantly correlation with days hospitalized) (Hwu, 1999). The inter-rater reliability of the YMRS in the present study was high (κ = 0.85).
a). Altman Self Rating Mania Scale (ASRM)
The ASRM (Altman et al., 1997; E.G. 2001) is self-report measure of 5 (hypo)mania symptoms rated on 5-point Likert scales over the past a week. Five items are summed to get a total score. A cutoff score of 6 or higher indicates a high probability of a manic or hypomanic condition (sensitivity: 85.5%, specificity: 87.3%). The ASRM was translated into Chinese and demonstrated acceptable internal consistency in this study (Cronbach’s α= 0.65), with a significant but low correlation with total scores on the YMRS (r = 0.28, p <0.001), suggesting that clinically observed mania and self-reported mania had minimal overlap in this study.
2.4. Statistical analysis
Data were analyzed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics for the demographic variables, the SRM-5, BIPQ, HDRS, DASS-depression, YMRS, and ASRM scores were first examined. Pearson correlations between the scale scores were examined. Then, multiple regression analyses were used to test whether each IP subscale (i.e., Consequence, Timeline, Personal Control, Treatment Control, Identity, Concern, Comprehension, Emotional Response) and SRM-5 scores was related to the mood symptom variables. The mood symptom measures included clinician-rated (YMRS, HDRS) and self-reported (DASS-depression, ASRM) depressive and hypomanic/manioc symptoms, respectively.
As exploratory analyses, we analyzed the interaction between social rhythms and IPs on the same mood outcomes. To avoid multiple comparisons, we examined an unfavorable IP variable and a favorable IPs variable for each participant. The PROCESS macro within SPSS was used to conduct the moderation analyses of favorable and unfavorable IPs (separately) with SRM-5 scores on mood symptoms (Hayes, 2017). Based on existing evidence in healthy samples (Monk et al., 2002), we classified participants as high in social rhythm disturbances (1 SD below the sample mean) or low in social rhythm disturbances (1 SD above the sample mean).
3. Results
3.1. Demographic characteristics
Of the 154 eligible participants, 131 (85.1%) completed the study. The mean age was 38.71 ± 13.65 (SD); most patients were female, unmarried, unemployed, and college-educated. Most had been diagnosed with BD-II, had never been hospitalized, and had been referred to the study from outpatient services (see Table 1).
Table 1.
Sociodemographic and clinical characteristics, illness perceptions, social rhythm stability, and mood symptoms (N = 131).
| Variables | Mean ± SD;% |
|---|---|
|
| |
| Age (years) | 38.71 ± 13.65 |
| Age at bipolar disorder onset (years) | 29.96 ± 12.30 |
| Female,% | 54.2 |
| Married,% | 45.0 |
| Employed,% | 42.7 |
| Education> 12 years,% | 60.3 |
| Outpatient,% | 78.6 |
| Diagnosis subtypes | |
| Bipolar I,% | 31.3 |
| Bipolar II,% | 68.7 |
| Illness duration (years) | 7.69 ± 7.90 |
| Hospitalizations, NO. | 1.06 ± 2.40 |
| Illness Perceptions (0–10) | |
| Unfavorable illness perceptions | 6.92 ± 1.74 |
| Consequence | 6.57 ± 2.40 |
| Timeline | 6.59 ± 2.66 |
| Identity | 6.52 ± 2.41 |
| Concern | 7.38 ± 2.50 |
| Emotional response | 7.53 ± 2.24 |
| Favorable illness perceptions | 6.32 ± 1.89 |
| Personal control | 5.88 ± 2.39 |
| Treatment control | 6.55 ± 2.29 |
| Comprehension | 6.53 ± 2.39 |
| Social rhythm (SRM)(0–5) | 2.69 ± 2.10 |
| Mood Symptoms | |
| HDRS (0–52) | 8.80 ± 3.61 |
| YMRS (0–60) | 9.50 ± 3.01 |
| DASS-depression (0–21) | 8.50 ± 6.21 |
| ASRM (0–20) | 4.28 ± 3.49 |
Abbreviations: SRM, Social Rhythm Metric; HDRS, Hamilton Depression Rating Scale; YMRS, Young Mania Rating Scale; DASS, Depression Anxiety Stress Scales; ASRM, Altman Self Rating Mania Scale.
3.2. Patients’ illness perceptions, social rhythm, and mood symptoms
The mean BIPQ subscale item scores ranged from 5.88–7.53. The highest scores were recorded for emotional response (an unfavorable item), and the lowest for personal control (a favorable item). The mean score for unfavorable IPs were significantly higher than the score for favorable IPs (M = 6.92, SD=1.74 versus M = 6.32, SD=1.89, respectively; t = −2.68, p=.008). The mean score on the SRM-5 was 2.69 (SD= 2.10) (see Table 1).
3.3. The associations of illness perceptions, social rhythm, and mood symptoms
Social rhythm stability scores were not associated with either favorable or unfavorable IPs or patient- or clinician-rated mood symptoms. For clinician-rated mood assessments, two unfavorable IPs – consequence and identity – were positively associated with depression, and all 3 favorable IPs – personal and treatment control, and comprehension – were negatively associated with depression. Personal control was the only IP associated (negatively) with clinician-rated manic symptoms.
For patient-rated mood assessments, all IPs were moderately associated with depression, except Concern (see Table 2). All three favorable IPs were negatively associated with depression, and all of the unfavorable IPs - Consequence, Timeline, Identity, and Emotional response - were positively associated with patient-reported depression. None of the IPs were associated with patient-rated manic symptoms.
Table 2.
Correlations among illness perceptions, social rhythm, and mood symptoms (N = 131).
| Variables | SRM | HDRS | YMRS | DASS-Depression | ASRM |
|---|---|---|---|---|---|
|
| |||||
| Illness Perceptions | |||||
| Consequence | −0.15 | .24** | .09 | 0.39** | .02 |
| Timeline | −0.09 | .13 | .10 | 0.27** | .07 |
| Personal control | −0.03 | −0.37** | −0.33** | −0.46** | .06 |
| Treatment control | .02 | −0.21* | −0.146 | −0.35** | −0.09 |
| Identity | −0.15 | .21* | .05 | 0.38** | .11 |
| Concern | −0.02 | −0.03 | −0.03 | −0.01 | .01 |
| Comprehension | .04 | −0.24** | −0.13 | −0.32** | .14 |
| Emotional response | −0.03 | .14 | 0.06 | 0.31** | .08 |
| SRM | 1 | .01 | −0.05 | .16 | −0.04 |
Note.
Abbreviations: SRM, Social Rhythm Metric; HDRS, Hamilton Depression Rating Scale; YMRS, Young Mania Rating Scale; DASS, Depression Anxiety Stress Scales; ASRM, Altman Self Rating Mania Scale.
p <.05.
p<.01.
In multiple regression analyses controlling for each of IPs and SRM scores, only personal control was associated with clinician-assessed depressive and manic symptoms. Personal control, treatment control, and emotional response were each significantly associated with patient-rated depression symptoms. Comprehension was the only IP significantly associated with patient-rated manic symptoms (see Table 3).
Table 3.
The associations between illness perceptions and social rhythm stability on mood symptoms (N = 131).
| HDRS | YMRS | DASS-Depression | ASRM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | B | t | p | B | t | p | B | t | p | B | t | p |
|
| ||||||||||||
| Constant | 10.28 | 5.97 | .00 | 11.92 | 7.84 | .00 | 8.6 | 3.30 | .00 | 2.16 | 1.20 | .23 |
| SRM | .08 | .53 | .60 | −0.08 | −0.61 | .54 | −0.01 | −0.03 | .97 | −0.02 | −0.15 | .88 |
| Consequence | .05 | .29 | .77 | −0.03 | −0.17 | .87 | .25 | .92 | .36 | −0.11 | −0.57 | .57 |
| Timeline | .01 | .10 | .92 | .01 | .08 | .94 | .17 | .82 | .41 | .17 | .84 | .41 |
| Personal control | −0.46 | −2.99 | .00 | −0.45 | −3.30 | .00 | −0.72 | −3.06 | .00 | .12 | .75 | .45 |
| Treatment control | −0.08 | −0.50 | .62 | −0.07 | −0.53 | .60 | −0.63 | −2.61 | .01 | −0.33 | −1.97 | .05 |
| Identity | .18 | .98 | .33 | .05 | .34 | .74 | .39 | 1.45 | .15 | .21 | 1.10 | .27 |
| Concern | .10 | .63 | .53 | .05 | .37 | .72 | −0.06 | −0.23 | .82 | −0.24 | −1.41 | .16 |
| Comprehension | −0.15 | −0.89 | .38 | .08 | .53 | .60 | −0.10 | −0.38 | .71 | .40 | 2.32 | .02 |
| Emotional response | .02 | .11 | .91 | −0.03 | −0.23 | .82 | .53 | 2.16 | .03 | .18 | 1.07 | .27 |
Abbreviations: HDRS, Hamilton Depression Rating Scale; YMRS, Young Mania Rating Scale; DASS, Depression Anxiety Stress Scales; ASRM, Altman Self Rating Mania Scale; SRM, Social Rhythm Metric.
Note.
p < .05
p <.01.
We then examined the interaction between favorable and unfavorable IPs (separately) with social rhythm stability on mood symptoms. These analyses revealed a significant interaction between unfavorable IPs and social rhythm scores on clinician-rated mania scores (b=−0.21, SE=0.08, p=.007; see Fig. 1). For patients with low social rhythm scores (i.e., greater social rhythm disturbances), unfavorable IPs were associated with more severe manic symptoms (b = 0.35, SE=0.19, p = .07). The association was reversed for patients with high social rhythm scores (i.e., low rhythm disturbances), such that unfavorable IPs were associated with lower clinician-rated manic symptoms (b=−0.53, SE=0.25, p=.04). There was no interaction of unfavorable IPs and social rhythm scores on clinician-rated depressive symptoms or self-reported manic symptoms or depressive symptoms. There was no interaction between favorable IPs and social rhythms on any of the mood variables.
Fig. 1.
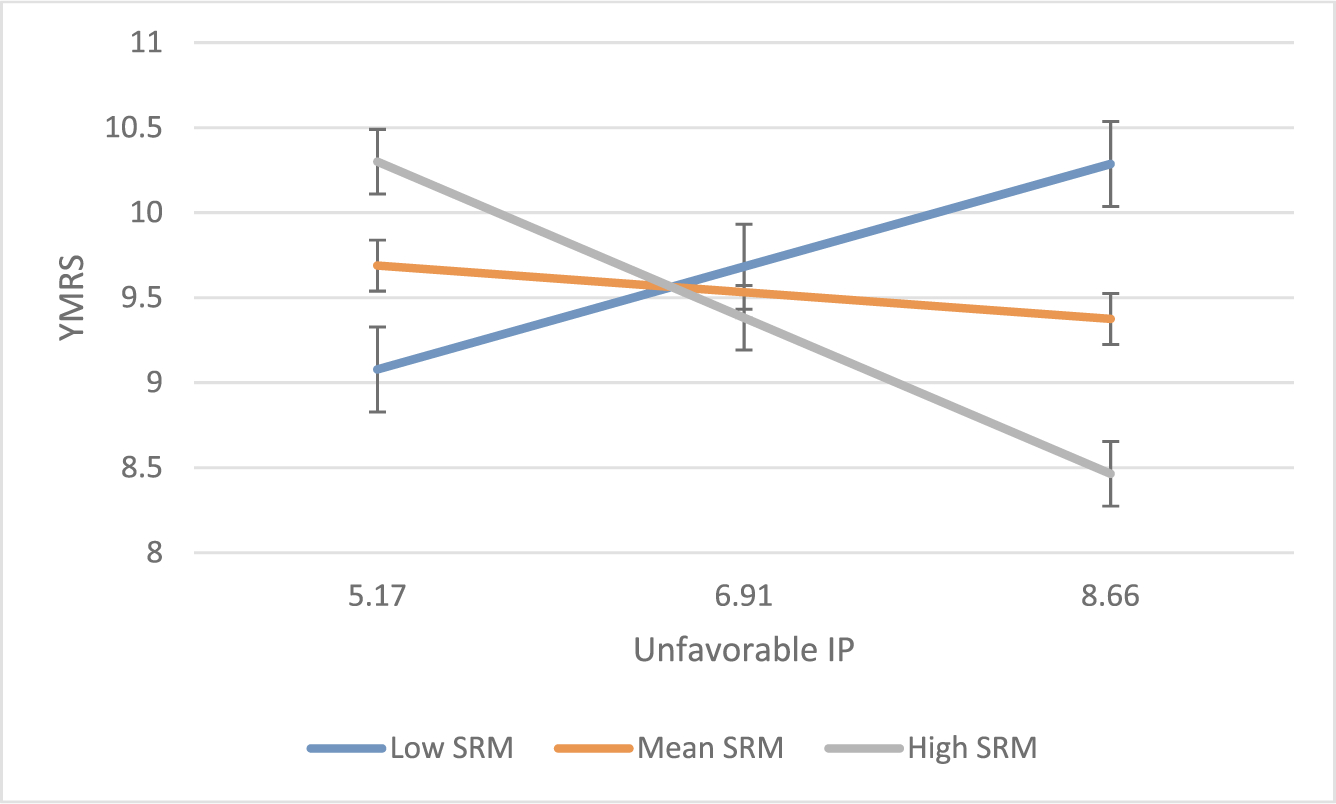
Interaction of unfavorable illness perceptions and social rhythm stability on manic symptoms
Note. Low and High SRM refer to +/− 1 SD from the mean, respectively. Standard error bars = +/− 1 standard error of the mean. IP = illness perception; SRM = Social Rhythm Metric; YMRS = Young Mania Rating Scale.
4. Discussion
To our knowledge, this is the first study to document a relationship between illness beliefs and concurrent mood symptoms in patients with BD. We found that beliefs about personal control, controlling for all other IPs and social rhythm, was the strongest IP associated with clinician-rated mania and depression and patient-rated depression. A similar finding emerged in a study of anxiety patients (Yap et al., 2019), which found that personal control and biological illness attributions were significant predictors of anxiety symptoms. Thus, patients who perceive greater control over their illness may have stronger confidence to manage their symptoms or may believe they are able to use their experience and skills to improve their symptoms (Scerri et al., 2019; Wisting et al., 2019; Yang et al., 2018). Our findings are in line with previous research on different medical conditions (Sawyer et al., 2019) suggesting that favorable IPs play a critical role in many health outcomes, including treatment adherence, symptom control, perceived stress, and quality of life. Alternatively, unfavorable IPs can hinder recovery and illness management efforts.
Although the social rhythm scores in this sample were more dysregulated than scores observed in two healthy control samples (Monk et al., 2002), there was lack of association between social rhythm regularity and mood symptoms, which is inconsistent with the bulk of previous research (Abreu and Braganca, 2015; Alloy et al., 2017). Possibly, the short period of assessment (the previous week) compared to previous research with longitudinal follow-up (e.g., Shen et al., 2008) or objective assessments (e.g., actigraphic recording; Jones et al., 2005) may have limited our ability to observe this relationship. It is also possible that social rhythm regularity is more clearly associated with future than concurrent symptoms. Importantly, studies observing an association between social rhythm stability and future mood symptoms find that this relationship is moderated by specific personality factors or cognitive appraisal styles not measured in this study, such as reward hypersensitivity or hypomanic personality features (Alloy et al., 2015; Banks et al., 2016; Meyer and Maier, 2006).
Despite no direct relationship between social rhythms and mood symptoms, we found that social rhythm stability moderated the relationship between unfavorable IPs and clinician-rated manic symptoms. Patients with more negative IPs had higher levels of hypomania when their daily routines and sleep/wake cycles were irregular. Conversely, patients with more negative IPs had low hypomania scores when they kept consistent social rhythms. Together, these findings suggest that social rhythm regularity may not individually affect manic symptoms, but may moderate the effects of negative cognitions on symptom states. Thus, a person who has been sleeping consistently may wake up in the morning with negative thoughts, but these thoughts may be less potent in affecting mood than they might have been with irregular sleep. Because this interaction between the risk factor of IPs and the protective factor of social rhythms only held for hypomanic symptoms, it appears that IPs are associated with depressive symptoms independently of social rhythm habits. This study did not test the causal direction between these variables. Future research should investigate whether changes in patients’ social rhythm behaviors affect the influence of negative cognitions on the course of bipolar disorder.
Consistent with evidence from research in a variety of diseases (Berner et al., 2018; Miceli et al., 2019; Sawyer et al., 2019; Scerri et al., 2019; Subramaniam et al., 2018; Wisting et al., 2019; Yang et al., 2018), our findings suggest that IPs have a strong relationship with mood symptoms in patients with BD. A cognitive-behavioral approach to improving mood symptoms would emphasize cultivating favorable IPs in patients’ concerning their understanding of BD and its controllability, challenging unfavorable IPs about negative consequences of the illness, and increasing awareness of the strategy of maintaining regular social rhythms. Future research should investigate whether integrating techniques from cognitive behavioral therapy and interpersonal and social rhythm therapy (Haynes et al., 2016; Salcedo et al., 2016) could enhance patients’ positive cognitions as well as adaptive behaviors relevant to maintaining daily and nightly routines.
Limitations of this study are acknowledged. First, the findings may not generalize to more severely ill patients, such as those who have been hospitalized; the majority of the patients had bipolar II disorder. The low severity of symptoms may have limited the study’s power to detect associations between social rhythms and mood symptoms. Second, a cross-sectional research design limits our ability to interpret the causal direction of these associations. Third, as discussed above, the short period of social rhythm assessment may not reflect the patient’s ordinary habits over longer intervals. Fourth, the accuracy of self-reported measures, in particular the ASRM and SRM-5, are subject to social desirability effects. Individuals’ recognition and awareness of their manic symptoms may be limited (Aspiazu et al., 2010; Regeer et al., 2015). Additionally, we used the abbreviated SRM-5 as opposed to the original 17-item SRM, which may have limited our ability to detect more subtle variations in daily routines (e.g., exercise routines) that might be correlates of mood states.
5. Conclusion
This study firstly indicates that BD patients’ beliefs about their illness – notably, beliefs about personal control - are associated with their concurrent mood states. The relationships between unfavorable beliefs and manic symptoms may be buffered by the regularity of their daily and nightly routines. Thus, enhancing social rhythms in individuals with unfavorable IPs may lead to greater stabilization of manic or hypomanic symptoms. Examining how patients develop unfavorable IPs would inform the development of interventions to ameliorate the impact of these illness perceptions on the course of the illness.
Acknowledgments
We thank the institutions and patients for their participation in this study.
Funding
This study was supported by grant MOST 104–2314-B-006–047-MY3 from the Taiwan Ministry of Science and Technology.
Footnotes
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
References
- Abreu T, Braganca M, 2015. The bipolarity of light and dark: a review on bipolar disorder and circadian cycles. J. Affec. Disord. 185, 219–229. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Walshaw PD, Neeren AM, 2006. Cognitive vulnerability to unipolar and bipolar mood disorders. J. Soc. Clin. Psychol. 25, 726–754. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Boland EM, Ng TH, Whitehouse WG, Abramson LY, 2015. Low social rhythm regularity predicts first onset of bipolar spectrum disorders among at-risk individuals with reward hypersensitivity. J. Abnorm. Psychol. 124, 944–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloy LB, Ng TH, Titone MK, Boland EM, 2017. Circadian rhythm dysregulation in bipolar spectrum disorders. Curr. Psychiatry Rep. 19 (4), 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman EG, Hedeker D, Peterson JL, Davis JM, 1997. The Altman self-rating mania scale. Biol. Psychiatry 42 (10), 948–955. [DOI] [PubMed] [Google Scholar]
- Altman EG, Hedeker D, Peterson JL, Davis JM, 2001. A comparative evaluation of three self-rating scales for acute mania. Biol. Psychiatry 50 (6), 468–471. [DOI] [PubMed] [Google Scholar]
- Aspiazu S, Mosquera F, Ibañez B, Vega P, Barbeito S, López P, Ruiz de Azúa S, Ugarte A, Vieta E, González-Pinto A, 2010. Manic and depressive symptoms and insight in first episode psychosis. Psychiatry Res. 178 (3), 480–486. [DOI] [PubMed] [Google Scholar]
- Averous P, Charbonnier E, Lagouanelle-Simeoni MC, Prosperi A, Dany L, 2018. Illness perceptions and adherence in bipolar disorder: an exploratory study. Compr. Psychiatry 80, 109–115. [DOI] [PubMed] [Google Scholar]
- Banks FD, Lobban F, Fanshawe TR, Jones SH, 2016. Associations between circadian rhythm instability, appraisal style and mood in bipolar disorder. J. Affect. Disord. 203, 166–175. [DOI] [PubMed] [Google Scholar]
- Berner C, Erlacher L, Fenzl KH, Dorner TE, 2018. A cross-sectional study on self-reported physical and mental health-related quality of life in rheumatoid arthritis and the role of illness perception. Health Qual. Life Outcomes 16 (1), 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadbent E, Petrie KJ, Main J, Weinman J, 2006. The brief illness perception questionnaire. J. Psychosom. Res. 60 (6), 631–637. [DOI] [PubMed] [Google Scholar]
- Ehlers CL, Frank E, Kupfer DJ, 1988. Social zeitgebers and biological rhythms. Arch. Gen. Psychiatry 45, 948–952. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, 1978. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch. Gen. Psychiatry 35 (7), 837–844. [DOI] [PubMed] [Google Scholar]
- Etain B, Scott J, Cochet B, Bellivier F, Boudebesse C, Drancourt N, Henry C, 2018. A study of the real-world effectiveness of group psychoeducation for bipolar disorders: is change in illness perception a key mediator of benefit? J. Affect. Disord. 227, 713–720. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Isasi A, Echeburua E, Liminana JM, Gonzalez-Pinto A, 2014. Psychoeducation and cognitive-behavioral therapy for patients with refractory bipolar disorder: a 5-year controlled clinical trial. Eur. Psychiatry 29, 134–141. [DOI] [PubMed] [Google Scholar]
- Grandin LD, Alloy LB, Abramson LY, 2006. The social Zeitgeber theory, circadian rhythms, and mood disorders: review and evaluation. Clin. Psychol. Rev. 26 (6), 679–694. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Koch S, Chatzisarantis NLD, Orbell S, 2017. The common sense model of self-regulation: meta-analysis and test of a process model. Psychol. Bull. 143 (11), 1117–1154. 10.1037/bul0000118. [DOI] [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, 2008. Sleep and circadian rhythms in bipolar disorder: seeking synchrony, harmony, and regulation. Am. J. Psychiatry 165 (7), 820–829. [DOI] [PubMed] [Google Scholar]
- Hayes AF, 2017. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Publications. [Google Scholar]
- Haynes PL, Gengler D, Kelly M, 2016. Social rhythm therapies for mood disorders: an update. Curr. Psychiatry Rep. 18 (8), 75. 10.1007/s11920-016-0712-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JD, Crawford JR, 2005. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 44, 227–239. [DOI] [PubMed] [Google Scholar]
- Hsiao YL, Wu YS, Wu JY, Hsu MH, Chen HC, Lee SY, Lee IH, Yeh TL, Yang YK, Ko HC, Lu RB, 2009. Neuropsychological functions in patients with bipolar I and bipolar II disorder. Bipolar Disord. 11 (5), 547–554. 10.1111/j.1399-5618.2009.00723.x. [DOI] [PubMed] [Google Scholar]
- Hwu HG, 1999. Psychiatric Diagnosis Manual. Health Cultural Enterprise Cooperation, Taipei. [Google Scholar]
- Jones SH, Hare DJ, Evershed K, 2005. Actigraphic assessment of circadian activity and sleep patterns in bipolar disorder. Bipolar Disord. 7 (2), 176–186. [DOI] [PubMed] [Google Scholar]
- Jones SH, Smith G, Mulligan LD, Lobban F, Law H, Dunn G, Welford M, Kelly J, Mulligan J, Morrison AP, 2015. Recovery-focused cognitive–behavioural therapy for recent-onset bipolar disorder: randomised controlled pilot trial. Br. J. Psychiatry 206, 58–66. [DOI] [PubMed] [Google Scholar]
- Kato T, 2019. Current understanding of bipolar disorder: toward integration of biological basis and treatment strategies. Psychiatry Clin. Neurosci. 10.1111/pcn.12852. [DOI] [PubMed] [Google Scholar]
- Keck PE, 2004. Defining and improving response to treatment in patients with bipolar disorder. J. Clin. Psychiatry 65 (Suppl 15), 25–29. [PubMed] [Google Scholar]
- Krok D, Telka E, Zarzycka B, 2019. Illness perception and affective symptoms in gastrointestinal cancer patients: a moderated mediation analysis of meaning in life and coping. Psycho-Oncology 28, 1728–1734. 10.1002/pon.5157. [DOI] [PubMed] [Google Scholar]
- Lauder S, Chester A, Castle D, Dodd S, Gliddon E, Berk L, Chamberlain J, Klein B, Gilbert M, Austin DW, Berk M, 2015. A randomized head to head trial of MoodSwings.net.au: an internet-based self-help program for bipolar disorder. J. Affect. Disord. 171, 13–21. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Benyamini Y, Brownlee S, Diefenbach M, Leventhal E, Patrick-Miller L, Robitaille C, 1997. Illness representations: theoretical foundations. In: Petrie KJ, Weinman J (Eds.), Perceptions of Health and illness: Current research and Applications. Harwood Academic Publishers, Amsterdam, pp. 19–45. [Google Scholar]
- Leventhal H, Leventhal EA, Cameron L, 2001. Representations, procedures, and affect in illness self-regulation: a perceptual-cognitive model. In: Baum A, Revenson TA, Singer JE (Eds.), Handbook of Health Psychology. Lawrence Erlbaum, Mahwah, New Jersey, pp. 19–48. [Google Scholar]
- Lima IMM, Peckham AD, Johnson SL, 2018. Cognitive deficits in bipolar disorders: implications for emotion. Clin. Psychol. Rev. 59, 126–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YP, Chiu KM, Wang T−J, 2011. Reliability and validity of the Chinese version of the Brief Illness Perception Questionnaire for patients with coronary heart disease. J. Orient. Inst. Technol. 31, 145–155. [Google Scholar]
- Lobban F, Barrowclough C, Jones S, 2004. The impact of beliefs about mental health problems and coping on outcome in schizophrenia. Psychol. Med. 34, 1165–1176. [DOI] [PubMed] [Google Scholar]
- Lukasiewicz M, Gerard S, Besnard A, Falissard B, Perrin E, Sapin H, Tohen M, Reed C, Azorin JM, Emblem Study Group, 2013. Young Mania Rating Scale: how to interpret the numbers? Determination of a severity threshold and of the minimal clinically significant difference in the EMBLEM cohort. Int. J. Methods Psychiatr. Res. 22 (1), 46–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malkoff-Schwartz S, Frank E, Anderson B, Hlastala S, Luther J, Sherrill J, Houck PR, Kupfer D, 2000. Social rhythm disruption and stressful life events in the onset of bipolar and unipolar episodes. Psychol. Med. 30 (5), 1005–1016. [DOI] [PubMed] [Google Scholar]
- Malkoff-Schwartz S, Frank E, Anderson B, Sherrill JT, Siegel L, Patterson D, Kupfer DJ, 1998. Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: a preliminary investigation. Arch. Gen. Psychiatry 55 (8), 702–707. [DOI] [PubMed] [Google Scholar]
- Melo MCA, Abreu RLC, Neto VBL, de Bruin PFC, de Bruin VMS, 2017. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med. Rev. 34, 46–58. [DOI] [PubMed] [Google Scholar]
- Meyer TD, Maier S, 2006. Is there evidence for social rhythm instability in people at risk for affective disorders? Psychiatry Res. 141, 103–114. [DOI] [PubMed] [Google Scholar]
- Miceli J, Geller D, Tsung A, Hecht CL, Wang Y, Pathak R, Cheng H, Marsh W, Antoni M, Penedo F, Burke L, Ell K, Shen S, Steel J, 2019. Illness perceptions and perceived stress in patients with advanced gastrointestinal cancer. Psychooncology [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk TK, Flaherty JF, Frank E, Hoskinson K, Kupfer DJ, 1990. The social rhythm metric: an instrument to quantify the daily rhythms of life. J. Nerv. Ment. Dis. 178 (2), 120–126. [DOI] [PubMed] [Google Scholar]
- Monk TH, Frank E, Potts JM, Kupfer DJ, 2002. A simple way to measure daily lifestyle regularity. J. Sleep Res. 11 (3), 183–190. [DOI] [PubMed] [Google Scholar]
- Mosleh SM, Almalik MM, 2016. Illness perception and adherence to healthy behaviour in Jordanian coronary heart diseasepatients. Eur. J. Cardiovasc. Nurs. 15 (4), 223–230. [DOI] [PubMed] [Google Scholar]
- Moussa MT, Lovibond P, Laube R, 2001. Psychometric properties of a Chinese version of the 21-item Depression Anxiety Stress Scales (DASS-21). In: Report for New South Wales Transcultural Mental Health Centre, Cumberland Hospital. Sydney. [Google Scholar]
- Murray G, Harvey A, 2010. Circadian rhythms and sleep in bipolar disorder. Bipolar Disord. 12, 459–472. [DOI] [PubMed] [Google Scholar]
- Nováková M, Praško J, Látalová K, Sládek M, Sumová A, 2015. The circadian system of patients with bipolar disorder differs in episodes of mania and depression. Bipolar Disord. 17, 303–314. [DOI] [PubMed] [Google Scholar]
- Regeer EJ, Kupka RW, Have MT, Vollebergh W, Nolen WA, 2015. Low self-recognition and awareness of past hypomanic and manic episodes in the general population. Int. J. Bipolar Disord. 3 (1), 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R, Jackson RL, Salekin KL, Neumann CS, 2003. Assessing Axis I symptomatology on the SADS-C in two correctional samples: the validation of subscales and a screen for malingered presentations. J. Pers. Assess. 81 (3), 281–290. [DOI] [PubMed] [Google Scholar]
- Salcedo S, Gold AK, Sheikh S, Marcus PH, Nierenberg AA, Deckersbach T, Sylvia LG, 2016. Empirically supported psychosocial interventions for bipolar disorder: current state of the research. J Affect Disord. 201, 203–214. [DOI] [PubMed] [Google Scholar]
- Sawyer AT, Harris SL, Koenig HG, 2019. Illness perception and high readmission health outcomes. Health Psychol. 6 (1), 2055102919844504 Open 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen GH, Alloy LB, Abramson LY, Sylvia LG, 2008. Social rhythm regularity and the onset of affective episodes in bipolar spectrum individuals. Bipolar Disord 10 (4), 520–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scerri J, Saliba T, Saliba G, Scerri CA, Camilleri L, 2019. Illness perceptions, depression and anxiety in informal carers of persons with depression: a cross-sectional survey. Qual. Life Res. 28 (2), 451–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam M, Abdin E, Jeyagurunathan A, Chang S, Samari E, Shafie S, Wei KC, Verma S, Chong SA, 2018. Exploration of illness perception among patients with mental illness in a multi-ethnic Asian sample. Psychiatry Res. 267, 516–527. [DOI] [PubMed] [Google Scholar]
- Tiemensma J, Gaab E, Voorhaar M, Asijee G, Kaptein AA, 2016. Illness perceptions and coping determine quality of life in COPD patients. Int. J. Chron. Obstruct. Pulmon. Dis. 11, 2001–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisting L, Rø A, Skrivarhaug T, Dahl-Jørgensen K, Rø Ø, 2019. Disturbed eating, illness perceptions, and coping among adults with type 1 diabetes on intensified insulin treatment, and their associations with metabolic control. J Health Psychol [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Yang L, Winslow B, Taylor E, Pothier P, 2018. Health perception and adherence with blood pressure control among rural Chinese adults with hypertension. J. Adv. Nurs [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Yap CK, Wong MY, Lim KK, 2019. Illness perception of anxiety patients in primary care in Singapore. Indian J. Psychol. Med. 41 (1), 75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA, 1978. A rating scale for mania: reliability, validity and sensitivity. Br. J. Psychiatry 133, 429–435. [DOI] [PubMed] [Google Scholar]
- Zhang N, Fielding RS, Soong I, Chan KK, Lee C, Ng A, Sze WK, Tsang J, Lee V, Lam WW, 2017. Psychometric assessment of the Chinese version of the brief illness perception questionnaire in breast cancer survivors. PloS one 12 (3), e0174093.. 10.1371/journal.pone.0174093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng YP, Zhao JP, Phillips M, Liu JB, Cai MF, Sun SQ, Huang MF, 1988. Validity and reliability of the Chinese Hamilton Depression Rating Scale. Br. J. Psychiatry 152, 660–664. [DOI] [PubMed] [Google Scholar]


