Abstract
Background
Dengue is a major public health issue worldwide and severe dengue (SD) is life threatening. It is critical to triage patients with dengue infection in the early stage. However, there is limited knowledge on early indicators of SD. The objective of this study is to identify risk factors for the prognosis of SD and try to find out some potential predictive factors for SD from dengue fever (DF) in the early of infection.
Methods
The PubMed, Cochrane Library and Web of Science databases were searched for relevant studies from June 1999 to December 2020. The pooled odds ratio (OR) or standardized mean difference (SMD) with 95% confidence intervals (CI) of identified factors was calculated using a fixed or random effect model in the meta-analysis. Tests for heterogeneity, publication bias, subgroup analyses, meta-regression, and a sensitivity analysis were further performed.
Findings
A total of 6,848 candidate articles were retrieved, 87 studies with 35,184 DF and 8,173 SD cases met the eligibility criteria. A total of 64 factors were identified, including population and virus characteristics, clinical symptoms and signs, laboratory biomarkers, cytokines, and chemokines; of these factors, 34 were found to be significantly different between DF and SD, while the other 30 factors were not significantly different between the two groups after pooling the data from the relevant studies. Additionally, 9 factors were positive associated with SD within 7 days after illness when the timing subgroup analysis were performed.
Conclusions
Practical factors and biomarkers for the identification of SD were established, which will be helpful for a prompt diagnosis and early effective treatment for those at greatest risk. These outcomes also enhance our knowledge of the clinical manifestations and pathogenesis of SD.
Introduction
Dengue disease is a mosquito-borne viral infection caused by the dengue virus (DENV). Patients infected with DENV have a wide spectrum of clinical manifestations, ranging from asymptomatic to dengue fever (DF) or severe dengue (SD), including dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS) [1, 2]. The World Health Organization (WHO) estimated that approximately 2.5 billion people living in dengue-endemic countries [3]. With an increasing incidence of DENV infections each year, it was estimated that there were 390 million dengue infections per year, of which 96 million manifested symptomatically [4]; additionally, it was estimated that there were 565,900 disabilities and 9110 deaths in 2013 [5]. The first licensed recombinant, live-attenuated dengue vaccine (Dengvaxia) recently became clinically available. However, a high risk of adverse outcomes was found among vaccinated individuals who had not been previously exposed to dengue [6, 7]. Severe and fatal cases were consistently reported in some endemic areas, such as Southeast Asia, the Western Pacific, and the Americas [8–10]. It has been reported that the DSS mortality is 50 times higher than that of DF [11], and SD has been a leading cause of serious illness and death among children in some Asian and Latin American countries [3]. Previous data showed that the SD mortality would decrease from more than 20% to less than 1% if SD were identified and properly treated in a timely fashion [3]. Hence, the early prediction and recognition of severe cases are critical for dengue disease management.
To help clinicians evaluate the likelihood of severe disease, risk factors for SD have been reported, such as secondary infection, gastrointestinal pain, vomiting, diarrhea, intravascular leakage and bleeding [12]. Efforts have been consistently made to identify predictive markers for SD [13–15]. Although dengue with warning signs (WS) was referenced in the newly updated WHO guideline [1], a multicenter study reported that approximately 30% of adults with DF had WS and only 10% developed SD [16], while another study showed that the sensitivity and specificity of WS were 59–98% and 41–99%, respectively, when they were used to identify SD [17]. Numerous potential markers for SD have been reported but some have been inconclusive [18–20]. To distinguish SD from DF in the early of infection and try to find out some potential predictive factors, we conducted this systematic review and meta-analysis.
Methods
Literature search and study selection
This systematic review was performed according to the recommendations of the PRISMA statement [21] (S1 Checklist).
The PubMed, Cochrane Library, and Web of Science online databases were systematically searched June 1999 to December 2020. The search was performed using the following query: (dengue) and ((shock) or (severe) or (severity) or (dss) or (dhf) or (dengue shock syndrome) or (dengue haemorrhage fever)). Moreover, the references of included studies and relevant reviews were manually retrieved to collect more studies.
Studies that met the following criteria were included: (1) dengue infections were confirmed by laboratory tests; (2) there were SD and DF groups with characteristic data, such as epidemiological factors, clinical signs, and laboratory parameters; (3) the studies provided original data; (4) the papers were written in English.
Studies meeting the following criteria were excluded: (1) papers with unavailable full texts or data; (2) case reports, reviews, animal studies and in vitro studies; (3) genetic studies; (4) duplicate publications.
All titles and abstracts were first independently reviewed by two authors. The full texts of studies that were potentially eligible to be included were obtained for further reading and scrutiny. Disagreements were resolved by consulting a third author.
Quality assessment
The Newcastle-Ottawa quality assessment scale (NOS) [22] was used to evaluate the quality of the included studies. Scores were determined by nine metrics: data collection, assignment of the patients, inclusion criteria, exclusion criteria, characteristics of the patient population, interpretation of other characteristics, methodological quality, interpretation of factors and dengue diagnosis. Two authors independently assessed the quality of each original study. Studies were defined as being of low, intermediate, and high quality according to NOS scores of 1–3, 4–6, and 7–9, respectively. The scoring system is available in S1 Table.
Data extraction
Data were independently extracted by two authors if that were presented at least two studies, and the following information was included: the first author, publication date, country/city of origin, patient recruitment period, age of patients, data type, diagnostic method, criteria for diagnosis, sampling time, quality score, and number of cases. DHF, DSS, and SD were defined collectively as SD in this study. Data that could not be reliably extracted or that overlapped were excluded. When duplication was noted, the largest data set was chosen for the meta-analysis. The information is recorded in S2 Table.
Statistical analyses
A meta-analysis for predictive factors was carried out using STATA version 12.0 (STATA Corporation, College Station, TX, USA). Heterogeneity was assessed using the Cochran Q test with its corresponding p values and I2 statistic. I2 values of 25%, 50%, and 75% indicated low, moderate, and high levels of heterogeneity, respectively. Heterogeneity was considered statistically significant if the p value was ≤0.10 and I2 was >40% [23, 24]. A random-effect model was used when there was significant heterogeneity; otherwise, a fixed-effect model was used [25]. Dichotomous and continuous variables were analyzed by calculating the pooled odds ratio (OR) and standardized mean difference (SMD), respectively, with 95% confidence intervals (CI) using a fixed or random effect model.
To explore the potential sources of high heterogeneity among the studies, subgroup analyses and meta-regression were performed for sampling time (≤7 days after onset), the population, data type, criteria for diagnosis, area of origin and study quality, when there were more than ten datasets included [26, 27]. The effect of co-variants was considered significant when p was < 0.05 or the 95% CI did not overlap with the original data.
Publication bias was assessed by Begg’s funnel plot and Egger’s linear regression test when there were more than ten datasets included [28, 29], and the trim and fill method from Duvall and Tweedie was used by adding studies that appeared to be missing to enhance the symmetry when publication bias was found (p<0.05) [30]. The adjusted pooled effect size and 95% CI were computed after adding the potential missing studies. In addition, the sensitivity analysis was carried out using the leave-one-out method to test whether a potential outlier within the included studies could have influenced the meta-analysis summary effects [31].
Previous studies showed that dengue virus was an important cause of childhood and adult morbidity in Asian and Latin American countries [32] and people with African ancestry were less susceptible to the severe manifestations of dengue infection [33, 34]. Therefore, the subgroups of Asia and America were compared in the Meta-analysis. And sensitivity and sub-analysis of co-variables on the summary effect and heterogeneity were performed for factors with more than ten studies included using the one study omitting analyses to test whether a potential outlier within included studies could have influenced the meta-analysis summary effects [31].
Results
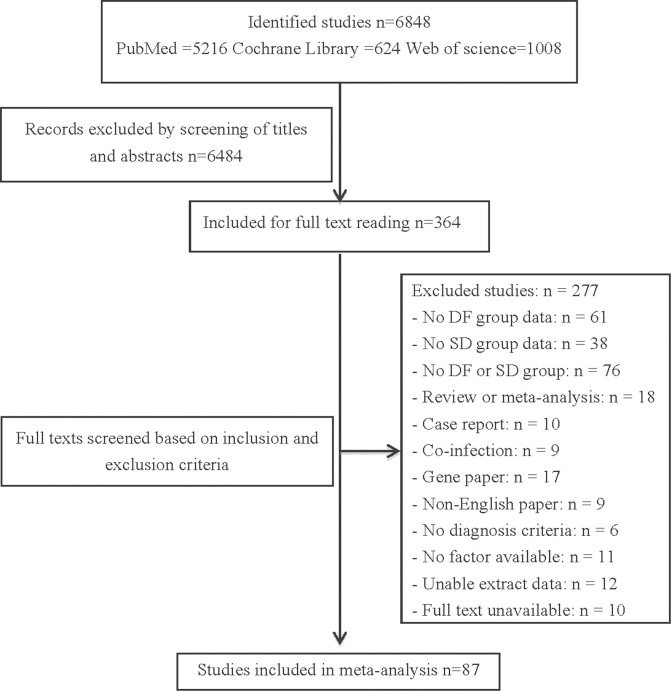
A total of 6848 studies were identified after the initial search of the databases. After the screening of titles and abstracts, 364 potentially relevant papers were retrieved for detailed assessment, and 87 studies with 35,184 DF and 8,173 SD cases were included in the meta-analysis based on the inclusion and exclusion criteria. A total of 34 factors were found to be significantly different between DF and SD, age, diabetes history, secondary infection, seroDENV-2/3, bleeding, vomiting, ascites, pleural effusion, lethargy and petechiae, were positive associated with SD; HCT, ALT, AST, CK, BUN, LDH, IL-10, IL-8, sVCAM-1, and IP-10 were increasing but total protein, albumin and PLT were decreasing in level during SD. The study selection flow diagram is depicted in Fig 1.
Fig 1. Flow diagram of the study selection process.
Identification of studies
A total of 87 studies published from January 2000 to December 2020 were ultimately included in the study, and 66 (75.9%), 19 (21.8%), 1 (1.1%), and 1 (1.1%) study originated from Asia, the Americas, Europe, and Oceania, respectively. The WHO 1997 [2], WHO 2009 [1], WHO 2011 [35], WHO 1999b [36] and Brazilian guidelines [37] were used for identifying SD in 53 (60.9%), 25 (28.7%), 5 (5.7%), 1 (1.1%) and 3 (3.4%) studies, respectively. The final articles consisted of 53 (60.9%) retrospective, 27 (31.0%) prospective and 7 (8.0%) cross-sectional studies. Based on the NOS scores, 30(34.5%), 55 (63.2%) and 2 (2.3%) studies were of high, inter-mediate and low quality, respectively (S2 Table). Twenty-two (25.3%) studies reported a population of children, 27 (31.0%) reported adult populations, 31 (35.6%) reported both and 7 (8.0%) did not describe the populations. Fifty-one studies stated the sampling time, of which 23 stated it was less than 7 days after onset when the samples were drawn. The details of the included studies are presented in S3 Table. Twenty-eight factors (I2>40%) were analyzed for sensitivity and 24 factors were heterogeneous in the subgroup meta-analysis except age and gender in population, hepatomegaly, vomit, and pleural effusion in sampling time (S4 Table).
Systematic analysis and meta-analysis
The data sets for 64 factors were extracted from at least two studies. Thirty-four factors were significantly different between patients with DF and those with SD (Table 1), and 30 factors were not correlated with severity (S5 Table). A total of 21 factors were identified and 9 revealed positive association with SD within 7 days after onset in the timing subgroup analysis (S5 Table).
Table 1. Positive factors associated with SD.
| Factors | Studies included | Sample size (SD/DF) | Model | Association with SD | Test of Heterogeneity | Publication bias p-value | |||
|---|---|---|---|---|---|---|---|---|---|
| OR/SMD (95% CI) | p-value | I2 (%) | p-value | Egger’s | Begg’s | ||||
| Age | 46 | 2655/11000 | Random | SMD = 0.151 | 0.017 | 82.4 | <0.001 | 0.763 | 0.507 |
| (0.027–0.275) | |||||||||
| Diabetes | 9 | 1560/4844 | Random | OR = 4.418 | <0.001 | 80.4 | <0.001 | - | - |
| (2.698–7.232) | |||||||||
| Secondary infection | 22 | 3140/21149 | Random | OR = 2.693 | <0.001 | 67.3 | <0.001 | 0.358 | 0.463 |
| (2.083–3.481) | |||||||||
| SeroDENV-1 | 15 | 2691/4462 | Random | OR = 0.709 | 0.048 | 73.4 | <0.001 | 0.023 | 0.921 |
| (0.504–0.997) | |||||||||
| SeroDENV-2 | 17 | 2690/4814 | Random | OR = 1.843 | 0.001 | 76.2 | <0.001 | 0.239 | 0.753 |
| (1.269–2.678) | |||||||||
| SeroDENV-3 | 16 | 2597/4424 | Random | OR = 0.694 | 0.037 | 54.9 | 0.004 | 0.332 | 0.113 |
| (0.492–0.979) | |||||||||
| Day of illness | 21 | 1218/3220 | Random | SMD = 0.614 | <0.001 | 91.0 | <0.001 | 0.084 | 0.097 |
| (0.346–0.882) | |||||||||
| Lethargy | 8 | 812/29412 | Random | OR = 2.563 | <0.001 | 83.6 | <0.001 | - | - |
| (1.517–4.329) | |||||||||
| Vomit | 26 | 2235/9417 | Random | OR = 1.533 | 0.001 | 76.2 | <0.001 | 0.107 | 0.107 |
| (1.203–1.953) | |||||||||
| Persistent vomiting | 3 | 65/813 | Fixed | OR = 5.569 | <0.001 | 0.0 | 0.835 | - | - |
| (3.041–10.200) | |||||||||
| Diarrhea | 16 | 1123/3750 | Fixed | OR = 1.245 | 0.042 | 15.8 | 0.273 | 0.383 | 0.096 |
| (1.008–1.537) | |||||||||
| Abdominal pain | 33 | 2774/27727 | Random | OR = 1.850 | <0.001 | 77.7 | <0.001 | 0.052 | 0.119 |
| (1.466–2.335) | |||||||||
| Hepatomegaly | 17 | 1601/20581 | Random | OR = 4.403 | <0.001 | 63.9 | <0.001 | 0.135 | 0.592 |
| (3.016–6.430) | |||||||||
| Petechiae | 19 | 1148/3529 | Random | OR = 2.508 | <0.001 | 57.2 | 0.001 | 0.101 | 0.093 |
| (1.720–3.655) | |||||||||
| Bleeding | 32 | 2748/27000 | Random | OR = 6.856 | <0.001 | 89.9 | <0.001 | 0.768 | 0.168 |
| (4.160–11.300) | |||||||||
| Pleural effusion | 19 | 1751/3666 | Random | OR = 15.836 | <0.001 | 87.3 | <0.001 | 0.002 | 0.529 |
| (6.974–35.967) | |||||||||
| Ascites | 12 | 1271/2213 | Random | OR = 24.299 | <0.001 | 90.9 | <0.001 | 0.001 | 0.837 |
| (4.337–136.138) | |||||||||
| Hypotension | 11 | 714/1804 | Random | OR = 3.692 | 0.001 | 69.7 | <0.001 | 0.006 | 0.062 |
| (1.670–8.162) | |||||||||
| HCT | 27 | 1791/7612 | Random | SMD = 0.327 | 0.003 | 91.8 | <0.001 | 0.699 | 0.404 |
| (0.109–0.546) | |||||||||
| High HCT * | 7 | 607/18180 | Random | OR = 12.389 | <0.001 | 81.2 | <0.001 | - | - |
| (6.091–25.199) | |||||||||
| PLT | 38 | 2586/26476 | Random | SMD = -1.070 | <0.001 | 94.3 | <0.001 | 0.01 | 0.012 |
| (-1.293- -0.848) | |||||||||
| Low PLT* | 12 | 728/1238 | Random | OR = 8.146 | <0.001 | 84.8 | <0.001 | 0.063 | 0.161 |
| (3.374–19.665) | |||||||||
| ALT | 30 | 1920/23694 | Random | SMD = 1.007 | 0.001 | 99.1 | <0.001 | 0.245 | 0.003 |
| (0.386–1.627) | |||||||||
| High ALT* | 8 | 528/1069 | Random | OR = 4.030 | <0.001 | 66.1 | 0.004 | - | - |
| (2.408–6.747) | |||||||||
| AST | 29 | 1888/25527 | Random | SMD = 1.278 | <0.001 | 99.2 | <0.001 | 0.338 | 0.011 |
| (0.640–1.916) | |||||||||
| High AST | 4 | 129/366 | Fixed | OR = 4.053 | <0.001 | 0.0 | 0.774 | - | - |
| (2.255–7.287) | |||||||||
| CK | 4 | 65/404 | Random | SMD = 2.647 | 0.001 | 94.9 | <0.001 | - | - |
| (1.117–4.177) | |||||||||
| ALB | 13 | 972/21740 | Random | SMD = -0.767 | <0.001 | 86.8 | <0.001 | 0.006 | 0.008 |
| (-0.989- -0.544) | |||||||||
| Low ALB* | 2 | 54/161 | Fixed | OR = 20.601 | <0.001 | 12.6 | 0.285 | - | - |
| (4.441–95.562) | |||||||||
| TP | 5 | 484/3390 | Random | SMD = -0.271 | 0.003 | 60.4 | 0.039 | - | - |
| (-0.449 - -0.093) | |||||||||
| Low TP* | 2 | 28/72 | Fixed | OR = 10.993 | <0.001 | 0.0 | 0.443 | - | - |
| (2.949–40.978) | |||||||||
| Proteinuria | 2 | 528/1098 | Random | OR = 3.681 | <0.001 | 80.1 | 0.025 | - | - |
| (2.038–6.649) | |||||||||
| BUN | 4 | 361/2966 | Random | SMD = 1.301 | 0.009 | 97.8 | 0.025 | - | - |
| (0.330–2.273) | |||||||||
| LDH | 5 | 111/469 | Random | SMD = 1.873 | 0.008 | 96.6 | 0.025 | - | - |
| (0.494–3.253) | |||||||||
| PT | 6 | 242/2611 | Random | SMD = 0.781 | 0.006 | 90.6 | <0.001 | - | - |
| (0.219–1.343) | |||||||||
| APTT | 6 | 229/2089 | Random | SMD = 0.529 | 0.032 | 80.6 | <0.001 | - | - |
| (0.046–1.013) | |||||||||
| IL-10 | 6 | 289/425 | Random | SMD = 0.868 | 0.011 | 92.7 | <0.001 | - | - |
| (0.197–1.539) | |||||||||
| IL-8 | 3 | 127/151 | Random | SMD = 3.337 | 0.004 | 97.3 | <0.001 | - | - |
| (1.059–5.615) | |||||||||
| sVCAM-1 | 2 | 37/70 | Fixed | SMD = 1.297 | <0.001 | 0.0 | 0.441 | - | - |
| (0.856–1.737) | |||||||||
| IP-10 | 2 | 92/86 | Random | SMD = 0.531 | 0.027 | 52.9 | 0.145 | - | - |
| (0.059–1.004) | |||||||||
Pooled odds ratios (OR) or standardized mean difference (SMD) with corresponding 95% confidence intervals (95% CI) of the published results were calculated when the factor was included in more than one study.
* Dichotomous variables
Characteristics of the populations
Age, gender, and diabetes history were identified. After pooling relevant studies, age and diabetes history were positively associated with SD in 46 (SMD = 0.151, 95% CI: 0.027–0.275, p = 0.017) and 9 (OR = 4.418, 95% CI: 2.698–7.232, p<0.001) studies with high heterogeneity (I2 = 82.4%, p<0.001; I2 = 80.4%, p<0.001), respectively. Furthermore, meta-regression analysis revealed that the population and sampling time contributed to the heterogeneity of age. However, based on the subgroup analyses, childhood had no correlation with severity in 10 studies (SMD = 0.004, 95% CI: -0.096–0.104, p = 0.679) without heterogeneity (I2 = 0.0%, p = 0.679); and age revealed no correlation with severity in 5 studies (SMD = 0.048, 95%CI: -0.192–0.095, p = 0.510) with low heterogeneity (I2 = 10.5%, p = 0.346) within 7 days after onset. Additionally, gender did not correlate with SD (S6 Table). Summary effects did not change significantly when the leave-one-out analyses were conducted.
Viral characteristics
Eighteen studies encompassing 7,659 cases reporting the dengue serotypes together with their severity were obtained, 13 of which originated from Asia and 5 from the Americas. The prevalence rates of DENV-1, DENV-2, DENV-3, and DENV-4 were 39.9%, 29.1%, 19.6% and 11.3%, respectively. A similar seroprevalence distribution in 6,847 cases in Asia was found, with rates of 37.1%, 31.6%, 19.8% and 11.6%, respectively. In contrast, in 812 cases from the Americas, the seroprevalence rates were 63.9%, 8.3%, 18.2% and 9.6%, respectively.
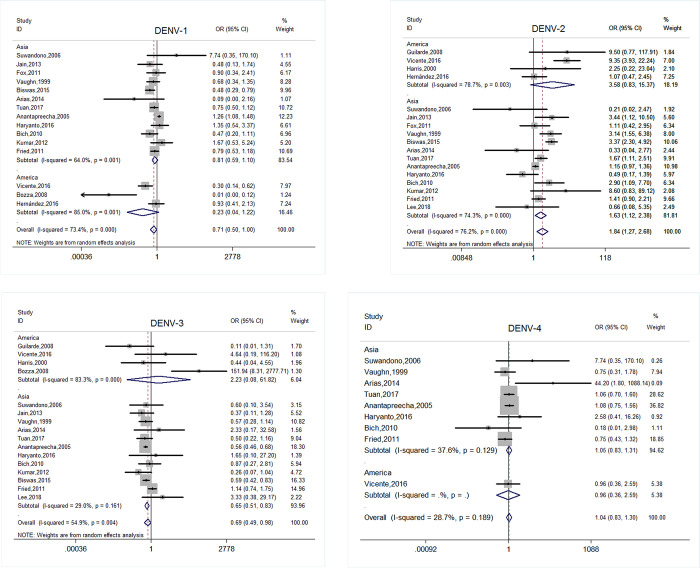
After pooling 17 studies, DENV-2 was positively associated with SD (OR = 1.843, 95% CI: 1.269–2.678, p = 0.001), whereas DENV-1 and DENV-3 had a negative association in 15(OR = 0.709, 95% CI: 0.504–0.997, p = 0.048) and 16(OR = 0.694, 95% CI: 0.492–0.979, p = 0.037) studies, respectively. However, in the subgroup analysis of epidemic areas, DENV-1 revealed an inconsistent result with SD in Asia (OR = 0.810, 95% CI: 0.594–1.104, p = 0.182) and in the Americas (OR = 0.230, 95% CI: 0.044–1.215, p = 0.084); DENV-3 revealed a similar result with SD (OR = 0.650, 95% CI: 0.511–0.828, p<0.001) in Asia but opposite in the Americas (OR = 2.226, 95% CI: 0.080–61.821, p = 0.637). DENV-4 showed no significant difference between the two groups in 9 studies. The details are presented in Fig 2. In addition, the pooled odds ratio of secondary infection in 22 studies revealed a positive association with SD (OR = 2.693, 95% CI: 2.083–3.481, p<0.001). Also, it revealed a consistent association with SD in 4 studies (OR = 2.448, 95% CI: 0.955–6.277, p = 0.062) within 7 days after onset. Excluding individual studies did not change the summary effects significantly.
Fig 2. Forest plot of the subgroup analysis of the area of origin for serotypes of DENV (DF vs SD, OR = odds ratio).
A: DENV-1; B: DENV-2; C: DENV-3; D: DENV-4.
Clinical manifestations
Days of illness was observed to be much longer in SD (SMD = 0.614, 95% CI: 0.346–0.882, p = 0.000) after pooling 21 studies. Lethargy/dizziness had a positive association with SD (OR = 2.563, 95% CI: 1.517–4.329, p<0.001) after pooling data from 8 studies. Vomiting and abdominal pain were observed to be risk factors for SD in 26 (OR = 1.533, 95% CI: 1.203–1.953, p = 0.001) and 33 (OR = 1.850, 95% CI: 1.466–2.335, p<0.001) studies, respectively, with high heterogeneity. In particularly, persistent vomiting as one of the WS was referred to in 3 studies and had a strong positive pooled effect (OR = 5.569, 95% CI: 3.041–10.000, p<0.001). Diarrhea was also associated with SD in 16 studies (OR = 1.245, 95% CI: 1.008–1.537, p = 0.042) with low heterogeneity (I2 = 15.8%, p = 0.273). Additionally, hepatomegaly was highly correlated with SD in 17 studies (OR = 4.403, 95% CI: 3.016–6.430, p<0.001). Hepatomegaly revealed a similar association with SD in 2 (OR = 9.264, 95% CI: 7.034–12.201, p<0.001) studies with low heterogeneity (I2 = 0.0%, p = 0.402) within 7 days after onset. The high heterogeneity and summary effect did not change significantly when subgroup analyses of other covariables and leave-one-out analyses were conducted.
Bleeding signs
Skin rash, petechiae, hematemesis, melena, gum bleeding, epistaxis, and the tourniquet test were identified as bleeding signs in this study. Severe bleeding, including hematemesis, melena, gum bleeding, and epistaxis, had a strong association with SD (OR = 6.856, 95% CI: 4.160–11.300, p = 0.000) after pooling data from 32 studies. It showed a positive association with SD (OR = 8.106, 95% CI: 3.094–21.241, p<0.001) as well when the sampling time subgroup analysis was performed in 7 studies. Additionally, petechiae had a positive association (OR = 2.508, 95% CI: 1.720–3.655, p = 0.000) after pooling data from 19 studies with moderate heterogeneity (I2 = 57.2%, p = 0.001).
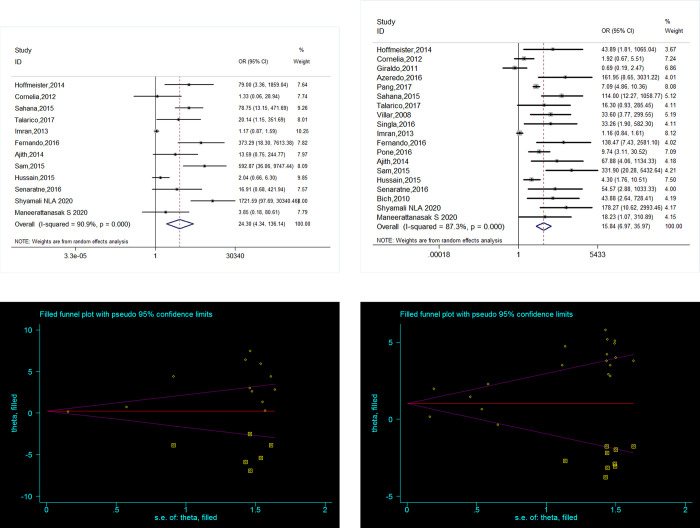
Plasma leakage
Pleural effusion and ascites had a strong association with SD after pooling data from 19 (OR = 15.838, 95% CI: 6.974–35.967, p<0.001) and 12 (OR = 24.299, 95% CI: 4.337–136.138, p<0.001) studies, respectively. However, there was publication bias in favor of positive studies according to Egger’s test (p<0.05) for both. Using the trim and fill method from Duval and Tweedie, no studies was added for ascites, and the positive association remained after 7 missing studies were added for pleural effusion (original OR = 2.731, 95% CI: 1.939–3.521, p = 0.000; adjusted OR = 1.823, 95% CI: 1.114–2.533, p = 0.000). Both revealed a stronger association with SD within 7 days after onset in 2 studies (OR = 87.143, 95% CI: 10.962–693.405, p<0.001; OR = 83.578, 95% CI: 3.786–1844.938, p = 0.005). The details are described in Fig 3. Additionally, hypotension was observed to be a risk factor for SD (OR = 3.692, 95% CI: 1.670–8.162, p = 0.001) in 11 studies, and publication bias was found. Using the trim and fill method from Duval and Tweedie, 4 missing studies were added, and the association remained unchanged (original OR = 0.672, 95% CI: 0.318–1.025, p<0.001; adjusted OR = 0.452, 95% CI: 0.110–0.793, p = 0.010). The high level of heterogeneity was not reduced, and the summary effect changed significantly when the leave-one-out analyses and subgroup analyses of covariables were conducted.
Fig 3. Association between plasma leakage and SDD.
(A, B) Forest plot for pleural effusion, ascites respectively DF vs SDD, OR: odds ratio. (C, D) Funnel Plots for pleural effusion, ascites respectively (Trim and Fill) DF vs SDD, SE: standardized error.
Blood cell counts
Among the markers investigated, a decrease in the platelet count was observed in 38 studies and was revealed to be a risk factor for SD (SMD = -1.070, 95% CI: -1.293–0.848, p<0.001). However, publication bias was observed (p<0.05). After 7 missing studies were added, the association was stronger (original SMD = -1.070, 95% CI: -1.293–0.848, p<0.001; adjusted SMD = -1.384, 95% CI: -1.665–1.102, p<0.001). Furthermore, another twelve dichotomous datasets were pooled and revealed that thrombocytopenia was strongly associated with SD (OR = 8.146, 95% CI: 3.374–19.665, p<0.001). Additionally, the quantitative analysis showed that hematocrit (HCT) was positively associated with SD (SMD = 0.327, 95% CI: 0.109–0.546, p = 0.003) in 27 studies, and there were 7 dichotomous datasets with elevated HCT levels, which was strongly associated with SD (OR = 12.389, 95% CI: 6.091–25.199, p<0.001). Moreover, sampling time (≤7 days after onset) subgroup analysis was performed and platelet count, thrombocytopenia and HCT were also observed to be risk factors of SD in 10 (SMD = -1.452, 95% CI: -1.872- -1.031, p<0.001), 3 (OR = 48.931, 95% CI: 1.873–1278.431, p<0.001), 7 (SMD = 0.706, 95% CI: 0.122–1.291, p = 0.018) studies, respectively.
Hepatic and renal manifestations, lipids
Within the list of serum markers, the levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were significantly higher in patients with SD than in those with DF (SMD = 1.007, 95% CI: 0.386–1.627, p = 0.001; SMD = 1.278, 95% CI: 0.640–1.916, p<0.001); Also, AST revealed a stronger association with SD in 7 studies (SMD = 1.712, 95% CI: 0.276–3.148, p = 0.019) within 7 days after onset. Additionally, the summary effect of elevated ALT and AST also showed a stronger association with SD after pooling 8 (OR = 4.030, 95% CI: 2.408–6.747, p<0.001) and 4 (OR = 4.053, 95% CI: 2.255–7.287, p<0.001) studies, respectively. However, publication bias was observed on Begg’s test for ALT (p<0.05) and AST (p<0.05); no study was added using the trim and fill method. Albumin (ALB) and total protein (TP) levels were significantly lower in patients with SD than in those with DF after pooling 13 (SMD = -0.767, 95% CI: -0.989–0.544, p<0.001) and 5 (SMD = -0.271, 95% CI: -0.449–0.093, p = 0.003) studies, respectively. Meanwhile, hypoproteinemia, hypoalbuminemia, proteinuria, and increased levels of creatine kinase (CK), lactate dehydrogenase (LDH) and blood urea nitrogen (BUN) were positively associated with SD (Table 1).
Coagulation tests
Prolonged prothrombin time (PT) and activated partial thromboplastin time (APTT) were found to be significantly associated with SD after pooling 6 studies (SMD = 0.781, 95% CI: 0.219–1.343, p = 0.006; SMD = 0.529, 95% CI: 0.046–1.013, p = 0.032). However, the summary effect of prolonged PT, prolonged APTT, and elevated D-dimer levels had a negative association with SD in two dichotomous datasets (S5 Table).
Cytokines and chemokines
Various detection methods and descriptions of the results were observed in the original literature. A wide blood sampling window was observed, ranging from the acute phase to the convalescence phase. Studies with mean differences in cytokines and chemokines available were selected for the current study. Overall, eleven cytokines and chemokines were identified after pooling the relevant studies. Levels of IL-10, IL-8, sVCAM-1, and IP-10 were positively associated with SD in 6, 3, 2 and 2 studies, respectively (Table 1). Furthermore, subgroup analyses of sampling time showed inconsistent results for IFN-γ. The level was significantly higher in 4 studies (SMD = 0.184, 95% CI: 0.023–0.344, p = 0.025) without heterogeneity (I2 = 0.0%, p = 0.480) when sampled early in the disease course (≤7 days of onset). Additionally, most cytokines (except sVCAM-1 and IP-10) had discordant results in the included individual studies.
Discussion
It is critically important to identify the predictive factors for SD, as the early diagnosis and treatment of SD could reduce mortality and decrease hospitalization durations and costs. The pathogenesis of SD is multifactorial and is not yet well understood. Antibody-dependent enhancement (ADE) due to non-neutralizing cross-reactive antibodies may play a vital role in the mechanism, especially in secondary infection cases [38, 39]. Zhang H, et al [40] conducted a meta-analysis that provided the evidence for the classifications of severe dengue disease according to the new WHO guideline 2009 based on the literature between 2000 and 2012. However, compared with symptoms and signs, virus serotype and plasma biomarkers results were obtained more objectively. In this study, 34 factors including clinical manifestations, virus serotypes, medical history, and plasma biomarkers, were found to be significantly different between DF and SD. Since the critical phase of dengue is usually on days 3–7 of illness [1], subgroups analysis for sampling time (≤7 days after onset) were performed in this study. Nine factors revealed association with SD within 7 days after onset and could be predictors for SD.
Clinical manifestations
It was further confirmed that SD was associated with secondary infections in the current study, indicating that DF patients with secondary infection had a 2.69 times higher risk of SD than those with only DF. The WS were further confirmed in the current meta-analysis; hepatomegaly, bleeding, pleural effusion, ascites, and persistent vomiting were associated with 4.4, 6.9, 15.8, 24.3, and 5.6 times the risk of SD, respectively, which were consistent with previous study [40]. Thus, patients with WS should be treated appropriately and in a timely manner to prevent the development of SD. Moreover, lethargy and hypotension had a positive association with SD, which meant that these manifestations are also predictors of SD. However, significant heterogeneity was observed among studies regarding these clinical manifestations. The heterogeneity might be due to inherent differences in populations.
Viral and host factors
This finding also showed a clear difference in the associations of dengue serotypes with the percentage of severe cases. Although DENV-1 accounted for the highest percentage of dengue infections, there was a lower risk of SD on overall, whereas, no statistically significant difference was revealed between patients with DF and those with SD in the Asia and in the Americas, respectively. DENV-2 was a risk factor for SD, even though it had the lowest seroprevalence in the Americas. However, DENV-3 had an inconsistent association with SD, with a negative association in Asia (OR = 0.669, p = 0.021) and no association in the Americas. However, it is premature to draw firm conclusions. The serotypes of DENV were not always reported in the included studies. Only 20.7% of the studies included provided serotype data, and many did not separate primary from secondary dengue infections caused by each dengue serotype. Meanwhile, discordant results have been observed in other studies. DENV-1 is seldom involved in severe cases in Brazil [41], whereas it was associated with DHF and SD in Singapore [42] DENV-4 was found to be strongly associated with DSS in Brazil [41] and individuals infected with DENV-4 had a higher prevalence of respiratory and cutaneous manifestations in South America [43] Rico-Hesse et al. proposed the term virulent genotypes and revealed an association between two distinct genotypes of DENV-2 and the appearance of DHF in the Americas [44]. Alternatively, it had been reported that the genetic changes in DENV-3 were associated with the increasing severe dengue epidemics in Sri Lanka [45]. Thus, the serotype of DENV can contribute to SD differently based on other factors, and the seroprevalence [46] and changes in the viral genotype [47] during epidemics might be potential factors affecting the development of SD; this needs further investigation.
In this study, there was no association between age and SD in children, but increasing age results in a higher risk of progressing into SD among adults after pooling 46 studies, agreeing with previous studies[15, 40, 48]. However, consistent conclusions were observed in different populations. For example, pregnant women are 3.4 times more likely to develop SD than non-pregnant women [49]; as high a proportion as 80% of infants hospitalized with dengue developed DHF/DSS [50]. Furthermore, individuals with a history of diabetes had a 4.42 times higher risk of SD than those without a history of diabetes. The reason might be that diabetes could result in immune and endothelial dysfunction [51, 52].
Plasma biomarkers
Some evidence also indicated that the incidence of low platelet counts, plasma leakage, shock and hemorrhagic manifestations were significantly different in infants compared with older children, and bleeding signs, including rash, petechiae and obvious bleeding were observed approximately 2 times more often in adults than children. [53, 54]. An increase in HCT concurrent with a rapid decrease in platelet count was defined as one of the WS by the WHO [1]. In the current study, thrombocytopenia, an increase in HCT and a decrease in the platelet count were associated with SD, so did in subgroup analysis for sampling time (≤7 days after onset). The leukocyte count is frequently used to evaluate suspected bacterial infections. It had been indicated to be a good marker for differentiating between bacterial versus viral infections in a prospective study [55]. In the early febrile phase, a decreasing white blood cell count makes the diagnosis of dengue very likely [1]. However, the counts of the total population and subpopulations of white blood cells were not different between patients with DF and those with SD. As the whole blood counts were dynamic throughout the pathogenic process, a subgroup analysis of sampling time was conducted, but the pooled effect showed no significant difference. Additionally, some studies revealed that atypical lymphocyte count, immature platelet fraction and triple positivity for NS1, Ig M and Ig G would be predictive for SD [56–58], although them couldn’t be included in this meta-analysis. Further studies should be performed to identify in the future.
Liver damage is a well-established characteristic of dengue patients, particularly in severe cases[1, 59], and ALT or AST≥1000 IU/L is a diagnostic criterion for SD [1]; these facts highlight that the liver is involved in the pathogenesis of dengue infection. In this meta-analysis, elevated ALT levels, elevated AST levels and hypoalbuminemia were positively associated with SD. Furthermore, the levels of LD, CK and BUN were increased in patients with SD compared with patients with DF. Unfortunately, there were not enough clinical data available to determine the cutoff values of the indicators. Thus, more clinical studies with defined cutoff values are needed to address these biomarkers in the future.
It is well known that cytokines and chemokines play important roles in the pathogeny of dengue infection but inconsistent association between DF and SD was observed in the literature because of the heterogeneity [13, 60, 61]. In the current study, the pooled results of IL-8, IL-10, sVCAM-1 and IP10 were positively associated with severity. However, these findings should be interpreted cautiously because conflicting results were observed among studies. One of the major hindrances is the inconsistent results in the literature caused by heterogeneity. Large variations were observed among studies with various sampling times. Regarding IFN-γ, a significant positive association with SD was revealed in the acute phase after removing studies with different sampling times. Additionally, the level of IFN-γ was significantly higher in patients with SD than in those with DF, but opposing results were observed during the defervescence and convalescent stages [62, 63]. As the levels of cytokines/chemokines are dynamic during the process of infection, they display differences in the timing of their peak responses [64, 65]. Thus, different factors should be measured during the appropriate phases. Furthermore, there were significant differences in the levels of IL-8 and VEGFR2 between serum and plasma samples [64, 65]. These results merit further investigation with better-defined methodologies, full descriptions of the results and transparency of the sampling time and serotypes. These data would be helpful in overcoming the weaknesses of the currently available publications.
Limitations
There were some limitations in our study. First, there were some markers, such as viremia, nutritional status, and serum levels of C-reactive protein, total cholesterol, and triglycerides, were not analyzed in this study because of insufficient data. Second, the significant heterogeneity was not fully explained by the six covariables investigated. It could have been driven by numerous other factors that were not addressed in this meta-analysis, which shows the need of controls for these factors in order to further confirm the findings in future research. Third, some reasons might conduct biases, such as most reports were retrospective, non-English studies were excluded, samples were processed into plasma or serum and different WHO classification methods were used to assign the disease’s severity.
Conclusion
A list of 34 potential severity markers was investigated in this study; and nine factors, secondary infection, retro orbital pain, hepatomegaly, bleeding, pleural effusion, ascites, increased HCT, and AST, decreased PLT revealed positive relation with SD in early stage (≤7 days after onset). Hence, this study provides information regarding markers that can be used to identify SD in the early stage, facilitating prompt disease management. However, heterogeneity was observed among current studies, which suggests that increased standardization is needed in future clinical reports.
Supporting information
(DOC)
(DOC)
(DOCX)
(DOCX)
(DOC)
(DOC)
(DOC)
(XLSX)
Acknowledgments
The authors would like to thank Dr. Peihuang Wu for assistance during the preparation of this manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was funded by Guangzhou Science Technology and Innovation Committee (https://sop.gzsi.gov.cn/egrantweb/, NO. 201607010163 awards to Lidong Liu), Health and Family Planning Commission of Guangdong Province (http://wsjkw.gd.gov.cn/, NO. A2016448 awards to Lidong Liu) and Guangzhou Medical University (https://www.gzhmu.edu.cn/, NO.2014C24 awards to Lidong Liu). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO. Dengue: guidelines for diagnosis, treatment, prevention and control. New Editio. WHO Press. Geneva, Switzerland; 2009. [PubMed] [Google Scholar]
- 2.WHO. Dengue haemorrhagic fever Diagnosis, treatment, prevention and control. SECOND EDI. WHO Press. Geneva, Switzerland; 1997. [Google Scholar]
- 3.WHO. Dengue and severe dengue. 2019. Available: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue/
- 4.Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, et al. The global distribution and burden of dengue. Nature. 2013;496: 504–507. doi: 10.1038/nature12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stanaway JD, Shepard DS, Undurraga EA, Halasa YA, Coffeng LE, Brady OJ, et al. The Global Burden of Dengue: an analysis from the Global Burden of Disease Study 2013 Europe PMC Funders Group. Lancet Infect Dis. 2016;16: 712–723. doi: 10.1016/S1473-3099(16)00026-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flasche S, Jit M, Rodríguez-Barraquer I, Coudeville L, Recker M, Koelle K, et al. The Long-Term Safety, Public Health Impact, and Cost-Effectiveness of Routine Vaccination with a Recombinant, Live-Attenuated Dengue Vaccine (Dengvaxia): A Model Comparison Study. PLoS Medicine. 2016;13: e1002181. doi: 10.1371/journal.pmed.1002181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sridhar S, Luedtke A, Langevin E, Zhu M, Bonaparte M, Machabert T, et al. Effect of Dengue Serostatus on Dengue Vaccine Safety and Efficacy. N Engl J Med. 2018;379: 327–340. doi: 10.1056/NEJMoa1800820 [DOI] [PubMed] [Google Scholar]
- 8.Yeh CY, Chen PL, Chuang KT, Shu YC, Chien YW, Perng GC, et al. Symptoms associated with adverse dengue fever prognoses at the time of reporting in the 2015 dengue outbreak in Taiwan. PLoS Neglected Tropical Diseases. 2017;11: e0006091. doi: 10.1371/journal.pntd.0006091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibson G, Souza-Santos R, San Pedro A, Alves Honório N, Sá Carvalho M. Occurrence of severe dengue in rio de janeiro: An ecological study. Revista da Sociedade Brasileira de Medicina Tropical. 2014;47: 684–691. doi: 10.1590/0037-8682-0223-2014 [DOI] [PubMed] [Google Scholar]
- 10.Kapuria D, Takyar VK, Etzion O, Surana P, O’Keefe JH, Koh C. Association of Hepatic Steatosis With Subclinical Atherosclerosis: Systematic Review and Meta‐Analysis. Hepatology Communications. 2018;2: 873–883. doi: 10.1002/hep4.1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anders KL, Nguyet NM, Chau NVV, Hung NT, Thuy TT, Lien LB, et al. Epidemiological factors associated with dengue shock syndrome and mortality in hospitalized dengue patients in Ho Chi Minh City, Vietnam. American Journal of Tropical Medicine and Hygiene. 2011;84: 127–134. doi: 10.4269/ajtmh.2011.10-0476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sam SS, Omar SFS, Teoh BT, Abd-Jamil J, AbuBakar S. Review of Dengue Hemorrhagic Fever Fatal Cases Seen Among Adults: A Retrospective Study. PLoS Neglected Tropical Diseases. 2013;7: e2194. doi: 10.1371/journal.pntd.0002194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar Y, Liang C, Bo Z, Rajapakse JC, Ooi EE, Tannenbaum SR. Serum Proteome and Cytokine Analysis in a Longitudinal Cohort of Adults with Primary Dengue Infection Reveals Predictive Markers of DHF. PLoS Neglected Tropical Diseases. 2012;6: e1887. doi: 10.1371/journal.pntd.0001887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Her Z, Kam YW, Gan VC, Lee B, Thein TL, Tan JJL, et al. Severity of Plasma Leakage Is Associated With High Levels of Interferon γ-Inducible Protein 10, Hepatocyte Growth Factor, Matrix Metalloproteinase 2 (MMP-2), and MMP-9 During Dengue Virus Infection. The Journal of infectious diseases. 2017;215: 42–51. doi: 10.1093/infdis/jiw494 [DOI] [PubMed] [Google Scholar]
- 15.Huy NT, Giang T Van, Ha D, Thuy D, Kikuchi M, Hien TT. Factors Associated with Dengue Shock Syndrome: A Systematic Review and Meta-Analysis. PLoS Neglected Tropical Diseases. 2013;7: e2412. doi: 10.1371/journal.pntd.0002412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Temprasertrudee S, Thanachartwet V, Desakorn V, Keatkla J, Chantratita W, Kiertiburanakul S. A multicenter study of clinical presentations and predictive factors for severe manifestation of dengue in adults. Japanese Journal of Infectious Diseases. 2018;71: 239–243. doi: 10.7883/yoken.JJID.2017.457 [DOI] [PubMed] [Google Scholar]
- 17.Thanachartwet V, Oer-areemitr N, Chamnanchanunt S, Sahassananda D, Jittmittraphap A, Suwannakudt P, et al. Identification of clinical factors associated with severe dengue among Thai adults: A prospective study. BMC Infectious Diseases. 2015;15: 420. doi: 10.1186/s12879-015-1150-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perdomo-Celis F, Salgado DM, Narváez CF. Magnitude of viremia, antigenemia and infection of circulating monocytes in children with mild and severe dengue. Acta Tropica. 2017;167: 1–8. doi: 10.1016/j.actatropica.2016.12.011 [DOI] [PubMed] [Google Scholar]
- 19.Tuan NM, Nhan HT, Van Vinh Chau N, Hung NT, Tuan HM, Van Tram T, et al. An evidence-based algorithm for early prognosis of severe dengue in the outpatient setting. Clinical Infectious Diseases. 2017;64: 656–663. doi: 10.1093/cid/ciw863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Clinico-laboratory spectrum of dengue viral infection and risk factors associated with dengue hemorrhagic fever: A retrospective study. BMC Infectious Diseases. 2015;15: 399. doi: 10.1186/s12879-015-1141-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339: b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomized studies in meta-analyses. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Google Scholar]
- 23.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine. 2002;21: 1539–1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327: 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee YH. Meta-analysis of genetic association studies. Trends in genetics. 2004;20: 339–444. doi: 10.1016/j.tig.2004.06.014 [DOI] [PubMed] [Google Scholar]
- 26.SG HJPT. How should meta-regression analyses be undertaken and interpreted? Statistics in medicine. 2002;21: 1559–1573. doi: 10.1002/sim.1187 [DOI] [PubMed] [Google Scholar]
- 27.Higgins J, Thompson S, Deeks J, Altman D. Statistical heterogeneity in systematic reviews of clinical trials: A critical appraisal of guidelines and practice. Journal of Health Services Research and Policy. 2002;7: 51–61. doi: 10.1258/1355819021927674 [DOI] [PubMed] [Google Scholar]
- 28.Begg CB, Mazumdar M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics. 1994;50: 1088–1101. [PubMed] [Google Scholar]
- 29.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315: 629–634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56: 455–463. doi: 10.1111/j.0006-341x.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 31.Tobias A. Assessing the influence of a single study in meta-analysis. Stata Technical Bulletin. 1999;47: 15–17. [Google Scholar]
- 32.Whitehorn J, Simmons CP. The pathogenesis of dengue. Vaccine. 2011;29: 7221–7228. doi: 10.1016/j.vaccine.2011.07.022 [DOI] [PubMed] [Google Scholar]
- 33.Guzmán MG, Kourí G. Dengue: an update. The Lancet Infectious Diseases. 2002;2: 33–42. doi: 10.1016/s1473-3099(01)00171-2 [DOI] [PubMed] [Google Scholar]
- 34.Halstead SB, Streit TG, Lafontant JG, Putvatana R, Russell K, Sun W, et al. Haiti: Absence of dengue hemorrhagic fever despite hyperendemic dengue virus transmission. American Journal of Tropical Medicine and Hygiene. 2001;65: 180–183. doi: 10.4269/ajtmh.2001.65.180 [DOI] [PubMed] [Google Scholar]
- 35.WHO. Comprehensive guidelines for prevention and control of dengue and dengue haemorrhagic fever. Revised an. WHO Regional Publication. New Delhi: World Health Organization; 2011. doi: 10.1017/CBO9781107415324.004 [DOI] [Google Scholar]
- 36.WHO. Guidelines for Treatment of Dengue Fever/Dengue Haemorrhagic Fever in Small Hospitals. WHO. New Delhi; 1999. doi: 10.1039/c1ib90048j [DOI] [Google Scholar]
- 37.Ministério da Saúde—Secretaria de Vigilância em Saúde. Dengue-diagnóstico e manejo clínico. Ministerio da Saude. 2013.
- 38.Guzman MG, Alvarez M, Halstead SB. Secondary infection as a risk factor for dengue hemorrhagic fever/dengue shock syndrome: An historical perspective and role of antibody-dependent enhancement of infection. Archives of Virology. 2013;158: 1445–1459. doi: 10.1007/s00705-013-1645-3 [DOI] [PubMed] [Google Scholar]
- 39.Alwis R De, Williams KL, Schmid MA, Lai C, Patel B, Smith SA, et al. Dengue Viruses Are Enhanced by Distinct Populations of Serotype Cross-Reactive Antibodies in Human Immune Sera. PLOS Pathogens. 2014;10: e1004386. doi: 10.1371/journal.ppat.1004386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang H, Zhou YP, Peng HJ, Zhang XH, Zhou FY, Liu ZH, et al. Predictive Symptoms and Signs of Severe Dengue Disease for Patients with Dengue Fever: A Meta-Analysis. BioMed Research International. 2014;2014: 359308. doi: 10.1155/2014/359308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vicente CR, Herbinger KH, Fröschl G, Romano CM, Cabidelle A de SA, Junior CC. Serotype influences on dengue severity: A cross-sectional study on 485 confirmed dengue cases in Vitória, Brazil. BMC Infectious Diseases. 2016;16: 320. doi: 10.1186/s12879-016-1668-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yung CF, Lee KS, Thein TL, Tan LK, Gan VC, Wong JGX, et al. Dengue serotype-specific differences in clinical manifestation, laboratory parameters and risk of severe disease in adults, Singapore. American Journal of Tropical Medicine and Hygiene. 2015;92: 999–1005. doi: 10.4269/ajtmh.14-0628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Halsey ES, Marks MA, Gotuzzo E, Fiestas V, Suarez L, Vargas J, et al. Correlation of serotype-specific dengue virus infection with clinical manifestations. PLoS Neglected Tropical Diseases. 2012;6. doi: 10.1371/journal.pntd.0001638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rico-Hesse R, Harrison LM, Salas RA, Tovar D, Nisalak A, Ramos C, et al. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology. 1997;230: 244–251. doi: 10.1006/viro.1997.8504 [DOI] [PubMed] [Google Scholar]
- 45.Kanakaratne N, Wahala WMPB, Messer WB, Tissera HA, Shahani A, Abeysinghe N, et al. Severe dengue epidemics in Sri Lanka, 2003–2006. Emerging infectious diseases. 2009;15: 192–199. doi: 10.3201/eid1502.080926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Silva S, Cuadra R, PÉrez MA, Mercado JC, Hammond SN, Harris E, et al. Serotype-Specific Differences in Clinical Manifestations of Dengue. The American Journal of Tropical Medicine and Hygiene. 2018;74: 449–456. doi: 10.4269/ajtmh.2006.74.449 [DOI] [PubMed] [Google Scholar]
- 47.William B. M, Duane J. G, Eva H, Kamalanayani S, DS Aravinda M. Emergence and global spread of a dengue serotype 3, subtype III virus. Emerging Infectious Diseases. 2003;9: 800–809. doi: 10.3201/eid0907.030038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.MinSheng L, KaoPin H, TunChieh C, PoLian L, TyenPo C. Clinical characteristics of dengue and dengue hemorrhagic fever in a medical center of southern Taiwan during the 2002 epidemic. Journal of Microbiology, Immunology and Infection. 2006;39: 121–129. [PubMed] [Google Scholar]
- 49.Machado CR, Machado ES, Rohloff RD, Azevedo M, Campos DP, Oliveira RB de, et al. Is Pregnancy Associated with Severe Dengue? A Review of Data from the Rio de Janeiro Surveillance Information System. PLoS Neglected Tropical Diseases. 2013;7: e2217. doi: 10.1371/journal.pntd.0002217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chau TNB, Anders KL, Lien LB, Hung NT, Hieu LTM, Tuan NM, et al. Clinical and virological features of dengue in Vietnamese infants. PLoS Neglected Tropical Diseases. 2010;4: e657. doi: 10.1371/journal.pntd.0000657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suzanne EG, Andy IMH. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunology and Medical Microbiology. 1999;26: 259–265. doi: 10.1111/j.1574-695X.1999.tb01397.x [DOI] [PubMed] [Google Scholar]
- 52.Dandona P, Aljada A, Chaudhuri A, Mohanty P. Endothelial Dysfunction, Inflammation and Diabetes. Reviews in Endocrine and Metabolic Disorders. 2004;5: 189–197. doi: 10.1023/B:REMD.0000032407.88070.0a [DOI] [PubMed] [Google Scholar]
- 53.Hung NT, Lei H, Lan NT, Lin Y, Huang K, Lien LB, et al. Dengue Hemorrhagic Fever in Infants: A Study of Clinical and Cytokine Profiles. The Journal of Infectious Diseases. 2004;189: 221–32. doi: 10.1086/380762 [DOI] [PubMed] [Google Scholar]
- 54.Hammond SN, Balmaseda A, Pérez L, Tellez Y, Saborío SI, Mercado JC, et al. Differences in dengue severity in infants, children, and adults in a 3-year hospital-based study in Nicaragua. American Journal of Tropical Medicine and Hygiene. 2005;73: 1063–1070. doi: 10.4269/ajtmh.2005.73.1063 [DOI] [PubMed] [Google Scholar]
- 55.Capretti M, Marsico C, Spinelli M, Angelis MD, Tridapalli E, Lazzarotto T, et al. Comparison of C-reactive Protein with Leukocytes and ESR for Differentiation between Bacterial and Viral Infections. Archives of Disease in Childhood. 2012;97: A267. doi: 10.1136/archdischild-2012-302724.0932 [DOI] [Google Scholar]
- 56.Clarice CSH, Abeysuriya V, de Mel S, Thilakawardana BU, de Mel P, de Mel C, et al. Atypical lymphocyte count correlates with the severity of dengue infection. PLoS ONE. 2019;14: 1–11. doi: 10.1371/journal.pone.0215061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abeysuriya V, Seneviratne SL, de Mel P, Clarice CSH, de Mel C, Chandrasena L, et al. The immature platelet fraction, a predictive tool for early recovery from dengue-related thrombocytopenia: a prospective study. Transactions of The Royal Society of Tropical Medicine and Hygiene. 2021; 1–9. doi: 10.1093/trstmh/traa095 [DOI] [PubMed] [Google Scholar]
- 58.de Mel S, Thilakawardana BU, de Mel P, Clarice CSH, Shalindi M, de Mel C, et al. Triple positivity for nonstructural antigen 1, immunoglobulin M and immunoglobulin G is predictive of severe thrombocytopaenia related to dengue infection. Journal of Clinical Virology. 2020; 104509. doi: 10.1016/j.jcv.2020.104509 [DOI] [PubMed] [Google Scholar]
- 59.Lee LK, Gan VC, Lee VJ, Tan AS, Leo YS, Lye DC. Clinical relevance and discriminatory value of elevated liver aminotransferase levels for dengue severity. PLoS Neglected Tropical Diseases. 2012;6: e1676. doi: 10.1371/journal.pntd.0001676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.De La Cruz Hernández SI, Puerta-Guardo H, Flores-Aguilar H, González-Mateos S, López-Martinez I, Ortiz-Navarrete V, et al. A strong interferon response correlates with a milder dengue clinical condition. Journal of Clinical Virology. 2014;60: 196–199. doi: 10.1016/j.jcv.2014.04.002 [DOI] [PubMed] [Google Scholar]
- 61.Chen LC, Lei HY, Liu CC, Shiesh SC, Chen SH, Liu HS, et al. Correlation of serum levels of macrophage migration inhibitory factor with disease severity and clinical outcome in dengue patients. American Journal of Tropical Medicine and Hygiene. 2006;74: 142–147. doi: 10.4269/ajtmh.2006.74.142 [DOI] [PubMed] [Google Scholar]
- 62.Sehrawat P, Biswas A, Kumar P, Singla P, Wig N, Dar L, et al. Role of Cytokines as Molecular Marker of Dengue Severity. Mediterr J Hematol Infect Dis. 2018;10: 2–6. doi: 10.4084/MJHID.2018.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Soundravally R, Hoti SL, Patil SA, Cleetus CC, Zachariah B, Kadhiravan T, et al. Association between proinflammatory cytokines and lipid peroxidation in patients with severe dengue disease around defervescence. International Journal of Infectious Diseases. 2014;18: 68–72. doi: 10.1016/j.ijid.2013.09.022 [DOI] [PubMed] [Google Scholar]
- 64.Lin YP, Luo Y, Chen Y, Lamers MM, Zhou Q, Yang XH, et al. Clinical and epidemiological features of the 2014 large-scale dengue outbreak in Guangzhou city, China. BMC Infectious Diseases. 2016;16: 102. doi: 10.1186/s12879-016-1379-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Soo K-M, Khalid B, Ching S-M, Tham CL, Basir R, Chee H-Y. Meta-analysis of biomarkers for severe dengue infections. PeerJ. 2017;5: e3589. doi: 10.7717/peerj.3589 [DOI] [PMC free article] [PubMed] [Google Scholar]