Abstract
Background:
Beginning in 2010, Los Angeles County Departments of Health Services and Mental Health collaborated to increase access to effective mental health care. The Mental Health Integration Program (MHIP) embedded behavioral health specialists in primary care clinics to deliver brief, problem-focused treatments and psychiatric consultation support for primary care-prescribed psychotropic medications.
Objective:
To compare primary care visits associated with psychiatric diagnoses before and after MHIP implementation.
Methods:
This retrospective cohort study (2009 –2014) examined 62,945 patients from eight safety-net clinics that implemented MHIP in a staggered fashion in Los Angeles. Patients’ primary care visits (n=695,354) were either associated or not with a previously identified or “new” (defined as having no diagnosis within the prior year) psychiatric diagnosis. Multilevel regression models used MHIP implementation to predict odds of visits being associated with psychiatric diagnoses, controlling for time, clinic, and patient characteristics.
Results:
9.4% of visits were associated with psychiatric diagnoses (6.4% depression, 3.1% anxiety, <1% alcohol and substance use disorders). Odds of visits being associated with psychiatric diagnoses were 9% higher (95% confidence interval [CI]=1.05–1.13; p=<.0001), and 10% higher for diagnoses that were new (CI=1.04–1.16; p=0.002), after MHIP implementation than before. This appeared to be fueled by increased visits for depression post-MHIP (OR=1.11; CI=1.06–1.15; p=<.0001).
Conclusions:
MHIP implementation was associated with more psychiatric-diagnoses coded in safety-net primary care visits. Scaling up this effort will require greater attention to the notable differences across patient populations and languages, as well as the markedly low coding of alcohol and substance use services in primary care.
Keywords: primary care, mental health, integrated care, access to care, underserved
Introduction
Though health care reform has improved access to primary care for low-income, racial-ethnic minority patients via safety-net health systems,1 accessing specialty services remains challenging2—notably in mental health and substance abuse treatment.3 Mental health disorders are prevalent, top the list of most costly conditions,4 and contribute to poor health and significant disability worldwide.5 Racial-ethnic minorities, many of whom are served in safety-net health systems, are disproportionately burdened by mental health related disability;6–8 however, they are consistently noted to use fewer mental health services than non-minorities.9 While safety-net health systems have delivered more mental health and substance abuse services in recent years, demand continues to outstrip supply.10
Racial-ethnic and income-related health disparities in mental health use are exacerbated by access barriers11 but can be mitigated by interventions to systematically improve disease diagnosis and treatment.12 Principled on patient-centered team care for a population, collaborative care models for the treatment of common psychiatric diseases are well-established and supported by over 79 randomized controlled trials.13, 14 Such programs typically embed behavioral health specialists in primary care clinics to deliver brief, problem-focused treatments and psychiatric consultation support for primary care-prescribed psychotropic medications. Behavioral health care managers track patients with identified behavioral health needs and liaison among team members to coordinate their services.
Beginning in 2010, the Los Angeles County Department of Health Services (LADHS) partnered with the Los Angeles County Department of Mental Health (the second largest public health system in the United States and the largest county mental health system in the US, respectively) to provide integrated mental health services within safety-net primary care settings. Funded in part by California’s Mental Health Services Act,15 the two Departments adapted the Mental Health Integration Program (MHIP), which was modeled after evidence-based collaborative care models in primary care and used by public health systems in other states (e.g., Washington).16 At the time of our currently study, approximately half of LADHS primary care clinics, that served the largest numbers of patients, were considered to be ready and willing to implement MHIP by Department leadership, and thus underwent numerous staffing and process changes below. At present day, all 20+ LADHS primary care clinics have MHIP in place.
The MHIP model is a patient-centered integrated care program delivered by onsite behavioral health providers (predominantly Licensed Clinical Social Workers) and indirect consultation of psychiatrists to deliver a range of services to the primary care clinic population. The program included regular screening for depressive, anxiety, and trauma disorders, mental health assessment, treatment planning, medication management consultation, and evidence-based treatment interventions, such as Problem-Solving Treatment, Cognitive Behavioral Therapy, or other behavioral interventions. Additional care management services include facilitated referrals to specialty mental health centers for more intensive services when appropriate (Appendix 1).
As with other large-scale disseminations of collaborative care models in the real world, LADHS faced implementation challenges requiring modifications to originally studied care models.16, 17 For example, different scheduling and documentation systems between both Departments stymied patient referrals and provider communication, necessitating innovation in asynchronous electronic communication via an e-Consult Mental Health platform.18 Inconsistent staffing and physical space limitations were implementation barriers but MHIP tried to maintain on-site mental health specialists at participating primary care clinics. While specialists were able to provide as needed psychotropic medication consultation and some short-term psychosocial treatments, MHIP struggled with broader care management for at-risk populations. Nonetheless, the LADHS’s experience represents one of the largest implementations of integrated mental health services within a safety-net system serving low-income, racial-ethnically diverse patients. This study compared primary care visit-associated psychiatric diagnoses before and after MHIP, as locally implemented among safety-net clinics.
Methods
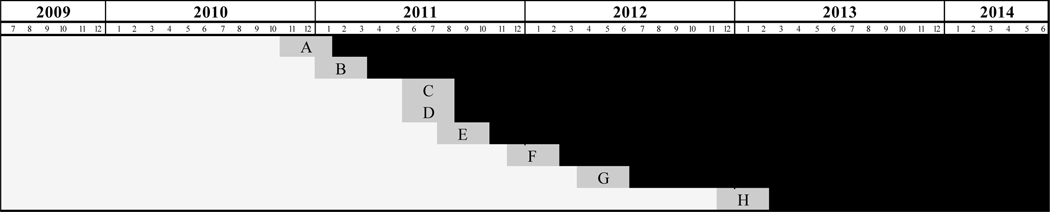
We retrospectively examined medical visits among 62,945 primary care patients from eight clinics that implemented MHIP in a staggered fashion between June 30, 2009 to July 1, 2014 (n=695,354 visits). This study used a non-randomized stepped wedge design19, which allows for rigorous assessment of program implementation across multiple healthcare sites by using both control state and implementation state data from each site. Like other safety-net systems, our study patients infrequently accessed primary care services, that is few had repeat visits each year. Furthermore, some patients switched primary care clinics during the 5-year study period, which is also common among safety-net populations. As a result, we used LADHS administrative databases to select a cohort of stable primary care users with at least two primary care visits in the baseline fiscal year (June 30, 2009 to July 1, 2010). Within our cohort, we tracked all primary care visits before and after MHIP implementation (with a 6-week buffer during implementation) in each study clinic (Figure 1). We focused solely on primary care visits because safety-net patients infrequently accessed mental health services, confirmed among our cohort to be only 0.01% relative to the number of primary care visits.
Figure 1. Staggered Implementation of Mental Health Integration in Primary Care Clinics, 2009–2014.
Each row and letter depict one distinct primary care clinic. Light gray bars represent the start of the study period and before program implementation. The midpoint of the gray bars represent the start of mental health integration and are accompanied by 6-week buffer periods before and after program implementation, during when visits were excluded from study analysis. Black bars represent the time period following the respective buffers, after program implementation.
Outcomes were dichotomized into whether visits were associated or not associated with a psychiatric diagnoses per International Classification of Diseases, Ninth Revision (ICD-9). In addition to psychiatric diagnoses in sum, we separately examined and grouped diagnoses as follows: depression, anxiety, alcohol use disorders, substance use disorders, posttraumatic stress disorder, bipolar disorder, and schizophrenia. Furthermore, we examined the occurrence of a “new” psychiatric diagnosis, which we defined as not having a psychiatric diagnosis documented in the year prior.
Our main explanatory variable was whether visits occurred before or after MHIP implementation, defined by the first administrative coding of integrated services buffered by six-week periods. We included patient-level covariates for all study years, including age, sex, race-ethnicity, marital status, primary language, and health insurance. To facilitate risk adjustment, we additionally calculated each patient’s Charlson Comorbidity Index using available ICD-9 diagnostic codes.20
In unadjusted analyses, we used chi-square tests to compare rates of visits associated with a psychiatric diagnosis by MHIP implementation status among study clinics. Finally, in multilevel regression models, we used MHIP implementation status to predict odds of having a visit being associated with a psychiatric diagnosis, adjusting for time, clinic, and patient characteristics. Each model contained fixed effects for time and both fixed and random effects for clinic, to account for secular trends (e.g., concurrent quality improvement projects) and time-invariant clinic characteristics (e.g., size, location, provider practice). Population characteristics (i.e. few repeat patient visits) prevented us from being able to estimate stable 3-level models (visits clustered by patients within clinics). In all models, we determined significance by using a two-tailed α of 0.05 and analyzed data in SAS, version 9.4. This research was approved by Institutional Review Boards at University of California, Los Angeles (IRB#19–001818), the LA County Department of Health Services, and the LA County Department of Mental Health (HSRC #302).
Results
The sociodemographic characteristic of our study patients largely characterized LA County’s safety-net primary care population. Patients were mostly 45–64 years (57.1%), Hispanic (55.7%), unmarried (63.1%), and women (62.0%). 49% were non-English speakers. While patients had relatively few physical comorbidities (96.4% Charlson Comorbidity Index of 0), they were medically underserved – uninsured (72.0%) or receiving Medicaid (14.6%). Patients had a median of 2 visits per year (interquartile range=1–4) and 12% (n=7438) switched clinics during the 5-year study period.
In our study, 9.4% of all primary care visits were associated with psychiatric diagnoses. Visits were most commonly associated with depression (6.4%) and anxiety (3.1%), while posttraumatic stress disorder was rarely encountered (0.03%). Fewer than 1% of all visits were associated with alcohol (0.6%) or substance use disorders (0.2%). Psychiatric diagnoses that are typically considered serious mental illness and often require intensive mental health services, specifically schizophrenia (0.2%) and bipolar disorder (0.3%), were uncommonly associated with primary care visits among this safety-net population.
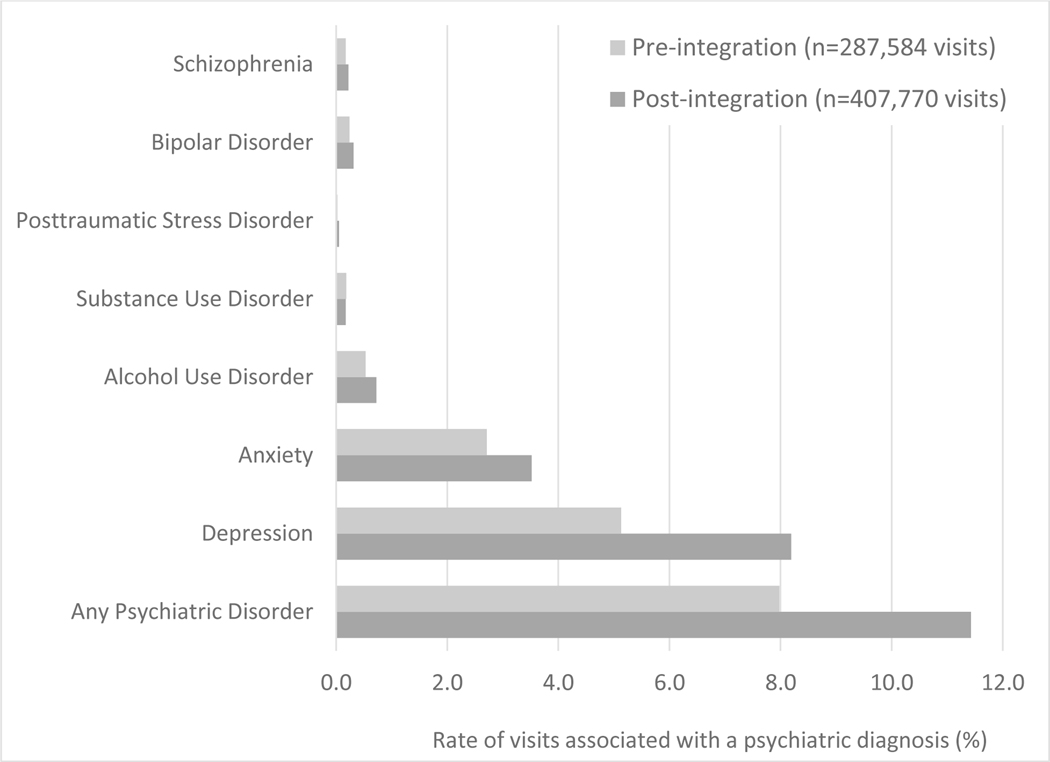
In unadjusted analyses, a higher proportion of primary care visits were associated with psychiatric diagnoses (8.0% pre- versus 11.4% post-implementation; p<.0001) and new psychiatric diagnoses (3.9% pre- versus 4.1% post-implementation; p<.0001) after MHIP implementation, compared to before (Figure 2). Findings persisted in fully adjusted models demonstrating a 9% higher odds of visits being associated with psychiatric diagnoses (95% confidence interval [CI]=1.05–1.13; p<.0001) and 10% higher odds of visits being associated with new psychiatric diagnoses (CI=1.04–1.16; p=0.002) pre- to post-MHIP implementation (Table 1). This change represents an increase in predicted probability of visits being associated with psychiatric diagnoses, from 8.1% pre- to 8.9% post-implementation (from 3.6 % pre- to 4% post-implementation for new psychiatric diagnoses), when controlling for all covariates at their means.
Figure 2. Percent of Primary Care Visits that were Associated with Psychiatric Diagnoses Before and After Clinic Mental Health Integration, 2009–2014.
There was a total of 695,354 primary care visits in the study sample. Light bars represent the proportion of visits associated with the designated psychiatric condition before clinic mental health integration. Dark bars represent the proportion of visits associated with the designated psychiatric condition after clinic mental health integration.
Table 1:
Proportion of Visits Associated with Psychiatric Conditions (Total and by Clinic Integration Status)
| Adjusted Results | |||||
|---|---|---|---|---|---|
| Visit Diagnostic Codes | Adjusted Odds Ratio | 95% Confidence Interval | p-value | ||
| Any Psychiatric Disorder | 1.09 | 1.05 | 1.13 | <.0001 | *** |
| New diagnosis | 1.10 | 1.04 | 1.16 | 0.002 | ** |
| Depression | 1.11 | 1.06 | 1.15 | <.0001 | *** |
| New diagnosis | 1.08 | 0.99 | 1.17 | 0.086 | |
| Anxiety | 1.06 | 0.99 | 1.13 | 0.093 | |
| New diagnosis | 1.07 | 0.96 | 1.19 | 0.221 | |
| Alcohol Use Disorder | 0.97 | 0.84 | 1.13 | 0.724 | |
| Substance Use Disorder | 0.90 | 0.67 | 1.21 | 0.490 | |
| Posttraumatic Stress Disorder | -- | -- | -- | -- | |
| Bipolar Disorder | 1.18 | 0.92 | 1.51 | 0.185 | |
| Schizophrenia | 1.05 | 0.80 | 1.39 | 0.705 | |
p<.05
p<.01
p<.001. We used clinic mental health integration status to predict odds of having a visit be associated with a psychiatric diagnosis. Adjusted odds ratios (and 95% confidence intervals) were reported from multilevel regression models, adjusting for time, clinic, and patient characteristics (i.e., age, sex, race-ethnicity, marital status, primary language, health insurance, Charlson Comorbidity Index). Due to small sample sizes, models did not converge for less common mental health diagnoses (i.e. posttraumatic stress disorder).
Similar trends were noted for primary care visits being associated with the two most common psychiatric disorders, depression (5.1% pre- versus 8.2% post-implementation; p<.0001) and anxiety (2.7% pre- versus 3.5% post-implementation; p<.0001) after MHIP implementation, compared to before. In fully adjusted models, these findings were significant for depression (odds ratio [OR]=1.11; CI=1.06–1.15; p=<.0001) but not for anxiety (OR=1.06; CI=.99–1.17; p=.093). This change represents an increase in predicted probability of visits being associated with depression diagnoses, from 4.6% pre- to 5.1% post-implementation, when controlling for all covariates at their means.
Significant differences among racial-ethnic and linguistic groups were observed for primary care visits being associated with psychiatric diagnoses. Odds of visits being associated with psychiatric diagnoses were consistently lower for minority patients, including Asian (OR=.39; CI=.36-.41; p<.0001), Black (OR=.67; CI=.63-.70; p<.0001), and Hispanic (OR=.82; CI=.78-.85; p<.0001), compared to White patients. Similarly, odds were 20% lower for Spanish- than English-speaking patients (CI=.78-.82; p<.0001). (Appendix 2) Predicted probabilities for patient subgroups having visits associated with psychiatric diagnoses are as follows: Asian (4%), Black (7%), Hispanic (9%), White (13%), Spanish-speaking (8%), and English-speaking (10%).
Discussion
In this study, the odds of primary care visits being associated with psychiatric diagnoses increased after implementation of mental health integration among LADHS clinics, after controlling for the effects of time, clinics, and relevant patient characteristics. Increases in post-MHIP visits were observed to a greater degree for new psychiatric diagnoses, suggesting improvements in disease detection from MHIP-supported depression screening.16 Accordingly, visits associated with depression, for which collaborative care models have been most often studied, appeared to drive observed MHIP-related increases.13 While some health systems have found no effect on mental health diagnoses and visit coding from collaborative care interventions,21 other systems have found greater availability of embedded specialists to be accompanied by increased use of mental health services by its primary care population.22 Despite the challenges of providing integrated care between separate, large public health agencies, the increased inclusion of psychiatric diagnoses in LADHS’s primary care documentation following integration provides encouraging support for a collaborative approach to care among safety-net health systems and adds to the mounting evidence for systematically enhancing care models to manage psychiatric diseases in primary care generally.13, 23 Findings also highlight the need for improvements toward services that address detection of new psychiatric diseases among users of public health systems.
During our five-year study period, only a small fraction (<10%) of primary care visits were associated with psychiatric needs—and an even smaller fraction of visits for addiction-related disorders (<1% of all primary care and mental visits). Findings add to extant research that mental health and substance abuse treatment remains out of reach for disadvantaged populations,3 despite the known widespread prevalence of psychiatric disease (over 1 in 4 in the United States),24 its contributions to national healthcare costs ($201 billion),4 and its global impact on disability (of which depression is the leading cause).5 Substance abuse treatment remains a particular challenge across different health systems.9 Yet, evidence continues to mount in favor of addressing common psychiatric issues, such as depression, anxiety, and alcohol use disorders, in a timely manner directly within primary care.13, 25 While significant variation in diagnostic coding of these psychiatric diseases existed from one primary clinic to another, our findings minimized bias by comparing the same eight clinics before and after staggered implementation of MHIP. Evaluations of mental health integration in other health systems that care for safety-net patients are needed to improve upon existing care models and to collectively address implementation and dissemination barriers.
Despite LADHS’s concerted efforts to support culturally aligned, equitable, high quality care for its diverse safety-net population, this evaluation highlights continued disparities in accessing mental health services among racial-ethnic minorities and non-English speaking patients.9, 11 Additional research is needed to understand whether MHIP implementation plays a role in mitigating or exacerbating existing racial-ethnic or linguistics disparities in mental health services use. While increasing adoption of universal screening and greater availability of behavioral health services may help mitigate disparities, other factors that contribute to racial-ethnic and language differences in mental health use require attention, such as accessibility of culturally and linguistically compatible providers and addressing mental health stigma and other health beliefs specific to minority groups.26 Future efforts may tackle racial-ethnic and linguistic disparities through implementation of mental health integration programs that explicitly target minority and groups and non-English speakers for increased outreach and treatment.
Though this study examines the longitudinal effects of county-wide program in a diverse patient cohort, our observational design does not permit causal inference and is limited by patients who are lost to primary care and drop out of our study cohort. In addition, as with all studies that rely on administrative data sources, there may be variation in the way mental health conditions were coded in the medical records by different providers and clinics. Furthermore, we do not know if increased coding in psychiatric diagnoses is equivalent to more psychiatric-related services being delivered. Finally, our study may be limited by co-occurring local quality improvement efforts (of which the authors were not aware), variable fidelity to program implementation, and other sudden clinic changes, such as a large influx or drop in number of patients served per clinic. Findings may not necessarily generalize to other health systems or to more recent time periods.
This evaluation documents early findings from one of few large-scale implementations of integrated mental health care programs within safety-net health systems. While MHIP increased access to mental health and substance abuse services in LA County, true integration will require building on early success and addressing gaps in addiction treatment and health care equity. In support of system-wide implementation, MHIP has necessitated adoption of technological innovations, such as eConsult, to improve communication with the Department of Mental Health18 and has required expansion to include additional collaborations with the Department of Public Health to address social determinants of health. There is new universal screening for unmet social needs, expanded addiction and social services (e.g., housing, food, transportation) for safety-net primary care patients. To assist with care coordination and social support, new mental health integration staff, including Clinical Social Work Supervisors, Clinical Social Workers, Medical Case Workers, Community Health Workers, and Substance Use counselors, have been added to primary care teams. Finally, mental health integration and associated services are currently accessible to all LACDHS primary care patients, with MHIP expanded to each and every safety-net clinic in the system. Efforts will hopefully deliver comprehensive safety-net care and enhance patient wellbeing within the Los Angeles County safety net.
Supplementary Material
Acknowledgments:
The authors would like to acknowledge Catherine Brayton, MPH and Jessica Severin, BS for their assistance in manuscript preparation.
Funding Statement: This work was funded by a Rapid Research Advances for Progress in Disparities (RRAPID) Mental Health Award from UCLA Clinical Translational Science Institute CTSI and California Behavioral Health Center of Excellence, supported by Mental Health Services Act funding allocated through Senate Bill 852. Dr. Leung us also supported by Career Development Award IK2 HX002867 from the United States Department of Veterans Affairs Health Services Research & Development Service.
Footnotes
Conflicts of Interest: None of the authors have any financial and other conflicts to disclose.
References
- 1.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance. JAMA Intern Med. Oct 1 2016;176(10):1501–1509. doi: 10.1001/jamainternmed.2016.4419 [DOI] [PubMed] [Google Scholar]
- 2.Seo V, Baggett TP, Thorndike AN, et al. Access to care among Medicaid and uninsured patients in community health centers after the Affordable Care Act. BMC Health Serv Res. May 8 2019;19(1):291. doi: 10.1186/s12913-019-4124-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rust G, Daniels E, Satcher D, Bacon J, Strothers H, Bornemann T. Ability of community health centers to obtain mental health services for uninsured patients. JAMA. Feb 2 2005;293(5):554–6. doi: 10.1001/jama.293.5.554-c [DOI] [PubMed] [Google Scholar]
- 4.Roehrig C. Mental Disorders Top The List Of The Most Costly Conditions In The United States: $201 Billion. Health affairs (Project Hope). Jun 1 2016;35(6):1130–5. doi: 10.1377/hlthaff.2015.1659 [DOI] [PubMed] [Google Scholar]
- 5.Friedrich MJ. Depression Is the Leading Cause of Disability Around the World. JAMA. Apr 18 2017;317(15):1517. doi: 10.1001/jama.2017.3826 [DOI] [PubMed] [Google Scholar]
- 6.Budhwani H, Hearld KR, Chavez-Yenter D. Depression in Racial and Ethnic Minorities: the Impact of Nativity and Discrimination. J Racial Ethn Health Disparities. Mar 2015;2(1):34–42. doi: 10.1007/s40615-014-0045-z [DOI] [PubMed] [Google Scholar]
- 7.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. Mar 2007;64(3):305–15. doi: 10.1001/archpsyc.64.3.305 [DOI] [PubMed] [Google Scholar]
- 8.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. Mar 2005;35(3):317–27. doi: 10.1017/s0033291704003514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Creedon TB, Cook BL. Access To Mental Health Care Increased But Not For Substance Use, While Disparities Remain. Health affairs (Project Hope). Jun 1 2016;35(6):1017–21. doi: 10.1377/hlthaff.2016.0098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Druss BG, Bornemann T, Fry-Johnson YW, McCombs HG, Politzer RM, Rust G. Trends in Mental Health and Substance Abuse Services at the Nation’s Community Health Centers: 1998–2003. Am J Public Health. Oct 2006;96(10):1779–84. doi: 10.2105/AJPH.2005.076943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Le Cook B, Manning W, Alegria M. Measuring disparities across the distribution of mental health care expenditures. J Ment Health Policy Econ. Mar 2013;16(1):3–12. [PMC free article] [PubMed] [Google Scholar]
- 12.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Serv Res. Apr 2003;38(2):613–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. Oct 17 2012;10:CD006525. doi: 10.1002/14651858.CD006525.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Advancing Integrated Mental Health Solutions. Collaborative Care. University of Washington. Accessed December 22, 2016, https://aims.uw.edu/collaborative-care [Google Scholar]
- 15.Starks SL, Arns PG, Padwa H, et al. System Transformation Under the California Mental Health Services Act: Implementation of Full-Service Partnerships in L.A. County. Psychiatr Serv. Jun 1 2017;68(6):587–595. doi: 10.1176/appi.ps.201500390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bao Y, McGuire TG, Chan YF, et al. Value-based payment in implementing evidence-based care: the Mental Health Integration Program in Washington state. Am J Manag Care. Jan 2017;23(1):48–53. [PMC free article] [PubMed] [Google Scholar]
- 17.Katzelnick DJ, Williams MD. Large-Scale Dissemination of Collaborative Care and Implications for Psychiatry. Psychiatr Serv. Sep 2015;66(9):904–6. doi: 10.1176/appi.ps.201400529 [DOI] [PubMed] [Google Scholar]
- 18.Leung LB, Benitez CT, Yee HF Jr. eConsult Mental Health: Electronic Referral and Consultation to Integrate Primary Care and Mental Health. The Journal of Ambulatory Care Management. 2019;42(1):47–50. [DOI] [PubMed] [Google Scholar]
- 19.Huynh AK, Lee ML, Farmer MM, Rubenstein LV. Application of a nonrandomized stepped wedge design to evaluate an evidence-based quality improvement intervention: a proof of concept using simulated data on patient-centered medical homes. BMC Med Res Methodol. Oct 21 2016;16(1):143. doi: 10.1186/s12874-016-0244-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. Jun 1992;45(6):613–9. [DOI] [PubMed] [Google Scholar]
- 21.Rossom RC, Solberg LI, Parker ED, et al. A Statewide Effort to Implement Collaborative Care for Depression: Reach and Impact for All Patients With Depression. Med Care. Nov 2016;54(11):992–997. doi: 10.1097/MLR.0000000000000602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leung LB, Rubenstein LV, Yoon J, et al. Veterans Health Administration Investments In Primary Care And Mental Health Integration Improved Care Access. Health affairs (Project Hope). Aug 2019;38(8):1281–1288. doi: 10.1377/hlthaff.2019.00270 [DOI] [PubMed] [Google Scholar]
- 23.Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. Jan 12 2000;283(2):212–20. doi: 10.1001/jama.283.2.212 [DOI] [PubMed] [Google Scholar]
- 24.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. Jun 2 2004;291(21):2581–90. doi: 10.1001/jama.291.21.2581 [DOI] [PubMed] [Google Scholar]
- 25.Watkins KE, Ober AJ, Lamp K, et al. Collaborative Care for Opioid and Alcohol Use Disorders in Primary Care: The SUMMIT Randomized Clinical Trial. JAMA Intern Med. Oct 1 2017;177(10):1480–1488. doi: 10.1001/jamainternmed.2017.3947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. May 2003;93(5):792–7. doi: 10.2105/ajph.93.5.792 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.