Abstract
Introduction:
Non-alcoholic fatty liver disease (NAFLD) is a growing problem in the United States and Hispanics experience the highest burden of this disease. Weight loss, physical activity (PA) and a healthy diet are the mainstay for NAFLD treatment, but patients experience barriers to behavior change. The purpose of this study was to identify barriers hindering Hispanic patients with NAFLD from making changes to PA and dietary habits.
Methods:
Participants referred to a multidisciplinary clinic completed self-administered questionnaires that measured barriers to greater PA engagement and eating healthier, with both close-ended and open-ended responses. One bilingual coder reviewed and categorized all open-ended responses.
Results:
The study population included 414 patients. The top five barriers for eating healthier were cost, perceptions that healthier food does not taste good, lack of time to cook, difficulty of cooking, and difficulty in going to the grocery store. Lack of time, feeling lazy, pain, a lack of place to exercise, and the perception that exercise is difficult were the top five barriers to PA engagement.
Conclusions:
Since Hispanic adults with NAFLD experience similar barriers to Hispanic adults more generally, existing behavioral lifestyle interventions may work well in this clinical population with some adaption for NAFLD-specific education.
Keywords: Hispanics, Latinos, diet, physical activity, barriers, behavior change, weight loss
Introduction
Non-alcoholic fatty liver disease (NAFLD) is the main hepatic consequence of excess body fat and is the leading cause of liver disease in the United States (Younossi et al., 2016). Hispanic/Latino (heretofore Hispanic) adults have the highest rates of NAFLD in the United States (Zhang et al., 2021). NAFLD can progress to highly morbid complications including cirrhosis and hepatocellular carcinoma (Younossi et al., 2016). Neither complication has a definitive cure apart from liver transplantation, which is unobtainable to most patients. Thus, treating NAFLD early and preventing these complications is vital.
Weight loss of 5% to 10% of one’s body weight through increased physical activity (PA) and dietary modifications is the only widely effective treatment for NAFLD (Chalasani et al., 2018). Increases in PA and modifications in dietary patterns have also been shown to reduce liver fat, even in the absence of significant weight loss (defined as ≥5% of baseline weight) (Romero-Gómez et al., 2017). However, it is difficult for patients with NAFLD to achieve and sustain lifestyle behavior change.
Structured behavioral interventions and programs can improve weight loss rates, but interventions targeted specifically for Hispanic patients with NAFLD do not exist. Culturally adapted interventions tend to be more effective than generic interventions (Barrera Jr et al., 2013; Hall et al., 2016). It is important that the interventions sufficiently address barriers that affect Hispanics with NAFLD. Barriers to improving PA and dietary habits are well documented among general populations of Hispanic adults (Chang et al., 2018; Greder et al., 2020; Ko et al., 2016; Larsen et al., 2015; Payán et al., 2019; Strong et al., 2016; Villegas et al., 2018); however, little known about the barriers that adults with NAFLD face (Haigh et al., 2019; Stine et al., 2020). Furthermore, to our knowledge, there are no published data available regarding the barriers experienced by Hispanic adults with NAFLD. Understanding the barriers that Hispanic patients with NAFLD grapple with is essential for appropriately targeting lifestyle interventions. Therefore, we conducted this study to identify barriers that hinder Hispanic patients with NAFLD from modifying their PA and dietary behaviors.
Methods
Study Design and Population
This study used data collected from 2015 to 2019 as part of the Harris County NAFLD Cohort (HCNC). The HCNC is an ongoing prospective cohort study that collects data from among Hispanic adult patients with NAFLD referred to a multidisciplinary clinic within a safety-net health care system in Harris County, Texas. NAFLD was diagnosed based on the presence of hepatic steatosis detected on liver imaging in the absence of clinical evidence for alternative liver disease etiologies (Chalasani et al., 2018) and 90% of patients responded to the questionnaire. This study was approved by the Institutional Review Boards of Baylor College of Medicine and Harris Health System. Patients first completed a written informed consent, followed by self-administered questionnaires that collected data on demographic characteristics, PA levels, dietary behaviors, and barriers to these behaviors.
Measures
Barriers.
Behavioral barriers were measured using two items. The first question, “If you could eat healthier, what is stopping you from eating healthier?” had five close-ended responses: “It is too difficult to cook healthy meals,” “It is too difficult to go to the grocery store,” “Healthy foods don’t taste good,” “Healthy foods take too much time to cook,” and “It costs more to eat healthy foods”. The second question, “If you think you need more physical activity, then what is stopping you?” had six close-ended responses: “I do not have time to exercise,” “It is too difficult to exercise,” “I feel too lazy to exercise,” “I have too much pain to exercise,” “There is no place for me to exercise”, and “It is too dangerous to exercise in my neighborhood.” For both items, participants were instructed to mark all relevant barriers (multiple responses were allowed) and there was additional space for open-ended responses.
PA and diet.
Physical activity was assessed with the Rapid Assessment of Physical Activity Scale. This scale has 7 items and asks participants about their PA engagement (Topolski et al., 2006). The National Cancer Institute’s Family Life, Activity, Sun, Health, and Eating (FLASHE) dietary screener was used to capture daily servings of fruit and vegetable intake (Smith et al., 2017).
NAFLD-specific dietary and PA guidelines do not exist. Therefore, we applied conventional, national guidelines to classify patients as meeting/not meeting target behaviors (Piercy et al., 2018). Participants were classified as active if they indicated engaging in moderate-intensity PA for ≥20 min/day for ≥5 days/week or vigorous-intensity PA for ≥30 min/day for ≥3 days/week. All other responses to the questionnaire were categorized as insufficiently active. Daily fruit and vegetable intake was quantified using two items that assessed the average number of servings consumed each day. In keeping with standard national guidelines (DeSalvo et al., 2016), participants were classified as meeting fruit and vegetable intake guidelines if they consumed at least 1½cups (women) or 2 cups (men) of fruit and 2½cups (women) or 3½cups (men) of vegetables daily. Those consuming less than these quantities were classified as not meeting guidelines.
Demographic and clinical characteristics.
Self-administered questionnaires measured demographic characteristics, including age, education, primary language, and country of birth. If born outside of the United States, participants were asked about age at migration to the United States and number of years living in the United States. The presence of prediabetes or type 2 diabetes was determined through medical evaluation. Patients’ height and weight were measured at study enrollment to calculate body mass index (BMI). We used standard BMI categories for analysis (normal 18 to <25 kg/m2, overweight ≥25 to <30 kg/m2, obese ≥30 kg/m2).
Statistical Analyses
To quantify open-ended responses to the barrier items, one bilingual coder (NH) reviewed all written-in responses in Spanish and English and developed codes for responses. Once all open-ended responses were coded, the coder went back through to consolidate similar categories. A total of nine more barrier categories emerged, six for eating healthier and three for PA engagement. We used univariate analyses to produce descriptive statistics of the sample and estimates of the top barriers and combination of barriers. We compared sociodemographic differences in the responses to barriers assessed with close-ended questions. Analyses were done using SPSS 26.0.
Results
This sample included 414 Hispanic patients with NAFLD; 86% identified Spanish as their primary language and 89% were born in Mexico or Central America (Table 1). Additionally, 97% were overweight or obese and 53% had diabetes.
Table 1.
Hispanic patients with NAFLD cohort characteristics
| Variable | All participants |
|---|---|
| M (SD) or N (%) | N = 414 |
| Age, M (SD) | 45.6 (11.2) |
| Primary Language | |
| Spanish | 349 (85.54) |
| English | 45 (11.03) |
| Both Spanish and English | 14 (3.43) |
| Country of Birth | |
| United States | 43 (10.83) |
| Mexico | 244 (61.46) |
| Central America | 110 (27.71) |
| Age migrated to the United States, M (SD) | 23.63 (11.19) |
| Length in United States (yr), M (SD) | 21.82 (10.34) |
| Education | |
| Less than High School | 186 (48.31) |
| High school degree | 119 (30.91) |
| Some higher education | 80 (20.78) |
| Diabetes | |
| No prediabetes or diabetes | 136 (32.85) |
| Diabetes | 221 (53.38) |
| Prediabetes | 57 (13.77) |
| BMI categories | |
| Normal Weight (18 to <25 kg/m2) | 12 (2.90) |
| Overweight (≥25 to <30 kg/m2) | 89 (21.50) |
| Obese (≥30 kg/m2) | 313 (75.60) |
| Physical activity | |
| Insufficiently Active | 227 (59.58) |
| Active | 154 (40.42) |
| Want to be more active | |
| Yes | 373 (94.20) |
| No | 23 (5.80) |
| Fruit and vegetable (FV) intake | |
| Not meeting FV intake guidelines | 327 (89.84) |
| Meeting FV intake guidelines | 37 (10.16) |
| Want to eat healthier | |
| Yes | 381 (97.44)) |
| No | 10 (2.56) |
Note: Missing: Primary language: n = 6, Country of birth: n = 17, education: n = 28, physical activity n = 33, fruit and vegetable intake n = 50, want to be more active n = 19, want to eat healthier n = 23.
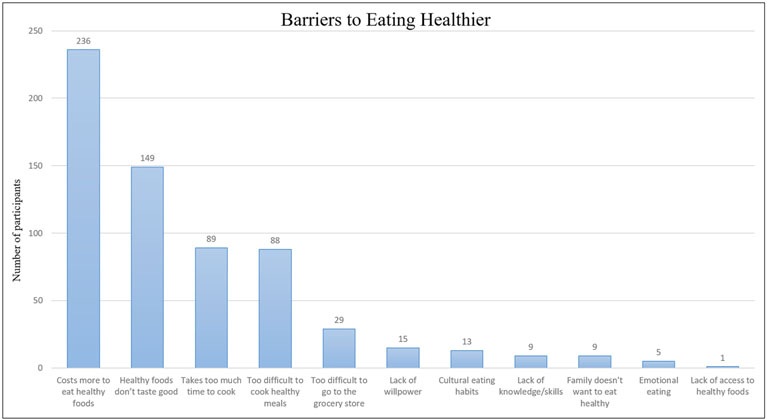
Almost 90% of patients did not meet national fruit and vegetable intake guidelines, though 97% wanted to eat healthier. The most salient barriers to eating healthier included perceptions that: it costs more to eat healthy foods (57%), healthy foods do not taste good (36%), healthy foods take too much time to cook (21%), and difficulty in cooking healthy meals (21%; Figure 1). Six additional barriers emerged from open-ended responses: a lack of willpower (4%), cultural eating habits interfering with attempts to eat healthier (3%), a lack of knowledge or skills to eating healthier (2%), family members not wanting to eat healthier (2%), eating for emotional reasons (1%) and a lack of access to healthy foods (<1%). Approximately 45% (n = 185) of participants reported more than one barrier to healthy eating. The most commonly reported combination of barriers was the perception that it costs more to eat healthy foods along with the perception that healthy foods do not taste good (n = 93). We did not find any striking differences in healthy eating barriers by sex, education, language, or country of origin.
Figure 1.
Barriers to eating healthier.
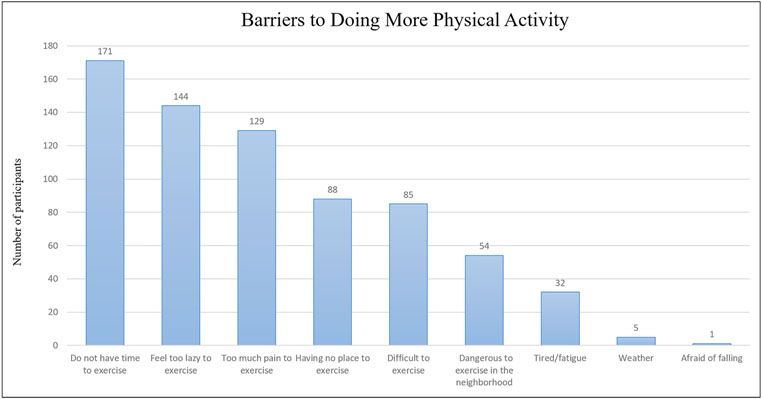
Almost 60% of patients were categorized as insufficiently active, though 94% of the overall sample indicated they wanted to be more active. The top barriers to engaging in more PA included not having time to exercise (41%), feeling too lazy to exercise (35%), and having too much pain to exercise (31%; Figure 2). Three additional barriers emerged from open-ended responses: tired/fatigue (8%), weather (1%), and being afraid of falling (1%). Approximately 48% (n = 199) of participants reported more than one barrier to PA engagement. The most common combinations of barriers reported were a combination of not having time with feeling too lazy to exercise (n = 62) and a combination of not having time with having no place to exercise (n = 60).
Figure 2.
Barriers to doing more physical activity.
There were demographic differences in barriers to PA engagement reported by participants. Women more frequently reported pain as a barrier than men (36% of women vs. 17% of men). A higher proportion of men (57%) reported a lack of time as a barrier than women (36%). We also found that having no place to exercise was a more commonly reported barrier in those with an 8th grade education or less (27%) compared to those with more than an 8th grade education (15%), and more commonly in those born in the U.S. (53%) than those born outside the U.S. (28%).
Discussion
To our knowledge, this is the first study to examine barriers related to dietary habits and PA levels among Hispanic patients with NAFLD. Although a higher proportion of patients did not meet dietary than guidelines, patients reported more barriers to PA engagement than healthy eating. We have found that the barriers observed among Hispanic patients with NAFLD are similar to barriers reported by qualitative and quantitative studies conducted among Hispanic adults (Table 2). Barriers specifically among adults with NAFLD have been reported by only two prior studies (Haigh et al., 2019; Stine et al., 2020). However, the lull breadth of barriers experienced by our study population were not captured by these previous two studies, neither of which represented the views of Hispanic patients with NAFLD in the U.S. (Table 2). This highlights the importance of research that addresses health behaviors specifically among Hispanic patients.
Table 2.
Comparison of most common barriers to lifestyle behaviors between Hispanic adults, adults with NAFLD, and Hispanic adults with NAFLD
| Hispanic adults |
Adults with NAFLD |
Hispanic adults with NAFLD (this study) |
|
|---|---|---|---|
| Eating | |||
| Costs more to eat healthy foods | X | X | |
| Healthy foods does not taste good | X | X | X |
| Takes too much time to cook | X | X | X |
| Too difficult to cook healthy meals | X | X | |
| Too difficult to go to grocery store | X | X | |
| Lack of willpower | X | X | X |
| Cultural eating habits | X | X | |
| Lack of knowledge or skills | X | X | |
| Family does not want to eat healthy | X | X | X |
| Emotional eating | X | X | |
| Lack of access to healthy foods | X | X | |
| Physical activity | |||
| Do not have time to exercise | X | X | X |
| Feel too lazy to exercise | X | X | |
| Too much pain to exercise | X | X | X |
| Having no place to exercise | X | X | |
| Difficult to exercise | X | X | |
| Dangerous to exercise in the neighborhood | X | X | |
| Tired/fatigue | X | X | X |
| Weather | X | X | X |
| Afraid of falling | X | X |
Time was the most frequently identified barrier to modifying PA and dietary behaviors among our study population. Time was similarly one of the most frequently reported barriers reported across studies conducted among general populations of Hispanic adults (Ko et al., 2016; Payán et al., 2019; Strong et al., 2016; Villegas et al., 2018) and the limited research that has been conducted among patients with NAFLD (Haigh et al., 2019). Beyond time, laziness, pain, perceived difficulty, and a lack of place to exercise were prominent barriers to PA engagement among our study population. Additional barriers to healthy eating included the perceived cost and taste of healthy foods, and perceived difficulties in cooking and going to the grocery store. Again, these barriers align with those previously reported by general populations of Hispanic adults (Chang et al., 2018; Ko et al., 2016; Larsen et al., 2015; Payán et al., 2019; Strong et al., 2016; Villegas et al., 2018). This is notable, as it supports the potential application of existing PA and nutrition promotion programs, with some adaption to include both NAFLD-specific education and culturally appropriate content. However, research is still needed to explore similarities and differences with other constructs that are key to lifestyle behaviors in Hispanic adults, such as self-efficacy and social support (Guntzviller et al., 2017; Heredia et al., 2019).
As noted, only two previous studies have assessed barriers to lifestyle change among patients with NAFLD: one, conducted in Northern Europe, assessed only barriers to dietary change and the second, conducted among a predominately non-Hispanic White population in the United States, assessed only barriers to PA (Haigh et al., 2019; Stine et al., 2020). In addition to identifying several more barriers experienced by Hispanic patients not captured by these previous studies, we found that barriers to pa engagement varied based on sex, educational level, and acculturation status among our study population. These differences are important considerations for future research as they may impact how to adapt interventions for specific target populations.
Strengths & Limitations
This paper focused on a population that experiences the highest burden of NAFLD in the United States: Hispanic adults. To our knowledge, we report for the first time barriers to two modifiable behaviors that prevent disease complications and may improve outcomes in this specific population. Single items were used to gauge barriers to PA (If you think you need more physical activity, then what is stopping you?) and eating healthier (If you could eat healthier, what is stopping you from eating healthier?) with several close-ended response options and an open-ended response option. We used this approach to minimize respondent burden and, consequently, were able to achieve a very high participation rate in the overall patient population (90%). We acknowledge that this approach may have limited the possibility of identifying additional barriers. Our study did mitigate this risk through the open-ended response option, which allowed nine additional barrier categories to emerge and enhanced the depth of the data collected. Previous research has used longer close-ended surveys. For example, Chang et al. (2018) asked participants 21 statements to measure seven barriers, with participants responding from “very unlikely” to “very likely” to statements such as “My free times during the day are too short to include exercise.” Qualitative methods, including focus groups or one-on-one interviews, are another method to consider, with previous research including prompts such as “Sometimes we want to makes changes to be even healthier in the way we live. What might stop you from trying to make healthy changes (in food, meals, physical activity)?” (Hammons et al., 2021). The decision to not use these more intensive data collection methods was a trade-off between participation rates and depth of data collection. Our findings serve as an important foundation that will help formulate future research questions, ideally integrating qualitative and quantitative methods, to continue to assess the full breadth of barriers to PA and healthy diet in Hispanic adults with NAFLD.
Conclusion
To appropriately design new or adapt existing interventions to manage NAFLD with lifestyle changes in Hispanic adults, it is crucial to first understand barriers that patients with NAFLD face to eating healthier and engaging in more PA. Research is still needed to explore other constructs that are key to successful behavioral lifestyle interventions. Since Hispanic adults with NAFLD appear to experience similar barriers to Hispanic adults without reported NAFLD, existing behavioral lifestyle interventions may work well in this clinical population with some adaptation for NAFLD-specific education.
Funding:
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article.
This work was supported in part by a National Institutes of Health grant P30 DK056338, which supports the Texas Medical Center Digestive Diseases Center. N.H. was supported, in part, by the Prevent Cancer Foundation.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Barrera M Jr, Castro FG, Strycker LA, & Toobert DJ (2013). Cultural adaptations of behavioral health interventions: A progress report. Journal of Consulting and Clinical Psychology, 81(2), 196. 10.1037/a0027085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, & Sanyal AJ (2018). The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology, 67(1), 328–357. 10.1002/hep.29367 [DOI] [PubMed] [Google Scholar]
- Chang C, Khurana S, Strodel R, Camp A, Magenheimer E, & Hawley N (2018). Perceived barriers to physical activity among low-income Latina women at risk for type 2 diabetes. The Diabetes Educator, 44(5), 444–453. 10.1177/0145721718787782 [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Olson R, & Casavale KO (2016). Dietary guidelines for Americans. JAMA, 315(5), 457–458. 10.1001/jama.2015.18396 [DOI] [PubMed] [Google Scholar]
- Greder K, Zaman A, Routh B, Hammons A, & Villegas E (2021). Rural Midwestern Mexican Fathers’ perspectives on family food, mealtimes, and physical activity. Ecology of Food and Nutrition, 60(4), 409–434. 10.1080/03670244.2020.1858408 [DOI] [PubMed] [Google Scholar]
- Guntzviller LM, King AJ, Jensen JD, & Davis LA (2017). Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. Journal of Immigrant and Minority Health, 19(2), 489–493. 10.1007/s10903-016-0384-4 [DOI] [PubMed] [Google Scholar]
- Haigh L, Bremner S, Houghton D, Henderson E, Avery L, Hardy T, & Anstee QM (2019). Barriers and facilitators to Mediterranean diet adoption by patients with nonalcoholic fatty liver disease in Northern Europe. Clinical Gastroenterology and Hepatology, 17(7), 1364–1371. e1363. 10.1016/j.cgh.2018.10.044 [DOI] [PubMed] [Google Scholar]
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, & Stice E (2016). A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy, 47(6), 993–1014. 10.1016/j.beth.2016.09.005 [DOI] [PubMed] [Google Scholar]
- Hammons A, Olvera N, Teran-Garcia M, Villegas E, & Fiese B (2021). Mealtime resistance: Hispanic mothers’ perspectives on making healthy eating changes within the family. Appetite, 159, 105046. 10.1016/j.appet.2020.105046 [DOI] [PubMed] [Google Scholar]
- Heredia NI, Walker TJ, Lee M, & Reininger BM (2019). The longitudinal relationship between social support and physical activity in Hispanics. American Journal of Health Promotion, 33(6), 921–924. 10.1177/0890117119828919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko LK, Rodriguez E, Yoon J, Ravindran R, & Copeland WK (2016). A brief community-based nutrition education intervention combined with food baskets can increase fruit and vegetable consumption among low-income Latinos. Journal of Nutrition Education and Behavior, 48(9), 609–617. e601. 10.1016/j.jneb.2016.06.010 [DOI] [PubMed] [Google Scholar]
- Larsen BA, Noble ML, Murray KE, & Marcus BH (2015). Physical activity in latino men and women: Facilitators, barriers, and interventions. American Journal of Lifestyle Medicine, 9(1), 4–30. 10.1177/1559827614521758 [DOI] [Google Scholar]
- Payán DD, Sloane DC, Illum J, & Lewis LB (2019). Intrapersonal and environmental barriers to physical activity among Blacks and Latinos. Journal of Nutrition Education and Behavior, 51(4), 478–485. 10.1016/j.jneb.2018.10.001 [DOI] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, & Olson RD (2018). The physical activity guidelines for Americans. JAMA, 320(19), 2020–2028. 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero-Gómez M, Zelber-Sagi S, & Trenell M (2017). Treatment of NAFLD with diet, physical activity and exercise. Journal of Hepatology, 67(4), 829–846. 10.1016/j.jhep.2017.05.016 [DOI] [PubMed] [Google Scholar]
- Smith TM, Calloway EE, Pinard CA, Hennessy E, Oh AY, Nebeling LC, & Yaroch AL (2017). Using secondary 24-h dietary recall data to estimate daily dietary factor intake from the FLASHE study dietary screener. American Journal of Preventive Medicine, 52(6), 856–862. 10.1016/j.amepre.2017.01.015 [DOI] [PubMed] [Google Scholar]
- Stine JG, Soriano C, Schreibman I, Rivas G, Hummer B, Yoo E, & Sciamanna C (2020). Breaking down barriers to physical activity in patients with nonalcoholic fatty liver disease. Digestive Diseases and Sciences, 1–8. 10.1007/s10620-020-06673-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong LL, Hoover DS, Heredia NI, Krasny S, Spears CA, Correa-Fernández V, & Fernandez ME (2016). Perspectives of Mexican-origin smokers on healthy eating and physical activity. Health Education Research, 31(4), 465–477. 10.1093/her/cyw026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, & Patrick MMB (2006). Peer reviewed: the Rapid Assessment of Physical Activity (RAPA) among older adults. Preventing Chronic Disease, 3(4), 1–8. [PMC free article] [PubMed] [Google Scholar]
- Villegas E, Coba-Rodriguez S, & Wiley AR (2018). Continued barriers affecting Hispanic families’ dietary patterns. Family and Consumer Sciences Research Journal, 46(4), 363–380. 10.1111/fcsr.12262 [DOI] [Google Scholar]
- Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, & Beckerman R (2016). The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology, 64(5), 1577–1586. 10.1002/hep.28785 [DOI] [PubMed] [Google Scholar]
- Zhang X, Heredia NI, Balakrishnan M, & Thrift AP (2021). Prevalence and factors associated with NAFLD detected by vibration controlled transient elastography among US adults: Results from NHANES 2017–2018. PloS One, 16(6), e0252164. 10.1371/journal.pone.0252164 [DOI] [PMC free article] [PubMed] [Google Scholar]