Abstract
From 2016 to 2019, the National Cancer Institute and the Centers for Disease Control and Prevention funded three Special Interest Projects focused on developing and testing multilevel HPV vaccination communication interventions. In this commentary, we highlight lessons learned from the funded projects, including the importance of engaging community members in the early stages of the research process, the challenges of evaluating multilevel interventions, and the need to consider stakeholder implementation preferences.
Implications.
Practice: Considering and being responsive to the preferences of partners and target communities can help ensure the success of multilevel HPV vaccine communication interventions.
Research: Further advancing multilevel HPV vaccine communication interventions will require the development of novel analytic methods for assessing both the individual and synergistic effects of intervention levels on study outcomes.
Policy: Policymakers can use lessons learned from multilevel intervention research to inform HPV vaccination efforts in their jurisdictions to achieve the Healthy People 2030 goal of 80% HPV vaccine coverage among adolescents.
INTRODUCTION
Human papillomavirus (HPV) vaccination is a powerful cancer prevention tool that protects against several types of cancer, including cervical, oropharyngeal, and anal cancer [1]. Despite robust evidence supporting the efficacy of the vaccine, HPV vaccination rates among adolescents remain below the Healthy People 2030 target of 80% coverage for both males and females [2,3]. The 2012–2013 President’s Cancer Panel Annual Report, “Accelerating HPV Vaccine Uptake: Urgency for Action to Prevent Cancer,” highlighted the importance of HPV vaccination as a national strategy for cancer prevention [4]. To achieve the goal of increasing uptake of the HPV vaccine, the report noted that research-tested, comprehensive communication strategies targeting healthcare providers, parents, caregivers, and eligible adolescents need to be developed [4]. The report also emphasized the importance of collaboration among researchers and partner organizations and the need to consider community context (e.g., local culture) in developing these communication strategies [4]. In a subsequent report published in 2018, the President’s Cancer Panel reviewed the ongoing challenges and opportunities in HPV vaccination and identified addressing inequalities among populations with high rates of HPV-related cancers (e.g., rural residents) as a priority [5].
In response to the first President’s Cancer Panel report on HPV vaccination, the National Cancer Institute (NCI) and Centers for Disease Control and Prevention (CDC) collaborated on a Special Interest Project (SIP) funding opportunity titled “Multilevel Communication Strategies to Promote HPV Vaccination Uptake” (HPV Vaccination SIP) in 2016. The ultimate goal of the funding opportunity was to increase HPV vaccination uptake among adolescents by promoting the development and testing of multilevel communication interventions to enhance vaccine acceptability, increase knowledge of vaccine benefits, address common misperceptions about HPV vaccine, address both initiation and completion of the vaccine series, reduce concerns about vaccine safety, and increase knowledge of cancer risk due to HPV. Through competitive awards to schools of public health or schools of medicine associated with the CDC’s Prevention Research Centers (PRC) network (https://www.cdc.gov/prc/), three teams were funded to conduct research around two aims: (1) developing and testing HPV communication messages for underserved and high-risk populations, with sensitivity to cultural considerations and other community-based factors; and (2) developing and testing multilevel communication strategies with partners (e.g., healthcare systems, community-based organizations) that address at least two levels within a socioecological framework [6]. The studies were approved by the Institutional Review Board at each funded institution. By emphasizing multilevel communication interventions, this initiative sought to advance communication research by building on prior HPV vaccine work that focused on a single intervention level (e.g., individual or organizational).
FOSTERING A MULTILEVEL APPROACH TO HPV VACCINE COMMUNICATION RESEARCH
Given that factors associated with HPV vaccination (e.g., personal knowledge, provider recommendations, use of clinic reminder systems) are multilevel [7], efforts to develop, test and implement communication strategies to promote HPV vaccine uptake may be most effective when research teams address multiple levels of the socioecological model—a conceptual framework that emphasizes factors across the intrapersonal (individual), interpersonal, institutional (organizational), community, and policy levels as targets for intervention [6]. In the context of the HPV vaccine, these factors may include adolescent, parent/caregiver, and healthcare provider attitudes at the intrapersonal level; interactions within families or between families and providers at the interpersonal level; leadership buy-in or health systems change at the organizational level; and values and norms at the community level.
Interest in the science of development and evaluation of multilevel interventions has grown, in part due to the increasing recognition that social and environmental factors influence successful behavior change and maintenance [8,9]. However, developing interventions impacting both individuals and the environments in which they live and work remains challenging [8]. Operationalizing relevant contextual features; identifying the most appropriate behavioral, social, organizational, community and policy targets for intervention; and measuring the influence one level has on another all remain significant hurdles to successfully implementing multilevel health interventions [8]. Other potentially important obstacles to multilevel health communication interventions include high cost and complex design [8]. Thus, the purpose of this commentary is to discuss the three multilevel communication interventions funded as part of the HPV Vaccination SIP to inform future multilevel work.
INTRODUCING THE RESEARCH PROJECTS
The first project, Multi-level Communication Strategies for HPV Vaccination Among Hmong Adolescents, was led by a research team based at the University of Minnesota Twin Cities. This project targeted Hmong-American adolescents and their parents as dyads. The study integrated intrapersonal factors influencing adolescents and their parents (e.g., knowledge, perception of risk, self-efficacy, cultural beliefs), and interpersonal factors influencing primary care providers’ delivery of HPV vaccinations (e.g., cultural competency). The project also explored organizational system changes to foster HPV vaccinations (i.e., electronic health record reminders) and investigated ways to mitigate societal cost factors by working with a federally qualified health center.
Focus groups with Hmong parents and adolescents were conducted to identify barriers and facilitators of vaccination across multiple levels of the socioecological model, including the individual level (e.g., low awareness, language barriers), community-level (e.g., narratives about traumatic experiences with vaccines, community connections), and institutional level (e.g., limited time in clinic appointments) [10]. Data from these focus groups informed the development of the multilevel intervention, including web-based applications for both adolescents and their parents (hmonghpv.com). For example, the concerns regarding literacy raised by Hmong parents during the focus groups [10] suggested that interventions needed to be language concordant and accessible. As a result, the parent-focused app was made available in both English and Hmong and had an audio option (where information was narrated rather than displayed as written text) to serve members of the community with lower levels of literacy. A pilot evaluation demonstrated that the app was successful in increasing knowledge about HPV and HPV vaccines, improving self-efficacy, and enhancing collaborative decision making among parents and adolescents. Although the study was not designed to assess HPV vaccine uptake, the number of children reported as having received at least one shot also increased from pre-intervention to follow-up [manuscript in preparation].
The second project, titled Promoting HPV Vaccines in Washington’s East African Communities, was led by a team at the University of Washington and focused on Somali, Ethiopian, and Eritrean immigrant populations. Informed by prior formative research [11] and focus groups with mothers [12] and healthcare providers [13], the multilevel communication intervention was culturally targeted to mothers and their adolescent children and was also directed at healthcare providers who serve patients in East African immigrant communities in Washington State. Components of the intervention included an online continuing education course for healthcare providers [13], interactive, native-language educational forums for mothers [14], and a comic book for adolescents [15].
Providers were recruited in 2018 to participate in the online continuing education course (HPV Vaccination: Framing the Conversation for East African Families [16]) and complete pre-test, post-test, and two-month follow-up surveys. The course, which was based on the Ask, Acknowledge, Advise communication model and focused on HPV vaccine concerns frequently voiced by mothers in East African communities, improved provider self-efficacy to recommend HPV vaccination to East African families and also increased their confidence in addressing common parental concerns [13].
The interventions for mothers and their 14–17-year-old adolescent children were delivered at ten ethno-linguistic-specific community dinner events (eight in the Somali community and two in the Ethiopian community) held between 2017 and 2018 [14]. Following communal socializing and a culturally appropriate meal, mothers participated in a 40-minute interactive session with a co-ethnic health professional, while adolescents read the comic book in a separate room. The impact of the intervention was evaluated using pre- and post-surveys, and results indicated that mothers’ HPV vaccine-related knowledge, attitudes, and intentions to vaccinate their adolescent children increased post-intervention [14]. Similarly, the comic book was effective at increasing adolescents’ HPV- and HPV-vaccine-related knowledge, comfort discussing the vaccine with parents, and willingness and intention to receive a vaccine [17]. Using the Washington State Immunization Information System to track vaccine uptake, the team found that the children of two of the 115 participating mothers had initiated HPV vaccination in the 6 months following the intervention [14].
The third project, Communicating Strategies to Increase HPV Vaccine Intentions, was conducted by researchers at the University of North Carolina. In this project, the team examined the multilevel message environment (public health messages, parent sentiment, and provider message delivery) to inform the development of an intervention to improve the frequency and quality of healthcare providers’ vaccine recommendations. The goal of the intervention was to ensure that providers had evidence-based messages to use when responding to parents’ concerns about HPV vaccination. The intervention targeted parents of adolescents at the individual level, parent-provider dyads at the interpersonal level, and clinics and professional associations at the organizational level.
To accomplish this, the research team catalogued and examined HPV vaccine messages in the public health communication environment [18], and then evaluated how effectively these messages address parental concerns through a survey with parents [19]. The team found that parents exposed to messages that addressed knowledge about HPV vaccines, included information about cancer prevention, were written at a higher reading level, and were longer, reported higher vaccine confidence and motivation [19]. Furthermore, the survey indicated that ending provider recommendations with clear advice to vaccinate the same day did not add much value after announcing that a child was due for the HPV vaccine and easing parental concerns using one of the tested messages, suggesting that expanding material on parental concerns and scaling back advice to vaccinate today would optimize the communication approach [20]. These findings were incorporated into an Announcement Approach communication training [21] to improve providers’ HPV vaccination recommendations. Providers’ attitudes toward vaccine discussions with parents, perceived norms, self-efficacy to address parental concerns, and HPV vaccine recommendation intentions are assessed pre-and post-training. Materials developed from the research are available at hpvIQ.org.
OPPORTUNITIES AND LESSONS LEARNED
The experiences of the three SIP teams offer lessons for future multilevel health communication intervention research. Considerations highlighted by the three SIP projects include different ways to conceptualize multilevel interventions, strategies for integrating community perspectives into intervention design, challenges in measuring outcomes across levels, and ways to improve intervention implementation and dissemination.
Conceptualizing and defining multilevel interventions: Integrating community perspectives
Due to the lack of a standardized definition for a “multilevel intervention” in the scientific literature [8], each team of investigators took a different approach to designing a multilevel intervention in order to accomplish the research aims proposed. This investigator-driven approach provided researchers with an opportunity to identify appropriate intervention levels based on their evaluation of a population’s needs, values, and resources, and consideration of the levers of influence for specific contexts.
The projects identified levels for intervention using conceptual frameworks, including the socioecological model [6]. However, operationalization of “multilevel” evolved for at least one project as the team responded to the needs and interests of the communities involved. The University of Minnesota team initially focused on communication targeting adolescents (individual level) and parents/families (interpersonal level), but focus groups indicated that providers and health systems (organizational level) were also critical to increasing HPV vaccination in this population. As a result, the team incorporated messages from providers into the intervention materials and started working to help link participants to local health care providers and systems.
Parameters for the intervention levels also sometimes had to be modified in response to community concerns and feedback. For example, the University of Washington team initially planned to target adolescents aged 11–17 at the individual level, but later narrowed the age range to 14–17 in order to ensure that the comic book content was both developmentally appropriate and appealing, based on focus group feedback. Similarly, although the team had initially proposed to intervene with physicians only, they expanded the organizational level intervention to include physician assistants, nurses, and medical assistants because formative research indicated these providers also played a key role in the vaccination process within the healthcare system for their target community. Thus, the flexibility offered to the research teams in defining a “multilevel intervention” allowed each team to delineate intervention levels most appropriate for their target community and be responsive to community needs.
Challenges and benefits of stakeholder engagement in designing multilevel interventions
Working with community members can help researchers identify the values and barriers to HPV vaccination that are important to target communities. Notably, while the scope of “community” and community- or stakeholder-engagement differed across the three projects, engagement in the formative stages of the research process facilitated the development of more targeted, culturally relevant interventions and established key partnerships, making interventions more sustainable and facilitating the use of multilevel approaches [22,23].
The University of Minnesota team worked with a community advisory board, community partners, and Hmong community researchers to develop appropriate intervention messages and translate them into the Hmong language. Developing appropriate, personalized, and culturally responsive content around HPV and HPV vaccination for Hmong adolescents and parents necessitated a substantial investment of time and resources early in the research process.
For the University of Washington team, focus groups offered an opportunity to get early buy-in from the intended audience. Like the University of Minnesota team, this team found that engaging target communities was resource-intensive. In addition, the translation of intervention materials into three different languages was found to be a distinct challenge for this project. Recruiting and training staff to conduct focus groups and facilitate intervention delivery and data collection at the mother/adolescent dinners in a consistent, standardized fashion was also challenging. In particular, dinner events required multiple staff members from target communities to recruit participants, facilitate intervention delivery, and administer the pre-/post-surveys. Notably, the team was ultimately unable to recruit the staff necessary to hold dinner events with the Eritrean community (despite holding a focus group with Eritrean mothers and translating intervention materials into Tigrinya). Although difficulties with staff recruitment and translation may pose a challenge for many single-level interventions, resource constraints are often magnified in multi-level interventions. For example, a larger team was needed to hold dinners for both mothers and adolescents than would have been the case if the intervention focused on just one group.
As part of their formative research, the team at the University of North Carolina completed an environmental scan of messaging in the communication environment and then gathered feedback on those messages from parents. The team reviewed, compiled, and categorized existing messages addressing parental concerns about HPV vaccination and created strategically different messages in each category to test via a survey of parents of adolescents. Unexpectedly, survey results indicated that parents preferred longer messages written at higher reading levels. Giving these messages to physicians would run counter to the team’s goal of providing shorter, more memorable messages that would be less burdensome for providers to remember and deliver. The team resolved the discrepancy between parent and provider needs by giving physicians shorter messages during the intervention training sessions but suggesting that providers could elaborate on the shorter messages to make them more effective. This experience demonstrates how formative research can help bring to light the potentially conflicting preferences and needs of various stakeholders across multiple levels, enabling researchers to preemptively address any potential issues in their intervention that might generate unintended consequences.
Measurement challenges and opportunities for multilevel interventions
Common data elements
The teams collectively began a conversation about common data elements that the three interventions could use. As the projects developed, each team negotiated the trade-off between creating a shared data ecosystem using established measures (e.g., a validated scale measuring self-efficacy) and ensuring measures were appropriate to local context. Finding a balance between these two goals presents a challenge to researchers seeking to incorporate validated prior measures into their work and perform comparative analyses across studies or with national data. The experience of the SIP projects suggests that adaptation of measures must be context-relevant and responsive to measurement needs at each intervention level. Developing a common definition of “levels” and taking an engaged approach with partners may also strengthen the acceptability of measures for cross-network collaboration in future initiatives.
Examination of synergistic effects across levels
A practical methodological question in multilevel research is how to assess both the individual and synergistic effects of intervention levels on study outcomes [24]. Such analyses often entail the application of complex statistical modeling (e.g., multilevel modeling, nested models) beyond more common procedures such as multivariable regression. Examination of this complexity requires careful planning and allocation of sufficient resources. At the same time, these methods can facilitate a deeper understanding of the impact of multilevel communication phenomena. For example, the University of North Carolina team found that multilevel analyses enabled them to identify specific principles for “what works” in messages addressing parental concerns regarding HPV vaccination. The team used multilevel linear models to examine how parental characteristics and message characteristics impact HPV vaccine confidence and motivation following exposure to provider-delivered HPV vaccine videos [19]. Examining those different factors enabled the team to determine how providers can communicate most effectively about the HPV vaccine with parents (emphasize vaccine benefits; do not express urgency) [19], and then incorporate those best practices into their provider communication training program.
When conducting multilevel interventions, researchers may need to consider the additional resources, time, and expertise required for the measurement and analysis of outcomes across multiple intervention levels. Multilevel conceptual models can help guide decision making on which constructs may be appropriate for evaluating multilevel influences on outcomes of interest, and these methods can be helpful in isolating key components of interventions when thinking about scaling up the interventions for broader implementation.
Considerations for dissemination and implementation
The combination of community partnerships and multilevel research can naturally lead to opportunities to facilitate the implementation and dissemination of communication interventions, since key stakeholders are engaged throughout the research process. Incorporating evaluation processes from implementation science models (e.g., [25]) that systematically measure stakeholder perceptions of the intervention, such as its feasibility and acceptability, could help ensure that interventions are able to be successfully implemented and scaled up, if found effective.
For the University of Washington team, measurement of such implementation outcomes provided a valuable tool for establishing buy-in with community partners, keeping them engaged, and avoiding burn-out over the course of intervention delivery. The University of Minnesota team gathered participant feedback on usability and satisfaction with the content and delivery of their web application to inform the future implementation and dissemination of the intervention. When utilized alongside behavioral outcomes, such as provider communication or vaccination uptake, these process measures can aid teams in better understanding appropriate delivery strategies and goodness of fit across each level of their intervention.
Another important lesson relevant to the implementation and dissemination of these interventions is the need to consider and respect the different implementation preferences of partners and target communities. The fact that multilevel interventions need to serve multiple audiences and be appropriate for multiple settings, suggests flexibility in dissemination strategies could be helpful. For instance, the University of North Carolina team partnered with the American Academy of Pediatrics to identify opportunities for state chapters to use the revised provider training intervention in their ongoing work. Each of the four state chapters the team worked with took a different approach to delivering the training: in one state, the chapter president delivered the training; in another state, the training was incorporated into an existing conference on adolescent health; a third state chapter worked with medical schools to deliver the training to residents; and in the last state the training was delivered during a monthly webinar. Each chapter had the flexibility to use the strategy that would be most effective for delivering the training to their respective communities, which expanded the reach of the intervention. In a similar vein, the University of Minnesota team realized that they would have to be flexible with their implementation approach to best serve their community’s needs. The team had initially planned to deliver their intervention through a mobile app, but based on formative research with the Hmong community, they came to understand that they would have more success implementing the intervention and recruiting for the study if they switched to a web-based application instead.
CONCLUSION
This commentary summarizes the experiences of three research teams in developing and delivering multilevel communication interventions to promote HPV vaccine uptake. A key lesson from this initiative is that a one-size-fits-all approach does not suit this type of work. Instead, for these pilot studies, multilevel interventions worked well in offering a flexible and adaptive structure for addressing an array of individual, interpersonal, organizational, and community needs that are likely to take different forms and be implemented differently from one community to the next. Although adapting interventions to community needs presented challenges to making comparisons across studies and developing generalizable approaches and measures, the flexibility that investigators had in conceptualizing their intervention was valuable because it allowed each team to select and operationalize the intervention levels, measures, and strategies that were most responsive to the needs of their target community.
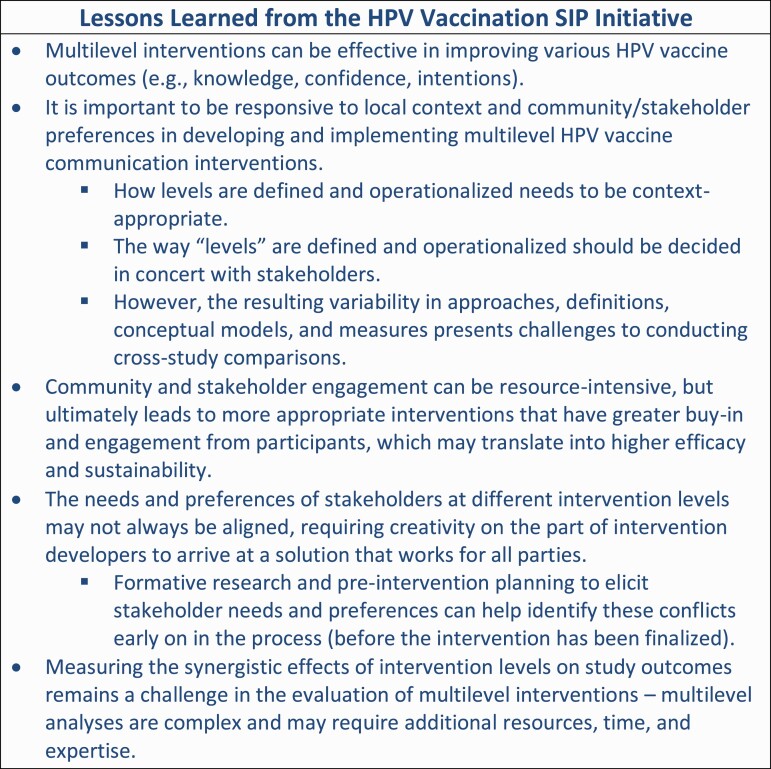
The projects described in this commentary represent initial steps toward achieving the integrated, comprehensive communication strategies and community partnerships called for in the President’s Cancer Panel reports [4,5] as critical actions for increasing HPV vaccination and ultimately reducing the burden of HPV cancers. The experience of the project teams demonstrates that a flexible and adaptive approach to developing multilevel interventions is necessary to ensure feasibility and acceptability when working with populations experiencing health disparities, and that engaging a diverse network of community members and partners in the research process is critical for intervention success. The complexity of the HPV vaccination landscape highlights the importance of tailored communication approaches across different contexts and settings, like those adopted by the SIP project teams, and the potential need for future adaptations of these interventions for different populations and organizations. Additional lessons learned through these innovative research efforts include the importance of engaging community members in the early stages of the research process (in order to identify multilevel barriers to vaccination, as well as potential misalignments in stakeholder perspectives at different levels), the need to develop advanced analytic methods for assessing both the individual and synergistic effects of intervention levels on study outcomes, and the need to be responsive to the implementation preferences of stakeholders to effectively disseminate these interventions (Fig. 1).
Fig. 1.
Lessons learned from the HPV vaccination SIP projects.
Contributor Information
April Oh, Division of Cancer Control and Population Sciences, National Cancer Institute, Rockville, MD, USA.
Anna Gaysynsky, Division of Cancer Control and Population Sciences, National Cancer Institute, Rockville, MD, USA; ICF Next Government, ICF, Rockville, MD, USA.
Rachel L Winer, Department of Epidemiology, University of Washington School of Public Health, Seattle, WA, USA.
Hee Y Lee, School of Social Work, University of Alabama, Tuscaloosa, AL, USA.
Noel T Brewer, Department Of Health Behavior, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, NC, USA; Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC, USA.
Arica White, Division of Cancer Prevention and Control, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Funding source: This publication is a product of the Prevention Research Centers Program at the Centers for Disease Control and Prevention (CDC). The work was supported by CDC and the National Cancer Institute (NCI) under Cooperative Agreement Numbers U48-DP005022, U48-DP005017, and U48-DP005013.
Compliance with Ethical Standards
Conflicts of Interest: Noel T. Brewer, Hee Y. Lee, and Rachel L. Winer received funding from CDC and NCI to conduct this work. Noel T. Brewer also serves as a paid advisor to Merck, WHO, and CDC on vaccines.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review boards of the funded institutions and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the studies described in the commentary.
Welfare of Animals: This commentary does not contain any studies with animals performed by any of the authors
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Cancer Institute.
References
- 1. Senkomago V, Henley S, Thomas C, Mix J, Markowitz L, Saraiya M. Human papillomavirus–attributable cancers—United States, 2012–2016. Morb Mortal Weekly Rep. 2019;68(33):724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Elam-Evans L, Yankey D, Singleton J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2019. Morb Mortal Weekly Rep. 2020;69(33):1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. U.S. Department of Health and Human Services – Office of Disease Prevention and Health Promotion. Increase the proportion of adolescents who get recommended doses of the HPV vaccine — IID-08. 2020. https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08.
- 4. The President’s Cancer Panel. Accelerating HPV Vaccine Uptake: Urgency for Action to Prevent Cancer. Bethesda, MD: National Cancer Institute; 2014. [Google Scholar]
- 5. The President’s Cancer Panel. HPV Vaccination for Cancer Prevention: Progress, Opportunities, and a Renewed Call to Action, Bethesda, MD: National Cancer Institute; 2018. [Google Scholar]
- 6. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. [DOI] [PubMed] [Google Scholar]
- 7. Rodriguez SA, Mullen PD, Lopez DM, Savas LS, Fernández ME. Factors associated with adolescent HPV vaccination in the U.S.: A systematic review of reviews and multilevel framework to inform intervention development. Prev Med. 2020;131:105968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hall KL, Oh A, Perez LG, et al. The ecology of multilevel intervention research. Transl Behav Med. 2018;8(6):968–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Agurs-Collins T, Persky S, Paskett ED, et al. Designing and Assessing Multilevel Interventions to Improve Minority Health and Reduce Health Disparities. Am J Public Health. 2019;109(S1):S86–S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xiong S, Kasouaher MY, Vue B, et al. “We will do whatever it takes”: Understanding Socioecological Level Influences on Hmong-American Adolescents and Parents’ Perceptions of the Human Papillomavirus Vaccine. J. Cancer Educat. 2021:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Greenfield LS, Page LC, Kay M, Li-Vollmer M, Breuner CC, Duchin JS. Strategies for increasing adolescent immunizations in diverse ethnic communities. J Adolesc Health. 2015;56(5 Suppl):S47–S53. [DOI] [PubMed] [Google Scholar]
- 12. Ko LK, Taylor VM, Mohamed FB, et al. “We brought our culture here with us”: A qualitative study of perceptions of HPV vaccine and vaccine uptake among East African immigrant mothers. Papillomavirus Res. 2019;7:21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McFadden SM, Ko LK, Shankar M, et al. Development and evaluation of an online continuing education course to increase healthcare provider self-efficacy to make strong HPV vaccine recommendations to East African immigrant families. Tumour Virus Res. 2021;11:200214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chu H, Ko LK, Ibrahim A, et al. The impact of an educational forum intervention on East African mothers’ HPV vaccine-related knowledge, attitudes, and intentions to vaccinate their adolescent children. Vaccine. 2021;39(28):3767–3776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Celentano I, Winer RL, Jang SH, et al. Development of a theory-based HPV vaccine promotion comic book for East African adolescents in the US. BMC Public Health. 2021;21(1):1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. HPV Vaccination: Framing the Conversation for East African Families [CME course]. 2018. http://www.cardeaservices.org/resourcecenter/hpv-vaccination-framing-the-conversation-for-east-african-families.
- 17. Shin M, Ko L, Ibrahim A, et al. The impact of comic book intervention on increasing East African-American adolescents’ HPV vaccine-related knowledge, attitudes and intentions to receive vaccine. American Public Health Association Annual Meeting and Expo. 2020. [Google Scholar]
- 18. Calo WA, Gilkey MB, Malo TL, Robichaud M, Brewer NT. A content analysis of HPV vaccination messages available online. Vaccine. 2018;36(49):7525–7529. [DOI] [PubMed] [Google Scholar]
- 19. Shah P, Calo W, Gilkey M, et al. Questions and concerns about HPV vaccine: a communication experiment. Pediatrics 2019;143(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shah PD, Calo WA, Gilkey MB, et al. Easing Human Papillomavirus Vaccine Hesitancy: A Communication Experiment With U.S. Parents. Am J Prev Med. 2021;61(1):88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brewer N, Hall M, Malo T, Gilkey M, Quinn B, Lathren C. Announcements versus conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics 2017;139(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Goodman MS, Sanders Thompson VL. The science of stakeholder engagement in research: classification, implementation, and evaluation. Transl Behav Med. 2017;7(3):486–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Meissner P, Cottler LB, Eder MM, Michener JL. Engagement science: The core of dissemination, implementation, and translational research science. J Clin Transl Sci. 2020;4(3):216–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cleary PD, Gross CP, Zaslavsky AM, Taplin SH. Multilevel interventions: study design and analysis issues. J Natl Cancer Inst Monogr. 2012;2012(44):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53. [DOI] [PMC free article] [PubMed] [Google Scholar]