Abstract
Background
Although troponin elevation is associated with worse outcomes among patients with coronavirus disease 2019 (COVID-19), prognostic implications of serial troponin testing are lacking. We investigated the association between serial troponin measurements and adverse COVID-19 outcomes.
Methods
Using Danish registries, we identified COVID-19 patients with a high-sensitivity troponin measurement followed by a second measurement within 1–24 h. All measurements during follow-up were also utilized in subsequent time-varying analyses. We assessed all-cause mortality associated with the absence/presence of myocardial injury (≥1 troponin measurement >99th percentile upper reference limit) and absence/presence of dynamic troponin changes (>20% relative change if first measurement elevated, >50% relative change if first measurement normal).
Results
Of 346 included COVID-19 patients, 56% had myocardial injury. Overall, 20% had dynamic troponin changes. In multivariable Cox regression models, myocardial injury was associated with all-cause mortality (HR = 2.56, 95%CI = 1.46–4.51), as were dynamic troponin changes (HR = 1.66, 95%CI = 1.04–2.64). We observed a low incidence of myocardial infarction (4%) and invasive coronary procedures (4%) among patients with myocardial injury.
Conclusions
Myocardial injury and dynamic troponin changes determined using serial high-sensitivity troponin testing were associated with poor prognosis among patients with COVID-19. The risk of developing myocardial infarction requiring invasive management during COVID-19 hospitalization was low.
Keywords: Coronavirus disease 2019, Myocardial injury, Troponin T, Troponin I, Outcomes
Graphical abstract
Prevalence of myocardial injury and dynamic cardiac troponin changes determined using serial high-sensitivity cardiac troponin testing and their association with all-cause mortality and future cardiovascular disease among patients with COVID-19.
Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; HR, hazard ratio; URL, upper reference limit.

1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2, constitutes an ongoing global pandemic with considerable implications for public health. As of February 01, 2022, >300 million cases have been reported in 188 countries, and >5 million deaths have been attributed to COVID-19 [1]. Patients with a high burden of cardiovascular risk factors or pre-existing cardiovascular disease appear to be particularly vulnerable during infection [2], [3], [4], [5], [6]. Furthermore, COVID-19 per se may increase the risk of cardiovascular complications such as arrhythmias, heart failure, or myocarditis [7], [8], [9].
Based on elevated cardiac troponin measurements at a single time point, early reports have shown a high, up to 36%, prevalence of myocardial injury among patients with COVID-19 [10], [11], [12], [13], [14], [15]. Besides isolated myocardial injury or type 2 myocardial infarction, such elevations may be indicative of myocarditis or type 1 myocardial infarction and may further be associated with both increased disease severity and mortality [10], [11], [12], [13], [14], [15]. While serial cardiac troponin testing plays crucial diagnostic and prognostic roles among patients presenting with acute-onset chest pain [16], [17], [18], [19], [20], evolving data also suggest that serial troponin assessment may improve prognostic stratification in patients with COVID-19 [21], [22], [23], [24].
Accordingly, in a Danish nationwide COVID-19 population undergoing serial testing with high-sensitivity cardiac troponin, we investigated prognostic implications of the absence/presence of myocardial injury and absence/presence of dynamic cardiac troponin changes. We further explored the incidence of diagnosed cardiovascular and non-cardiovascular conditions and related procedures following serial testing.
2. Methods
2.1. Data sources
Data from Danish nationwide administrative registries were linked on an individual level using a unique personal identifier. Data on age and sex were obtained from the Danish Civil Registration System, and vital status was acquired using the Danish Registry of Causes of Death. The Danish National Patient Registry was used to obtain data on inpatient and outpatient encounters based on International Classification of Diseases, 8th Revision (ICD-8) codes until 1994, after which ICD-10 codes were utilized. Through this registry, we also collected data on procedures based on Nordic Medico-Statistical Committee Classification of Surgical Procedures (NCSP) codes. From the Danish National Prescription Registry, we obtained data on filled prescriptions based on Anatomical Therapeutic Chemical (ATC) codes from all Danish pharmacies. Finally, blood test results were obtained from the Registry of Laboratory Results for Research. All registries have been described in detail previously [25], [26], [27], [28], [29].
2.2. Study setting and population
This study was conducted as a retrospective cohort study, in which all Danish residents >18 years of age were eligible for inclusion. Patients who were examined in a hospital and had a diagnosis of COVID-19 (ICD-10 codes: B342, B342A, B972, and B972A) registered after February 01, 2020, were included. The diagnosis code for COVID-19 has been validated previously with a positive predictive value of 98% [30]. The index date was the day of diagnosis of COVID-19. Patients were required to have a cardiac troponin measurement at or following the index date and a subsequent measurement within 1–24 h.
2.3. Myocardial injury and dynamic cardiac troponin changes
A variety of high-sensitivity cardiac troponin assays were used at the discretion of each institution: Elecsys Troponin T-high sensitive (Roche Diagnostics, 99th percentile upper reference limit [URL]: 14 ng/L), STAT-Troponin I (Abbott Diagnostics ARCHITECT, 99th percentile URL: 25 ng/L), Troponin I Ultra (Siemens Healthcare Diagnostics ADVIA Centaur, 99th percentile URL: 40 ng/L), Troponin I Flex reagent (Siemens Healthcare Dimension Vista, 99th percentile URL: 45 ng/L), and high-sensitivity troponin I (Siemens Healthcare Dimension Vista, 99th percentile URL: 59 ng/L).
In accordance with the Fourth Universal Definition of Myocardial Infarction [17], we defined myocardial injury as cardiac troponin >99th percentile URL on either measurement, while patients with cardiac troponin within the normal range on both measurements were considered to have no myocardial injury.
We defined dynamic cardiac troponin changes (i.e., significant rise and/or fall patterns) as a >20% relative change among those with cardiac troponin >99th percentile URL on the first measurement or >50% relative change among those with cardiac troponin within the normal range on the first measurement, as suggested by the European Society of Cardiology [20]. Therefore, patients with or without myocardial injury could present with dynamic cardiac troponin changes.
2.4. Covariates
Comorbidities of interest for the present study were ischemic heart disease including prior myocardial infarction, heart failure, atrial fibrillation or flutter, valvular heart disease, hypertension, hyperlipidemia, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, chronic liver disease, rheumatic disease, and malignancy. Drug prescriptions filled within 180 days prior to the index date that were recorded included angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers, beta-blockers, calcium channel blockers, diuretics, mineralocorticoid receptor antagonists, and antiplatelets. Since hypertension, hyperlipidemia, diabetes, and chronic obstructive pulmonary disease are often managed in primary care, patients may not necessarily have ICD codes registered. Accordingly, prior filled prescriptions for antihypertensives (at least dual therapy), lipid-lowering drugs, antidiabetics, and beta-adrenergic or anticholinergic inhalants were also used to define these conditions. Table S1 in the Supplement displays ICD-8, ICD-10, NCSP, and ATC codes used for the present study.
C-reactive protein (CRP), hemoglobin, D-dimer, and creatinine levels measured concomitantly with cardiac troponin were included as additional biomarkers, and the estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation [31].
2.5. Outcomes
Patients were followed from serial cardiac troponin testing to the occurrence of an outcome or censoring due to end of follow-up on August 26, 2020. The primary outcome was all-cause mortality. The secondary outcome was a composite of severe COVID-19 (ICD-10 code: B972A [i.e., COVID-19 with severe acute respiratory syndrome]), intensive care unit (ICU) admission (NCSP codes: NABE and NABB), or all-cause mortality.
The incidence of diagnosed cardiovascular and non-cardiovascular conditions and related procedures following serial cardiac troponin testing was also reported. Associated ICD-10 and NCSP codes are displayed in Table S2 in the Supplement.
2.6. Statistical analysis
Continuous variables were reported as medians (25th–75th percentiles) and categorical variables as counts (%). Between-group differences were assessed using Mann-Whitney U and chi-squared tests, as appropriate.
Absolute risks of outcomes according to the absence/presence of myocardial injury and absence/presence of dynamic cardiac troponin changes were estimated using the Kaplan-Meier method, and event distributions were compared with the log-rank test. Multivariable Cox proportional-hazards regression analysis was used to compute hazard ratios (HRs) with 95% confidence intervals (CIs) of the association between the absence/presence of myocardial injury or absence/presence of dynamic cardiac troponin changes and outcomes. We also performed a time-varying analysis to assess the associations, in which we utilized all cardiac troponin measurements for each patient and accounted for newly diagnosed comorbidities during follow-up [32].
All models were adjusted for age, sex, ischemic heart disease including prior myocardial infarction, heart failure, atrial fibrillation or flutter, valvular heart disease, hypertension, hyperlipidemia, diabetes, chronic obstructive pulmonary disease, and chronic kidney disease including eGFR <30 mL/min/1.73 m2.
Due to non-linearity, age was grouped by the median value (<71 or ≥71 years). The proportional-hazards assumption was assessed using Martingale residuals and was not violated. Models were also examined for statistical interactions between the absence/presence of myocardial injury or absence/presence of dynamic cardiac troponin changes, each covariate, and outcomes. In these analyses, a two-sided p-value < 0.01 was considered statistically significant, and no interactions were found. In all other analyses, a p-value < 0.05 was considered statistically significant.
Data management and analysis were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
2.7. Sensitivity analysis
To test the robustness of the association between the absence/presence of dynamic cardiac troponin changes and outcomes, we stratified the analysis by the absence/presence of myocardial injury, obtaining the following subgroups: no myocardial injury and no dynamic cardiac troponin changes (reference), no myocardial injury and dynamic cardiac troponin changes, myocardial injury and no dynamic cardiac troponin changes, and myocardial injury and dynamic cardiac troponin changes. Due to sample size limitations, we only adjusted for age and sex.
2.8. Ethics
In Denmark, registry-based studies do not require ethical committee approval or individual patient consent if the study is conducted for the sole purpose of statistics and scientific research, as defined in the Data Protection Act. Approval to use the data sources for research purposes was granted by the data responsible institute in the Capital Region of Denmark in accordance with the General Data Protection Regulation (approval number, P-2019-191).
3. Results
3.1. Patients and characteristics
Of 5490 confirmed cases of COVID-19 (Fig. 1), 1013 (19%) patients had at least one high-sensitivity cardiac troponin measurement during hospitalization. Differences in characteristics and outcomes between patients with and without cardiac troponin measurements are displayed in Table S3 in the Supplement. Overall, patients with cardiac troponin measurements were older, more often males, had a higher burden of cardiovascular disease, more often filled prescriptions for cardiovascular drugs, and were more likely to experience outcomes compared with those who did not have measurements available.
Fig. 1.
Flowchart of patient selection.
ASee Table S3 in the Supplement for comparison of characteristics and outcomes between patients with and without cardiac troponin measurements.
BSee Table S4 in the Supplement for comparison of characteristics and outcomes between patients with and without serial cardiac troponin testing.
Abbreviations: COVID-19, coronavirus disease 2019.
We included a total of 346 (34%) patients who underwent serial cardiac troponin testing, and characteristics appeared overall well balanced between these patients compared with those who did not have a second cardiac troponin measurement within 1–24 h (n = 667, 66%) (Table S4 in the Supplement).
Baseline characteristics of patients with serial cardiac troponin testing are shown in Table 1. A total of 195 (56%) patients had myocardial injury, of whom 173 (89%) had two concomitantly elevated cardiac troponin measurements, and 22 (11%) had only one elevated measurement. A total of 70 (20%) patients had dynamic cardiac troponin changes, of whom 42 (60%) had a rise pattern from first to second measurement. The most frequently utilized assay was Elecsys Troponin T-high sensitive (50%). Compared with patients without myocardial injury, those with myocardial injury were older, predominantly males, had higher CRP levels, and lower eGFR levels. They were also more likely to have cardiovascular comorbidities and fill prescriptions for cardiovascular drugs.
Table 1.
Patient characteristics.
| No myocardial injury (n = 151) | Myocardial injury (n = 195) | Total (n = 346) | p-Value | |
|---|---|---|---|---|
| Age, years | 63 [51.5–74.0] | 76 [68–83] | 71.5 [61–80] | <0.001 |
| Males | 77 (51.0) | 123 (63.1) | 200 (57.8) | 0.032 |
| High-sensitivity assay (99th percentile URL) | <0.001 | |||
| Elecsys Troponin T-high sensitive (14 ng/L) | 32 (21.2) | 141 (72.3) | 173 (50.0) | |
| STAT-Troponin I (25 ng/L) | 9 (6.0) | 5 (2.6) | 14 (4.0) | |
| Troponin I Ultra (40 ng/L) | <3 | 4 (2.1) | NA | |
| Troponin I Flex reagent (45 ng/L) | 31 (20.5) | 11 (5.6) | 42 (12.1) | |
| High-sensitivity troponin I (59 ng/L) | 77 (51.0) | 34 (17.4) | 111 (32.1) | |
| Time from COVID-19 diagnosis to first measurement, days | 2 [0–8] | 1 [0–5] | 1 [0–7] | 0.468 |
| Time from first to second measurement, hours | 17 [5–24] | 8 [5–19] | 10.5 [5–23] | <0.001 |
| Dynamic cardiac troponin changes present | 12 (7.9) | 58 (29.7) | 70 (20.2) | <0.001 |
| C-reactive protein, mg/L | 59 [13–143] | 76 [34–147] | 71 [19.0–146.5] | 0.248 |
| Missing | 6 | 6 | 12 | |
| Hemoglobin, mmol/L | 8.1 [6.9–8.7] | 7.6 [6.8–8.5] | 7.8 [6.8–8.6] | 0.301 |
| Missing | 12 | 6 | 18 | |
| D-dimer, mg/L | 1.0 [0.5–2.0] | 1.2 [0.7–2.9] | 1.1 [0.6–2.6] | 0.030 |
| Missing | 33 | 71 | 104 | |
| Estimated glomerular filtration rate, mL/min/1.73 m2 | 86 [71–97] | 64 [42.2–86.0] | 76 [52–92] | <0.001 |
| Missing | 8 | 5 | 13 | |
| Ischemic heart disease | 23 (15.2) | 66 (33.8) | 89 (25.7) | <0.001 |
| Myocardial infarction | 6 (4.0) | 33 (16.9) | 39 (11.3) | <0.001 |
| Heart failure | 6 (4.0) | 33 (16.9) | 39 (11.3) | <0.001 |
| Atrial fibrillation or flutter | 24 (15.9) | 58 (29.7) | 82 (23.7) | 0.004 |
| Valvular heart disease | 5 (3.3) | 25 (12.8) | 30 (8.7) | 0.003 |
| Hypertension | 41 (27.2) | 98 (50.3) | 139 (40.2) | <0.001 |
| Hyperlipidemia | 36 (23.8) | 88 (45.1) | 124 (35.8) | <0.001 |
| Diabetes | 23 (15.2) | 49 (25.1) | 72 (20.8) | 0.034 |
| Chronic obstructive pulmonary disease | 28 (18.5) | 48 (24.6) | 76 (22.0) | 0.222 |
| Chronic kidney disease | 8 (5.3) | 26 (13.3) | 34 (9.8) | 0.021 |
| Chronic liver disease | 6 (4.0) | 7 (3.6) | 13 (3.8) | 0.999 |
| Rheumatic disease | 10 (6.6) | 17 (8.7) | 27 (7.8) | 0.604 |
| Malignancy | 20 (13.2) | 36 (18.5) | 56 (16.2) | 0.246 |
| ACEIs or ARBs | 41 (27.2) | 85 (43.6) | 126 (36.4) | 0.002 |
| Beta-blockers | 27 (17.9) | 70 (35.9) | 97 (28.0) | <0.001 |
| Calcium channel blockers | 21 (13.9) | 40 (20.5) | 61 (17.6) | 0.145 |
| Diuretics | 25 (16.6) | 73 (37.4) | 98 (28.3) | <0.001 |
| Mineralocorticoid receptor antagonists | 7 (4.6) | 8 (4.1) | 15 (4.3) | 0.999 |
| Antiplatelets | 22 (14.6) | 59 (30.3) | 81 (23.4) | 0.001 |
Values reported as median [25th–75th percentiles] or n (%). p-values based on Mann-Whitney U and chi-squared tests, as appropriate.
Cells containing values <3 have been denoted in such a manner to withhold the exact number of patients to maintain confidentiality, as in compliance with rules by Statistics Denmark.
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; N/A, not applicable; URL, upper reference limit.
3.2. Myocardial injury, dynamic cardiac troponin changes, and adverse outcomes
Median (25th–75th percentiles) follow-up was 116 (45–146) days (primary outcome, i.e., all-cause mortality) and 45 (1−132) days (secondary outcome, i.e., composite of severe COVID-19, ICU admission, or all-cause mortality). A total of 89 patients (26%) died, and 174 (50%) experienced a secondary outcome event, most commonly severe COVID-19 (n = 84, 48%). Absolute risks of outcomes according to the absence/presence of myocardial injury and absence/presence of dynamic cardiac troponin changes are shown in Fig. 2. Overall, patients with myocardial injury had higher absolute risks, which was also the case for patients with dynamic cardiac troponin changes.
Fig. 2.
Absolute risk of primary (A) and secondary (B) outcomes according to the absence/presence of myocardial injury and absence/presence of dynamic cardiac troponin changes.
Abbreviations: COVID-19, coronavirus disease 2019; ICU, intensive care unit.
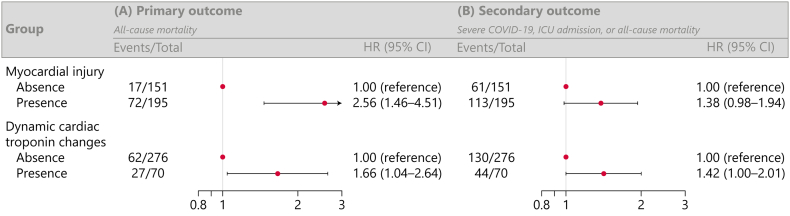
Adjusted HRs are shown in Fig. 3. The presence of myocardial injury was only associated with the primary outcome (HR = 2.56, 95% CI = 1.46–4.51). A significant association was not evident for the secondary outcome (HR = 1.38, 95% CI = 0.98–1.94). Similar findings were observed for the presence of dynamic cardiac troponin changes (primary outcome: HR = 1.66, 95% CI = 1.04–2.64; secondary outcome: HR = 1.42, 95% CI = 1.00–2.01).
Fig. 3.
Association between the absence/presence of myocardial injury or absence/presence of dynamic cardiac troponin changes and primary (A) and secondary (B) outcomes.
Adjusted for age, sex, ischemic heart disease including prior myocardial infarction, heart failure, atrial fibrillation or flutter, valvular heart disease, hypertension, hyperlipidemia, diabetes, chronic obstructive pulmonary disease, and chronic kidney disease.
Abbreviations: CI, confidence interval; COVID-19, coronavirus disease 2019; HR, hazard ratio; ICU, intensive care unit.
3.2.1. Time-varying analysis
Findings from the time-varying analysis are shown in Fig. 4. On average, patients had 3 cardiac troponin measurements suitable for assessing myocardial injury during follow-up, yielding 3505 measurements. Furthermore, patients had on average 1 pair of consecutive cardiac troponin measurements within 1–24 h of each other suitable for assessing dynamic cardiac troponin changes, yielding 1877 pairs of measurements. Overall, we observed a similar association with the primary outcome as in the main analysis (myocardial injury: HR = 2.24, 95% CI = 1.94–2.58; dynamic troponin changes: HR = 1.92, 95% CI = 1.59–2.31).
Fig. 4.
Time-varying analysis of the association between the absence/presence of myocardial injury or absence/presence of dynamic cardiac troponin changes and all-cause mortality.
Adjusted for age, sex, and changes in comorbidities (i.e., ischemic heart disease including prior myocardial infarction, heart failure, atrial fibrillation or flutter, valvular heart disease, hypertension, hyperlipidemia, diabetes, chronic obstructive pulmonary disease, and chronic kidney disease) during follow-up.
Abbreviations: CI, confidence interval; HR, hazard ratio.
3.2.2. Sensitivity analysis
In the sensitivity analysis, we observed that having the combination of both myocardial injury and dynamic cardiac troponin changes present was associated with the worst prognosis (primary outcome: HR = 3.75, 95% CI = 1.86–7.57; secondary outcome: HR = 1.85, 95% CI = 1.20–2.87) (Fig. S1 in the Supplement).
3.3. Diagnoses and procedures following serial cardiac troponin testing
Table 2 shows the incidence of cardiovascular and non-cardiovascular conditions and related procedures following serial cardiac troponin testing. Overall, patients with myocardial injury or dynamic cardiac troponin changes were more likely to be diagnosed with a cardiovascular condition. The incidence of myocardial infarction was low (4% among those with myocardial injury, 6% among those with dynamic cardiac troponin changes), and very few invasive coronary procedures, including coronary angiography or percutaneous coronary intervention (4% for both subgroups) and coronary artery bypass grafting (0% for both subgroups), were performed. No patients with myocardial injury or dynamic cardiac troponin changes were formally diagnosed with myocarditis or pericarditis. The most frequently occurring conditions were cerebrovascular disease, heart failure, and acute kidney injury including renal replacement therapy.
Table 2.
Incidence of diagnosed cardiovascular and non-cardiovascular conditions and related procedures following serial cardiac troponin testing.
| Myocardial injury |
Dynamic cardiac troponin changes |
|||
|---|---|---|---|---|
| Presence (n = 195) | Absence (n = 151) | Presence (n = 70) | Absence (n = 276) | |
| Any cardiovascular disease | 89 (45.6) | 47 (31.1) | 33 (47.1) | 103 (37.3) |
| Myocardial infarction | 8 (4.1) | <3 | 4 (5.7) | 5 (1.8) |
| Coronary angiography or percutaneous coronary intervention | 7 (3.6) | <3 | 3 (4.3) | 6 (2.2) |
| Coronary artery bypass grafting | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Heart failure | 16 (8.2) | <3 | 5 (7.1) | 13 (4.7) |
| Myocarditis or pericarditis | 0 (0.0) | <3 | 0 (0.0) | <3 |
| Aortic valve disease | 6 (3.1) | 4 (2.6) | <3 | 9 (3.3) |
| Ventricular arrhythmia or cardiac arrest | 3 (1.5) | <3 | <3 | 3 (1.1) |
| Pulmonary embolism | 8 (4.1) | 10 (6.6) | 5 (7.1) | 13 (4.7) |
| Aortic dissection | <3 | 0 (0.0) | 0 (0.0) | <3 |
| Cerebrovascular disease | 17 (8.7) | 5 (3.3) | 7 (10.0) | 15 (5.4) |
| Acute kidney injury including renal replacement therapy | 16 (8.2) | 6 (4.0) | 12 (17.1) | 10 (3.6) |
Values reported as n (%).
Cells containing values <3 have been denoted in such a manner to withhold the exact number of patients to maintain confidentiality, as in compliance with rules by Statistics Denmark.
4. Discussion
In this Danish nationwide study of hospitalized patients with COVID-19 undergoing serial high-sensitivity cardiac troponin testing, myocardial injury was highly prevalent and strongly associated with poor prognosis. The presence of a relative change between the first and second cardiac troponin measurements also carried prognostic significance among these patients. Time-varying analyses, in which we accounted for all suitable cardiac troponin measurements per patient and newly diagnosed comorbidities during follow-up, corroborated these initial findings. Conversely, the likelihood of developing myocardial infarction requiring invasive management was low (graphical abstract).
Our finding of adverse COVID-19 outcomes associated with myocardial injury based on serial high-sensitivity cardiac troponin assessment is in line with existing evidence [21], [22], [23], [24] and underscores the value of serial cardiac troponin measurements in patients with COVID-19. However, current evidence is limited by the definitions of myocardial injury employed, lack of data on serial testing and thereby dynamic cardiac troponin changes, use of inconsistent sampling intervals, and use of non-high-sensitivity assays [12]. As such, the exact prevalence and clinical implications of myocardial injury in COVID-19 remain unclear. Gou et al. [15] found that 28% of hospitalized Chinese patients with COVID-19 had myocardial injury, defined as a troponin T level >99th percentile URL, and these patients were more often older and had cardiovascular disease. The authors further noted that among patients with fatal COVID-19, cardiac troponin levels were higher during hospitalization compared with levels detected at admission. This association between increasing cardiac troponin during hospitalization and a fatal COVID-19 course was also noted in another study [5]. Shi et al. [10] demonstrated that 20% of hospitalized Chinese patients with COVID-19 had myocardial injury, defined as a high-sensitivity troponin I level >99th percentile URL, and also found older age and cardiovascular disease to be associated with cardiac troponin elevation. The authors further observed a more than 3-fold increased mortality risk among those with myocardial injury relative to those without. Finally, Lala et al. [14] reported the frequency of myocardial injury, defined as a troponin I level >30 ng/L, among US patients with COVID-19 to be 36%, and further observed a graded increase in mortality risk according to the degree of cardiac troponin elevation.
Overall, 20% met criteria for a relative change between the first and second cardiac troponin measurements using thresholds suggested by the European Society of Cardiology [20], and the association with all-cause mortality was strong. Although dynamic cardiac troponin changes hold diagnostic, and possibly prognostic, value, additional clinical data including cardiovascular symptoms, electrocardiogram, echocardiogram, and coronary angiography findings are warranted to determine if significant rise and/or fall patterns of cardiac troponin are due to myocardial infarction, particularly type 1, in COVID-19. However, only few patients received a diagnosis of myocardial infarction and underwent an invasive coronary procedure. This suggests that non-coronary mechanisms such as cerebrovascular disease, heart failure, or acute kidney injury may play an important role in the elevation of cardiac troponin. Furthermore, circulating levels of the inflammatory marker CRP are positively correlated with cardiac troponin, suggesting a link between COVID-19 virulence, increased systemic inflammation, and myocardial injury [2], [10], [15], [33].
Based on the low incidence of invasively treated myocardial infarction among COVID-19 patients with myocardial injury or dynamic cardiac troponin changes, we recommend clinicians to have an overall more judicious approach toward using cardiac troponin testing for the assessment of potential cardiac involvement of COVID-19. Only in cases where cardiac troponin measurement is clinically indicated, such as suspected type 1 myocardial infarction or myocarditis, should serial rather than single-point testing be performed because of the independent diagnostic and prognostic information that dynamic cardiac troponin changes then provide. Importantly, chest discomfort, which is frequent among patients with COVID-19, may not necessarily be associated with myocardial injury, and may even obscure true angina in the minority of patients who have type 1 myocardial infarction. Conversely, in case of myocardial injury determined on single-point testing, clinicians may also be tempted to initiate unnecessary examinations or treatments, which may lead to unwanted exposure of health care professionals during the pandemic. The optimal risk-benefit balance remains unclear as no specific means of differentiating myocardial injury from infarction in this setting has been established.
4.1. Limitations
Our study has several limitations. In particular, the observational design only allowed for the assessment of association, not causation. Danish patients with COVID-19 do not routinely undergo cardiac troponin testing, and those included were strictly required to have two measurements recorded temporally close to each other, which resulted in a limited sample size despite use of nationwide registry-based data. Furthermore, it is possible that a selection bias toward more severe cases of COVID-19, with a higher likelihood of having elevated cardiac troponin, was present. Indeed, patients who had cardiac troponin measurements available as well as patients who were subjected to serial testing had a higher cardiovascular disease burden and likelihood of experiencing adverse outcomes of COVID-19 than those without. Conversely, although most cases of COVID-19 in Denmark are located in the capital and more densely populated areas, the use of nationwide data with consecutively included patients with a positive COVID-19 infection was a major strength. Although we did adjust the multivariable models thoroughly, our registries do not hold data on potential confounding factors like cardiovascular symptoms, body mass index, smoking status, electrocardiographic changes, left ventricular ejection fraction, or imaging evidence of myocardial ischemia. Finally, data on cause of death were not available.
5. Conclusions
Myocardial injury was a common finding among patients with COVID-19, and cardiac troponin changes were present in one fifth of the population. The presence of myocardial injury and dynamic cardiac troponin changes determined using serial high-sensitivity cardiac troponin testing were both associated with poor prognosis. The risk of developing myocardial infarction requiring invasive management during COVID-19 hospitalization was low.
Funding
None.
CRediT authorship contribution statement
CP, KK, and MP conceptualized the hypothesis, designed the work, analyzed and interpreted the data, drafted the manuscript, and revised the manuscript critically for important intellectual content. MK, MA, JB, JP, EF, MS, DB, AS, LK, GG, CB, and CT designed the work, interpreted the data, and revised the manuscript critically for important intellectual content. All authors have read and approved the final version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the article are appropriately investigated and resolved.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Dr. Manan Pareek discloses the following relationships – Advisory Board: AstraZeneca, Janssen-Cilag; Speaker Honorarium: AstraZeneca; Bayer; Boehringer Ingelheim, Janssen-Cilag.
Dr. Deepak L. Bhatt discloses the following relationships - Advisory Board: Bayer, Boehringer Ingelheim, Cardax, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, Janssen, Level Ex, Medscape Cardiology, MyoKardia, NirvaMed, Novo Nordisk, PhaseBio, PLx Pharma, Regado Biosciences, Stasys; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: Inaugural Chair, American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Boston Scientific (Chair, PEITHO trial), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Contego Medical (Chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Novartis, Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Chair, ACC Accreditation Oversight Committee), Arnold and Porter law firm (work related to Sanofi/Bristol-Myers Squibb clopidogrel litigation), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Canadian Medical and Surgical Knowledge Translation Research Group (clinical trial steering committees), Cowen and Company, Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), K2P (Co-Chair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Piper Sandler, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co‑leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today's Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Cardax, CellProthera, Cereno Scientific, Chiesi, CSL Behring, Eisai, Ethicon, Faraday Pharmaceuticals, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Garmin, HLS Therapeutics, Idorsia, Ironwood, Ischemix, Janssen, Lexicon, Lilly, Medtronic, MyoKardia, NirvaMed, Novartis, Novo Nordisk, Owkin, Pfizer, PhaseBio, PLx Pharma, Regeneron, Roche, Sanofi, Stasys, Synaptic, The Medicines Company, 89Bio; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald's Heart Disease); Site Co-Investigator: Abbott, Biotronik, Boston Scientific, CSI, St. Jude Medical (now Abbott), Philips, Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, Takeda.
The other authors report no relevant disclosures.
Acknowledgements
None.
Footnotes
Supplemental material to this article can be found online at https://doi.org/10.1016/j.ahjo.2022.100131.
Appendix A. Supplemental material
Supplemental material
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., Ma K., Xu D., Yu H., Wang H., Wang T., Guo W., Chen J., Ding C., Zhang X., Huang J., Han M., Li S., Luo X., Zhao J., Ning Q. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368 doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., Liu L., Shan H., Lei C.L., Hui D.S.C., Du B., Li L.J., Zeng G., Yuen K.Y., Chen R.C., Tang C.L., Wang T., Chen P.Y., Xiang J., Li S.Y., Wang J.L., Liang Z.J., Peng Y.X., Wei L., Liu Y., Hu Y.H., Peng P., Wang J.M., Liu J.Y., Chen Z., Li G., Zheng Z.J., Qiu S.Q., Luo J., Ye C.J., Zhu S.Y., Zhong N.S., China medical treatment expert Group for C Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pareek M., Singh A., Vadlamani L., Eder M., Pacor J., Park J., Ghazizadeh Z., Heard A., Cruz-Solbes A.S., Nikooie R., Gier C., Ahmed Z.V., Freeman J.V., Meadows J., Smolderen K.G.E., Lampert R., Velazquez E.J., Ahmad T., Desai N.R. Relation of cardiovascular risk factors to mortality and cardiovascular events in hospitalized patients with coronavirus disease 2019 (from the Yale COVID-19 cardiovascular Registry) Am. J. Cardiol. 2021;146:99–106. doi: 10.1016/j.amjcard.2021.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Masoumi A., Jain S.S., Burkhoff D., Kumaraiah D., Rabbani L., Schwartz A., Uriel N. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 8.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., Brown T.S., Der Nigoghossian C., Zidar D.A., Haythe J., Brodie D., Beckman J.A., Kirtane A.J., Stone G.W., Krumholz H.M., Parikh S.A. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M., Madhur M.S., Tomaszewski M., Maffia P., D’Acquisto F., Nicklin S.A., Marian A.J., Nosalski R., Murray E.C., Guzik B., Berry C., Touyz R.M., Kreutz R., Wang D.W., Bhella D., Sagliocco O., Crea F., Thomson E.C., McInnes I.B. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020;116(10):1666–1687. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., Gong W., Liu X., Liang J., Zhao Q., Huang H., Yang B., Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi S., Qin M., Cai Y., Liu T., Shen B., Yang F., Cao S., Liu X., Xiang Y., Zhao Q., Huang H., Yang B., Huang C. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur. Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sandoval Y., Januzzi J.L., Jr., Jaffe A.S. Cardiac troponin for the diagnosis and risk-stratification of myocardial injury in COVID-19: JACC review topic of the week. J. Am. Coll. Cardiol. 2020;76(10):1244–1258. doi: 10.1016/j.jacc.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lombardi C.M., Carubelli V., Iorio A., Inciardi R.M., Bellasi A., Canale C., Camporotondo R., Catagnano F., Dalla Vecchia L.A., Giovinazzo S., Maccagni G., Mapelli M., Margonato D., Monzo L., Nuzzi V., Oriecuia C., Peveri G., Pozzi A., Provenzale G., Sarullo F., Tomasoni D., Ameri P., Gnecchi M., Leonardi S., Merlo M., Agostoni P., Carugo S., Danzi G.B., Guazzi M., La Rovere M.T., Mortara A., Piepoli M., Porto I., Sinagra G., Volterrani M., Specchia C., Metra M., Senni M. Association of troponin levels with mortality in Italian patients hospitalized with coronavirus disease 2019: results of a multicenter study. JAMA Cardiol. 2020;5(11):1274–1280. doi: 10.1001/jamacardio.2020.3538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lala A., Johnson K.W., Januzzi J.L., Russak A.J., Paranjpe I., Richter F., Zhao S., Somani S., Van Vleck T., Vaid A., Chaudhry F., De Freitas J.K., Fayad Z.A., Pinney S.P., Levin M., Charney A., Bagiella E., Narula J., Glicksberg B.S., Nadkarni G., Mancini D.M., Fuster V., Mount Sinai Covid informatics C Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J. Am. Coll. Cardiol. 2020;76(5):533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T., Wang H., Wan J., Wang X., Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neumann J.T., Twerenbold R., Ojeda F., Sorensen N.A., Chapman A.R., Shah A.S.V., Anand A., Boeddinghaus J., Nestelberger T., Badertscher P., Mokhtari A., Pickering J.W., Troughton R.W., Greenslade J., Parsonage W., Mueller-Hennessen M., Gori T., Jernberg T., Morris N., Liebetrau C., Hamm C., Katus H.A., Munzel T., Landmesser U., Salomaa V., Iacoviello L., Ferrario M.M., Giampaoli S., Kee F., Thorand B., Peters A., Borchini R., Jorgensen T., Soderberg S., Sans S., Tunstall-Pedoe H., Kuulasmaa K., Renne T., Lackner K.J., Worster A., Body R., Ekelund U., Kavsak P.A., Keller T., Lindahl B., Wild P., Giannitsis E., Than M., Cullen L.A., Mills N.L., Mueller C., Zeller T., Westermann D., Blankenberg S. Application of high-sensitivity troponin in suspected myocardial infarction. N. Engl. J. Med. 2019;380(26):2529–2540. doi: 10.1056/NEJMoa1803377. [DOI] [PubMed] [Google Scholar]
- 17.Thygesen K., Alpert J.S., Jaffe A.S., Chaitman B.R., Bax J.J., Morrow D.A., White H.D., Executive Group on behalf of the Joint European Society of Cardiology /American College of Cardiology /American Heart Association /World Heart Federation Task Force for the Universal Definition of Myocardial I Fourth universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72(18):2231–2264. doi: 10.1016/j.jacc.2018.08.1038. 2018. [DOI] [PubMed] [Google Scholar]
- 18.Ibanez B., James S., Agewall S., Antunes M.J., Bucciarelli-Ducci C., Bueno H., ALP Caforio, Crea F., Goudevenos J.A., Halvorsen S., Hindricks G., Kastrati A., Lenzen M.J., Prescott E., Roffi M., Valgimigli M., Varenhorst C., Vranckx P., Widimsky P., Group ESCSD 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 19.Roffi M., Patrono C., Collet J.P., Mueller C., Valgimigli M., Andreotti F., Bax J.J., Borger M.A., Brotons C., Chew D.P., Gencer B., Hasenfuss G., Kjeldsen K., Lancellotti P., Landmesser U., Mehilli J., Mukherjee D., Storey R.F., Windecker S., Group ESCSD 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2016;37(3):267–315. doi: 10.1093/eurheartj/ehv320. [DOI] [PubMed] [Google Scholar]
- 20.Thygesen K., Mair J., Giannitsis E., Mueller C., Lindahl B., Blankenberg S., Huber K., Plebani M., Biasucci L.M., Tubaro M., Collinson P., Venge P., Hasin Y., Galvani M., Koenig W., Hamm C., Alpert J.S., Katus H., Jaffe A.S., Study group on biomarkers in cardiology of ESCWGoACC How to use high-sensitivity cardiac troponins in acute cardiac care. Eur. Heart J. 2012;33(18):2252–2257. doi: 10.1093/eurheartj/ehs154. [DOI] [PubMed] [Google Scholar]
- 21.Ghossein M.A., Driessen R.G.H., van Rosmalen F., Sels J.E.M., Delnoij T., Geyik Z., Mingels A.M.A., van Stipdonk A.M.W., Prinzen F.W., Ghossein-Doha C., van Kuijk S.M.J., van der Horst I.C.C., Vernooy K., van Bussel B.C.T. Serial assessment of myocardial injury markers in mechanically ventilated patients with SARS-CoV-2 (from the prospective MaastrICCht Cohort) Am. J. Cardiol. 2022;170:118–127. doi: 10.1016/j.amjcard.2022.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nuzzi V., Merlo M., Specchia C., Lombardi C.M., Carubelli V., Iorio A., Inciardi R.M., Bellasi A., Canale C., Camporotondo R., Catagnano F., Dalla Vecchia L.A., Giovinazzo S., Maccagni G., Mapelli M., Margonato D., Monzo L., Oriecuia C., Peveri G., Pozzi A., Provenzale G., Sarullo F., Tomasoni D., Ameri P., Gnecchi M., Leonardi S., Agostoni P., Carugo S., Danzi G.B., Guazzi M., La Rovere M.T., Mortara A., Piepoli M., Porto I., Volterrani M., Senni M., Metra M., Sinagra G. The prognostic value of serial troponin measurements in patients admitted for COVID-19. ESC Heart Fail. 2021;8(5):3504–3511. doi: 10.1002/ehf2.13462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Marzo V., Di Biagio A., Della Bona R., Vena A., Arboscello E., Emirjona H., Mora S., Giacomini M., Da Rin G., Pelosi P., Bassetti M., Ameri P., Porto I., Gecovid Study G. Prevalence and prognostic value of cardiac troponin in elderly patients hospitalized for COVID-19. J Geriatr Cardiol. 2021;18(5):338–345. doi: 10.11909/j.issn.1671-5411.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zaninotto M., Mion M.M., Padoan A., Babuin L., Plebani M. Cardiac troponin I in SARS-CoV-2-patients: the additional prognostic value of serial monitoring. Clin. Chim. Acta. 2020;511:75–80. doi: 10.1016/j.cca.2020.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arendt J.F.H., Hansen A.T., Ladefoged S.A., Sorensen H.T., Pedersen L., Adelborg K. Existing data sources in clinical epidemiology: laboratory information system databases in Denmark. Clin. Epidemiol. 2020;12:469–475. doi: 10.2147/CLEP.S245060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helweg-Larsen K. The danish register of causes of death. Scand. J. Public Health. 2011;39(7 Suppl):26–29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 27.Kildemoes H.W., Sorensen H.T., Hallas J. The Danish National Prescription Registry. Scand. J. Public Health. 2011;39(7 Suppl):38–41. doi: 10.1177/1403494810394717. [DOI] [PubMed] [Google Scholar]
- 28.Lynge E., Sandegaard J.L., Rebolj M. The Danish National Patient Register. Scand. J. Public Health. 2011;39(7 Suppl):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 29.Pedersen C.B. The danish civil registration system. Scand. J. Public Health. 2011;39(7 Suppl):22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 30.Fosbol E.L., Butt J.H., Ostergaard L., Andersson C., Selmer C., Kragholm K., Schou M., Phelps M., Gislason G.H., Gerds T.A., Torp-Pedersen C., Kober L. Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. JAMA. 2020;324(2):168–177. doi: 10.1001/jama.2020.11301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levey A.S., Stevens L.A., Schmid C.H., Zhang Y.L., Castro A.F., 3rd, Feldman H.I., Kusek J.W., Eggers P., Van Lente F., Greene T., Coresh J., Ckd E.P.I. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomas L., Reyes E.M. Tutorial: survival estimation for cox regression models with time-varying coefficients using SAS and R. J. Stat. Softw. 2014;61(1):1–23. [Google Scholar]
- 33.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from WuhanChina. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material