Abstract
Background
French Guiana is used as a drug trafficking pipeline of cocaine to Europe. The number of arrests for transporting cocaine in corpore has increased exponentially in recent years. Since 2010, Cayenne Hospital's emergency care unit has applied a medical management protocol system for body‐packers. Our objective was to describe the epidemiology of body‐packers and to evaluate medical management.
Method
A retrospective descriptive study was performed among patients hospitalized in Cayenne Hospital for transporting cocaine in corpore between January 2010 and November 2015. In addition, a qualitative study including interviews of body‐packers imprisoned in Rémire‐Montjoly prison was conducted in April 2016.
Result
A total of 282 patients were included in the study. The median age was 24 years and the sex ratio M/W was to 4/1. Among them, 3.5% showed signs of severity (9 with pre‐existing condition and 1 with severe form). No surgery or deaths were reported. Ten endoscopies were performed because of the delay in evacuation without complications. Approximately 28% of patients had urinary screening, of which 60.7% were positive. The median length of stay was 1.8 days. Prolonged length of stay was significantly associated with the presence of gastrointestinal symptoms, hypoglycemia, or having swallowed a minimum of 10 pellets.
Conclusion
This study led to a change in the management of body‐packers in the hospital setting in Guiana. A computed tomography scan at discharge became more prevalent. Endoscopy has emerged as an effective and safe alternative to surgery. Despite the increase in the number of patients treated, it should be noted that there were few complications and no deaths in our cohort.
Keywords: body packer, body packing, cocaine, drug, French Guiana, mule
1. INTRODUCTION
Cocaine is a stimulant of the central nervous system and its consumption is booming in Western countries. 1 Cocaine produced in Colombia and Venezuela transits through the airports of Suriname and French Guiana (FG) to reach the European market. In the last decade, FG has become a hub for cocaine trafficking. At the local level, this has resulted in a significant increase in the number of arrests related to the transportation of cocaine, particularly in Cayenne, the main city and location of the main airport.
Body‐packers are defined as people who ingest professionally packaged illicit drugs for the purpose of smuggling. The number of persons arrested and hospitalized for being suspected body‐packers increased from 22 in 2011 to 176 in 2015. The transport of cocaine pellets by body‐packing may expose the patient to severe medical complications such as acute cocaine poisoning, bowel obstruction, or perforation. 2 Each swallowed pellet contains between 8 and 10 g of cocaine, which is 8 times the potential lethal dose. 3 Cocaine pellets have been classified since 1983 into categories according to the quality of packaging 4 : type 1, with a high risk of fracture, corresponds to handcrafted manufacture by manually superimposing condoms or other plasticized containers, whereas type 2 responds to a semi‐industrial mode of manufacture by several layers of superimposed latex surrounding a very compact powder and is at very low risk of rupture. These are currently the 2 main types of pellets identified in FG.
The main objective of our study was to describe body‐packers and medical practices at Cayenne Hospital between 2010 and 2015, in order to optimize the medical care of people transporting cocaine in corpore.
2. MATERIAL AND METHODS
2.1. Study design and population
This is a retrospective case series of suspected body‐packers from Cayenne Hospital from January 2010 to November 2015.
2.2. Inclusion and exclusion criteria
Suspected patients were recruited in 2 ways: taken into custody by airport customs or rarely self‐referred to the emergency department (ED) claiming to have ingested cocaine pellets. All suspected patients underwent abdominal radiography to confirm or deny the presence of intrabody pellets. The exclusion criteria were the absence of pellets in the abdominal X‐ray. A confirmed body‐packer was defined by the presence of pellets in the abdominal x‐ray or by the witnessed excretion of pellets.
2.3. Data collection, definition of terms, and analysis
The Bottom Line.
Often practiced for transporting illicit substances, body packing can be harmful if the packing medium breaks down. In this series of 282 body‐packers treated in French Guinea, no patients died or required surgery. Only 3.5% had signs of drug toxicity, and none required treatment. Interventions included an initial X‐ray and an osmotic laxative with monitoring an average of 1.8 days. Ten endoscopies were performed after incomplete evacuation after a week.
Data extracted from patient's records included age, sex, history of addiction or disease, type of illicit substance and number of packets, clinical presentations, radiographic finding(s), and follow‐up data. Patients were classified as asymptomatic or symptomatic. Symptomatic forms were divided into simple and severe forms. A severe symptomatic form was defined by the failure of 1 or more organs related to cocaine intoxication including seizures, hemorrhagic and ischemic strokes, myocardial infarction, aortic dissection, rhabdomyolysis, mesenteric ischemia, acute renal injury and multiple organ failure or mechanical complication of the pellets, such as intestinal obstruction. 5 Cocaine poisoning was defined by the presence of clinical signs that could not be explained by the arrest alone (stress, anxiety) AND by the presence of known clinical signs of cocaine poisoning AND by the presence of a positive urine test for cocaine (look for metabolite benzoylecgonine). Hospitalization criteria included confirmed body‐packing or inability to perform medical imaging. The length of hospitalization depended mainly on the time of expelling of the pellets. High blood pressure was defined by systolic pressure higher than 145 mm Hg associated to diastolic pressure higher than 95 mm Hg, tachycardia was defined as a pulse over 100 beats/min. The duration of 4 days’ hospitalization chosen in the analysis corresponded to the maximal period of police custody.
2.4. Management of body‐packers at the Cayenne Hospital
The medical management of patients hospitalized for body‐packing is not consensus‐based and varies between centers and host countries. According to the local protocol implemented in 2010, abdominal X‐ray and sacrum profile confirmed the diagnosis at the time of arrival at the hospital, after an initial consultation by a doctor of Medical Judicial Unit (forensic medicine). Patients were only referred to the ED if the diagnosis was confirmed. Then, a clinical evaluation was performed for each patient with the prescription of standard biological examinations and a urine test for metabolite benzoylecgonine detection. Patients were hospitalized in a medical ward under police surveillance if the initial assessment was normal. In other cases, close medical surveillance was provided at the intensive care unit. The collection of pellets was carried out under the supervision of a police officer. Vital signs were only recorded 3 times daily unless an anomaly was reported by police officers. A radiological examination was performed during hospitalization when the elimination of the pellets was supposed to be complete. It was repeated until no pellets were present. In case of doubt about the persistence of pellets, an abdomino‐pelvic computed tomography (CT) was performed. A daily osmotic laxative treatment was prescribed. A digestive endoscopy was considered in case of incomplete evacuation after 1 week. The final decision was made by the specialist in charge of the endoscopy.
2.5. Statistical analysis
The data was collected using the Microsoft Excel 2010 software and analyzed with STATA 12.0 software (College Station, TX, USA). Continuous variables were described by calculating the median and interquartile range and binomial variables using frequencies and percentages. The variables were compared in bivariate analysis using a chi‐square test for binomial variables. The significance threshold was set at 5%.
2.6. Ethical and regulatory approval
Regulatory approval was given by the Commission Nationale Informatique et libertés (CNIL19963570). The study was approved by the Ethics Committee of Cayenne Hospital and each patient who participated in the interviews signed an informed consent form.
3. RESULTS
3.1. General data
Over the period from January 2011 to November 2015, 480 patients were admitted to Cayenne Hospital for suspicion of body‐packing. Abdominal radiography was positive for 256 patients (53.3%). Including the 26 confirmed cases of 2010 (no data available for suspected cases), 282 patients were confirmed body‐packers (Figure 1). The percentage of suspected but unconfirmed cases was 60% from 2011 to 2013 and decreased to 35.7% in 2014 and 27.5% in 2015. Among the 282 confirmed body‐packers, and the sex ratio M/W was to 4/1 and the median age was 24 years (interquartile range [IQR], 20–31; range, 15–64). Sixteen patients (5.7%) were minors (15–17 years) and 116 patients (41.1%) were hospitalized in 2015 alone (Figure 2). The median length of stay was 1.8 days. Seventy‐nine urine cocaine‐screening tests were performed (28.0%) and 60.7% were positive. The diagnosis was confirmed by abdominal X‐ray for 278 patients (98.6%), according to the local protocol. Six CT scans (2.2%) were performed before hospital discharge, all were negative. Thirty‐six patients (12.8%) were hospitalized for >4 days (maximum legal length of police custody) and 5 for >10 days.
FIGURE 1.
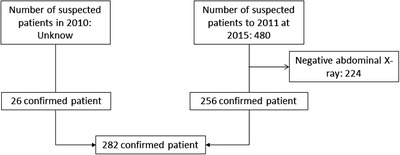
Flow chart of the study
FIGURE 2.
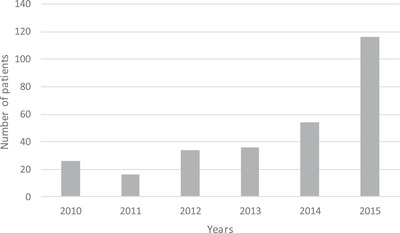
Number of confirmed body‐packing patients hospitalized at Cayenne Hospital per year (n = 282)
3.2. Clinical presentations at the emergency
Among the 282 study patients, 141 were asymptomatic (50.0%), 140 were symptomatic without complications (49.6%), and 1 presented with severe symptoms (0.4%). Among the symptomatic forms, 63.4% of patients had tachycardia (n = 90) and 35.5% high blood pressure (n = 50) that decreased to 0.7% and 7.8%, respectively, during hospitalization. Abdominal symptoms were notified for 17.8% of the patients (n = 23/129), mostly abdominal pain or vomiting. Among the 141 symptomatic patients, 9 (6.4%) had more pre‐existing conditions and 1 (0.4%) had a severe complication. Nine patients presented clinical symptoms of cocaine poisoning (Table 1) confirmed by positive urine test: malaise with prodromes (n = 1), chest pain (n = 2), isolated mydriasis (n = 3), agitation associated with a severe headache (n = 1), and cardiac rhythm anomalies such as atrio‐ventricular block 1 and extra ventricular systoles (n = 2). One had an occlusive syndrome associated with cocaine impregnation signs. The severe case was an upper digestive occlusion that was revealed by gastric stasis of the pellets for >5 days. The endoscopy showed a necrotic ulcer of the bulb, complicated by constriction and anemia. There were no deaths in our series. All 9 patients with pre‐existing symptoms had a favorable evolution under symptomatic treatment and monitoring alone.
TABLE 1.
Symptoms that may be associated with cocaine poisoning
| Clinical data | No. |
|---|---|
| Malaise | 1 |
| Chest pain | 2 |
| Mydriasis | 2 |
| Mydriasis and vomiting | 1 |
| Agitation and headache | 1 |
| Disorders of rhythm (AVB1, EVS) | 2 |
| Total | 9 |
AVB, atrio‐ventricular block; EVS, extra ventricular systoles.
3.3. Evolution, management, and hospitalization data
All patients received treatment with oral osmotic laxative (∼ 4 liters of polyethylene glycol per 24 hours), unless patients refused (n = 11, 4.0%) or had already eliminated pellets. Hospitalization allowed the monitoring of patients during the pellet evacuation period. The patients were monitored for 2 types of complications: the risk of rupture, therefore of cocaine intoxication, and the risk of occlusion because of the lack of evacuation. Of the 9 patients presenting with cocaine poisoning symptoms, no treatment was required. However, 10 digestive endoscopies were carried out because of pellet evacuation delays, but there were no complications. The pellets could not be completely removed in 2 cases and were eliminated naturally later after the procedure. No patient required abdominal surgery. Of the 10 patients who underwent endoscopy, only 2 (20%) had digestive symptoms. Endoscopy was performed with an average delay of 8.2 days from entry. Anatomical variants or morphological abnormalities were revealed by endoscopy in 3 patients (exceptional length of the colon, closed left colonic angle, and gastric duodenal ulcer with stenosis). The presence of digestive signs during hospitalization, the ingestion of >10 pellets, and the occurrence of hypoglycemia during hospitalization were significantly associated with a prolonged stay (Table 2). Hypoglycemia was observed for 8.3% of hospitalized patients, usually in a fasting context.
TABLE 2.
Bivariate analysis for stays >4 days
| Hospitalization >4 days (%), n = 36 | Hospitalization ≤4 days (%), n = 246 | OR (95% CI) | P | |
|---|---|---|---|---|
| Male | 29/36 (80.5) | 199/246 (80.8) | 0.97 (0.38–2.8) | 0.90 |
| Fever a | 0/32 | 5/216 (3.96) | 0 (0–5.23) | 0.38 |
| Tachycardia a | 12/36 (33.3) | 80/241 (33.1) | 1.00 (0.43–2.22) | 0.98 |
| High blood pressurea | 15/36 (41.6) | 135/240 (56.3) | 0.55 (0.25–1.19) | 0.10 |
| Digestive signs | 11/34 (32.3) | 22/215 (10.2) | 4.19 (1.61–10.4) | <0.01 |
| No. pellets ≥10 | 34/36 (94.4) | 162/232 (69.8) | 7.34 (1.78–64) | <0.01 |
| Gastric pellets | 11/25 (44) | 54/185 (29.2) | 1.9 (0.73–4.8) | 0.13 |
| Laxative intake | 35/36 (97.2) | 226/236 (95.7) | 1.5 (0.2–69) | 0.67 |
| Hypoglycemia | 5/24 (20) | 5/96 (5.2) | 4.79 (0.07–22.7) | 0.01 |
95% CI, 95% confidence interval; OR, odds ratio.
aSigns presents during first evaluation.
3.4. Analysis of women
Out of 54 women, including 53 women <55 years old, 5 (9.4%) had ongoing pregnancies and 2 had interrupted pregnancies. Among them, only 2 were aware of the current pregnancy.
4. DISCUSSION
This large case series of body‐packers demonstrates the safety of our clinical practice that includes the use of screening abdominal X‐rays, observation in a non‐intensive care setting with vital signs measured 3 times a day, daily osmotic laxatives, and monitoring for the expelling of drug packets. There was a small rate of endoscopy for those who did not expel their packets after a week of observation.
Among patients brought in for suspected body‐packing, 53% were found to have radiologic evidence of drug pellets. Usually, in the literature, this rate is between 16% and 22%. 6 In our study, this rate was much higher because of limited number of possible arrests per day (2 or 3 persons), which leads to more targeted arrests. Hypertension and tachycardia were common among these patients but most resolved without intervention and were felt to be because of the anxiety surrounding their arrest and not cocaine toxicity. Only 3.5% of these patients developed overt signs of cocaine toxicity, and only 1 patient needed pharmacologic treatment. These patients were mostly male, young, and with a low rate of pre‐existing illness.
There were no deaths and no surgery in this cohort. With 3.5% of patients presenting preoccupying condition or severe form, our study confirms the low risk of complications in body‐packers. 7 , 8 , 9 , 10 , 11 , 12 These results were in favor of a purely medical management of asymptomatic patients. Simple observation is already effective in a number of Anglo‐Saxon countries. 8 , 9 , 10 , 12 , 13 , 14 A hospitalization in a medical ward is coherent implying training of personnel to recognize alert signs and implement appropriate intervention protocols. Urine cocaine screening tests represent an important follow‐up test but were too rarely used in our study. A negative test on admission that becomes positive during hospitalization, or remains positive for >4 days, is suggestive of permeable pellets. 7
For patients with warning signs, initial close medical surveillance also seems warranted thus limiting the indications for immediate surgery. Contrary to what is usually found in the literature, endoscopy was preferred to surgery as a first choice among stable patients 15 , 16 ; it could be used for stable patients with type 2 pellets. Endoscopy can be particularly useful for esophageal or gastric pellets avoiding thoracotomy or laparotomy depending on the level of obstruction. 14 A significant number of patients with long expulsion times had anatomical variations that could be identified by endoscopy.
Factors associated with prolonged hospitalization were consistent with clinical practice. Presence of digestive signs required a longer surveillance. Similarly, the presence of a large number of pellets required more time for resolution. The patients were fasting during the entire period of hospitalization, which explains the hypoglycemia. There are no clear guidelines regarding the indication for fasting in asymptomatic patients. Some allow liquid feeding or light feeding in the absence of obstructive signs. 12 Here, we recommended an infusion of 10% serum glucose or the introduction of a light liquid diet after 48 hours. If digestive signs were present, fasting was prolonged. As others have observed, there were no complications after systemic use of osmotic laxatives. 17
CT scan represents the gold standard. 18 , 19 , 20 It has been shown that 10% of patients have residual pellets despite 2 pellet‐free evacuations and a “normal” X‐ray with a negative predictive value ranged between 28.6% and 35.7%. 21 This study highlights the need to follow international recommendations in the management of body‐packers in FG. Although most of the patients in this retrospective cohort did not benefit from this, patients now benefit from a systematic exit CT.
Because of the retrospective nature of the study, the completeness of the history, clinical presentation, and management was variable. Until this study, there was no real protocol to homogenize practices but rather management habits. We had to define the definitions and criteria of severity (eg, signs of poisoning) a posteriori. Nevertheless, to limit bias, objective criteria were used, such as clinical and biological associations (clinical signs compatible with poisoning and positive urine test for cocaine).
5. CONCLUSION
The number of body‐packers in Guiana has increased significantly over the past decade. Because of the good quality of pellet preparation, body‐packing has resulted in very few complications and no deaths in this cohort. Given this observation, a CT scan at discharge became more prevalent. Endoscopy has emerged as an alternative to surgery for patients with significant ongoing symptoms or ileus.
AUTHOR CONTRIBUTIONS
CB, TB, and KH conceived the study and designed the trial. CB, AP, DJ, DL, and VA supervised the conduct of the trial and data collection. CB, MN, and TB provided statistical advice on study design and analyzed the data. CB drafted the manuscript, and all authors contributed substantially to its revision. CB takes responsibility for the paper as a whole.
CONFLICT OF INTEREST
The authors declare no competing interests.
ACKNOWLEDGMENTS
We thanks the customs and forensic medicine service.
Biography
Timothee Bonifay, MD, is a physician in the Department of General Medicine at the University of French West Indies and Guiana in French Guiana, France.

Bonnefoy C, Nacher M, Egmann G, et al. Epidemiology and medical management of body‐packers in French Guiana between 2010 and 2015. JACEP Open. 2022;3:e12603. 10.1002/emp2.12603
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Karl Sporer, MD.
Contributor Information
Clemence Bonnefoy, Email: clem.bonnefoy@gmail.com.
Timothee Bonifay, Email: timothee.bonifay@gmail.com.
REFERENCES
- 1. Pousset M. Cocaines, données essentielles . Observatoire Français des Drogues et des Toxicomanies ‐ OFDT; 2012:232.
- 2. Booker RJ, Smith JE, Rodger MP. Packers, pushers and stuffers–managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J. 2009;26(5):316‐320. [DOI] [PubMed] [Google Scholar]
- 3. Cocaïne et crack: fiche drogue | www.emcdda.europa.eu [Internet] . [cité 5 févr 2021]. Disponible sur: https://www.emcdda.europa.eu/publications/drug‐profiles/cocaine_fr
- 4. McCarron MM, Wood JD. The cocaine ‘body packer’ syndrome: diagnosis and treatment. JAMA. 1983;250(11):1417‐1420. [PubMed] [Google Scholar]
- 5. Zimmerman JL. Cocaine intoxication. Crit Care Clin. 2012;28(4):517‐526. [DOI] [PubMed] [Google Scholar]
- 6. Asha SE, Higham M, Child P. Sensitivity and specificity of CT scanning for determining the number of internally concealed packages in ‘body‐packers’. Emerg Med J. 2015;32(5):387‐391. [DOI] [PubMed] [Google Scholar]
- 7. de Prost N, Lefebvre A, Questel F, et al. Prognosis of cocaine body‐packers. Intensive Care Med. 2005;31(7):955‐958. [DOI] [PubMed] [Google Scholar]
- 8. Mandava N, Chang RS, Wang JH, et al. Establishment of a definitive protocol for the diagnosis and management of body packers (drug mules). Emerg Med J. 2011;28(2):98‐101. [DOI] [PubMed] [Google Scholar]
- 9. Dorn T, Ceelen M, de Keijzer KJC, et al. Prevalence and medical risks of body packing in the Amsterdam area. J Forensic Leg Med. 2013;20(2):86‐90. [DOI] [PubMed] [Google Scholar]
- 10. Bulstrode N, Banks F, Shrotria S. The outcome of drug smuggling by ‘body packers’–the British experience. Ann R Coll Surg Engl. 2002;84(1):35. [PMC free article] [PubMed] [Google Scholar]
- 11. Pidoto RR, Agliata AM, Bertolini R, Mainini A, Rossi G, Giani G. A new method of packaging cocaine for international traffic and implications for the management of cocaine body packers. J Emerg Med. 2002;23(2):149‐153. [DOI] [PubMed] [Google Scholar]
- 12. Beckley I, Mohsen Y. Clinical management of cocaine body packers: the Hillingdon experience. Can J Surg. 2009;52(5):417. [PMC free article] [PubMed] [Google Scholar]
- 13. Glovinski PV, Lauritsen ML, Bay‐Nielsen M, Brandstrup B, Bisgaard T. Asymptomatic body packers should be treated conservatively. Dan Med J [Internet]. 2013;60(11):A4723. https://www.researchgate.net/profile/Birgitte_Brandstrup/publication/258313757_Asymptomatic_body_packers_should_be_treated_conservatively/links/559e94bc08aea946c06a348a.pdf. [cité 4 avr 2016]. Disponible sur. [PubMed] [Google Scholar]
- 14. de Bakker JK, Nanayakkara PWB, Geeraedts LMG, de Lange ESM, Mackintosh MO, Bonjer HJ. Body packers: a plea for conservative treatment. Langenbecks Arch Surg. 2012;397(1):125‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Macedo G, Ribeiro T. Esophageal obstruction and endoscopic removal of a cocaine packet. Am J Gastroenterol. 2001;96(5):1656‐1657. [DOI] [PubMed] [Google Scholar]
- 16. Covarelli P, Burini G, Castellani E, et al. Surgical treatment in drug body packers. Am Surg. 2014;80(3):76‐78. [PubMed] [Google Scholar]
- 17. Farmer JW, Chan SB. Whole body irrigation for contraband bodypackers. J Clin Gastroenterol. 2003;37(2):147‐150. [DOI] [PubMed] [Google Scholar]
- 18. Sica G, Guida F, Bocchini G, Iaselli F, Iadevito I, Scaglione M. Imaging of drug smuggling by body packing. Semin Ultrasound CT MR. 2015;36(1):39‐47. [DOI] [PubMed] [Google Scholar]
- 19. Flach PM, Ross SG, Ampanozi G, et al. “Drug mules” as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol. 2012;81(10):2518‐2526. [DOI] [PubMed] [Google Scholar]
- 20. Bulakci M, Kalelioglu T, Bulakci BB, Kiris A. Comparison of diagnostic value of multidetector computed tomography and X‐ray in the detection of body packing. Eur J Radiol. 2013;82(8):1248‐1254. [DOI] [PubMed] [Google Scholar]
- 21. Rousset P, Chaillot P‐F, Audureau E, et al. Detection of residual packets in cocaine body packers: low accuracy of abdominal radiography—a prospective study. Eur Radiol. 2013;23(8):2146‐2155. [DOI] [PubMed] [Google Scholar]