Abstract
The liver plays an important role in glucose and lipid homeostasis, drug metabolism, and bile synthesis. Metabolic disorder and inflammation synergistically contribute to the pathogenesis of numerous liver diseases, such as metabolic-associated fatty liver disease (MAFLD), liver injury, and liver cancer. Celastrol, a triterpene derived from Tripterygium wilfordii Hook.f., has been extensively studied in metabolic and inflammatory diseases during the last several decades. Here we comprehensively review the pharmacological activities and the underlying mechanisms of celastrol in the prevention and treatment of liver diseases including MAFLD, liver injury, and liver cancer. In addition, we also discuss the importance of novel methodologies and perspectives for the drug development of celastrol. Although celastrol has been claimed as a promising agent against several metabolic diseases, both preclinical and clinical studies are highly required to accelerate the clinical transformation of celastrol in treating different liver illness. It is foreseeable that celastrol-derived therapeutics is evolving in the field of liver ailments.
Keywords: celastrol, liver diseases, liver injury, liver cancer, MAFLD
Introduction
The liver is a metabolic organ that is responsible for glucose and lipid homeostasis, drug metabolism, and bile synthesis (Diehl-Jones and Askin, 2002; Almazroo et al., 2017; Tappy, 2021). Liver diseases contain non-alcoholic fatty liver disease (NAFLD) and its related diseases, drugs or infections induced liver injury, liver cancer, and among others. With the aging of the population and the prevalence of obesity, NAFLD, known as metabolic-associated fatty liver disease (MAFLD), is becoming a threat to human health in the world, (Eslam et al., 2020). MAFLD begins with the accumulation of hepatic lipid, metabolic syndrome (central adiposity, hyperglycemia, dyslipidemia, and hypertension) (Mundi et al., 2020). Environment factors like dietary habits and the genetic factors such as PNPLA3 (encoding patatin-like phospholipase domain-containing protein3), TM6SF2 (encoding transmembrane 6 superfamily member 2), and epigenetic factors are the risk factors of MAFLD (Younossi et al., 2018). The current global prevalence of MAFLD is approximately 25%, which may develop into non-alcoholic steatohepatitis, eventually leading to liver fibrosis, cirrhosis, and even liver cancer if not treated in a timely fashion (Ye et al., 2020). Except for the liver damage, MAFLD and non-alcoholic steatohepatitis can also aggravate or induce insulin resistance, which are closely related to the high incidence of type 2 diabetes and cardiovascular disease (Liang et al., 2022). Liver injury as a loss of liver function is mainly caused by drug, infections, and intrahepatic cholestasis (Thawley, 2017). The drug-induced liver injury (DILI) is one of the most common and serious adverse drug reactions, which can lead to acute liver failure and even death in severe cases (Licata, 2016). With 831,000 death cases and 905,000 new cases in 2020, liver cancer with high mortality and incidence remains a global menace (Sung et al., 2021). Although many patients are diagnosed and treated at an early stage of the disease, the recurrence rate is still high. For middle and late-stage hepatic carcinoma, the prognosis is even less optimistic. Therefore, new therapy or drugs with better efficacy and lower toxicity are of great importance.
Traditional Chinese Medicine (TCM) was used to treat various diseases such as metabolic diseases, liver diseases, inflammation, and cancers for many years. In light of their numerous pharmacological activities, low toxicity, and low side effects, nature compounds from TCM are widely used to protect against liver diseases, such as berberine, curcumin, ginsenoside, celastrol, to name a few (Xu et al., 2018a). In Europe and America, up to 65% of patients choose herbal medicines to treat liver diseases (Zhang et al., 2013; Madrigal-Santillán et al., 2014; Bagherniya et al., 2018). Celastrol, a pharmacologically active compound from Tripterygium wilfordii Hook.f., possesses therapeutic properties for multiple diseases, such as rheumatoid arthritis, inflammatory bowel diseases, hepatitis, as well as anti-cancer, anti-obesity, and metabolic modulating (Feng et al., 2013; Lin et al., 2015; Liu et al., 2015; Tseng et al., 2017; Saito et al., 2019; Song et al., 2019). In recent years, celastrol has attracted the attention of researchers and the pharmaceutical industry due to its benefits on human health. Here, we summarized the studies exploring the pharmacological properties of celastrol in liver protection during 15 years from 2007 to 2021, and made a general statement about its mechanisms in liver-related diseases.
Study Design
The PubMed and Web of Science databases were used to search related articles from 2007 to 2021. Cellular, animal, or human studies were searched with the keywords (celastrol) and (liver). Papers were extracted using the following inclusion criteria: (1) these studies should be research articles to estimate the hepatoprotective effects of celastrol; (2) only articles written in English were included. All titles and abstracts of publications retrieved were reviewed to select potentially eligible studies. Full texts of literatures potentially eligible were reviewed by two independent investigators. From a total of 181 results, 76 unique studies were identified, 88 duplication, 5 reviews, and 12 other article styles were excluded. After carefully reviewing the title and/or abstract, 18 were excluded 5 publications are irrelevant. A total of 53 articles were included in this review. A flowchart of this is illustrated in Figure 1.
FIGURE 1.
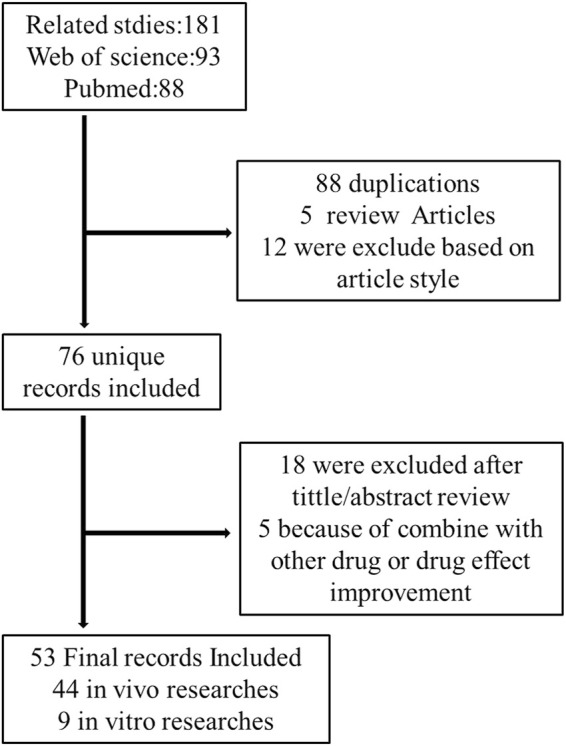
Flow chart of the study design.
Celastrol and Liver Diseases
Celastrol and MAFLD
MAFLD, characterized by the hepatic fat accumulation, is usually correlated with the metabolic disorder related obesity (Samuel and Shulman, 2018; Jarvis et al., 2020), hepatic inflammation (Kazankov et al., 2019), oxidative stress (Ore and Akinloye, 2019; Świderska et al., 2019), and intestinal microbiome dysbiosis (Caussy and Loomba, 2018). Lipotoxicity induced by abnormal hepatic fat deposition activated Kuepfer cell (KC) to promote inflammation in MAFLD patients (Lanthier, 2015). Oxidative stress and endoplasmic reticulum (ER) stress resulted in mitochondrial reactive oxygen species (ROS) accumulation in hepatocytes, which in turn impaired glycolipid metabolism, accelerated inflammatory response, and introduced cell death in MAFLD (Ore and Akinloye, 2019; Świderska et al., 2019; Chen et al., 2020a). The reasonable management of body weight and dietary habits should be given a high priority in MAFLD patients. Although the antidiabetic and lipid-lowering drugs may help to reduce hepatic lipid accumulation (Mundi et al., 2020), there are no specific drugs for MAFLD approved in Europe and the United States. Recent research mainly focused on the metabolic targets, immune targets, fibrosis, cell stress, and apoptosis (Friedman et al., 2018). Celastrol as a promising compound exhibits good anti-obesity and anti-inflammatory effect on treating MAFLD.
Anti-Obesity Effects
The liver is vital for lipid and glucose metabolism and homeostasis, protein, and amino acid metabolism, where bile acids produce and flux to the digestive system. Numerous evidences supported that obesity is strongly associated with MAFLD development (Fabbrini et al., 2010). The liver protective effect and molecular mechanism of celastrol on high fat diet (HFD) induced MAFLD animal models have been well-investigated (Wang et al., 2014; Ma et al., 2015; Zhang et al., 2017a; Hu et al., 2017; Luo et al., 2017; Kyriakou et al., 2018; Pfuhlmann et al., 2018; Zhang et al., 2018; Feng et al., 2019a; Zhao et al., 2019a; Feng et al., 2019b; Chellappa et al., 2019; Fang et al., 2019; Abu Bakar et al., 2020; Hu et al., 2020; Zhu C. et al., 2021; Zhu Y. et al., 2021; Hua et al., 2021; Ouyang et al., 2021; Yang et al., 2021).
As a typical feature of obesity, leptin resistance was involved in the hepatic steatosis during the development of MAFLD (Myers et al., 2010; Boutari and Mantzoros, 2020). Leptin, a hormone secreted by adipose tissue, directly interacted with the leptin receptor in the brain and mediated food intake, energy metabolism, body weight, and other physiological processes (Xu et al., 2018b; Caron et al., 2018; Pan and Myers, 2018). Brain leptin promoted hepatic lipid flux and reduced lipogenesis in the liver (Hackl et al., 2019). Celastrol as a leptin sensitizer exhibited significant weight loss and food consumption reduction in HFD-obesity animals (Wang et al., 2014; Liu et al., 2015; Ma et al., 2015; Zhang et al., 2017a; Hu et al., 2017; Luo et al., 2017; Kyriakou et al., 2018; Pfuhlmann et al., 2018; Zhang et al., 2018; Feng et al., 2019a; Zhao et al., 2019a; Feng et al., 2019b; Chellappa et al., 2019; Fang et al., 2019; Saito et al., 2019; Abu Bakar et al., 2020; Hu et al., 2020; Zhu C. et al., 2021; Zhu Y. et al., 2021; Hua et al., 2021; Ouyang et al., 2021; Yang et al., 2021) (Table 1).
TABLE 1.
The summary of preclinical studies of celastrol in HFD induced MAFLD models.
| Experimental model used | Model inducer | Dosage and drug-delivery way | Drug treatment period | Phenotype and mechanism | Reference |
|---|---|---|---|---|---|
| Wild type animal models | |||||
| Male Sprague–Dawley rats | HFD | 1 mg/kg/day, 3 mg/kg/day, and 9 mg/kg/day by oral administration | 6 weeks | Promoted weight loss and lipid metabolism, attenuated oxidative injury through improving ABCA1 and antioxidant enzymes activities, reducing NADPH oxidase activity | Wang et al. (2014) |
| HFD for 11 weeks | 500 μg/kg/day by oral administration | 3 weeks | Decreased body weight and lipid accumulation in liver, promoted energy expenditure by increasing ratio of Bacteroidetes to Firmicutes rather than food intake, leptin signaling pathway, gut microbiota homeostasis | Hu et al. (2020) | |
| HFD for 17 weeks | 1 mg/kg/day, 3 mg/kg/day mixed with drinking water | 8 weeks | Reduced body weight, alleviated inflammatory response in adipose tissue and enhanced mitochondrial functions in skeletal muscle by upregulation of AMPK/SIRT1 signaling pathways | Abu Bakar et al. (2020) | |
| Male C57BL/6J mice | HFD for16-20 weeks | 100 μg/kg/day by i.p injection, or 10 mg/kg/day by oral administration | 3 weeks | Improved weight loss and glucose homeostasis by reducing food consumption and ER stress in hypothalamus | Liu et al. (2015) |
| NCD or HFD for 9 weeks | 100 μg/kg/day or 500 μg/kg/day by i.p injection | 24 days | Reduced body weight and fat mass by decreased food intake, improved metabolism by increased homeostatic regulation of energy balance related gene expressions in the hypothalamus | Saito et al. (2019) | |
| HFD for 8 weeks | 1 mg/kg/day, 3 mg/kg/day mixed with food | 3 weeks | Enhanced energy expenditure, and mitochondrial function in fat and muscle by activated HSF1-PGC1α axis | Ma et al. (2015) | |
| HFD for 14 weeks | 200 μg/kg/every 2 days by i.p injection | 4 weeks | Inhibited lipid synthesis by downregulation of Srebp-1c expression, reduced oxidative stress and inflammation by enhanced the phosphorylation of hepatic AMPKα and Sirt1 | Zhang et al. (2017a) | |
| HFD for 12 weeks | 100 μg/kg/day by i.p injection | 2 weeks | Suppressed hepatic inflammation and immune cell accumulation by reducing expression and production of IL-1β and IL-6 | Hu et al. (2017) | |
| HFD for 16 weeks | 100 μg/kg/day by i.p injection | 8 weeks | Attenuated inflammation and insulin resistance by inhibition of TLR4/NF-κB | Zhang et al. (2018) | |
| HFD for 32 weeks | 100 μg/kg/day by i.p injection | 6 days | Promoted weight loss through hypoplasia and activation of leptin-STAT3 signaling in elder mice | Pfuhlmann et al. (2018) | |
| HFD for 8–12 weeks | 100 μg/kg/day by i.p injection | 10 days | Lowered body weight by inhibition of PTP1B and TCPTP in hypothalamus | Kyriakou et al. (2018) | |
| HFD for16-20 weeks | 100 μg/kg/day by i.p injection | 4 days | Celastrol’s anti-obesity effects was not dependent on LCN2 | Feng et al. (2019a) | |
| HFD for 16 weeks | 0.1 mg/kg/day by i.p injection | 21 days | Suppressed gluconeogesis by activating CREB/PGC-1α pathway | Fang et al. (2019) | |
| HFD for 12 weeks | 150 μg/kg, 300 μg/kg by i.p injection | 3 weeks | Reduced weight gain without affecting food intake, ameliorated metabolic disorder and hepatic inflammation by inhibition of TLR3/NLRP3 inflammasome | Yang et al. (2021) | |
| HFD for 6 weeks | 3 mg/kg/day was mixed with food | 24 days | Prevented intestinal lipid absorption by downregulation of CD36, FATP2, FATP4 | Hua et al. (2021) | |
| HFD for 12 weeks | 50 μg/kg/day, 100 μg/kg/day, 200 μg/kg/day by i.p injection | 12 weeks | Attenuated inflammation through the suppression of MMP-2 and MMP-9 | Ouyang et al. (2021) | |
| HFD for 16 weeks | 0.75 mg/kg/day,1.5 mg/kg/day,3 mg/kg/day by oral administration | 25 days | Reduced body weight gain, insulin resistance, hepatic steatosis, and inflammation by inhibition of CAP1‒resistin interaction, PKA‒NF-kB pathway | Zhu Y. et al. (2021) | |
| Male C57BL/6 N mice | HFD for 12 weeks | 5 mg/kg/day and 7.5 mg/kg/day mixed with food | 3 weeks | Prevented M1 macrophage polarization, inflammation, and insulin resistance via regulating Nrf2/HO‐1, MAPK signal, and NF-κB pathway | Luo et al. (2017) |
| HFD for12 weeks | 5 mg/kg/day or 7.5 mg/kg/day by oral administration | 3 weeks | Reduced body weight and fat mass inhibited inflammatory response by downregulation of expression of macrophage M1 biomarkers (e.g., IL-6, IL-1β, TNF-α, iNOS) and enhanced expression of macrophage M2 biomarkers (e.g., Arg-1, IL-10) | Zhao et al. (2019a) | |
| Genetic deficency animal models | |||||
| Lepdb mice | NCD | 100 μg/kg/day by i.p. injection, or 10 mg/kg/day by oral administration | 3 weeks | No significant change of body weight | Liu et al. (2015) |
| 100 μg/kg/day by subcutaneous injection | 6 days | Pfuhlmann et al. (2018) | |||
| 100 μg/kg by i.p. injection | 3 weeks | Feng et al. (2019b) | |||
| 100 μg/kg by i.p. injection | 4 days | Feng et al. (2019a) | |||
| 0.1 mg/kg/day by i.p. injection for 10 days, then 0.5 mg/kg by i.p.injection for 15 days | 25 days | Body weight slightly reduced | (Saito et al., 2019)] | ||
| Lep−/+ rats and Lep−/− rats | HFD for 17 weeks | 0.5 mg/kg/day or 1 mg/kg/day by oral administration | 3 weeks | 1,000 μg/kg celastrol decreased the BW of Lep−/+ rats not Lep−/− rats | Hu et al. (2020) |
| Lepob mice | NCD for 6 or 14 weeks | 100 μg/kg/day by subcutaneous injection | 6 days | Promoted weight loss in young Lepob mice not old Lepob mice | Liu et al. (2015) |
| HSF1 −/− Mice | HFD for 4 weeks | 3 mg/kg/day mixed with powdered chow | 4 weeks | Had no effects on body weight and energy consumption | Ma et al. (2015) |
| Liver specific Sirt1 KO mice | HFD for 14 weeks | 200 μg/kg/every 2 days by i.p.injection | 4 weeks | Reduced food intake and increased the hepatic lipid accumulation by inhibited phosphorylation of AMPKα and hepatic LKB1 expression | Zhang et al. (2017a) |
| Nur77 −/−mice | HFD for 17 weeks | 0.1 mg/kg/day by i.p injection | 2 weeks | Mild reduced the body weight and anti-inflammation effects attenuated | Hu et al. (2017) |
| Global PTP1B KO mice | NCD or HFD for 10 weeks | 0.1 mg/kg/day by i.p injection | 7 days | Induced weight loss both in NCD and HFD PTP1B mice, reduction of fat and lean mass is owing to weight loss of HFD PTP1B mice not for NCD mice | Pfuhlmann et al. (2018) |
| UCP1 KO mice | HFD for 20 weeks | 100 μg/kg/day by subcutaneous injection | 6 days | Decreased body weight and food intake by fat mass loss | Pfuhlmann et al. (2018) |
| IL1R1−/− mice | HFD for 20 weeks | 100 μg/kg/day by i.p. injection | 3 weeks | No change of body weight, fat mass, and food intake | Zhao et al. (2019a) |
| Lcn2−/− mice | NCD or HFD for 16-20 weeks | 100 μg/kg/day by i.p. injection | 3 weeks | Reduced body weight and fat mass without affected food intake in NCD Lcn2−/− mice, inhibited hepatosteatosis, and metabolic disorder induce by HFD in Lcn2−/− mice | Feng et al. (2019a) |
| ApoE−/- mice | NCD or HFD for 12 weeks | 100 μg/kg/day by oral administration | 12 weeks | Alleviated inflammatory reaction in apoE−/- mice fed with HFD | Zhu Y. et al. (2021) |
| Melanocortin 4 receptor (MC4R)-null mice | NCD | 0.1 mg/kg/day by i.p injection for 10 days, then 0.5 mg/kg/day by i.p injection for 15 days | 25 days | Reduced body weight, food intake, fat and lean mass, enhanced energy expenditure by upregulation of adrenergic receptor and PRDM16 without affecting UCP-1 and PGC-1α | Saito et al. (2019) |
| HnRNPA1 deficency/overexpression mice | NCD | 2 mg/kg/day by gavage administration | 12 days | Inhibited energy expenditure and abrogated weight loss effects in HnRNPA1 overexpression mice | Zhu C. et al. (2021) |
| Other model | |||||
| Young (4–6 month) and Old (18–22 month) male mice | NCD | 100–200 μg/kg/day by i.p. injection | 4–6 days | Promoted weight and lean mass loss by lowering food intake in aged mice, but not in young controls | Chellappa et al. (2019) |
HFE, high fat emulsion; NCD, normal chow diet; HFD, high fat diet; ABCA1, ATP-binding cassette transporter A1; NADPH, nicotinamide adenine dinucleotide phosphate; AMPK, Adenosine 5‘-monophosphate (AMP)-activated protein kinase; SIRT1, sirtuin1; ER, endoplasmic reticulum; HSF1, heat shock factor 1; PGC-1α, Peroxisome proliferator-activated receptor γ coactivator 1α; Srebp-1c, sterol regulatory element binding protein-1c; IL-1β, interleukin-1β; IL-6, interleukin-6; TLR4, Toll-like receptor 4; NF-κB, nuclear factor kappa-B; STAT3, signal transducer and activator of transcription 3; LCN2, lipocalin-2; PTP1B, protein tyrosine phosphatase (PTP) 1B; TCPTP,T-cell PTP; TLR3, Toll-like receptor 3; NLRP3, NOD-like receptor protein 3; CD36, cluster of differentiation 36; FATP2, very-long-chain acyl-CoA, synthetase; FATP4, fatty acid transport protein 4; MMP-2, Matrix metalloproteinase-2; MMP-9, Matrix metalloproteinase-9; CAP1, adenylate cyclase-associated protein 1; PKA, Protein kinase A; NF-kB, nuclear factor kappa B; Nrf2, nuclear respiratory factor 1; HO-1, Heme oxygenase 1; MAPK, mitogen-activated protein kinase; TNF-α, tumor necrosis factor α, iNOS, inducible nitric oxide synthase; Arg-1, arginase-1; IL-10, interleukin-10; Lep, leptin; BW, body weight; LKB1, liver kinase B1; PTP1B, Protein tyrosine phosphatase 1; ApoE, apolipoproteinE; PRDM16, PR, domain-containing 16; UCP-1, Uncoupling protein 1; HnRNPA1,heterogeneous nuclear ribonucleoprotein A1.
Celastrol (100 μg/kg by intraperitoneally injection [i.p], or 10 mg/kg by oral administration [OA]) increased the leptin sensitivity to suppress food intake and reduce body weight in HFD induced C57BL/6J mice and was firstly reported in 2015 by Ozcan’s group (Liu et al., 2015), while the benefits of celastrol on obesity were abrogated in lean mice, leptin receptor-deficient (db/db), or leptin-deficient (ob/ob) mice/rats (Liu et al., 2015; Pfuhlmann et al., 2018; Feng et al., 2019a; Feng et al., 2019b; Saito et al., 2019; Hu et al., 2020). Compared with leptin or celastrol alone, the combined use of leptin and celastrol could significantly inhibit appetite and weight gain of different mice, even for ob/ob mice (Liu et al., 2015). Numerous studies verified the effect of leptin sensitizer celastrol on appetite as showing in Table 1.
The underlying molecular mechanism of celastrol anti-obesity and increase the leptin sensitivity can be attributed to Sirtuin 1(Sirt1) (Zhang et al., 2017a; Abu Bakar et al., 2020), interleukin-1 receptor 1(IL1R1) (Feng et al., 2019b), protein tyrosine phosphatase (PTP) 1B (PTP1B), and T-cell PTP (TCPTP) (Kyriakou et al., 2018). SIRT1 as a deacetylase activated by energy deprivation was involved in glucose, lipid, and bile acid metabolism regulation (Purushotham et al., 2009; García-Rodríguez et al., 2014). It has been reported that celastrol exacerbated liver metabolic disorder by suppressing the phosphorylation of AMP-activated protein kinase α (AMPKα) in liver specific Sirt1 knock out mice fed with HFD (Zhang et al., 2017a). In line with that, celastrol (3 mg/kg/day for 8 weeks) significantly increased insulin sensitivity and weight loss through enhancing AMPK/SIRT1 signaling in HFD-induced rats (Abu Bakar et al., 2020). IL1R1, a cytokine receptor, was associated with cell death and inflammation. IL1R1 deficient mice showed the phenotype of mature-onset obesity and leptin resistance (García et al., 2006). Feng and his colleagues demonstrated that the protective property of celastrol on obesity reversed by IL1R1 deficiency, which indicated that IL1R1 is essential for celastrol to reduce food consumption and body weight, alleviate glucose intolerance and insulin tolerance, as well as hepatic steatosis in HFD mice (Feng et al., 2019). However, these studies were only performed in genetic deficient animals, and whether the hepatoprotective effects of celastrol depended on its direct interaction with Sirt1 or IL1R1 need further studies. The surface plasmon resonance (SPR) assay, circular dichroism (CD) spectroscopy, and other methods might be effective methods to verify the above hypothesis. PTP1B and TCPTP negatively regulate leptin signaling in the hypothalamus (Dodd et al., 2019). Eleni et al. demonstrated that celastrol-induced weight loss was attributed to the supression of PTP1B and TCPTP, and inhibition of PTP1B and TCPTP is mediated by reversible noncompetitive binding to an allosteric pocket close to the active site (Kyriakou et al., 2018). In addition, different studies demonstrated the anti-obesity effect of celastrol was independent on melanocortin 4 receptor (MC4R), and lipocalin 2 (Lcn2) (Feng et al., 2019a; Saito et al., 2019), because the deletion of these genes did not weaken the weight-loss and liver-protecting effect of celastrol in mice.
Obesity related MAFLD was triggered by energy imbalance, with features of excessive lipid deposition. Peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α), a nuclear transcriptional coactivator factor, increased energy expenditure by regulating mitochondrial function and biogenesis (Vega et al., 2000; Rodgers et al., 2005; Minsky and Roeder, 2015). Liver-specific deficient PGC-1α mice exhibit hepatic steatosis (Rodgers et al., 2005). Accumulating evidences uncovered that celastrol promotes the white adipose tissue (iWAT) browning and brown adipose tissue (BAT) activation by upregulating PGC-1α and uncoupling protein 1(UCP1, a downstream effector of PGC-1α, is responsible for electron transport of mitochondrial oxidative phosphorylation) expression (Table 2). A total of 3 mg/kg/day celastrol (OA) significantly increased the HSF1 (Heat Shock Transcription Factor 1)/PGC-1α axis activity and protected against obesity in HFD mice by increasing energy expenditure, including iWAT browning, BAT activation, and mitochondrial gene transcription, while such benefit was abrogated by HSF1 depletion (Ma et al., 2015). In agreement with this result, several reports also clarified that celastrol increased the energy expenditure by activating iWAT browning through upregulation of PGC-1α and UCP1 (Fang et al., 2019; Yang et al., 2021). However, these studies were challenged by Katrin’s group, and they showed that celastrol intervention only upregulated the UCP1, while the expression of PGC-1α in BAT of HFD mice was not altered, and UCP1 deletion in HFD mice did not abolish food consumption and body weight reduction effects of celastrol (Pfuhlmann et al., 2018). This indicated that weight loss effect of celastrol was not dependent on UCP1-mediated thermogenesis under nutrient stress. In accordance with Katrin’s study, other researchers did not observe that the upregulation of UCP1 and PGC-1α expression in iWAT and BAT of HFD induced mice and rats with celastrol administration (Saito et al., 2019; Hu et al., 2020; Hua et al., 2021). The disparity of above observations of celastrol’s hepatoprotective effects might be caused by different celastrol-delivery way (OA vs. i.p), dosage, and intervention time period (Table 2). All above results indicated that iWAT browning happened at a specific time after celastrol treatment, and celastrol improved energy expenditure through other pathways not only depending on browning of iWAT.
TABLE 2.
The regulation of celastrol on iWAT browning and BAT thermogenesis gene.
| Animal model | Model inducer | Dosage | Intervention time | Gene | Reference | |
|---|---|---|---|---|---|---|
| UCP-1 | PGC-1α | |||||
| Male Sprague–Dawley rats | HFD for 11 weeks | 0.5 mg/kg/day by oral administration | 3 weeks | no change | no change | Hu et al. (2020) |
| C57BL/6J | NCD or HFD for 9 weeks | 0.1 mg/kg/day or 0.5 mg/kg/day by i.p injection | 24 days | no change | no change | Saito et al. (2019) |
| HFD for 6 weeks | 3 mg/kg/day celastrol was mixed with food | 24 days | no change | no change | Hua et al. (2021) | |
| HFD for 8 weeks | 1 mg/kg/day, 3 mg/kg/day mixed with food | 3 weeks | upregulated | upregulated | Ma et al. (2015) | |
| HFD for 12 weeks | 0.1 mg/kg/day,0.3 mg/kg/day by i.p injection | 3 weeks | upregulated | upregulated | Yang et al. (2021) | |
| HFD for 16 weeks | 0.1 mg/kg/day by i.p injection | 21 days | upregulated | upregulated | Fang et al. (2019) | |
| HFD for 32 weeks | 0.1 mg/kg/day by i.p injection | 6 days | upregulated | no change | Pfuhlmann et al. (2018) | |
| MC4R-null mice | NCD | 0.1 mg/kg/d by i.p injection for 10 days, then 0.5 mg/kg/d by i.p injection for 15 days | 25 days | no change | no change | Saito et al. (2019) |
| HSF1 −/− mice | NCD for 8 weeks | 3 mg/kg/day mixed with food | 4 weeks | no change | no change | Ma et al. (2015) |
iWAT, inguinal white adipose tissue; BAT, brown adipose tissue; SD, Sprague–Dawley; UCP-1, Uncoupling protein 1; PGC-1α, Peroxisome proliferator-activated receptor γ coactivator 1α; MC4R, melanocortin 4 receptor; HSF1, heat shock factor 1; NCD, normal chow diet; HFD, high fat diet.
Numerous studies proved that gut microbiota dysbiosis can also be attributed to fatty liver disease development (Le Roy et al., 2013; Canfora et al., 2019; Frazier and Chang, 2020). Oral administration of 500 μg/kg/day celastrol markedly enhanced energy expenditure and enhanced liver lipid metabolism in HFD rats by improving the gut microbiota homeostasis and activating the hypothalamic leptin signaling pathway rather than affecting food intake (Hu et al., 2020). Firmicutes promoted lipid absorption not fatty acid oxidation (Murphy et al., 2013). Increased ratio of Bacteroidetes to Firmicutes played a critical role in improvement of lipid consumption in celastrol-treated HFD rats (Murphy et al., 2013). Consistent with this, oral administration of celastrol (3 mg/kg/d) inhibited intestinal lipid absorption to ameliorate metabolic disturbance by reconstructing the gut microbiota profile in HFD mice (Hua et al., 2021). Although it has been reported that celastrol improved lipid metabolism by modulating gut microbiota, its specific mechanism of gut microbiota involved in MAFLD still needs to be explored. In addition, recent study demonstrated that age-associated obesity mice injected with celastrol (100–200 μg/kg) exhibited reduction body weight and fasting glucose level owing to fat loss and circadian rhythms restored without impact on lean mass (Chellappa et al., 2019), and whether gut microbiota act as an actuator of host circadian rhythms involved in the procedure remains to be studied (Frazier and Chang, 2020; Saran et al., 2020).
In summary, celastrol reduced body weight and hepatic fat accumulation mainly by increasing leptin sensitivity, enhancing energy metabolism, and modulating gut microbiota. Above all, Sirt1, IL1R1, PTP1B, and TCPTP might be the potential targets of celastrol, but whether celastrol directly interacted with these targets should be deeply explored. Moreover, the effect of celastrol on PGC-1α and UCP1 is controversial, and further studies should be performed to verify this effect. Gut microbiota have been extensively studied in recent years, but the molecular mechanism of celastrol on anti-obesity through gut microbiota is still unclear.
Anti-Inflammatory Response Activity
Macrophage infiltration and inflammation caused by dyslipidemia is associated with progression of MAFLD (Kazankov et al., 2019; Katsiki et al., 2016; Luo et al., 2018). Different animal experiments have elucidated that the inflammation in fatty liver mice treated with celastrol are remarkably attenuated (Table 1). Macrophage infiltration and inflammatory factors (IL-1β, IL-18, MCP-1α, and TNF-α) were reduced in liver of HFD induced C57BL/6J or C57BL/6N mice by celastrol treated for 3 weeks (Hu et al., 2017; Luo et al., 2017; Zhang et al., 2018; Ouyang et al., 2021; Zhu Y. et al., 2021). In addition, adipose tissue inflammation and mitochondrial dysfunction in skeletal muscle ameliorated in HFD-induced SD rats treated with 3 mg/kg/day celastrol for 8 weeks (Abu Bakar et al., 2020). The mechanism exhibited that celastrol can activate AMPK/SIRT1 signaling pathways for mitochondrial function improvement and attenuate inflammatory responses via decreasing nuclear factor kappa-B (NF-κB) activity (Abu Bakar et al., 2020). Celastrol-mediated hepatoprotective effects in C57BL/6J mice fed with HFD abolished in liver specific Sirt1-deficient mice fed HFD (Zhang et al., 2017a). Celastrol directly interacted with adenylyl cyclase associated protein 1 (CAP1) in macrophages contributed to improvement of metabolism and attenuation of inflammatory response through NF-κB signaling pathway in HFD-induced mice (Zhu Y. et al., 2021). Apart from that, LPS induced acute liver inflammation and HFD induced chronic inflammation are both inhibited by celatrol through binding Nur77 and promoting Nur77 interact with TRAF2 inducing autophagy (Hu et al., 2017). Deletion of Nur77 or Sirt1 impaired the anti-inflammation ability of celastrol, but LCN2 or ApoE deficiency did not influence the anti-hepatosteatosis of celastrol (Hu et al., 2017; Zhang et al., 2017a; Feng et al., 2019b; Ouyang et al., 2021). In general, the protective effects of celastrol against inflammation might be attributed to suppression of NF-κB involved signaling pathway.
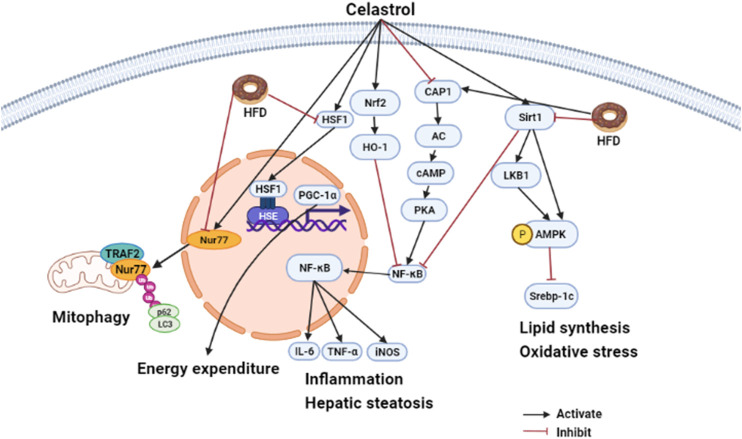
In summary, different animal experiments confirmed that celastrol had metabolic improvement effect on HFD induced SD rats/mice or aged-obesity mice, but has no effect on gene deficiency mice such as HSF1 deletion mice, IL1R1 null mice, Sirt1 deficient mice, etc. (Ma et al., 2015; Zhang et al., 2017a; Feng et al., 2019b). This indicated that HSF1, IL1R1, and Sirt1 might act as the target of celastrol. In addition, oral administration of celastrol hardly affects food intake but has the same benefit on metabolic compared to intraperitoneal injection. Therefore, it is better to use oral administration to explore the pharmacological mechanism of celastrol. The effects of celastrol on MAFLD are summarized in Figure 2.
FIGURE 2.
Hepatoprotective effects of celastrol in HFD induced animal model (edited by Biorender software). Diagram of the mechanism of celastrol in regulating hepatic energy expenditure, inflammation, and lipid metabolism. Under HFD stress, celastrol attenuated inflammation by inducing Nur77 interaction with TRAF2 to promote mitochondrial autophagy. Macrophages mediated inflammation was also ameliorated by celastrol targeted CAP1 via inhibition of cAMP-PKA-NF-κB signaling pathway, and macrophage M1 polarization was suppressed by celastrol via regulating Nrf2-HO-1-NF-κB pathways. In addition, celastrol can also regulate metabolism disorder. On the one hand, it can promote energy metabolism by activating HSF1-PGC1α; on the other hand, it can target SIRT1 to promote AMPK α phosphorylation and inhibit Srebp-1c-mediated lipid synthesis against oxidative stress and inflammation TRAF2, TNFR-associated factor2; CAP1, adenylyl cyclase-associated; protein 1 cAMP, cyclic adenylate monophosphate; PKA, protein kinase A; NF-κB, nuclear factor kappa-B; Srebp-1c, sterol regulatory element binding protein 1c; AMPKα, AMP-activated protein kinase α.
Celastrol and Liver Injury
Liver injury characterized by a loss of hepatocyte function in patients resulted from mitochondrial oxidative stress, endoplasmic reticulum stress, inflammation, and autophagy in hepatocyte (Vento and Cainelli, 2020). Drugs, infections, and intrahepatic cholestasis can all lead to liver injury (Fontana et al., 2014). Celastrol, an anti-inflammatory drug, ameliorated the damage in hepatocyte or liver injury (Abdelaziz et al., 2017; El-Tanbouly et al., 2017; Jannuzzi et al., 2018; Wu et al., 2018; Zhao et al., 2019b; Guo et al., 2019; Wang et al., 2020; Zhao et al., 2020; Yan et al., 2021) (Table 3).
TABLE 3.
Pharmacological activities of celastrol in the treatment of liver injury.
| Model style | Cell/animal | Inducer | Dosage of celastrol | Treatment time | Phenotype/mechanism | Reference |
|---|---|---|---|---|---|---|
| Chemicals induced liver injury | HepG2 cells | APAP | 50, 100, and 200 nM | 24 h | Ameliorated oxidative stress and cytotoxicity caused by APAP | Jannuzzi et al. (2018) |
| Chemicals induced liver injury | Male BALB/c mice | APAP | 2 mg/kg by i.p injection | 2 h prior APAP-induction | Prevented oxidative stress and inflammation by attenuating inflammatory cells accumulation and reducing inflammation factors | Abdelaziz et al. (2017) |
| Chemicals induced liver injury | Male WT mice and Ppara−/− mice on the 129/Sv genetic background | CCl4 | 10 mg/kg by oral treatment | 5 days | Inhibited inflammatory cytokine and oxidative stress by suppressing PPARα signaling pathway, the effects of celastrol attenuated DCA-EGR1-inflammatory factor signaling in CCl4-induced PPARα deleted mice | Zhao et al. (2020) |
| Chemicals induced liver injury | Male Sprague | CCl4 | 0.25 mg/kg/day,0.5 mg/kg/day,1 mg/kg/day by i.p injection | 4 weeks | Suppressed inflammation in liver fibrosis by activating AMPK-SIRT3 signaling | Wang et al. (2020) |
| Dawley rats | ||||||
| Cholestatic liver injury | Male C57BL/6J mice | ANIT | 10 mg/kg/day by oral administration | 5 days | Alleviated cholestatic liver injury by activation SIRT1-FXR signaling pathway | Zhao et al. (2019b) |
| Male C57BL/6J mice and Fxr-null mice | TAA | FXR disruption attenuated protection effects of celastrol on cholestatic liver injury | ||||
| Cholestatic liver injury | Female Sprague-Dawley rats | EE | 5 mg/kg/day by an oral administration | 5 days | Alleviated phenotype of ICP by inhibited MMP-2 and MMP-9 | Guo et al. (2019) |
| Sepsis induced liver injury | Male Sprague Dawley rats | CLP | 1 mg/kg by i.p injection | 60 min before CLP | Attenuated inflammation by suppressing NF- κB, reduced TLR-4 and 5-LOX expression, downregulated the expression of IL-6 | El-Tanbouly et al. (2017) |
| Sepsis induced liver injury | Male C57BL/6 mice | LPS | 1.5 mg/kg/day by i.p injection | 24 h before LPS induction, after LPS intoxiant for another 24 h | Aggravated liver injury through activating inflammation and deteriorating oxidative stress | Wu et al. (2018) |
| Sepsis induced liver injury | Male C57BL/6J mice and NLRP3-/- mice | P. acnes/LPS | 0.5 or 0.25 mg/kg by i.p injection on every other day after P. acnes induction for 3 days | 3 days | Suppressed NLRP3 inflammasome formation by blocking deubiquitylation of NLRP3 | Yan et al. (2021) |
APAP, acetaminophen; CCl4, carbon tetrachloride; AMPK, Adenosine 5′-monophosphate (AMP)-activated protein kinase; SIRT3, sirtuin3; PPARα, Peroxisome Proliferator Activated Receptor α; DCA, deoxycholic acid; EGR1, Early Growth Response 1; ANIT,α-naphthyl isothio-cyanate; TAA, thioacetamide; SIRT1, sirtuin1; FXR, Farnesoid X receptor; EE, 17 -ethinyl estradiol; ICP, intrahepatic cholestasis of pregnancy; MMP-2, Matrix metalloproteinase-2; MMP-9, Matrixmetalloproteinase-9; CLP, cecal ligation and puncture; NF-κB, nuclear factor kappa-B; TLR4, Toll-like receptor 4; 5-LOX, 5-Lipoxygenase; IL-6, Interleukin-6; LPS, lipopolysaccharides; P. acnes/LPS, Propionibacterium acnes/lipopolysaccharides; NLRP3, NOD-like receptor protein 3.
As the number and variety of drug applications grow rapidly, drug-induced liver injury (DILI), especially acetaminophen (APAP) overdose, is becoming the most common cause of acute liver failure (ALF) in America and Europe (Shehu et al., 2017). A series of studies demonstrated that pretreatment with celastrol attenuated the APAP-induced oxidative stress and inflammation by raising antioxidant enzyme activities such as glutathione peroxidase (GPx), glutathione reductase (GR), catalase, and superoxide dismutase (SOD) activities both in vitro and in vivo (Abdelaziz et al., 2017; Jannuzzi et al., 2018). CCl4 as another hepatotoxic chemical could induce liver injury by inflammatory activation and antioxidant enzymes inhibition (Zhang et al., 2017b). Celastrol might also suppress inflammation in CCl4 induced liver injury rat by activating AMPK-SIRT3 signaling (Wang et al., 2020). In the latest research, Li and his colleagues found that celastrol could eliminate oxidative stress and reduce the release of proinflammatory cytokines by activating PPARα signaling pathway in CCl4 intoxicant mice (Zhao et al., 2020). However, celastrol itself as a drug also has toxicity, the balance between the liver protection and liver injury needs to be further studied, and new structure modification and formulation should be developed to reduce toxicity and enhance efficacy.
Cholestasis is a pathophysiological process caused by bile secretion and excretion disorders. It is manifested as excessive accumulation of bile components such as bile acid, cholesterol, and bilirubin in the liver and systemic circulation, causing damage to liver cells and whole body. Long-term continuous cholestasis will progress to liver fibrosis and even cirrhosis (Zollner and Trauner, 2008; Padda et al., 2011). Li and his colleagues demonstrated that celastrol ameliorated cholestatic liver injury induced by α-naphthyl isothiocyanate (ANIT) and thioacetamide (TAA) through activation of SIRT1-FXR signaling pathway, while the hepatoprotective effects of celastrol were abrogated in FXR deficiency or SIRT1 inhibition mice (Zhao et al., 2019b). In addition to that, 5 mg/kg/day celastrol remarkably alleviated intrahepatic cholestasis of pregnancy via downregulating matrix metalloproteinase (MMP-2 and MMP-9) and total bile acid in pregnant rats (Guo et al., 2019).
Sepsis is a serious clinical syndrome caused by many organisms including bacteria, viruses, and fungi, which might lead to liver injury (Strnad et al., 2017). Cecal ligation and puncture (CLP) model and lipopolysaccharide (LPS) inducement is often used to mimics sepsis (Zhang et al., 2014; Xiong et al., 2017; Li et al., 2020). Celastrol attenuated CLP induced hepatic dysfunction in rats by inhibiting toll-like receptor-4 (TLR-4)/NF-κB (El-Tanbouly et al., 2017). In addition, celastrol pretreatment was found to attenuate propionibacterium acnes/lipopolysaccharides induced liver damage via NLRP3 inflammasome suppression and inflammatory inhibition (Yan et al., 2021). On the contrary, celastrol aggravated liver injury by exacerbation of inflammatory and elevation of oxidative stress in LPS intoxicant mice (Wu et al., 2018). The contradictory results were attributed to the different dosage of LPS and celastrol, and it is hard for high dosage of celastrol to reverse the severe liver failure that resulted from high dose of LPS, and the toxicity of celastrol should be taken into consideration in treating sepsis.
In short, these data suggested that celastrol is a potential candidate for treatment of hepatic injury, mainly owing to its ability to inhibit inflammation and oxidative stress and recover bile acid homeostasis. While protecting the liver injury, the toxicity of celastrol should be also taken into consideration to avoid side effects.
Celastrol and Liver Cancer
Hepatocellular carcinoma (HCC) as one highly malignant cancer remains a global menace. Effective systemic treatment of HCC is impeded by its complicated molecular pathogenesis, high rate of metastasis, recurrence, and chemo-resistance. It is imperative to explore effective therapy strategies for liver cancer. Natural medicine with long history of clinical use exhibited great potential in anti-cancer due to its high efficiency and availability, as well as low side effects (Hu et al., 2013). Numerous studies have shown that celastrol exerts anticancer effects by inhibiting their proliferation, metastasis, and inflammatory properties depending on modulating a variety of signaling pathways (Kashyap et al., 2018).
Anti-Proliferation and Pro-Apoptotic Effects In Vitro
Celastrol arrested cell cycle and promoted apoptosis through suppression of STAT3/JAK2 signaling, PI3 K/Akt signaling, and ER-stress/UPR signaling in different hepatocellular cell lines (Table 4) (Chen et al., 2011; Rajendran et al., 2012; Li et al., 2013; Wei et al., 2014; Li et al., 2015; Ma et al., 2017; Ren et al., 2017; Du et al., 2020; Kun-Ming et al., 2020). In addition, celastrol inhibited hepatoma cell line growth and proliferation via arresting cell cycle in sub-G1 (Rajendran et al., 2012) and G2/M phase (Chen et al., 2011; Ren et al., 2017). Further studies showed that celastrol reduced the expression of c-myc and cyclin D1 which was closely related to cell cycle arrest of tumor cells in vivo on a time- and dose-dependent manner (Rajendran et al., 2012; Ma et al., 2017). Mechanistic studies revealed that celastrol could impede liver cancer through downregulation of HSP90 proteins, activation of c-Jun NH2 terminal kinase (JNK), and weakened MRC complex I activity (Chen et al., 2011). Apart from that, celastrol could also inhibit the migration, invasion, and metastasis of liver cancer by inhibiting the ROCK2-mediated phosphorylation of ezrin at Thr567 (Du et al., 2020), suppressing NF-κB and Akt activity, and downregulating miR-224, MMP-2, and MMP-9 (Li et al., 2013).
TABLE 4.
Anti-cancer effects of celastrol in vitro.
| Cell line | Effect of celastrol | Mechanism | Doses | Time | Reference |
|---|---|---|---|---|---|
| HepG2, Bel-7402 | Anti-proliferation, induce apoptosis | Downregulated the expression of E2F1 | 2.5 and 5 µM | 24 h, 48 h | Ma et al. (2017) |
| HepG2, Bel-7402 | Anti-proliferation, induce apoptosis | Induced autophagy and ER stress, lead to G2/M phase arrested | 1.25, 2.5, and 5 µM | 24 h | Ren et al. (2017) |
| Bel-7402 | Anti-proliferation, induce apoptosis | Promoted cytochrome c release, increase the expression of cleaved caspase-9, caspase 3 and the ratio of Bax/Bcl-2 | 0.78, 1.56, and 3.12 μg/ml | 24, 48, and 72 h | Li et al. (2015) |
| HepG2 | Anti-proliferation, anti-migration | Inhibited the CXCR4 mediated PI3K/Akt pathway, lead to sub-G0 phase arrested | 0.1, 0.3, 0.625, and 1 µM | 24 h | Kun-Ming et al. (2020) |
| HepG2 | Anti-proliferation, induce apoptosis | Induced ROS accumulation and G2-M phase blockage | 2, 4, and 6 µM | 24 h | Chen et al. (2011) |
| HepG2 | Anti-metastasis | Repressed NF-κB and Akt activity, downregulate the expression of miR-224, MMP2, and MMP9 | 0.1, 0.5, 1 µM | 18 h | Li et al. (2013) |
| Huh7, Hep3B | Anti-proliferation, Anti-migration, Anti-invasion and Enhanced Apoptosis | Repressed circ_SLIT3 and Bcl-2, raised the Bax expression, impeded circ_SLIT3/miR-223-3p/CXCR4 signaling | 0.5, 1 µM | 48 h | (Si et al., 2013; Kun-Ming et al., 2020) |
| C3A | Anti-proliferation, induce apoptosis, anti-metastasis | Modulated STAT3 activation with the inhibition of c-Src, JAK1, and JAK2 activation; downregulate the expression of cyclin D1, Bcl-2, Bcl-xL, survivin, Mcl-1, and VEG, caused sub-G1 phase arrested | 2.5, 5, and 10 µM | 24, 48, and 72 h | Rajendran et al. (2012) |
| MHCC97H | Anti-migration | Inhibited the ROCK2 mediated phosphorylation of ezrin at Thr567 | 0.5 µM | 4 and 8 h | Du et al. (2020) |
E2F1, E2F transcription factor 1; ER, endoplasmic reticulum; Bcl-2, B-cell lymphoma-2; Bax, BCL2- Associated X,; CXCR4, C-X-C motif chemokine receptor 4; PI3K, phosphatidylinositol-3 -kinase; AKT, protein kinase B; ROS, reactive oxygen species; NF-κB, nuclear factor kappa B; MMP2, Matrix metallopeptidase 2; MMP9, Matrix metallopeptidase 9; ccirc_SLIT3, circRNA, slit guidance ligand 3; JAK1, Janus kinase1; JAK2, Janus kinase2; Mcl-1, Myeloid Cell Leukemia Sequence 1; VEGF, vascular endothelial growth factor; ROCK2, Rho Associated Coiled-Coil Containing Protein kinase 2.
Tumor Suppression Effects In Vivo
As show in Table 5 (Chen et al., 2011; Rajendran et al., 2012; Wei et al., 2014; Chang et al., 2016; Kun-Ming et al., 2020; Saber et al., 2020; Si et al., 2021), studies have manifested that celastrol exhibits anticancer activity against a variety of liver cancer animal models such as HCC patient-derived xenografts BALB/cJ mice (Wei et al., 2014), different hepatocellular carcinoma cells derived xenografts mouse models (Rajendran et al., 2012; Ma et al., 2014; Ren et al., 2017; Si et al., 2021), and DEN induced HCC rats/mice (Chang et al., 2016; Saber et al., 2020) with dosage of 1–10 mg/kg for 3–10 weeks. Celastrol (4 mg/kg) prevented tumor proliferation and increased apoptosis via inhibition of STAT3/JAK2 signaling pathway in PLC/PRF5 cells derived xenografts HCC mice (Rajendran et al., 2012). Recently, different studies validated that inhibition of circ_SLIT3/miR-223-3p/CXCR4 signaling is involved in the anti-HCC activity of celastrol both in vitro and in vivo (Kun-Ming et al., 2020; Si et al., 2021). Meanwhile, celastrol has been demonstrated to decrease the hepatic lesions and elevation of serum alanine aminotransferase (ALT), glutamic oxalacetic transaminase (AST), alkaline phosphatase (ALP), and alpha fetoprotein (AFP) in diethylnitrosamine (DEN)-induced hepatocellular carcinoma (HCC) rats, due to activation of mitochondrial apoptosis induced by p53 (Chang et al., 2016; Saber et al., 2020). Consistent with this, combination therapy with celastrol (2 mg/kg) and metformin (200 mg/kg) not only attenuated hepatic injury with elevated liver enzymes but also decreased NLRP3 mediated NF-κB signaling to suppress anti-apoptotic processes in mice with DEN-induced HCC (Saber et al., 2020). Meanwhile, Jiang and his colleagues found that synergistic use of celastrol and PHA665752 (a c-Met inhibitor) significantly inhibited cell growth, migration in c-met deficient Huh7 cells, and Huh7 xenografts nude mice (Jiang et al., 2013). Besides that, celastrol could enhance the activity of anti-liver cancer drugs including sorafenib, lapatinib, and ABT-737 by cell growth inhibition and apoptosis induction (Zhu et al., 2012; Yan et al., 2014; Zhang et al., 2019). These results indicated that celastrol not only has good efficiency on killing cancer cells but also can improve the anti-cancer ability of first-line drugs for tumor therapy.
TABLE 5.
The anti-tumor effects of celastrol in vivo.
| Cancer model (animal) | Dose and formulation | Treatment period | Tumor volume | Mechanism | Reference |
|---|---|---|---|---|---|
| HCC patient-derived xenografts (BALB/cJ mice) | 4 mg/kg/day by intravenous injection | 3 weeks | Reduce 2–5 fold | Pro-apoptosis, anti-proliferation through inhibited phosphorylation of protein kinases in the Raf/MEK/ERK and PI3K/AKT/mTOR signaling pathways | Wei et al. (2014) |
| H22 cells derived xenografts (female BALB/c mice) | 1 and 2 mg/kg/day by i.p injection | 3 weeks | Reduce 2–4 fold | Induced of ER stress and apoptosis | Ren et al. (2017) |
| Hep3B cells derived xenografts (athymic nu/nu female mice) | 3 and 10 mg/kg/day by oral administration three times a week | 5 weeks | Reduce 2–2.5 fold | Reduced the hypoxia-induced accumulation of HIF-1α protein, inhibited angiogenesis, invasion, and metastasis | Ma et al. (2014) |
| PLC/PRF5 cells derived xenografts (athymic nu/nu female mice) | 1 and 2 mg/kg/day by i.p injection | 3 weeks | Reduce 1.5–2.5 fold | Antiproliferative and proapoptotic effects through suppression of STAT3 signaling | Rajendran et al. (2012) |
| Hep3B cells derived xenografts (athymic nu/nu female mice) | 2 mg/kg/day by i.p injection every 5 days | 30 days | Reduce 2–2.5 fold | Inhibited circ_SLIT3/miR-223-3p/CXCR4 signaling | Si et al. (2021) |
| DEN induced HCC in rats | 2, 4, and 8 mg/kg/day by oral administration | 10 weeks | Reduce 1.5–3 fold | Activated mitochondrial apoptosis pathway | (Chang et al., 2016; Saber et al., 2020) |
i.p, intraperitoneal; Raf, rapidly accelerated fibrosarcoma; ERK, Extracellular-signal-regulated kinases; MEK, Mitogen-activated protein kinase/ERK kinase; PI3K, phosphatidylinositol-3-kinase; AKT, protein kinase B; mTOR, mammalian target of rapamycin; STAT3, signal transducer and activator of transcription 3; HIF-1α, hypoxia-inducible factor, circ_SLIT3, circRNA slit guidance ligand 3; CXCR4, C-X-C motif chemokine receptor.
The Role of Hypoxia-Inducible Factor in Anti-Tumor Activity of Celastrol
Hypoxia was one of most important regulators in liver cancer progression. Hypoxia-inducible factor (HIF-1), a nuclear transcription factor, might be activated under hypoxia and specifically regulated oxygen and metabolic homeostasis (Balamurugan, 2016). HIF-1/2α protein is highly expressed in human HCC tissues, and correlates with tumor invasion and metastasis in HCC patients (Bangoura et al., 2004; Wong et al., 2014). In addition to antiproliferative and proapoptotic effects, celastrol repressed tumor growth, angiogenesis, invasion, and metastasis through reduced hypoxia-induced accumulation of HIF-1α protein (Ma et al., 2014). Ma et al. demonstrated that celastrol inhibited the hypoxia-induced accumulation of HIF-1α protein due to the downregulation of mTOR/p70S6K/EIF4E and ERK1/2 phosphorylation in Hep3B cells derived xenografts nude female mice, and the expression of angiogenesis related factors-vascular endothelial growth factor (VEGF) and erythropoietin (EPO) are both prevented (Ma et al., 2014). However, this result was challenged by Han and his co-workers, who found that celastrol promoted HIF-1α protein accumulation by inducing ROS and activating Akt/p70S6K signaling in HepG2 cells under hypoxia, and celastrol suppressed cancer cell growth by promoting mitochondrial autophagy and apoptosis in vitro (Han et al., 2014). The difference in hypoxia exposure time (16 h in Han et al.’s work vs. 6 h in Ma et al.’s study) of HepG2 cells might contribute to the discrepant results on HIF-1a expression for celastrol in the above studies.
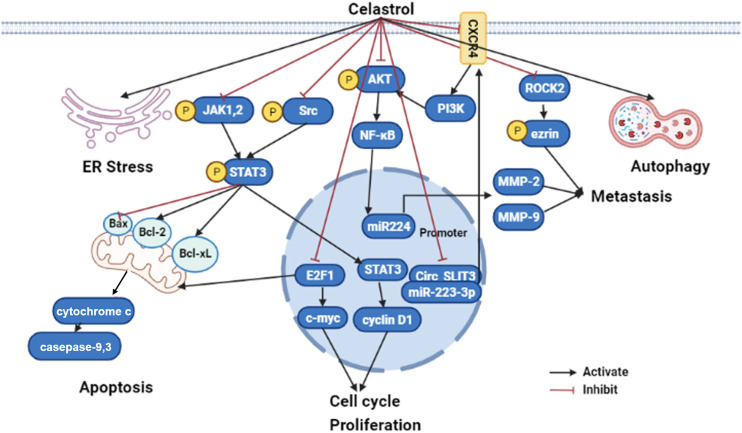
Summarily, celastrol might be a potential therapeutic candidate for the treatment of liver cancer due to reduction of the oxidative stress, inhibition of inflammatory response, and activation of mitochondrial autophagy. Although the studies were performed both in vitro and in vivo, the clinical research still should be performed to evaluate whether celastrol could apply as effective drug or adjuvant drug to further improve clinical outcomes. The mechanisms of celastrol on anti-cancer are summarized in Figure 3.
FIGURE 3.
The molecular mechanisms of celastrol in liver cancer (edited by Biorender software). Celastrol exert anticancer effect by restraining their cell growth, metastasis, and inflammatory response, while boosting ER stress, apoptosis, and autophagy depending on modulated different signaling pathways. Firstly, celastrol can activate cancer cell apoptosis through inhibiting JAK2 and STAT3 phosphorylation, then downregulated BCL-2 family proteins (Bcl-2 and Bcl-xl) and upregulated caspase family proteins (caspase 3 and caspase 9). Secondly, celastrol repressed tumor cell proliferation by suppressing cyclin D1 and c-myc through E2F1 and STAT3; Lastly, celastrol prohibited tumor metastasis by NF-κB signaling pathway modulated MMP-2 and MMP-9 through the CXCR4-related signaling pathway, as well as the ROCK2-mediated phosphorylation of ezrin at Thr567. ER, endoplasmic reticulum; JAK1, Janus kinase1; JAK2, Janus kinase2; STAT3, signal transducer and activator of transcription 3; Bcl-2, B-cell lymphoma-2; PI3K, phosphatidylinositol-3-kinase; AKT, protein kinase B; NF-kB, nuclear factor kappa B; MMP2, Matrix metallopeptidase 2; MMP9, Matrix metallopeptidase 9; circ_SLIT3, circRNA slit guidance ligand 3; ROCK2, Rho Associated Coiled-Coil Containing Protein kinase 2.
Limitations and Strategies for the Use of Celastrol
Although celastrol exhibited many benefits on various liver diseases, the shortcomings of celastrol limited its clinical transformation. On the one hand, the poor water solubility of celastrol (13.25 ± 0.83 μg/ml at 37°C) results in low oral bioavailability (17.06% in rat) (Qi et al., 2014), and more researches should be conducted on improving its water solubility and oral bioavailability. On the other hand, the side effects of celastrol and narrow therapeutic window of dose also could be a big problem for its clinical use. While 0.25 mg or 0.5 mg/kg/d, celastrol (i.p.) attenuated the LPS induced inflammation (Yan et al., 2021), 1.5 mg/kg/d, celastrol (i.p.) (Wu et al., 2018) aggravated the liver injury induced by celastrol. Beyond that, it was insufficient for CYP450s to metabolize celastrol, which led to the hepatotoxicity. In addition to damaging the liver, celastrol also has side effects on kidney (Wu et al., 2018), cardiovascular system, and hematopoietic system (Zhang et al., 2012). New modification and formulation are urgently needed to overcome the shortcomings and improve its efficacy.
Hopefully, new approaches have been reported to improve the water solubility and bioavailability of celastrol. Lipid-based nanocarriers (including the self-microemulsifying drug delivery system [SMEDDS] [Chen et al., 2012], nanostructured lipid carrier [NLC], and phytosomes) (Freag et al., 2018), polymer-based nanocarriers like PEG-PCL (poly(ethylene glycol)-poly(ɛ-caprolactone) copolymers) nanoparticles (Zhao et al., 2019a), and galactosylated liposomes (Chen et al., 2020b) markedly enhanced the water solubility and oral bioavailability of celastrol. Combination with other drugs can be an effective approach to reduce the toxicity and enhance the efficacy of celastrol. Currently, celastrol combined with chemotherapeutic agents, tumor necrosis factor superfamily, active ingredients of TCM, ionizing radiation, nucleic acid, and other therapies have been applied to the treatment of various cancers in vitro (Shi et al., 2020). The combined therapy reduced the dosage of celastrol and the related adverse effect, while the efficacy of celastrol improved. In addition, structural modifications will be a promising way to reduce the toxicity and improve the water bioavailability of celastrol, and the correlation between structure and toxicity have been well studied (Hou et al., 2020). Chemical modifications of celastrol mainly focused on the A/B ring and C-20 carboxyl group. In addition to chemical modifications, Chang et al. demonstrated that the glycosylation of celastrol formed by biotransformation showed over 53-fold higher water solubility and exhibited 50-fold less toxicity than celastrol in vivo (Chang et al., 2021), which indicated that biotransformation or biosynthesis might be a useful strategy for the clinical use of celastrol.
Conclusion and Perspectives
A large number of studies have shown that celastrol might be a potential drug for different liver diseases treatment. In this review, we summarized the recent studies about the protective effects and mechanisms of celastrol in several liver diseases, including MAFLD, and it caused liver injury, or liver cancer. The liver protection effect could be attributed to modulating metabolic balance, inhibiting inflammatory response, and activating autophagy by altering different cellular pathways (Tables 1–5). Although many researchers elucidated the molecular mechanisms of celastrol in liver diseases, the direct targets of celastrol are unknown. The SPR assay, affinity chromatographic methods, and other methods might be used to explore the direct interaction between celastrol and the potential targets. At the same time, with the development of omics, celastrol regulates gut microbes and liver metabolism to exert hepatoprotective effects required further investigated.
Moreover, although accumulating evidence demonstrated that celastrol grants tremendous potential in liver diseases at cellular or animal levels, the clinical studies of celastrol in liver diseases are very rare. Comprehensive studies on efficacy, safety, and toxicity in humans urgently need to be carried out. Besides, the poor water solubility, low bioavailability, and narrow therapeutic window of dose also limited the clinical application of celastrol. New modifications and formulations are needed to overcome the shortcomings and improve its efficacy. It is foreseeable that celastrol and its derivatives will be a promising drug for the treatment of liver diseases.
Acknowledgments
The author acknowledges and thanks Dr. Haijian Sun and Dr. Raphael N. Alolga for editing our article.
Author Contributions
SJ, ML, and L-WQ conceived the study, SJ and ML worte the manuscript, FX and LW drew the figure, ML, SJ, and GZ performed tables analysis. All authors contributed to the article and approved the submitted version.
Funding
This research funded by the National Natural Science Foundation of China (Grant No. 81900780 and Grant No. 82003933).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Abdelaziz H. A., Shaker M. E., Hamed M. F., Gameil N. M. (2017). Repression of Acetaminophen-Induced Hepatotoxicity by a Combination of Celastrol and Brilliant Blue G. Toxicol. Lett. 275, 6–18. 10.1016/j.toxlet.2017.04.012 [DOI] [PubMed] [Google Scholar]
- Abu Bakar M. H., Shariff K. A., Tan J. S., Lee L. K. (2020). Celastrol Attenuates Inflammatory Responses in Adipose Tissues and Improves Skeletal Muscle Mitochondrial Functions in High Fat Diet-Induced Obese Rats via Upregulation of AMPK/SIRT1 Signaling Pathways. Eur. J. Pharmacol. 883, 173371. 10.1016/j.ejphar.2020.173371 [DOI] [PubMed] [Google Scholar]
- Almazroo O. A., Miah M. K., Venkataramanan R. (2017). Drug Metabolism in the Liver. Clin. Liver Dis. 21, 1–20. 10.1016/j.cld.2016.08.001 [DOI] [PubMed] [Google Scholar]
- Bagherniya M., Nobili V., Blesso C. N., Sahebkar A. (2018). Medicinal Plants and Bioactive Natural Compounds in the Treatment of Non-alcoholic Fatty Liver Disease: A Clinical Review. Pharmacol. Res. 130, 213–240. 10.1016/j.phrs.2017.12.020 [DOI] [PubMed] [Google Scholar]
- Balamurugan K. (2016). HIF-1 at the Crossroads of Hypoxia, Inflammation, and Cancer. Int. J. Cancer 138, 1058–1066. 10.1002/ijc.29519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangoura G., Yang L. Y., Huang G. W., Wang W. (2004). Expression of HIF-2alpha/EPAS1 in Hepatocellular Carcinoma. World J. Gastroenterol. 10, 525–530. 10.3748/wjg.v10.i4.525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutari C., Mantzoros C. S. (2020). Adiponectin and Leptin in the Diagnosis and Therapy of NAFLD. Metabolism 103, 154028. 10.1016/j.metabol.2019.154028 [DOI] [PubMed] [Google Scholar]
- Canfora E. E., Meex R. C. R., Venema K., Blaak E. E. (2019). Gut Microbial Metabolites in Obesity, NAFLD and T2DM. Nat. Rev. Endocrinol. 15 (5), 261–273. 10.1038/s41574-019-0156-z [DOI] [PubMed] [Google Scholar]
- Caron A., Lee S., Elmquist J. K., Gautron L. (2018). Leptin and Brain-Adipose Crosstalks. Nat. Rev. Neurosci. 19, 153–165. 10.1038/nrn.2018.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caussy C., Loomba R. (2018). Gut Microbiome, Microbial Metabolites and the Development of NAFLD. Nat. Rev. Gastroenterol. Hepatol. 15, 719–720. 10.1038/s41575-018-0058-x [DOI] [PubMed] [Google Scholar]
- Chang T. S., Wang T. Y., Chiang C. M., Lin Y. J., Chen H. L., Wu Y. W., et al. (2021). Biotransformation of Celastrol to a Novel, Well-Soluble, Low-Toxic and Anti-oxidative Celastrol-29-O-β-Glucoside by Bacillus Glycosyltransferases. J. Biosci. Bioeng. 131, 176–182. 10.1016/j.jbiosc.2020.09.017 [DOI] [PubMed] [Google Scholar]
- Chang W., He W., Li P. P., Song S. S., Yuan P. F., Lu J. T., et al. (2016). Protective Effects of Celastrol on Diethylnitrosamine-Induced Hepatocellular Carcinoma in Rats and its Mechanisms. Eur. J. Pharmacol. 784, 173–180. 10.1016/j.ejphar.2016.04.045 [DOI] [PubMed] [Google Scholar]
- Chellappa K., Perron I. J., Naidoo N., Baur J. A. (2019). The Leptin Sensitizer Celastrol Reduces Age-Associated Obesity and Modulates Behavioral Rhythms. Aging cell 18, e12874. 10.1111/acel.12874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Zhang X., Zhao M., Wang Y., Cheng X., Wang D., et al. (2011). Celastrol Targets Mitochondrial Respiratory Chain Complex I to Induce Reactive Oxygen Species-dependent Cytotoxicity in Tumor Cells. BMC cancer 11, 170. 10.1186/1471-2407-11-170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Hu X., Hu J., Qiu Z., Yuan M., Zheng G. (2020). Celastrol-Loaded Galactosylated Liposomes Effectively Inhibit AKT/c-Met-Triggered Rapid Hepatocarcinogenesis in Mice. Mol. Pharm. 17, 738–747. 10.1021/acs.molpharmaceut.9b00428 [DOI] [PubMed] [Google Scholar]
- Chen Y., Yuan L., Zhou L., Zhang Z. H., Cao W., Wu Q. (2012). Effect of Cell-Penetrating Peptide-Coated Nanostructured Lipid Carriers on the Oral Absorption of Tripterine. Int. J. Nanomedicine 7, 4581–4591. 10.2147/IJN.S34991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Tian R., She Z., Cai J., Li H. (2020). Role of Oxidative Stress in the Pathogenesis of Nonalcoholic Fatty Liver Disease. Free Radic. Biol. Med. 152, 116–141. 10.1016/j.freeradbiomed.2020.02.025 [DOI] [PubMed] [Google Scholar]
- Diehl-Jones W. L., Askin D. F. (2002). The Neonatal Liver, Part 1: Embryology, Anatomy, and Physiology. Neonatal. Netw. 21, 5–12. 10.1891/0730-0832.21.2.5 [DOI] [PubMed] [Google Scholar]
- Dodd G. T., Xirouchaki C. E., Eramo M., Mitchell C. A., Andrews Z. B., Henry B. A., et al. (2019). Intranasal Targeting of Hypothalamic PTP1B and TCPTP Reinstates Leptin and Insulin Sensitivity and Promotes Weight Loss in Obesity. Cell Rep 28, 2905–e5. 10.1016/j.celrep.2019.08.019 [DOI] [PubMed] [Google Scholar]
- Du S., Song X., Li Y., Cao Y., Chu F., Durojaye O. A., et al. (2020). Celastrol Inhibits Ezrin-Mediated Migration of Hepatocellular Carcinoma Cells. Sci. Rep. 10, 11273. 10.1038/s41598-020-68238-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Tanbouly G. S., El-Awady M. S., Megahed N. A., Salem H. A., El-Kashef H. A. (2017). The NF-Κb Inhibitor Celastrol Attenuates Acute Hepatic Dysfunction Induced by Cecal Ligation and Puncture in Rats. Environ. Toxicol. Pharmacol. 50, 175–182. 10.1016/j.etap.2017.02.002 [DOI] [PubMed] [Google Scholar]
- Eslam M., Sanyal A. J., George J., International Consensus P. (2020). MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 158, 1999–2014. 10.1053/j.gastro.2019.11.312 [DOI] [PubMed] [Google Scholar]
- Fabbrini E., Sullivan S., Klein S. (2010). Obesity and Nonalcoholic Fatty Liver Disease: Biochemical, Metabolic, and Clinical Implications. Hepatology 51, 679–689. 10.1002/hep.23280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang P., He B., Yu M., Shi M., Zhu Y., Zhang Z., et al. (2019). Treatment with Celastrol Protects against Obesity through Suppression of Galanin-Induced Fat Intake and Activation of PGC-1α/GLUT4 axis-mediated Glucose Consumption. Biochim. Biophys. Acta Mol. Basis Dis. 1865, 1341–1350. 10.1016/j.bbadis.2019.02.002 [DOI] [PubMed] [Google Scholar]
- Feng L., Zhang D., Fan C., Ma C., Yang W., Meng Y., et al. (2013). ER Stress-Mediated Apoptosis Induced by Celastrol in Cancer Cells and Important Role of Glycogen Synthase Kinase-3β in the Signal Network. Cell Death Dis 4, e715. 10.1038/cddis.2013.222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X., Guan D., Auen T., Choi J. W., Salazar Hernández M. A., Lee J., et al. (2019). IL1R1 Is Required for Celastrol's Leptin-Sensitization and Antiobesity Effects. Nat. Med. 25, 575–582. 10.1038/s41591-019-0358-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X., Guan D., Auen T., Choi J. W., Salazar-Hernandez M. A., Faruk F., et al. (2019). Lipocalin 2 Does Not Play A Role in Celastrol-Mediated Reduction in Food Intake and Body Weight. Sci. Rep. 9, 12809. 10.1038/s41598-019-49151-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontana R. J., Hayashi P. H., Gu J., Reddy K. R., Barnhart H., Watkins P. B., et al. (2014). Idiosyncratic Drug-Induced Liver Injury Is Associated with Substantial Morbidity and Mortality within 6 Months from Onset. Gastroenterology 147, 96–e4. 10.1053/j.gastro.2014.03.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier K., Chang E. B. (2020). Intersection of the Gut Microbiome and Circadian Rhythms in Metabolism. Trends Endocrinol. Metab. 31, 25–36. 10.1016/j.tem.2019.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freag M. S., Saleh W. M., Abdallah O. Y. (2018). Self-assembled Phospholipid-Based Phytosomal Nanocarriers as Promising Platforms for Improving Oral Bioavailability of the Anticancer Celastrol. Int. J. Pharm. 535, 18–26. 10.1016/j.ijpharm.2017.10.053 [DOI] [PubMed] [Google Scholar]
- Friedman S. L., Neuschwander-Tetri B. A., Rinella M., Sanyal A. J. (2018). Mechanisms of NAFLD Development and Therapeutic Strategies. Nat. Med. 24, 908–922. 10.1038/s41591-018-0104-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García M. C., Wernstedt I., Berndtsson A., Enge M., Bell M., Hultgren O., et al. (2006). Mature-onset Obesity in Interleukin-1 Receptor I Knockout Mice. Diabetes 55, 1205–1213. 10.2337/db05-1304 [DOI] [PubMed] [Google Scholar]
- García-Rodríguez J. L., Barbier-Torres L., Fernández-Álvarez S., Gutiérrez-de Juan V., Monte M. J., Halilbasic E., et al. (2014). SIRT1 Controls Liver Regeneration by Regulating Bile Acid Metabolism through Farnesoid X Receptor and Mammalian Target of Rapamycin Signaling. Hepatology 59, 1972–1983. 10.1002/hep.26971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Wang Y., Wang N., Bai Y., Shi D. (2019). Celastrol Attenuates Intrahepatic Cholestasis of Pregnancy by Inhibiting Matrix Metalloproteinases-2 and 9. Ann. Hepatol. 18, 40–47. 10.5604/01.3001.0012.7860 [DOI] [PubMed] [Google Scholar]
- Hackl M. T., Fürnsinn C., Schuh C. M., Krssak M., Carli F., Guerra S., et al. (2019). Brain Leptin Reduces Liver Lipids by Increasing Hepatic Triglyceride Secretion and Lowering Lipogenesis. Nat. Commun. 10, 2717. 10.1038/s41467-019-10684-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X., Sun S., Zhao M., Cheng X., Chen G., Lin S., et al. (2014). Celastrol Stimulates Hypoxia-Inducible Factor-1 Activity in Tumor Cells by Initiating the ROS/Akt/p70S6K Signaling Pathway and Enhancing Hypoxia-Inducible Factor-1α Protein Synthesis. PloS one 9, e112470. 10.1371/journal.pone.0112470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W., Liu B., Xu H. (2020). Celastrol: Progresses in Structure-Modifications, Structure-Activity Relationships, Pharmacology and Toxicology. Eur. J. Med. Chem. 189, 112081. 10.1016/j.ejmech.2020.112081 [DOI] [PubMed] [Google Scholar]
- Hu M., Luo Q., Alitongbieke G., Chong S., Xu C., Xie L., et al. (2017). Celastrol-Induced Nur77 Interaction with TRAF2 Alleviates Inflammation by Promoting Mitochondrial Ubiquitination and Autophagy. Mol. Cell 66, 141–e6. 10.1016/j.molcel.2017.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu W., Wang L., Du G., Guan Q., Dong T., Song L., et al. (2020). Effects of Microbiota on the Treatment of Obesity with the Natural Product Celastrol in Rats. Diabetes Metab. J. 44, 747–763. 10.4093/dmj.2019.0124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Wang S., Wu X., Zhang J., Chen R., Chen M., et al. (2013). Chinese Herbal Medicine-Derived Compounds for Cancer Therapy: a Focus on Hepatocellular Carcinoma. J. Ethnopharmacol 149, 601–612. 10.1016/j.jep.2013.07.030 [DOI] [PubMed] [Google Scholar]
- Hua H., Zhang Y., Zhao F., Chen K., Wu T., Liu Q., et al. (2021). Celastrol Inhibits Intestinal Lipid Absorption by Reprofiling the Gut Microbiota to Attenuate High-Fat Diet-Induced Obesity. iScience 24, 102077. 10.1016/j.isci.2021.102077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jannuzzi A. T., Kara M., Alpertunga B. (2018). Celastrol Ameliorates Acetaminophen-Induced Oxidative Stress and Cytotoxicity in HepG2 Cells. Hum. Exp. Toxicol. 37, 742–751. 10.1177/0960327117734622 [DOI] [PubMed] [Google Scholar]
- Jarvis H., Craig D., Barker R., Spiers G., Stow D., Anstee Q. M., et al. (2020). Metabolic Risk Factors and Incident Advanced Liver Disease in Non-alcoholic Fatty Liver Disease (NAFLD): A Systematic Review and Meta-Analysis of Population-Based Observational Studies. Plos Med. 17, e1003100. 10.1371/journal.pmed.1003100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang H. L., Jin J. Z., Wu D., Xu D., Lin G. F., Yu H., et al. (2013). Celastrol Exerts Synergistic Effects with PHA-665752 and Inhibits Tumor Growth of C-Met-Deficient Hepatocellular Carcinoma In Vivo . Mol. Biol. Rep. 40, 4203–4209. 10.1007/s11033-013-2501-y [DOI] [PubMed] [Google Scholar]
- Kashyap D., Sharma A., Tuli H. S., Sak K., Mukherjee T., Bishayee A. (2018). Molecular Targets of Celastrol in Cancer: Recent Trends and Advancements. Crit. Rev. Oncol. Hematol. 128, 70–81. 10.1016/j.critrevonc.2018.05.019 [DOI] [PubMed] [Google Scholar]
- Katsiki N., Mikhailidis D. P., Mantzoros C. S. (2016). Non-alcoholic Fatty Liver Disease and Dyslipidemia: An Update. Metabolism 65, 1109–1123. 10.1016/j.metabol.2016.05.003 [DOI] [PubMed] [Google Scholar]
- Kazankov K., Jørgensen S. M. D., Thomsen K. L., Møller H. J., Vilstrup H., George J., et al. (2019). The Role of Macrophages in Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Nat. Rev. Gastroenterol. Hepatol. 16, 145–159. 10.1038/s41575-018-0082-x [DOI] [PubMed] [Google Scholar]
- Kun-Ming C., Chih-Hsien C., Chen-Fang L., Ting-Jung W., Hong-Shiue C., Wei-Chen L. (2020). Potential Anticancer Effect of Celastrol on Hepatocellular Carcinoma by Suppressing CXCR4-Related Signal and Impeding Tumor Growth In Vivo . Arch. Med. Res. 51, 297–302. 10.1016/j.arcmed.2020.03.001 [DOI] [PubMed] [Google Scholar]
- Kyriakou E., Schmidt S., Dodd G. T., Pfuhlmann K., Simonds S. E., Lenhart D., et al. (2018). Celastrol Promotes Weight Loss in Diet-Induced Obesity by Inhibiting the Protein Tyrosine Phosphatases PTP1B and TCPTP in the Hypothalamus. J. Med. Chem. 61, 11144–11157. 10.1021/acs.jmedchem.8b01224 [DOI] [PubMed] [Google Scholar]
- Lanthier N. (2015). Targeting Kupffer Cells in Non-alcoholic Fatty Liver Disease/non-Alcoholic Steatohepatitis: Why and How? World J. Hepatol. 7, 2184–2188. 10.4254/wjh.v7.i19.2184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roy T., Llopis M., Lepage P., Bruneau A., Rabot S., Bevilacqua C., et al. (2013). Intestinal Microbiota Determines Development of Non-Alcoholic Fatty Liver Disease in Mice. Gut. 62 (12), 1787–1794. 10.1136/gutjnl-2012-303816 [DOI] [PubMed] [Google Scholar]
- Li H., Li Y., Liu D., Sun H., Liu J. (2013). miR-224 Is Critical for Celastrol-Induced Inhibition of Migration and Invasion of Hepatocellular Carcinoma Cells. Cell Physiol Biochem 32, 448–458. 10.1159/000354450 [DOI] [PubMed] [Google Scholar]
- Li P. P., He W., Yuan P. F., Song S. S., Lu J. T., Wei W. (2015). Celastrol Induces Mitochondria-Mediated Apoptosis in Hepatocellular Carcinoma Bel-7402 Cells. Am. J. Chin. Med. 43, 137–148. 10.1142/S0192415X15500093 [DOI] [PubMed] [Google Scholar]
- Li Z., Feng H., Han L., Ding L., Shen B., Tian Y., et al. (2020). Chicoric Acid Ameliorate Inflammation and Oxidative Stress in Lipopolysaccharide and D-Galactosamine Induced Acute Liver Injury. J. Cell Mol Med 24, 3022–3033. 10.1111/jcmm.14935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y., Chen H., Liu Y., Hou X., Wei L., Bao Y., et al. (2022). Association of MAFLD with Diabetes, Chronic Kidney Disease, and Cardiovascular Disease: A 4.6-Year Cohort Study in China. J. Clin. Endocrinol. Metab. 107, 88–97. 10.1210/clinem/dgab641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licata A. (2016). Adverse Drug Reactions and Organ Damage: The Liver. Eur. J. Intern. Med. 28, 9–16. 10.1016/j.ejim.2015.12.017 [DOI] [PubMed] [Google Scholar]
- Lin L., Sun Y., Wang D., Zheng S., Zhang J., Zheng C. (2015). Celastrol Ameliorates Ulcerative Colitis-Related Colorectal Cancer in Mice via Suppressing Inflammatory Responses and Epithelial-Mesenchymal Transition. Front. Pharmacol. 6, 320. 10.3389/fphar.2015.00320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Lee J., Salazar Hernandez M. A., Mazitschek R., Ozcan U. (2015). Treatment of Obesity with Celastrol. Cell 161, 999–1011. 10.1016/j.cell.2015.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo D., Guo Y., Cheng Y., Zhao J., Wang Y., Rong J. (2017). Natural Product Celastrol Suppressed Macrophage M1 Polarization against Inflammation in Diet-Induced Obese Mice via Regulating Nrf2/HO-1, MAP Kinase and NF-Κb Pathways. Aging (Albany NY) 9, 2069–2082. 10.18632/aging.101302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X., Li H., Ma L., Zhou J., Guo X., Woo S. L., et al. (2018). Expression of STING Is Increased in Liver Tissues from Patients with NAFLD and Promotes Macrophage-Mediated Hepatic Inflammation and Fibrosis in Mice. Gastroenterology 155, 1971–e4. 10.1053/j.gastro.2018.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Han L. Z., Liang H., Mi C., Shi H., Lee J. J., et al. (2014). Celastrol Inhibits the HIF-1α Pathway by Inhibition of mTOR/p70S6K/eIF4E and ERK1/2 Phosphorylation in Human Hepatoma Cells. Oncol. Rep. 32, 235–242. 10.3892/or.2014.3211 [DOI] [PubMed] [Google Scholar]
- Ma L., Peng L., Fang S., He B., Liu Z. (2017). Celastrol Downregulates E2F1 to Induce Growth Inhibitory Effects in Hepatocellular Carcinoma HepG2 Cells. Oncol. Rep. 38, 2951–2958. 10.3892/or.2017.5971 [DOI] [PubMed] [Google Scholar]
- Ma X., Xu L., Alberobello A. T., Gavrilova O., Bagattin A., Skarulis M., et al. (2015). Celastrol Protects against Obesity and Metabolic Dysfunction through Activation of a HSF1-Pgc1α Transcriptional Axis. Cell Metab 22, 695–708. 10.1016/j.cmet.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Madrigal-Santillán E., Madrigal-Bujaidar E., Álvarez-González I., Sumaya-Martínez M. T., Gutiérrez-Salinas J., Bautista M., et al. (2014). Review of Natural Products with Hepatoprotective Effects. World J. Gastroenterol. 20, 14787–14804. 10.3748/wjg.v20.i40.14787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minsky N., Roeder R. G. (2015). Direct Link between Metabolic Regulation and the Heat-Shock Response through the Transcriptional Regulator PGC-1α. Proc. Natl. Acad. Sci. U S A. 112, E5669–E5678. 10.1073/pnas.1516219112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundi M. S., Velapati S., Patel J., Kellogg T. A., Abu Dayyeh B. K., Hurt R. T. (2020). Evolution of NAFLD and its Management. Nutr. Clin. Pract. 35, 72–84. 10.1002/ncp.10449 [DOI] [PubMed] [Google Scholar]
- Murphy E. F., Cotter P. D., Hogan A., O'Sullivan O., Joyce A., Fouhy F., et al. (2013). Divergent Metabolic Outcomes Arising from Targeted Manipulation of the Gut Microbiota in Diet-Induced Obesity. Gut 62, 220–226. 10.1136/gutjnl-2011-300705 [DOI] [PubMed] [Google Scholar]
- Myers M. G., Jr., Leibel R. L., Seeley R. J., Schwartz M. W. (2010). Obesity and Leptin Resistance: Distinguishing Cause from Effect. Trends Endocrinol. Metab. 21, 643–651. 10.1016/j.tem.2010.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ore A., Akinloye O. A. (2019). Oxidative Stress and Antioxidant Biomarkers in Clinical and Experimental Models of Non-alcoholic Fatty Liver Disease. Medicina (Kaunas) 55. 10.3390/medicina55020026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang M., Qin T., Liu H., Lu J., Peng C., Guo Q. (2021). Enhanced Inflammatory Reaction and Thrombosis in High-Fat Diet-Fed ApoE-/- Mice Are Attenuated by Celastrol. Exp. Clin. Endocrinol. Diabetes 129, 339–348. 10.1055/a-1010-5543 [DOI] [PubMed] [Google Scholar]
- Padda M. S., Sanchez M., Akhtar A. J., Boyer J. L. (2011). Drug-induced Cholestasis. Hepatology 53, 1377–1387. 10.1002/hep.24229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan W. W., Myers M. G., Jr. (2018). Leptin and the Maintenance of Elevated Body Weight. Nat. Rev. Neurosci. 19, 95–105. 10.1038/nrn.2017.168 [DOI] [PubMed] [Google Scholar]
- Pfuhlmann K., Schriever S. C., Baumann P., Kabra D. G., Harrison L., Mazibuko-Mbeje S. E., et al. (2018). Celastrol-Induced Weight Loss Is Driven by Hypophagia and Independent from UCP1. Diabetes 67, 2456–2465. 10.2337/db18-0146 [DOI] [PubMed] [Google Scholar]
- Purushotham A., Schug T. T., Xu Q., Surapureddi S., Guo X., Li X. (2009). Hepatocyte-specific Deletion of SIRT1 Alters Fatty Acid Metabolism and Results in Hepatic Steatosis and Inflammation. Cell Metab 9, 327–338. 10.1016/j.cmet.2009.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi X., Qin J., Ma N., Chou X., Wu Z. (2014). Solid Self-Microemulsifying Dispersible Tablets of Celastrol: Formulation Development, Charaterization and Bioavailability Evaluation. Int. J. Pharm. 472, 40–47. 10.1016/j.ijpharm.2014.06.019 [DOI] [PubMed] [Google Scholar]
- Rajendran P., Li F., Shanmugam M. K., Kannaiyan R., Goh J. N., Wong K. F., et al. (2012). Celastrol Suppresses Growth and Induces Apoptosis of Human Hepatocellular Carcinoma through the Modulation of STAT3/JAK2 Signaling cascade In Vitro and In Vivo . Cancer Prev. Res. (Phila) 5, 631–643. 10.1158/1940-6207.CAPR-11-0420 [DOI] [PubMed] [Google Scholar]
- Ren B., Liu H., Gao H., Liu S., Zhang Z., Fribley A. M., et al. (2017). Celastrol Induces Apoptosis in Hepatocellular Carcinoma Cells via Targeting ER-Stress/UPR. Oncotarget 8, 93039–93050. 10.18632/oncotarget.21750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers J. T., Lerin C., Haas W., Gygi S. P., Spiegelman B. M., Puigserver P. (2005). Nutrient Control of Glucose Homeostasis through a Complex of PGC-1alpha and SIRT1. Nature 434, 113–118. 10.1038/nature03354 [DOI] [PubMed] [Google Scholar]
- Saber S., Ghanim A. M. H., El-Ahwany E., El-Kader E. M. A. (2020). Novel Complementary Antitumour Effects of Celastrol and Metformin by Targeting IκBκB, Apoptosis and NLRP3 Inflammasome Activation in Diethylnitrosamine-Induced Murine Hepatocarcinogenesis. Cancer Chemother. Pharmacol. 85, 331–343. 10.1007/s00280-020-04033-z [DOI] [PubMed] [Google Scholar]
- Saito K., Davis K. C., Morgan D. A., Toth B. A., Jiang J., Singh U., et al. (2019). Celastrol Reduces Obesity in MC4R Deficiency and Stimulates Sympathetic Nerve Activity Affecting Metabolic and Cardiovascular Functions. Diabetes 68, 1210–1220. 10.2337/db18-1167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel V. T., Shulman G. I. (2018). Nonalcoholic Fatty Liver Disease as a Nexus of Metabolic and Hepatic Diseases. Cell Metab 27, 22–41. 10.1016/j.cmet.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saran A. R., Dave S., Zarrinpar A. (2020). Circadian Rhythms in the Pathogenesis and Treatment of Fatty Liver Disease. Gastroenterology 158, 1948–1966. 10.1053/j.gastro.2020.01.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehu A. I., Ma X., Venkataramanan R. (2017). Mechanisms of Drug-Induced Hepatotoxicity. Clin. Liver Dis. 21, 35–54. 10.1016/j.cld.2016.08.002 [DOI] [PubMed] [Google Scholar]
- Shi J., Li J., Xu Z., Chen L., Luo R., Zhang C., et al. (2020). Celastrol: A Review of Useful Strategies Overcoming its Limitation in Anticancer Application. Front. Pharmacol. 11, 558741. 10.3389/fphar.2020.558741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si H., Wang H., Xiao H., Fang Y., Wu Z. (2021). Anti-Tumor Effect of Celastrol on Hepatocellular Carcinoma by the circ_SLIT3/miR-223-3p/CXCR4 Axis. Cancer Manag. Res. 13, 1099–1111. 10.2147/CMAR.S278023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song X., Zhang Y., Dai E., Du H., Wang L. (2019). Mechanism of Action of Celastrol against Rheumatoid Arthritis: A Network Pharmacology Analysis. Int. Immunopharmacol 74, 105725. 10.1016/j.intimp.2019.105725 [DOI] [PubMed] [Google Scholar]
- Strnad P., Tacke F., Koch A., Trautwein C. (2017). Liver - Guardian, Modifier and Target of Sepsis. Nat. Rev. Gastroenterol. Hepatol. 14, 55–66. 10.1038/nrgastro.2016.168 [DOI] [PubMed] [Google Scholar]
- Sung H., Ferlay J., Siegel R. L., Laversanne M., Soerjomataram I., Jemal A., et al. (2021). Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A. Cancer J. Clin. 71, 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Świderska M., Maciejczyk M., Zalewska A., Pogorzelska J., Flisiak R., Chabowski A. (2019). Oxidative Stress Biomarkers in the Serum and Plasma of Patients with Non-alcoholic Fatty Liver Disease (NAFLD). Can Plasma AGE Be a Marker of NAFLD? Oxidative Stress Biomarkers in NAFLD Patients. Free Radic. Res. 53, 841–850. 10.1080/10715762.2019.1635691 [DOI] [PubMed] [Google Scholar]
- Tappy L. (2021). Metabolism of Sugars: A Window to the Regulation of Glucose and Lipid Homeostasis by Splanchnic Organs. Clin. Nutr. 40, 1691–1698. 10.1016/j.clnu.2020.12.022 [DOI] [PubMed] [Google Scholar]
- Thawley V. (2017). Acute Liver Injury and Failure. Vet. Clin. North America: Small Anim. Pract. 47, 617–630. 10.1016/j.cvsm.2016.11.010 [DOI] [PubMed] [Google Scholar]
- Tseng C. K., Hsu S. P., Lin C. K., Wu Y. H., Lee J. C., Young K. C. (2017). Celastrol Inhibits Hepatitis C Virus Replication by Upregulating Heme Oxygenase-1 via the JNK MAPK/Nrf2 Pathway in Human Hepatoma Cells. Antivir. Res 146, 191–200. 10.1016/j.antiviral.2017.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega R. B., Huss J. M., Kelly D. P. (2000). The Coactivator PGC-1 Cooperates with Peroxisome Proliferator-Activated Receptor Alpha in Transcriptional Control of Nuclear Genes Encoding Mitochondrial Fatty Acid Oxidation Enzymes. Mol. Cell Biol 20, 1868–1876. 10.1128/mcb.20.5.1868-1876.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vento S., Cainelli F. (2020). Acute Liver Failure. Lancet 395, 1833. 10.1016/S0140-6736(20)30046-5 [DOI] [PubMed] [Google Scholar]
- Wang C., Shi C., Yang X., Yang M., Sun H., Wang C. (2014). Celastrol Suppresses Obesity Process via Increasing Antioxidant Capacity and Improving Lipid Metabolism. Eur. J. Pharmacol. 744, 52–58. 10.1016/j.ejphar.2014.09.043 [DOI] [PubMed] [Google Scholar]
- Wang Y., Li C., Gu J., Chen C., Duanmu J., Miao J., et al. (2020). Celastrol Exerts Anti-inflammatory Effect in Liver Fibrosis via Activation of AMPK-SIRT3 Signalling. J. Cell Mol Med 24, 941–953. 10.1111/jcmm.14805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei W., Wu S., Wang X., Sun C. K., Yang X., Yan X., et al. (2014). Novel Celastrol Derivatives Inhibit the Growth of Hepatocellular Carcinoma Patient-Derived Xenografts. Oncotarget 5, 5819–5831. 10.18632/oncotarget.2171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C. C., Kai A. K., Ng I. O. (2014). The Impact of Hypoxia in Hepatocellular Carcinoma Metastasis. Front. Med. 8, 33–41. 10.1007/s11684-013-0301-3 [DOI] [PubMed] [Google Scholar]
- Wu M., Chen W., Yu X., Ding D., Zhang W., Hua H., et al. (2018). Celastrol Aggravates LPS-Induced Inflammation and Injuries of Liver and Kidney in Mice. Am. J. Transl Res. 10, 2078–2086. [PMC free article] [PubMed] [Google Scholar]
- Xiong X., Ren Y., Cui Y., Li R., Wang C., Zhang Y. (2017). Obeticholic Acid Protects Mice against Lipopolysaccharide-Induced Liver Injury and Inflammation. Biomed. Pharmacother. 96, 1292–1298. 10.1016/j.biopha.2017.11.083 [DOI] [PubMed] [Google Scholar]
- Xu J., Bartolome C. L., Low C. S., Yi X., Chien C. H., Wang P., et al. (2018). Genetic Identification of Leptin Neural Circuits in Energy and Glucose Homeostases. Nature 556, 505–509. 10.1038/s41586-018-0049-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Zhao W., Wang D., Ma X. (2018). Chinese Medicine in the Battle against Obesity and Metabolic Diseases. Front. Physiol. 9, 850. 10.3389/fphys.2018.00850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan C. Y., Ouyang S. H., Wang X., Wu Y. P., Sun W. Y., Duan W. J., et al. (2021). Celastrol Ameliorates Propionibacterium acnes/LPS-Induced Liver Damage and MSU-Induced Gouty Arthritis via Inhibiting K63 Deubiquitination of NLRP3. Phytomedicine 80, 153398. 10.1016/j.phymed.2020.153398 [DOI] [PubMed] [Google Scholar]
- Yan Y. Y., Guo Y., Zhang W., Ma C. G., Zhang Y. X., Wang C., et al. (2014). Celastrol Enhanced the Anticancer Effect of Lapatinib in Human Hepatocellular Carcinoma Cells In Vitro . J. BUON 19, 412–418. [PubMed] [Google Scholar]
- Yang X., Wu F., Li L., Lynch E. C., Xie L., Zhao Y., et al. (2021). Celastrol Alleviates Metabolic Disturbance in High-Fat Diet-Induced Obese Mice through Increasing Energy Expenditure by Ameliorating Metabolic Inflammation. Phytother Res. 35, 297–310. 10.1002/ptr.6800 [DOI] [PubMed] [Google Scholar]
- Ye Q., Zou B., Yeo Y. H., Li J., Huang D. Q., Wu Y., et al. (2020). Global Prevalence, Incidence, and Outcomes of Non-obese or Lean Non-alcoholic Fatty Liver Disease: a Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 5, 739–752. 10.1016/S2468-1253(20)30077-7 [DOI] [PubMed] [Google Scholar]
- Younossi Z., Anstee Q. M., Marietti M., Hardy T., Henry L., Eslam M., et al. (2018). Global burden of NAFLD and NASH: Trends, Predictions, Risk Factors and Prevention. Nat. Rev. Gastroenterol. Hepatol. 15, 11–20. 10.1038/nrgastro.2017.109 [DOI] [PubMed] [Google Scholar]
- Zhang A., Sun H., Wang X. (2013). Recent Advances in Natural Products from Plants for Treatment of Liver Diseases. Eur. J. Med. Chem. 63, 570–577. 10.1016/j.ejmech.2012.12.062 [DOI] [PubMed] [Google Scholar]
- Zhang D. G., Zhang C., Wang J. X., Wang B. W., Wang H., Zhang Z. H., et al. (2017). Obeticholic Acid Protects against Carbon Tetrachloride-Induced Acute Liver Injury and Inflammation. Toxicol. Appl. Pharmacol. 314, 39–47. 10.1016/j.taap.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Zhang J., Li C. Y., Xu M. J., Wu T., Chu J. H., Liu S. J., et al. (2012). Oral Bioavailability and Gender-Related Pharmacokinetics of Celastrol Following Administration of Pure Celastrol and its Related Tablets in Rats. J. Ethnopharmacol 144, 195–200. 10.1016/j.jep.2012.09.005 [DOI] [PubMed] [Google Scholar]
- Zhang R., Chen Z., Wu S. S., Xu J., Kong L. C., Wei P. (2019). Celastrol Enhances the Anti-liver Cancer Activity of Sorafenib. Med. Sci. Monit. 25, 4068–4075. 10.12659/MSM.914060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Yang N., Ni S., Li W., Xu L., Dong P., et al. (2014). Pretreatment of Lipopolysaccharide (LPS) Ameliorates D-GalN/LPS Induced Acute Liver Failure through TLR4 Signaling Pathway. Int. J. Clin. Exp. Pathol. 7, 6626–6634. [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Wang Y., Ge H. Y., Gu Y. J., Cao F. F., Yang C. X., et al. (2018). Celastrol Reverses Palmitic Acid (PA)-caused TLR4-MD2 Activation-dependent Insulin Resistance via Disrupting MD2-related Cellular Binding to PA. J. Cell Physiol 233, 6814–6824. 10.1002/jcp.26547 [DOI] [PubMed] [Google Scholar]
- Zhang Y., Geng C., Liu X., Li M., Gao M., Liu X., et al. (2017). Celastrol Ameliorates Liver Metabolic Damage Caused by a High-Fat Diet through Sirt1. Mol. Metab. 6, 138–147. 10.1016/j.molmet.2016.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Luo D., Zhang Z., Fan N., Wang Y., Nie H., et al. (2019). Celastrol-loaded PEG-PCL Nanomicelles Ameliorate Inflammation, Lipid Accumulation, Insulin Resistance and Gastrointestinal Injury in Diet-Induced Obese Mice. J. Control. Release 310, 188–197. 10.1016/j.jconrel.2019.08.026 [DOI] [PubMed] [Google Scholar]
- Zhao Q., Liu F., Cheng Y., Xiao X. R., Hu D. D., Tang Y. M., et al. (2019). Celastrol Protects from Cholestatic Liver Injury through Modulation of SIRT1-FXR Signaling. Mol. Cell Proteomics 18, 520–533. 10.1074/mcp.RA118.000817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Q., Tang P., Zhang T., Huang J. F., Xiao X. R., Zhu W. F., et al. (2020). Celastrol Ameliorates Acute Liver Injury through Modulation of PPARα. Biochem. Pharmacol. 178, 114058. 10.1016/j.bcp.2020.114058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu C., Yang J., Zhu Y., Li J., Chi H., Tian C., et al. (2021). Celastrol Alleviates Comorbid Obesity and Depression by Directly Binding Amygdala HnRNPA1 in a Mouse Model. Clin. Transl Med. 11, e394. 10.1002/ctm2.394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H., Yang W., He L. J., Ding W. J., Zheng L., Liao S. D., et al. (2012). Upregulating Noxa by ER Stress, Celastrol Exerts Synergistic Anti-cancer Activity in Combination with ABT-737 in Human Hepatocellular Carcinoma Cells. PloS one 7, e52333. 10.1371/journal.pone.0052333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Wan N., Shan X., Deng G., Xu Q., Ye H., et al. (2021). Celastrol Targets Adenylyl Cyclase-Associated Protein 1 to Reduce Macrophages-Mediated Inflammation and Ameliorates High Fat Diet-Induced Metabolic Syndrome in Mice. Acta Pharm. Sin B 11, 1200–1212. 10.1016/j.apsb.2020.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zollner G., Trauner M. (2008). Mechanisms of Cholestasis. Clin. Liver Dis. 12, 1–26. 10.1016/j.cld.2007.11.010 [DOI] [PubMed] [Google Scholar]