Abstract
The ‘implementation gap’ between national plans and successful implementation is a central theme in addressing non-communicable diseases (NCDs). It is a factor that has undermined Sustainable Development Goal 3.4, which aims to achieve a one-third reduction in premature mortality from four major NCDs by 2030. Responding to the potential of implementation research to support low-income and middle-income countries to effectively advance their strategies, we describe ways to make NCD plans more robust by including implementation steps. These steps are (1) choosing some (but not all) effective and cost-effective options; (2) tailoring interventions and their scale-up to national capacity; and (3) making the priorities implementable. We illustrate with examples from several countries.
Keywords: Health policy
Summary box.
Progress to implement effective solutions to non-communicable diseases in low- and middle- income countries varies; and for progress to accelerate more widely, it is essential to understand what currently undermines implementation.
Implementation research has been identified as a means to address the NCD ‘implementation gap’, yet application has been limited, and examples relate to specific, isolated aspects of implementation.
This paper presents a model that links analyses that address specific aspects of implementation into a coherent step-by-step process, illustrated with examples from various countries, and highlights where national capacity needs to be strengthened.
Introduction
Achieving Sustainable Development Goal (SDG) 3.4 to reduce premature mortality from non-communicable diseases (NCDs) is in jeopardy and is most threatened in low-income and middle- income countries, where NCDs are already 7 in 10 deaths.1 Progress in implementing effective solutions varies. For progress to accelerate, it is paramount to understand what undermines implementation.2 The ‘implementation gap’ is often discussed as if it were an end-stage issue—that is, countries somehow fail to successfully implement strong plans.
Rather than this final implementation stage being the problem, we suggest there are critical upstream issues. The value of implementation research has been recognised and applied with strong results for other health needs. It has been advocated as a means to better address NCDs,3 yet application has been limited. To realise this potential,4 coauthors drew from their experience, developing and leading national implementation plans and undertaking implementation research. Our aim was to create a coherent step-by-step process using specific implementation analyses and highlighting capacity gaps to create stronger NCD plans. We drew from our earlier NCD implementation roadmap,5 the WHO Multisectoral Action Plan (MAP) toolkit6 and the experiences of several countries.
The WHO has developed policy intervention recommendations for addressing NCDs, including the ‘Best Buys’7 for cost-effectiveness, PEN (Package of Essential Noncommunicable Disease Interventions) for primary care,8 MPOWER (Monitor, Protect, Offer, Warn, Enforce and Raise) for tobacco,9 SHAKE (Surveillance, Harness, Adopt, Knowledge and Environment) for salt,10 and SAFER (Strengthen, Advance, Facilitate, Enforce and Raise) for alcohol.11 Countries select policies that will be most impactful and cost-effective in their economic, social and institutional context, taking account of their capacity and needs. This requires assessing what is needed to put interventions into practice, identifying potential obstacles, and using this information to tailor intervention design and create supporting measures. The terms feasibility and viability have sometimes been used12; however, we use ‘implementability’ for its stronger link to successful implementation rather than its theoretical possibility, also encompassing the concept of ‘readiness’.13
We describe a practical process to guide countries to create more implementable NCD plans. We elaborate one possible model to explain and illustrate how implementation research can provide stakeholders with the data and insights they require. The steps are presented as sequential but their application need not be. Countries can simultaneously build on progress while identifying weaknesses and ways to address these. Countries face unique challenges relating to their context, but the proposed process focuses on addressing important common challenges undermining implementation. Developing national and local implementation research capacity is key, as this not only enables application of the ‘standard’ steps set out in this paper, but also empowers stakeholders to find solutions to any context-specific challenges.
The process and supporting analyses are set out in figure 1.
Figure 1.
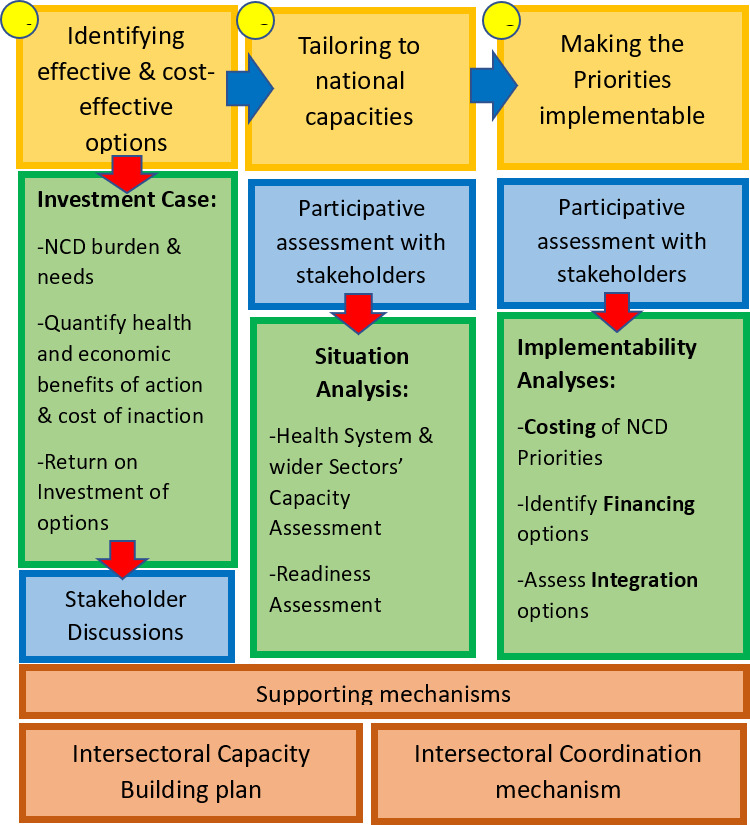
Steps for strengthening the implementability of national plans. NCD, non-communicable disease.
Step 1: choosing effective and cost-effective options
Step 1 entails an investment case, although other names are used.14 Investment cases contribute to prioritisation of cost-effective interventions and are feasible for the context. Investment cases raise political awareness of the costs of inaction, quantify the health and economic returns from investing, and demonstrate their contribution to SDG targets. They also can catalyse discussions about prioritising NCDs within national plans and budgets.15
Armenia’s investment case for NCDs led to parliamentary discussions to pass a 2020 tobacco control law.16 The Jamaica NCD investment case supported the prime minister’s declared economic growth targets demonstrating economic benefits from reducing NCD risks.17 Both examples fed into existing policy processes and were used by stakeholders to advance their goals. An NCD investment case for Peru Ministry of Health (MOH) found policy packages targeting NCD risk factors, particularly salt and alcohol consumption, had higher health and economic returns than treatment choices. The Peru NCD investment case identified hypertension screening and early treatment initiation as having a high return in lives saved, healthy life years gained and economic savings.18
Historically healthcare services predominated priority-setting discussions, with primary and secondary prevention relegated to a minor role, failing to reflect their critical importance. This might be because there is a powerful and vocal constituency for increased health services, including people living with diseases. Applying an analytical process enables a more even-handed consideration of a broader set of options to identify which will deliver the strongest health and economic benefits for a country. These may be in the policy domain as in the aforementioned examples or derive from preventive interventions delivered by the health system. The critical need to invest in prevention as well as treatment was apparent to Kenya MOH after an initial analysis identified a weak return on investment for cancer treatment in the short-medium term.19 For example, with support from the World Bank in Kenya, RTI International analysed preventive interventions for two highly prevalent cancers. The new analysis demonstrated that the benefits of early detection and treatment outweigh the costs in the long run, recommending scale-up of human papillomavirus vaccination and clinician and population awareness initiatives to improve early breast cancer diagnosis.20
To initiate a discussion about greater resource needs for NCD prevention and control, the Uganda MOH requested the United Nations Inter-Agency Task Force on NCDs (UNIATF) to develop evidence-based arguments. With stakeholder input and review of national data and documents, the Uganda investment case provided return on investment for detailed health service scale-up scenarios.21 The investment case has helped policymakers become aware that population health can provide long-term benefits and is being used to mobilise resources.
The United Nations Development Programme and UNIATF have responded to more than 50 country requests for investment cases since 2016. Meanwhile, advances in analytical methods are underway to improve the country-level data used, adhere to best practice recommendations for economic evaluations, and display and disseminate results to capture media and policy audience attention.22 A UNIATF meeting in April 2021 to share investment case methods strongly recommended framing investment cases as priority-setting exercises.23 It also highlighted how investment cases have been used as learning tools to identify weaknesses, gaps and opportunities. It was further noted that their results can gain wider traction when the sponsoring NCD division has links and relationships within and beyond the MOH, enabling it to leverage investment case results to achieve change beyond their division’s own purview.
Data relating to disease prevalence, programme coverage, costs and intervention effectiveness play a central role within these analyses, yet it is the case that NCD data, health information systems (HIS) more generally, and monitoring and evaluation in many low-income and middle-income countries (LMICs) are weak.24 Credibility is improved when locally produced data are used, underlining the critical need for countries to strengthen NCD surveillance systems—for example, undertaking STEPS (WHO STEPwise Approach to NCD Risk Factor Surveillance) surveys—and extend HIS to incorporate NCDs where this is not yet the case, supported by staff and infrastructure capacity development. National, system-wide HIS developments have been achieved in various countries but NCDs have frequently been excluded, resulting in fragmented and weak data. Given that NCD prevalence now exceeds that of many other health needs across LMICs, strengthening and mainstreaming NCD data need to be a domestic and donor priority.
Step 2: tailoring to national capacities
Even prioritised interventions may remain unimplemented unless they are grounded in national health system capacity and that of wider sectors that play essential roles for prevention policies.25 In step 2, national capacities and readiness to scale and integrate interventions are assessed. Participatory implementation research with stakeholders can be used to make such assessments and identify existing capacities including workforce skillset, infrastructure and systems, and community reach, as well as areas requiring capacity building.
Global analysis indicates various gaps in the infrastructure required to deliver NCD interventions in LMICs, such as workforce training, access to essential medicines, equipment and technology, guidelines and protocols, and laboratory services.26 In contrast, country-level needs assessments must be highly specific to what is needed to put national priority NCD interventions into practice. Undertaking a capacity assessment highlights areas where sufficient capacities exist to support implementation and specific gaps that need to be addressed—and this evidence of specific need can enable resource allocation (domestic or donor) to fill the gap. The WHO Service Availability and Readiness Assessment (SARA) is a tool to assess capacity across different health services27 and the WHO-PEN for primary healthcare in low-resource settings8 enables detailed health service assessment specifically for NCDs. For example, the Ugandan MOH Programme for the Prevention and Control of NCDs and the Uganda Initiative for Integrated Management of NCDs applied PEN to conduct the first national assessment of the readiness of public sector health facilities to provide NCD services. This identified areas of strength and gaps and weaknesses at specific levels and need to address availability of NCD-specific equipment, medicines, laboratory tests and in the workforce. The assessment also pinpointed weaknesses in basic screening and prevention services and the need for greater emphasis on quality assurance and monitoring.28
In contrast, the 2008 Tanzanian National NCD Strategy did not include or draw on capacity and readiness assessment,29 whereas subsequent assessments identified important gaps and weaknesses to explain the plan’s limited effectiveness. Tanzania’s 2016 National NCD Strategy explicitly included situational analysis using the SARA tool and could thereby articulate more detailed policy priorities and implementation activities.30 The lesson is that steps to determine exactly what capabilities are needed and where—in the health system, ministries or wider parts of government, and in civil society—should precede implementation.
Addressing NCDs requires greater priority for health promotion and prevention and these will be identified at step 1 as some of the most effective and cost-effective options. Capacity assessment for these is therefore important. These policies have been highlighted in various global reports and guidance as central,7 and often require involvement and sometimes the leadership of non-health sectors and partnerships across and beyond the government. The SARA assessment focuses on health system interventions; however, the national prevention policy and community actions that take place beyond the health system need to be assessed. Broadening capacity assessment to other sectors, including existing cross-sectoral policies, is important to identify gaps that would undermine what on paper may appear to be a strategic and strong NCD intervention and enable adequate planning and resourcing.31 Multistakeholder coordination mechanisms are a proven means to facilitate such engagement for various health conditions, being notably well developed for HIV-AIDS.32 While some cross-sectoral mechanisms have existed for many years—in Bangladesh for instance—more countries are developing NCD cross-sectoral groups and these may be used to assess the wider capacities available to support NCD prevention policies, strengthening requirements, and to identify barriers and how the strategy should address these. Review of the Tonga National NCD Strategy 2010–2015 found that critical governance and infrastructure gaps were impeding the implementation of NCD prevention and control strategies. As a result, in 2014, a national NCD committee with cross-government membership began to coordinate national NCD planning.33
Step 3: making the plans and priorities implementable
The next step involves a set of enabling processes, detailed below, that can make the difference between an NCD plan being only ‘a document on a shelf’ or being an implemented plan. Specific analyses can define and put in place these enabling processes aligned with national circumstances, opportunities and constraints.
Costing
Costing a national plan or strategy is an implementation prerequisite, not only to assess what is affordable but more fundamentally to ensure the required resources for NCDs are allocated within the national health budget. Lack of costing for national NCD plans has been reported as a contributory factor for non-implementation in high-income countries34 and LMICs.35 The situation is improving, however, as global NCD service cost estimates have recently become available36 and more countries have costed NCD strategies.36 Capacity building for local health economists and budget specialists has enabled health ministries to participate in the all-important government budgeting cycle,37 and those responsible for NCD strategy implementation need to be involved.38
Costing exercises reinforce the idea that providing a package of NCD services can be costly. Watkins et al35 report that 25%–34% of costs for the high-priority health intervention package in lower-income and lower-middle-income countries, respectively, would be required to fund 27 priority NCD interventions.35 Yet, without a realistic cost assessment for meeting NCD needs, ministries and stakeholders cannot request and advocate for (more) appropriate allocations. Moreover, rigorous costing for a package of priority NCD services can highlight potential savings by showing where prices can be reduced (eg, medicines) and cost efficiencies may be achieved (eg, integrating service delivery for comorbidities). The US Centers for Disease Control (CDC) developed a costing tool to accompany the WHO Global HEARTS technical package that has been used in various countries to assess NCD service costs.39
In 2021 the Government of Kenya launched its new Strategic Plan for the Prevention and Control of NCDs (2021–2025).40 Based on previous experience, whereby implementation of the preceding NCD strategy had been hampered by an absence of detailed costing, a costing analysis was undertaken to assist the development of realistic annual budgets to support the new plan. Activity-based costing was used to allocate input costs for activities where data existed and identify drivers of potential cost changes. The WHO One Health Tool was used to generate estimates for NCD commodity costs where forecasting and quantification data were lacking, alongside a pilot NCD Forecasting Tool for hypertension and diabetes medicines and technologies.
Financing options
Strong plans require adequate resources to put them into practice. Currently the financial resources available for NCD implementation are inadequate relative to the scale of burden and the capacity development required in many systems.41 Increasing domestic budgetary allocations to NCDs is needed, yet the COVID-19 pandemic hit the Gross Domestic Product (GDPs) of African countries especially hard. This situation calls for international donors and multilaterals to step up to address current NCD needs, to help countries strive to meet SDG 3.4 and to achieve long-term savings from slowing the onset of NCDs. Increasing national NCD resourcing is also vital to reduce the inordinate proportion of patient household income currently spent on out-of-pocket healthcare fees.
The necessary complement to costing NCD implementation is to identify the most appropriate financing options. Funding for NCDs will not be considered in isolation but as part of overall health system funding, and is best supported by good costing, priority-setting and budget planning within the MOH process. MOH NCD divisions can engage more strongly in financing dialogues after having assessed current and future needs and the funding gap. Thus, the ability to generate additional NCD financing within the domestic budget depends on the NCD unit having adequate information to justify requests. Ethiopia is an example of using strengthened domestic economic and budgeting capacity to bring about a robust discussion of NCD needs, resulting in significant scale-up of NCD services.36
Most LMIC NCD funding comes from domestic resources and NCD demand on domestic budgets will grow. An increased NCD budget will be more achievable if the economy is growing and there is willingness to allow increases in the total health budget. Other prerequisites are assuring value for money of implemented programmes and meeting equity goals. Assessment of financing options can explore the potential for additional revenue from, for example, resource reallocation, increased taxation, and innovative sources such as development bonds or social investment partnerships. Some countries, for instance Thailand and Philippines, have raised impressive revenues from taxing NCD-causing excisable products, such as alcohol, tobacco, unhealthy food and beverages, and fossil fuels, yet this strategy is generally underutilised.42
Innovative financing for NCDs is often touted as the solution to the financing gap.43 Social impact bonds (SIBs) are an innovative financing tool with seeming relevance to NCDs; however, a recent review found no LMIC examples of SIBs providing significant support for NCD programmes, and few high-income country examples had achieved their targets, suggesting that more experience is needed before SIBs will be a significant NCD funding contributor.44 In 2015, the WHO Global Coordination Mechanism Working Group provided recommendations for improving NCD financing and provided a template to help countries assess needs and options.45 The WHO is now developing a more detailed tool to guide NCD divisions, finance and budget officials in measuring the NCD financing gap and identifying options for reducing it.
Assessing integration options
Integration of NCDs into other health systems and services has been advocated as a potential means to address national capacity gaps and progress action.46 There is emerging evidence that this can also improve value for money.47 Step 3 includes assessing the scope and readiness for integrating NCDs within a country’s health system and programmes and drawing on existing capacities and infrastructure. Integration can be understood in different ways: co-located services providing more coordinated, user-centric care; and integration to achieve continuity of care over time, such as a child health package including antenatal, postnatal, newborn and young child services. Financing, budgeting, policymaking, management and even cross-sectoral collaboration can be considered integrated when simultaneously addressing multiple diseases and health goals.48
Many countries are currently testing integration options and identifying what type of integration may be most useful and how best to implement this. Integration of NCD care with HIV services is the programme area that has been tested to the greatest extent so far, and many countries have paired tuberculosis and diabetes care.49 Draft WHO guidance identifies health system readiness as an influential factor for successful integration, with certain levels of integration being suitable for different countries based on overall health system development. It identifies six assessment questions to assess readiness and strengths for NCD integration in primary healthcare, including governance, finance, human resources, service delivery, medicines and technology, and health information.46
In Uganda, the increased longevity of people living with HIV and the consequent growing burden of chronic disease in this population provided impetus to develop an NCD integration strategy in HIV care and other major vertical health programmes such as tuberculosis and maternal health. To better understand primary healthcare facilities’ capacity to manage NCDs, a needs assessment was undertaken helping the ministry understand gaps and mobilise resources to fill these. Integration pilot projects have been developed across different facility levels and regions to test diabetes and hypertension care delivery among these patient groups, and have generated evidence of patient and system benefit and learning related to integration planning.50 51 Training materials and NCD recording tools have been developed, alongside health worker training in NCD management. Supervision reports suggest increased screening and treatment initiation in regions where training has taken place.
Implementation planning
Steps 2 and 3 recommend specific analyses to address common NCD implementation pitfalls and strengthen national NCD planning. Nonetheless, there remains potential for strategies to be ineffective and poorly implemented if the ‘nuts and bolts’ of implementation planning, such as timelines, targets, monitoring and evaluation indicators, and assignment of delivery responsibility, are neglected52—something that is the case in high-income countries as well as LMICs.34 The WHO MAP toolkit includes a checklist highlighting these considerations.6 Moreover, LMIC governments and health ministries possess planning expertise, and this existing internal capacity may be leveraged to support stronger NCD implementation planning.53 54
Political will
Political will and leadership are essential for effective NCD policies to be passed and implemented.55 Even after addressing key information and planning gaps, an NCD strategy may still be unimplementable if political will and leadership are lacking. Our model does not address how to build and maintain political will. Nonetheless, the steps we have detailed can indirectly strengthen political will, first at step 1 by identifying the options most likely to provide health and economic gains enhancing their political attractiveness. The data can further strengthen buy-in when it is used for public advocacy, allowing politicians to appreciate public support for policies. Additionally, steps 2 and 3 enable a realistic assessment of what is possible and what needs to be done to make implementation effective, thus addressing the need for politicians to know that a strategy is implementable if they are to commit support.
Limitations
Our evidence derives from analyses focused on the individual steps, which we propose may instead be considered components of an overarching process that can generate practical information to address specific gaps and strengthen national NCD plan implementability. Our contention is that ‘the whole is greater than the sum of its parts’, and countries can benefit by addressing important weak points as a linked process rather than in isolation. Some countries have undertaken components of our model; however, we are unaware of the full process being applied. Research should therefore be undertaken to assess application of the model, evaluate outcomes and understand how the analyses may work best within a nationally led process.
Conclusion
A majority of LMICs face a future in which the burden of NCDs on health systems and economies is a reality. Dealing with that burden is widely acknowledged to be the responsibility of ministries of health with cross-sectoral support from various other ministries. Ministries are actively seeking tools and guidance to make progress against the rise of NCDs, but the danger of failing to attain SDG 3.4 is palpable, even had COVID-19 not further spotlighted the additional vulnerability of people with NCDs.56 The NCD literature is awash with calls for governments to ‘act on NCDs’. Rather than non-implementation representing simply a ‘lack of political will’, we suggest it also relates to weaknesses in the process of developing NCD strategies and plans. Indeed, these processes can help foster political will.
The steps described can be used by countries to set a direction and timetable for delivering. We suggest that a joined-up process using the kind of analyses presented can help countries identify how to strengthen their NCD strategies, implementation plans and processes. The COVID-19 pandemic impacted and continues to impact health systems and NCD implementation in various ways, both positive and negative.57 The process outlined provides an opportunity to understand and design responsive NCD plans. In parallel to the tools and technical guidance now available on specific NCD issues, tools are also needed to help countries undertake the more specific types of analysis. Alongside the tools, however, as NCD national-level planning in many LMICs is still relatively new, support during initial planning cycles combined with capacity building will help build confidence and capacity while contributing to stronger implementation in the immediate term. In this way countries can move closer to closing their NCD ‘implementation gap’ and achieve the kind of progress that their national NCD strategies promise.
Footnotes
Handling editor: Seye Abimbola
Twitter: @angiembjm, @martenrobert, @rachelnugent
Contributors: All authors contributed to discussion and writing of the manuscript. AMJ-M developed the concept in discussion with RN, and then expanded this further in discussion with RM, GM and EM.
Funding: RTI International provided publication fees.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Not required.
References
- 1.World Health Organisation . Noncommunicable diseases progress monitor 2020.
- 2.World Health Organisation . WHO Discussion Paper for the Regional Expert Consultations (Version dated 20 August 2021) Development of an Implementation Roadmap 2023–2030 for the Global Action Plan for the Prevention and Control of NCDs 2013–2030 [Internet], 2020. Available: https://cdn.who.int/media/docs/default-source/documents/health-topics/non-communicable-diseases/eb150-who-discussion-paper-on-ncd-roadmap-development-(20-aug-2021)-for-web.pdf?sfvrsn=58b8c366_5&download=true
- 3.Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ 2013;347:f6753. 10.1136/bmj.f6753 [DOI] [PubMed] [Google Scholar]
- 4.Marten R, Mikkelsen B, Shao R, et al. Committing to implementation research for health systems to manage and control non-communicable diseases. Lancet Glob Health 2021;9:e108–9. 10.1016/S2214-109X(20)30485-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackson-Morris A, Nugent R. Tailored support for national NCD policy and programme implementation: an over-looked priority. BMJ Glob Health 2020;5:e002598. 10.1136/bmjgh-2020-002598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation . Tools for national Multisectoral action plan for prevention and control of noncommunicable diseases (NCD MAP tool), 2021. [Google Scholar]
- 7.World Health O. Tackling NCDs: “Best buys” and other recommended interventions for the prevention and control of noncommunicable diseases. Geneva: World Health Organization, 2017. [Google Scholar]
- 8.World Health Organisation . WHO Package of Essential Non-Communicable (PEN) Disease Interventions [Internet]. WHO. Available: https://www.who.int/publications/i/item/who-package-of-essential-noncommunicable-(pen)-disease-interventions-for-primary-health-care
- 9.WHO . WHO | MPOWER brochures and other resources.
- 10.World Health Organisation . SHAKE the salt habit: the Technical package for salt Reduction [Internet], 2016. Available: https://apps.who.int/iris/bitstream/handle/10665/250135/9789241511346-eng.pdf;sequence=1
- 11.World Health Organisation . SAFER: A world free from alcohol related harms - the Technical Package [Internet]. WHO, 2019. Available: https://www.who.int/publications/i/item/the-safer-technical-package
- 12.Zou G, Witter S, Caperon L, et al. Adapting and implementing training, guidelines and treatment cards to improve primary care-based hypertension and diabetes management in a fragile context: results of a feasibility study in Sierra Leone. BMC Public Health 2020;20:1185. 10.1186/s12889-020-09263-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peters DH, Tran NT, Adam T. Implementation Research in Health - A Practical Guide [Internet]. Alliance for Health Policy and Syatems Research, World Health Organisation, 2013. Available: https://www.who.int/alliance-hpsr/alliancehpsr_irpguide.pdf
- 14.Hutchinson B, Nugent R. Guidance note for the development of national investment cases for neglected diseases, 2020. Uniting efforts for innovation, access and delivery. Available: https://adphealth.org/upload/resource/2849_ADP_Uniting_Efforts_Guidance_Note_171120_final.pdf
- 15.Hutchinson B, Small R, Acquah K, et al. The investment case as a mechanism for addressing the NCD burden: evaluating the NCD institutional context in Jamaica, and the return on investment of select interventions. PLoS One 2018;14:e0223412. 10.1371/journal.pone.0223412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organisation Regional Office for Europe . The Parliament of Armenia approves new law on tobacco control [Internet], 2020. Available: https://www.euro.who.int/en/countries/armenia/news/news/2020/2/the-parliament-of-armenia-approves-new-law-on-tobacco-control
- 17.The Gleaner, Jamaica, West Indies . Christopher Tufton | Clear the smokescreen – big tobacco ignoring evidence [Internet], 2021. Newspaper article. Available: https://jamaica-gleaner.com/article/commentary/20210801/christopher-tufton-clear-smokescreen-big-tobacco-ignoring-evidence
- 18.Panamerican Health Orgnanisation, United Nations Interagency Taskforce on NCDs, United Nations Development Programme . Prevención y control de las enfermedades no transmisibles y los trastornos mentales en el Perú. El caso a favor de la inversión. (The investment case for non-communicable disease prevention and control in Peru), 2021. Wasshington DC. Available: https://iris.paho.org/handle/10665.2/54414
- 19.Mensah J, Korir J, Nugent R. Combating noncommunicable diseases in Kenya: an investment case. Republic of Kenya: The World Bank Group; Ministry of Health, 2020. http://documents1.worldbank.org/curated/en/428881586197529642/pdf/Combating-Noncommunicable-Diseases-in-Kenya-An-Investment-Case.pdf [Google Scholar]
- 20.The World Bank . Economic evaluation of breast and cervical cancer control interventions in Kenya. Results report.
- 21.WHO Regional Office for Africa, WHO Uganda Country Office, UN Inter-Agency Task Force on the Prevention and Control of NCDs,, United Nations Development Programme . Prevention and control of noncommunicable diseases in Uganda the case for investment.
- 22.Bertram M, Banatvala N, Kulikov A, et al. Using economic evidence to support policy decisions to fund interventions for non-communicable diseases. BMJ 2019;365:l1648. 10.1136/bmj.l1648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mutale W, Bosomprah S, Shankalala P, et al. Assessing capacity and readiness to manage NCDs in primary care setting: gaps and opportunities based on adapted WHO PEN tool in Zambia. PLoS One 2018;13:e0200994. 10.1371/journal.pone.0200994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gouda HN, Richards NC, Beaglehole R, et al. Health information priorities for more effective implementation and monitoring of non-communicable disease programs in low- and middle-income countries: lessons from the Pacific. BMC Med 2015;13:233. 10.1186/s12916-015-0482-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Breda J, Wickramasinghe K, Peters DH, et al. One size does not fit all: implementation of interventions for non-communicable diseases. BMJ 2019;367:l6434. 10.1136/bmj.l6434 [DOI] [PubMed] [Google Scholar]
- 26.World Health Organisation . Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2019 global survey [Internet], 2020. WHO. Available: https://www.who.int/publications/i/item/ncd-ccs-2019
- 27.World Health Organisation . Service Availability and Readiness Assessment (SARA): an annual monitoring system for service delivery Reference Manual, Version 2.2 [Internet]. WHO, 2015. Available: https://www.who.int/healthinfo/systems/sara_introduction/en/#:~:text=The%20service%20availability%20and%20readiness%20assessment%20(SARA)%20methodology,developed%20by%20WHO,%20and%20the%20service%20provision
- 28.Rogers HE, Akiteng AR, Mutungi G, et al. Capacity of Ugandan public sector health facilities to prevent and control non-communicable diseases: an assessment based upon WHO-PEN standards. BMC Health Serv Res 2018;18:606. 10.1186/s12913-018-3426-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ministry of Health and Social Welfare . United Republic of Tanzania. National non-communicable disease strategy, June 2008, 2008. Available: https://www.iccp-portal.org/system/files/plans/Tanzania_National%20%20NCD%20strategy_2008-1.pdf
- 30.Government of the Republic of Tanzania,, Ministry of Health, Community Development, Gender, Elderly and Children . Strategic and action plan for the prevention and control of non communicable diseases in Tanzania 2016-2020, 2016. Available: https://www.worlddiabetesfoundation.org/sites/default/files/NCD%20Stategic%20Plan%202016%20-%202020.pdf#:~:text=The%20National%20NCDS%20Strategic%20Plan%20II%20%282016-2020%29%20for,developed%20after%20the%20previous%20Strategic%20Plan%20period%20ended
- 31.Tobacco Free Initiative, World Health Organisation . Assessing the national capacity to implement effective tobacco control policies Operational manual on planning, conduct and follow-up of joint national capacity assessments [Internet]. WHO, 2013. Available: https://apps.who.int/tobacco/publications/building_capacity/manual/en/index.html
- 32.Dickinson C, Druce N. Perspectives integrating country coordinating mechanisms with existing National health and AIDS structures: emerging issues and future directions. 4. Global Health Governance [Internet], 2010. http://www.ghgj.org/Dickinson%20and%20Druce_final.pdf [Google Scholar]
- 33.Tonga Health Promotion Foundation (TongaHealth) . National strategy for prevention and control of non-communicable diseases, 2015, 2016. Available: https://www.dfat.gov.au/sites/default/files/tonga-national-non-communicable-disease-strategy-2015-20.pdf
- 34.Theis DRZ, White M. Is obesity policy in England fit for purpose? Analysis of government strategies and policies, 1992-2020. Milbank Q 2021;99:126–70. 10.1111/1468-0009.12498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Watkins DA, Qi J, Kawakatsu Y, et al. Resource requirements for essential universal health coverage: a modelling study based on findings from disease control priorities, 3rd edition. Lancet Glob Health 2020;8:e829–39. 10.1016/S2214-109X(20)30121-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hailu A, Eregata GT, Stenberg K, et al. Is universal health coverage affordable? Estimated costs and fiscal space analysis for the Ethiopian essential health services package. Health Systems & Reform 2021;7:e1870061. 10.1080/23288604.2020.1870061 [DOI] [PubMed] [Google Scholar]
- 37.Bergen centre for ethics and priority setting (BCEPS), 2021. Available: https://www.uib.no/en/bceps/127910/about-bceps
- 38.Husain MJ, Allaire BT, Hutchinson B, et al. Assessing costs of a hypertension management program: an application of the HEARTS costing tool in a program planning workshop in Thailand. J Clin Hypertens 2020;22:111–7. 10.1111/jch.13773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.RTI International . HEARTS Costing Tool [Internet]. TEPHINET: Training in Epidemiology and Public Health Intreventions Network, 2022. Available: https://www.tephinet.org/tephinet-learning-center/tephinet-library/hearts-costing-tool
- 40.Republic of Kenya, Ministry of Health . National strategic plan for the Prevention and Control of Non-Communicable Diseases 2021/22 - 2025/26. Available: https://www.health.go.ke/wp-content/uploads/2021/07/Kenya-Non-Communicable-Disease-NCD-Strategic-Plan-2021-2025.pdf
- 41.Micah AE, Cogswell IE, Cunningham B, et al. Tracking development assistance for health and for COVID-19: a review of development assistance, government, out-of-pocket, and other private spending on health for 204 countries and territories, 1990–2050. The Lancet 2021;398:1317–43. 10.1016/S0140-6736(21)01258-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Task Force on Fiscal Policy for Health . Health Taxes to Save Lives: Employing Effective Excise Taxes on Tobacco, Alcohol, and Sugary Beverages [Internet]. New York: Bloomberg Philanthropies, 2019. https://www.bloomberg.org/program/public-health/task-force-fiscal-policy-health/ [Google Scholar]
- 43.Atun R, Knaul FM. Innovative financing: local and global opportunities. In: Closing the cancer divide. Harvard University Press, 2012. [Google Scholar]
- 44.Hulse ESG, Atun R, McPake B, et al. Use of social impact bonds in financing health systems responses to non-communicable diseases: Scoping review. BMJ Glob Health 2021;6:e004127. 10.1136/bmjgh-2020-004127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.WHO Global Coordination Mechanism on the Prevention and Control of Noncommunicable Diseases . Final report and recommendations from the Working Group on how to realize governments’ commitments to provide financing for NCDs. World Health Organization, 2016. [Google Scholar]
- 46.World Health Organisation . Implementation Guidance to INTEGRATE Noncommunicable Disease Services into Other Programmatic Areas and Health Systems [Internet], 2021. Available: https://www.who.int/news-room/articles-detail/publication-consultation-on-implementation-guidance-how-to-integrate-non-communicable-diseases-with-national-hiv-aids-tb-sexual-and-reproductive-health-programmes-and-into-the-health-system
- 47.Shiri T, Birungi J, Garrib AV, et al. Patient and health provider costs of integrated HIV, diabetes and hypertension ambulatory health services in low-income settings - an empirical socio-economic cohort study in Tanzania and Uganda. BMC Med 2021;19:230. 10.1186/s12916-021-02094-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organisation . Integrated health services - what and why? Technical Brief No.1 [Internet]. WHO, 2008. Available: http://www.who.int/healthsystems/service_delivery_techbrief1.pdf
- 49.USAID, Mangaement Services for Health, Challenge TB . Integrating Service Delivery for TB and Diabetes Mellitus – An Innovative and Scalable Approach in Ethiopia [Internet], 2017. Available: https://www.msh.org/sites/msh.org/files/ctb_brief_ethiopia_on_tb-dm_100317ms.pdf
- 50.Kwarisiima D, Atukunda M, Owaraganise A, et al. Hypertension control in integrated HIV and chronic disease clinics in Uganda in the SEARCH study. BMC Public Health 2019;19:511. 10.1186/s12889-019-6838-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sando D, Kintu A, Okello S, et al. Cost-effectiveness analysis of integrating screening and treatment of selected non-communicable diseases into HIV/AIDS treatment in Uganda. J Int AIDS Soc 2020;23(Suppl 1):e25507. 10.1002/jia2.25507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tuangratananon T, Wangmo S, Widanapathirana N, et al. Implementation of national action plans on noncommunicable diseases, Bhutan, Cambodia, Indonesia, Philippines, Sri Lanka, Thailand and Viet Nam. Bull World Health Organ 2019;97:129–41. 10.2471/BLT.18.220483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McRobie E, Wringe A, Nakiyingi-Miiro J, et al. HIV policy implementation in two health and demographic surveillance sites in Uganda: findings from a national policy review, health facility surveys and key informant interviews. Implement Sci 2017;12:47. 10.1186/s13012-017-0574-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cawley C, McRobie E, Oti S, et al. Identifying gaps in HIV policy and practice along the HIV care continuum: evidence from a national policy review and health facility surveys in urban and rural Kenya. Health Policy Plan 2017;32:1316–26. 10.1093/heapol/czx091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.UN Interagency Taskforce on NCDs . Investing in the prevention and control of non-communicable diseases for sustainable development: countries discussed the role of investment cases, 2019. Available: https://www.who.int/ncds/un-task-force/october2019-investment-case/en/
- 56.Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. The Lancet 2020;395:1678–80. 10.1016/S0140-6736(20)31067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pan American Health Organization . Rapid assessment of service delivery for NCDs during the COVID-19 pandemic in the Americas, 2020. Available: https://www.paho.org/en/documents/rapid-assessment-service-delivery-ncds-during-covid-19-pandemic-americas-4-june-2020
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.


