Abstract
Introduction
Understanding the health of immigrant children from birth to 18 years of age is important given the significance of the early childhood years and complexity of factors that may influence the health status of immigrant populations. Thus, the purpose of this review was to understand the extent and nature of the literature on the health of immigrant children in Canada.
Methods
We conducted a scoping review of the literature. The review was focused on studies of first-generation and second-generation immigrant children aged 0–18 years. We completed standardised data extraction of immigration status, immigration route, age of children, data source, health or clinical focus, country of origin and major findings.
Results
In total, 250 published papers representing data from 237 studies met the inclusion criteria for this study. A total of 178 articles used quantitative methodologies (mostly survey and cross-sectional study designs), 54 used qualitative methodologies and 18 used mixed methodologies. The articles considered in this review included 147 (59%) focusing on physical health, 76 (30%) focusing on mental health and 37 (15%) focusing on the social aspects of health for refugee and first-generation and second-generation immigrant children across the provinces and territories of Canada.
Conclusions
Several literature gaps exist with respect to child immigrant health in Canada. For instance, there are no exclusive studies on immigrant boys and limited studies on children of international students.
Keywords: child health, health policy, public health, review
What is already known on this topic
According to a phenomenon known as the healthy immigrant effect, immigrants to Canada arrive in better health than their Canadian-born counterparts, but many experience a decline in their health status with time in Canada.
Immigrant children in Europe and North America are at increased risk for communicable diseases, chronic illness, mental health disorders and poor social well-being.
What this study adds
Our review identified that experiences of discrimination and a lack of cultural competence within healthcare systems represent barriers to immigrant families using or seeking services for their children.
While immigrant children in Canada experience inequitable access to resources, their unique migration experiences differentially impact their physical health, mental health and social well-being.
How this study might affect research, practice or policy
Findings from this review support the development of collaborative and multisectoral networks that enact cultural safety for immigrant families, particularly newcomer immigrants and refugees, towards facilitating access to the Canadian healthcare system.
Introduction
Globally, trends in migration are increasing due to factors such as conflict, persecution, poor living environments and lack of personal safety.1 As of 2016, approximately 7 540 830 foreign-born individuals lived in Canada, representing 21.9% of the population.2 The size of Canada’s foreign-born population is also reflected in the proportion of immigrant children. Children under the age of 15 years with an immigrant background (ie, first-generation and second-generation immigrants) number nearly 2.2 million in Canada and could represent up to 49% of the total population of children by the year 2036.3 Considering the growing population of immigrant children in Canada, the significance of the early childhood years, and increasing evidence that immigration status profoundly influences well-being, an understanding of immigrant children’s outcomes from birth to 18 years of age is invaluable towards ensuring their long-term health and well-being.4
Evidence suggests immigrants arrive in Canada with better health than their Canadian-born counterparts, however, inequitable access to societal resources negatively influences the wholesome health they experience on arrival, a phenomenon referred to as the ‘healthy immigrant effect’.4 5 Social determinants of health such as housing, education, employment, food security, access to healthcare services and other social supports are foundational to well-being, and notably, these are also areas within which many immigrants face difficulties.6 7 Despite this generalisation, individuals from immigrant backgrounds are diverse and have unique intersecting factors that predispose them to increased vulnerabilities compared with their native counterparts. Various combinations of premigration and postmigration experiences also contribute to the health issues experienced by immigrants.5
Canadian primary care providers have identified several high priority issues among immigrant and refugee populations new to the country, such as certain infectious diseases, mental health conditions, iron deficiency anaemia, diabetes, dental caries and other key maternal and child health conditions.8 Children and infants of immigrant/refugee women may have poor nutritional status due to interruption of feeding, poor breastfeeding practices and lack of healthy food access.1 Additionally, many immigrants and refugees come from areas with increased incidences of communicable diseases which increase their risk of infection. However, non-communicable diseases leading to chronic illnesses are increasingly recognised as shaping the health status of immigrants and refugees.1
A systematic study in Europe demonstrated that immigrant children may be increasingly at risk of mental health disorders and medical conditions such as tuberculosis and dental caries9; in North America, Asian children have a higher risk of developing mental health issues due to ‘high acculturation stress, low English language competence, language brokering and discrepancies in children’s and parent’s cultural orientation (the non-Western cultural orientation, eg, collectivistic, acceptance feelings of parents or harsh parenting)’.10 By and large, immigrant children face compounded challenges during adolescence, as Pottie et al11 stressed, noting that first-generation immigrants are more likely to experience bullying, violence and suicidal behaviours compared with native-born or later-generation immigrants. Furthermore, exposure to adverse living conditions and unmet social determinants of health as children can have negative outcomes that lead to cycles of adversity and influence health across the lifespan and across generations.12 Therefore, the nested environment of immigrant children also has implication for future generations and requires increased attention.
This paper reports on a scoping review of evidence on immigrant child health in Canada. To our knowledge, this is the first comprehensive synthesis of the literature on the health of immigrant children in Canada. This review aimed to determine the extent, range and scope of the literature related to immigrant child health in Canada. Our approach allows for reflection on how future research, policy and practice can improve the health of Canadian children with an immigrant background.
Methods
We used a scoping review methodology to collate studies focusing on immigrant child health in Canada. Scoping reviews are appropriate for broad topics with diverse study designs.13 Arksey and O’Malley13 indicated five stages in conducting a scoping review. The first and second stages are identification of research questions and relevant studies through literature searches. The third stage includes study selection, and stages 4 and 5 comprise data extraction and collation.
Identification of research questions and relevant studies
We identified broad research questions as guided by Arksey and O’Malley13: (1) What is the extent and nature of the literature on the health of immigrant children in Canada? and (2) What are the gaps in evidence on the health of immigrant children in Canada? A health science librarian assisted in refining our search strategy and in searching the following databases: PUBMED, CINAHL, Scopus, SocIndex and Sociological Abstract. We combined three sets of keywords. The first set were those that represented immigrant populations, such as immigrant*, migrant*, immigration*, migration* and transients. The second set were those related to child, such as child*, adolescent*, infant, toddler and preschool. The third set were those that represented health, such as health*, wellness, wellbeing, illness*, disease* and morbidit*. We conceptualised immigrants inclusively, to describe ‘a person who moves into a country other than that of his or her nationality or usual residence, so that the country of destination effectively becomes his or her new country of usual residence’, whether short-term or long-term, corresponding to a stay between 3 and 12 months or >12 months, respectively.14We conceptualised health broadly, in line with WHO’s15 definition of health as ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. Our three keyword sets were also combined with the word Canada and the names of each Canadian province/territory (online supplemental file 1).
bmjgh-2021-008189supp001.pdf (67.4KB, pdf)
Our initial search was completed in 2017 to focus on articles from the previous 20 years; our updated database search was completed in May 2021. Journal articles were also identified through a review of the reference lists of articles meeting our inclusion criteria. We subsequently completed a grey literature search in February 2022 with revision of our initial submission to the journal. Grey literature were identified through targeted Google searches using the keywords applied in our database search. Our grey literature search also included the university grey literature collection; a search in ProQuest Dissertations and Theses and searches of the websites of government agencies, research institutes and organisations that focus on immigrant child health, child health or population health. We reviewed the first 100 results when searches yielded more than 10 pages. Our grey literature search is outlined in online supplemental file 2.
bmjgh-2021-008189supp002.pdf (759.2KB, pdf)
Study selection
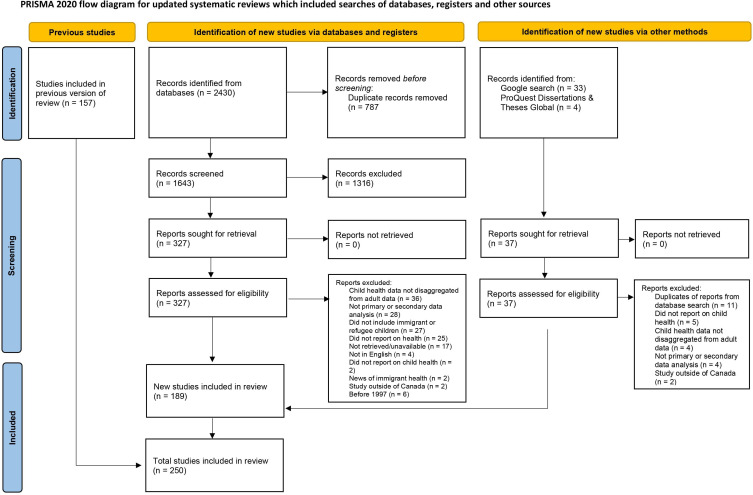
Due to the vast literature retrieved, we limited our analysis to articles published in the past 20 years at the time of the initial search in 2017, then updated our results to include articles published up to May 2021 when the last search was completed, then added the publications identified from our grey literature search. Two members of the research team read the titles and abstracts, then full text of relevant articles to identify those that met the inclusion criteria. Disagreements were resolved by a third member of the research team. Articles were included that: (1) focused on first-generation or second-generation immigrant children age 0–18 years; (2) contained primary data or secondary analysis and (3) reported on studies completed in Canada. In our screening, we conceptualised first-generation and second-generation immigrant children as children born outside of Canada or children with at least one parent born outside of Canada, respectively; this was inclusive of children of international students and transient foreign workers. We excluded reviews and articles focused on the education system without information on health. Grey literature were also reviewed using these criteria. Figure 1 details each stage of the selection process.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of selected studies. Adapted from Page et al.100 For more information, visit: http://www.prisma-statement.org/.
Data extraction and collation
We extracted the following information: author name(s), year of study, purpose, methodology, data collection method, sampling, sample size, gender of participants, immigration status, immigration route, age of child, data source (parent, child, health professional, etc), health or clinical focus, country of origin, province/territory of participants and major findings. Based on the approach by Arksey and O’Malley,13 we did not complete a quality appraisal of included studies as the main objective was to map out the extent of the literature. The team read the results and identified preliminary categories. These were then expanded and eventually collapsed into three major categories.
Results
In total, 250 published papers representing data from 237 studies met our inclusion criteria and are summarised in online supplemental file 3. A total of 178 articles used quantitative methodologies (mostly survey and cross-sectional study designs), 54 used qualitative methodologies (mostly explorative) and 18 used mixed methodologies. Most of the research studies were conducted in non-clinical settings. The type and size of the selected sample varied according to the study design. In quantitative studies, both probability and non-probability types of sampling were used. The most common was convenience sampling based on predetermined inclusion and exclusion criteria. Other common types were cluster or snowball sampling and secondary data analysis. Many studies used a combination of sampling strategies. Ninety-eight articles did not clearly describe the sampling strategy employed.
bmjgh-2021-008189supp003.pdf (56.7KB, pdf)
The sample size for quantitative studies ranged from 36 to 3 370 641 participants. Among qualitative studies, mostly purposive sampling was adopted, and the sample sizes ranged from 1 to 94. In mixed-method studies, various types of sampling techniques were used, and sample sizes ranged from 12 to 1225 participants. The main data sources were children and adolescents (n=119) followed by parents and caregivers (n=80). Large Canadian national datasets, various surveys and registries (n=66) as well as document, chart and record reviews (n=31) were also used as major sources of data. In a few studies, data were also collected from teachers (n=5), adults (n=7), families (n=6), healthcare professionals and service providers (n=15) and stakeholders and leaders (n=6).
Most studies included both male and female children (83%); however, a few studies focused primarily on adolescent girls. The most common age group was 13–18 years (27%) followed by 0–5 years (17%) and 6–12 years (10%). Immigrants listed regions of Asia, Africa, America, Europe, the Caribbean, the Middle East and Oceania as their countries of origin. Most studies broadly identified immigrants (56%) as the target population. The second-largest group identified was second-generation immigrants born in Canada (41%) followed by refugees (35%). Very few studies focused on children of international students or undocumented/failed claimant children. While the majority of studies specified the generation of the immigrant child as either first or second, approximately 23% of the studies did not provide this information. The majority of the selected studies in this scoping review were conducted in Ontario (45%), Québec (29%), British Columbia (16%) and Alberta (14%).
The 250 publications considered in this review included 147 (59%) focusing on physical health, 76 (30 %) focusing on mental health and 37 (15%) focusing on the social aspects of health. Due to poor delineation between first-generation and second-generation immigrant children in reports of findings, the synthesis of results focuses on studies addressing the health of refugee children, first-generation immigrant children and studies where the differences in the outcomes of first-generation and second-generation immigrant children are specified.
Physical health
Our review revealed a myriad of investigations into the causes, relationships, experiences and prevalence of physical illness among immigrant children. The most frequent topic was the identification and screening of tuberculosis in children and adolescents, with findings generally reporting poor outcomes. Immigrant children were at higher risk of testing positive for tuberculosis owing to low vaccination rates and high incidence rates in the countries from which they migrated.16–20 Dhawan et al21 identified that younger children, aged 4 years and below, had the highest prevalence of tuberculosis in an Albertan sample. Vitamin D deficiency followed as the second most studied physical health topic. This was highlighted as an under-recognised public health problem, with reports indicating immigrant children had lower-than-desirable vitamin D levels compared with the Canadian-born population and would benefit from dietary supplementation.22–25 Additionally, refugee children tended to have more significant levels of vitamin D deficiency compared with newcomer immigrant children.26 HIV and malaria were also of concern in immigrant child populations due to high incidence in countries of origin.27 28
Dental and oral health outcomes were less favourable for immigrant and refugee children due to poor oral hygiene, unawareness of publicly funded facilities and lack of dental health insurance, which jointly contributed to increased risk and prevalence of early childhood caries.29–33 Utilisation of dental services and adherence to preventative dental routines were facilitated by access to high-quality services, friendly and knowledgeable staff and providers, referrals or reminders and community-based dental programmes.34 A high prevalence of asthma among immigrant children postmigration to Canada was attributed to environmental factors, especially in relation to duration of residence.35 36 However, the overall incidence of asthma was lower in immigrants compared with long-term Canadian residents and the incidence in first-generation immigrant children was slightly lower than in second-generation immigrant children.37 Bin Yameen et al38 found refugee children had a higher prevalence of disparate visual acuity and unmet eye care needs compared with the general Canadian paediatric population. Several other health conditions were also identified in the literature. For example, refugee children younger than 5 years had a higher prevalence of anaemia than refugee children <15 years overall,39 and high rates of past or current infectious disease has been documented among immigrant and refugee children in Canada.40
Health behaviours and metrics that contributed to physical health were also investigated. Maticka-Tyndale et al41 found the median age of first intercourse for immigrant adolescent girls was comparable to their non-immigrant counterparts, but higher for adolescent immigrant boys. While newcomer youth who are sexually active are generally more likely to have accessed sexual health services, Salehi42 also found no association between gender and likelihood of accessing sexual health services. In comparison to their Canadian-born counterparts, immigrant youth had a lower incidence of tobacco use or smoking in general and first-generation immigrant adolescents were less likely to use cannabis.43–45
Studies on body mass index (BMI) and body fat showed an interesting mix of higher and lower BMI in immigrant child populations.46–49 BMI was lower among immigrant youth than their non-immigrant counterparts but subject to increases over time.50 Factors such as an abundance of fast food in Canada, the high cost of healthy foods, food insecurity and a change in diet from their home countries contributed to an upward trend in BMI and poor nutritional status in immigrant children; however, findings across studies showed BMI also differed with ethnicity.51 52 There was a lower prevalence of physical injury among immigrant children, but they also tended to have more severe injuries or were more likely to report multiple injuries compared with Canadian-born children.53 Refugee children typically benefitted from federal health programmes to bridge their access to primary and emergency care.54
Mental health
This review looked closely at the mental health of immigrant children in relation to acculturation, adaptation and discrimination. Some studies reported the mental health outcomes of immigrant adolescents as poor, as they displayed more emotional and behavioural problems in comparison to counterparts back in their home country.55 56 Other studies reported immigrant children generally had better mental health status than non-immigrant children, with an indication that second-generation immigrant children had poorer mental health status than first-generation immigrant children.57–59 Younger age at migration was associated with a greater risk of mood disorders and substance abuse.60–62 Notably, immigrant and refugee adolescents tended to have higher levels of resilience than non-migrants despite having experienced more trauma.63
Rousseau et al64 reported that while parents assessed their children’s mental health as generally good despite the stresses of resettlement, teenagers’ self-reports showed they internalised emotional problems to a great extent with this declining over adolescence. In a more recent study examining mothers’ perspectives, mothers reported concerns with poor mental in their children related to issues of discrimination, resettlement challenges, access and stigma.65 66 Results also described how immigrant children perceived themselves in light of their ethnic, linguistic and cultural similarities to peers, which influenced their sense of belonging, overall life satisfaction and was sometimes detrimental to their mental health.57 67–69
Postmigration perceptions of discrimination predicted both emotional problems and aggressive behaviour, especially among adolescent immigrants.70 This generally improved with family support and longer stays in the resettlement country.71 Refugee children with greater engagement with their family routines had better anger regulation, and postmigratory daily hassles were positively associated with increased sadness regulation in children with lower levels of premigratory life stressors.72 For some immigrant children, a weaker relationship with their parents was identified as a significant predictor of behavioural problems such as physical aggression, indirect aggression and property offences.73
The promotion of multiculturalism in Canada greatly enhanced adaptation, yet immigrant adolescents still felt discriminated against for their skin colour, especially within the first year of arrival in Canada.74 The sensitive subject of understanding immigrant children’s diagnoses through a collaborative lens by health service providers75—which should involve liaising with social agencies, schools, immigration or housing—was stressed. A multimodal approach was found to ease the integration of refugee children who fled to Canada to escape war and terrorism in their home countries.76 A good understanding of immigrant and refugee child mental health was emphasised to include appreciation of cultural differences, fostering emotional safety, inclusion of family and community in interventions, collaborative decision-making pathways and consideration of migration-specific variables.77–82
Social health
Coping strategies are required to adjust to a new society, and family support was shown in the findings of this study to be an integral strategy of resettlement and social adjustment.83 Immigrant adolescents navigated loss of family, friends and cultural familiarity due to migration, resulting in feelings of disconnection and a lack of belonging.78 84 Adjustment was often also critically affected by the low income levels of working immigrant families, which negatively impacted their children’s well-being.85 Low social support and sustained poverty were more common among minority migrants with young children. This social determinant of health weaved into greater deprivation indexes that accounted for disparities in help-seeking behaviours. These children presented more frequently to Canadian paediatric emergency departments and faced long wait times when seeking care.86–88 Other social barriers to access in Canada were language, especially for immigrants who were not native English or French speakers, and cultural differences, which fostered mistrust of institutional systems and doubts about provider compassion and competence.
Discussion
As the population of immigrants in Canada increased over the past several decades, the body of literature on their health outcomes grew accordingly. In recent years, a number of reviews have been undertaken which synthesise the outcomes and experiences of various immigrant populations in Canada, with a small proportion focusing on immigrant children. Our review thus fills a gap in knowledge by providing a comprehensive synthesis of the extant literature and outlining key findings about the physical health, mental health and social well-being of immigrant children in Canada. Our findings are consistent with recent reviews which emphasise interacting microfactors, mesofactors and macrofactors that impact the health of immigrant children in Canada.89–92 The interplay of diverse factors that improve, support or worsen the health of immigrant children stress the importance of attending to this population with multicomponent approaches that acknowledge their needs, strengths and unique experiences.
Of particular interest in the literature on immigrant health are the manifestations of the healthy immigrant effect within various immigrant populations and its effects on their short-term and long-term health outcomes. While this phenomenon is often broadly applied to all immigrant groups, recent systematic reviews highlight that the degree to which it occurs depends heavily on migration route, life-stage at the time of migration and the measures assessed.93 Economic-class immigrants tend to have a prominent health advantage on migration to Canada, while the research on refugee populations has been inconclusive.94 Additionally, adults aged 20–65 years are more likely to experience a decline in their health postmigration, but this varies across metrics such as level of overweight and prevalence of chronic conditions; furthermore, there is variability in the prevalence of healthy immigrant effect between male and female immigrants.94 Overall, patterns of health congruent with the healthy immigrant effect are more prominent in recent immigrants, immigrants from poorer countries and immigrants from culturally dissimilar countries compared with Canada, implicating broader structural factors which contribute to the health status of adult and child immigrant populations.93 95
For immigrant children, efforts to understand their postmigration health outcomes have yielded mixed results, as corroborated by our findings and other similar reviews.93 95 While previous findings on the well-being of immigrant youth demonstrate that they fare well in terms of health, social integration and school achievement despite bullying and other negative interactions with peers, our review reports varied outcomes.96 For example, our findings on the physical health revealed that immigrant children had worse outcomes in some areas (eg, tuberculosis, vitamin D deficiency, oral health, degree of injury), but better outcomes in others (eg, asthma, BMI, incidence of injury).16–26 29–37 Ethnicity and gender also influenced the variability of outcomes. Ethnic minority children had higher levels of vitamin D deficiency, with the highest seen in immigrant girls.51 Additionally, immigrant girls were more likely to be overweight, while immigrant boys had a higher prevalence of decayed, missing or filled teeth.26 31 Moreover, differences in physical health outcomes such as higher rates of asthma in second-generation immigrant children and increased prevalence of anaemia and unmet visual needs in refugee children further reflect the diversity in their health needs.29–33 38 39 This combination of findings also exposes the differential impacts of migration context and social determinants of health on the outcomes of immigrant children.95
Findings on the mental health and social well-being of immigrant children have historically been inconsistent as well. In several of the studies included in our review, immigrant children were reported to have better outcomes,57–59 63 82 with the reverse documented in other studies.55 56 On one occasion, parents’ reports of positive mental health in their children contradicted children’s self-reports which actually revealed high incidences of poor mental health64; furthermore, another group of parents reported concern about poor mental health in their children.65 Nevertheless, it should be acknowledged that parental reports of mental health are shaped by their cultural conceptualisations of mental health which may not correspond with Western conceptualisations, thus influencing how and what they communicate about their children’s mental health.82 Parents also reported socioeconomic status as a barrier to mental health service access,65 82 and it has been documented that socioeconomic status contributes to immigrant children’s self-perceived mental health and their shared sense of well-being within the family.66 84 96 Yet, despite the higher prevalence of poverty in immigrant households, immigrant children generally experience better mental and social well-being than their Canadian counterparts, in part, due to protective factors such as social networks and bonds with others of similar cultural and ethnic backgrounds which foster a sense of belonging.95 Social support is crucial to the well-being of children and youth, and especially important during periods of adjustment. In many immigrant families, strong transnational ties ameliorate the emotional, social, cultural and economic stresses associated with resettlement.97 However, discordance between cultural values in their home country and their host country can contribute to tension and pose greater challenges with identity and acculturation as immigrant children reconstruct their sense of self.82
Despite the mixed evidence on mental health and social well-being, consistent across studies were reports of discrimination which contributed to the development of emotional problems and aggressive behaviours. Children’s experiences with racism and discrimination deteriorated their self-esteem, leading to feelings of social isolation, and subsequently discouraged them from seeking professional assistance for physical or mental health concerns.41 65 Discrimination experienced by parents impacted immigrant children through the restrictions of opportunities available to their parents who balanced multiple low-wage jobs to meet material needs, leaving less time to nurture the development of social and emotional well-being in their children.65 Additionally, mental health in immigrant youth was also impacted by parental experiences with resettlement, parental mental health and parenting approach.65 81 The literature thus demonstrates that immigrant children’s experiences are not entirely independent from their parents’, nor are they isolated from the broader contexts of their migration. Factors which affect the health of immigrant parents are also implicated in their children’s health outcomes, most notably, in terms of health access and informed decision-making. This underscores the importance of a global perspective that accounts for children’s needs as separate, yet nested within their parents’ circumstances.65 83
Our findings highlight a number of systemic barriers that impact healthcare access for immigrant children and are echoed in a recent qualitative study on healthcare access for immigrant children in Canada.90 Social determinants of health such as education, employment, income, housing and food security, gender, social security and belonging have a pronounced influence on the health of immigrant populations.95 In addition to encounters with discrimination, immigrant populations in Canada experience access barriers related to culture, socioeconomic status, communication, knowledge and the structure of the healthcare system.98 Furthermore, language barriers, cultural discordance and challenges with acquiring information serve as deterrents to accessing many institutional systems such as primary care, mental health services or specialised care services for children with disabilities, asthma or cancer.65 90 99
The studies analysed in our review primarily focused on those aged 13–18 years, highlighting a significant lack of research on preteens and preschool-aged children despite how vital these years are to long-term health and well-being.4 Research on this population should focus on strategies to improve the health of refugee children, especially in terms of nutritional deficiencies, oral health and eye health due to their disparate outcomes in these areas.22–24 26 29–33 38 39 54 The extent of health coverage for refugee and undocumented migrant children is unknown, and little to no research has been done on the children of international students and transient foreign workers. It is also concerning that little research focuses on the health of immigrant boys; furthermore, none of the articles identified in our review addressed the health of immigrant children identifying as lesbian, gay, bisexual, transgender or queer. This is a missed opportunity to understand associations of gender and health, especially since gender has been identified as an important demographic factor in the health outcomes of immigrant children.70 83 For greater inclusivity and thorough consideration of intersectionality in research on immigrant child health, diverse gender categories need to be considered in future inquiries.
Additionally, notable differences exist across studies with respect to the definition of first-generation versus second-generation immigrants and in some studies, this was not delineated for the population of interest. The lack of disaggregated data across generations of immigrant children poses potential challenges in assessing for differences in their health outcomes. Standardised conceptualisations in data collection will facilitate a shared understanding of how various social determinants of health influence immigrant children’s health outcomes. Our review also reveals an apparent gap in research by presenting evidence that, despite findings by Rousseau et al,86 indicating undocumented immigrant children face an especially great risk of health inequities and disparities due to their precarious legal status, very few studies have focused on this vulnerable group. Longitudinal studies also need greater focus on unaccompanied minors and children of undocumented migrants to understand the health effects of migration status, unemployment and poverty.
Given the diverse backgrounds and experiences of immigrant populations, it is necessary to provide a full range of services, including culturally sensitive community-based treatment services and trauma-focused care.79 80 Further research on belief-related barriers among parents is needed to inform changes to existing services and programmes for newcomer families. Importantly, research should extend towards understanding the role of family, peer and educational systems in developing effective mental health programmes for immigrant children to build on the protective role of social support.62 67 68 81 83 95 Finally, there is a significant need for multidisciplinary research to explore broader familial and institutional factors constituting barriers to healthcare access for immigrant children.
Conclusion
Although this review was limited by the lack of clarity between first-generation and second-generation outcomes in some studies, it remains the first comprehensive document of its kind and provides a thorough overview of the literature for any healthcare professional wishing to engage in research involving immigrant child health in Canada. Our review revealed that there are still gaps in our knowledge of the health of immigrant children in Canada and this population still experiences challenges with healthcare access and disparate health outcomes across various measures. Collaborative multisectoral partnerships across health and social services may improve immigrant’s experiences with navigating services which are fundamental to their health and well-being.
Acknowledgments
We thank Sumera Idris for assisting with the identification of articles in updating this review.
Footnotes
Handling editor: Seema Biswas
Contributors: BS conceptualised the project and mentored research personnel. All authors participated in article selection, screening and data extraction. MO completed an updated search of articles. All authors except OS wrote parts of the paper for publication. BS and OS provided critical feedback on the paper. All authors contributed to the finalisation of the manuscript for submission. BS is acting as the guarantor.
Funding: The project was partially funded through graduate research assistantship support provided by the Faculty of Nursing, University of Alberta.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.World Health Organization . Draft 4+: global action plan to promote the health of refugees and migrants, 2018. Available: https://www.who.int/migrants/Global_Action_Plan_for_migration.pdf [Accessed 21 Oct 2021].
- 2.Statistics Canada . Immigration and ethnocultural diversity: key results from the 2016 census, 2017. Available: https://www150.statcan.gc.ca/n1/daily-quotidien/171025/dq171025b-eng.htm [Accessed 21 Oct 2021].
- 3.Statistics Canada . Children with an immigrant background: bridging cultures, 2017. available from:. Available: https://www12.statcan.gc.ca/census-recensement/2016/as-sa/98-200-x/2016015/98-200-x2016015-eng.cfm [Accessed 21 Oct 2021].
- 4.McDonald JT, Kennedy S. Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med 2004;59:1613–27. 10.1016/j.socscimed.2004.02.004 [DOI] [PubMed] [Google Scholar]
- 5.De Maio FG, Kemp E. The deterioration of health status among immigrants to Canada. Glob Public Health 2010;5:462–78. 10.1080/17441690902942480 [DOI] [PubMed] [Google Scholar]
- 6.Raphael D. Social determinants of health: Canadian perspectives. 3rd edn. Toronto, CA: Canadian Scholars’ Press Inc, 2016. [Google Scholar]
- 7.World Health Organization . Health impact assessment (HIA): the determinants of health, 2019. Available: https://www.who.int/hia/evidence/doh/en/ [Accessed 21 Oct 2021].
- 8.Swinkels H, Pottie K, Tugwell P, et al. Development of guidelines for recently arrived immigrants and refugees to Canada: Delphi consensus on selecting preventable and treatable conditions. CMAJ 2011;183:E928–32. 10.1503/cmaj.090290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gualdi-Russo E, Toselli S, Masotti S, et al. Health, growth and psychosocial adaptation of immigrant children. Eur J Public Health 2014;24:16–25. 10.1093/eurpub/cku107 [DOI] [PubMed] [Google Scholar]
- 10.Belhadj Kouider E, Koglin U, Petermann F. Emotional and behavioral problems in migrant children and adolescents in American countries: a systematic review. J Immigr Minor Health 2015;17:1240–58. 10.1007/s10903-014-0039-2 [DOI] [PubMed] [Google Scholar]
- 11.Pottie K, Dahal G, Georgiades K, et al. Do first generation immigrant adolescents face higher rates of bullying, violence and suicidal behaviours than do third generation and native born? J Immigr Minor Health 2015;17:1557–66. 10.1007/s10903-014-0108-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics 2009;124:S163–75. 10.1542/peds.2009-1100D [DOI] [PubMed] [Google Scholar]
- 13.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 14.International Organization of Migration . Key migration terms. Available: https://www.iom.int/key-migration-terms [Accessed 7 Mar 2022].
- 15.World Health Organization . Constitution of the World Health Organization as adopted by the International Health Conference, New York, 19–22 June 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948. In: Grad, Frank P. (2002). ‘The Preamble of the Constitution of the World Health Organization’. Bull WHO 1946;80:982. [Google Scholar]
- 16.Alvarez GG, Clark M, Altpeter E, et al. Pediatric tuberculosis immigration screening in high-immigration, low-incidence countries. Int J Tuberc Lung Dis 2010;14:1530–7. [PubMed] [Google Scholar]
- 17.Brassard P, Steensma C, Cadieux L, et al. Evaluation of a school-based tuberculosis-screening program and associate investigation targeting recently immigrated children in a low-burden country. Pediatrics 2006;117:e148–56. 10.1542/peds.2005-1534 [DOI] [PubMed] [Google Scholar]
- 18.Fortin K, Carceller A, Robert M, et al. Prevalence of positive tuberculin skin tests in foreign-born children. J Paediatr Child Health 2007;43:768–72. 10.1111/j.1440-1754.2007.01169.x [DOI] [PubMed] [Google Scholar]
- 19.Yang C, Yasseen AS, Stimec J, et al. Prevalence of tuberculosis infection and disease in children referred for tuberculosis medical surveillance in Ontario: a single-cohort study. CMAJ Open 2018;6:E365–71. 10.9778/cmajo.20180043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yasseen AS, Rea E, Hirji MM, et al. Paediatric tuberculosis among the foreign-born: utility of the Canadian TB immigration medical surveillance programme. Int J Tuberc Lung Dis 2019;23:105–11. 10.5588/ijtld.18.0317 [DOI] [PubMed] [Google Scholar]
- 21.Dhawan V, Bown J, Lau A, et al. Towards the elimination of paediatric tuberculosis in high-income, immigrant-receiving countries: a 25-year conventional and molecular epidemiological case study. ERJ Open Res 2018;4:00131-2017. 10.1183/23120541.00131-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aucoin M, Weaver R, Thomas R, et al. Vitamin D status of refugees arriving in Canada: findings from the calgary refugee health program. Can Fam Physician 2013;59:e188–94. [PMC free article] [PubMed] [Google Scholar]
- 23.Beukeboom C, Arya N. Prevalence of nutritional deficiencies among populations of newly arriving government assisted refugee children to Kitchener/Waterloo, Ontario, Canada. J Immigr Minor Health 2018;20:1317–23. 10.1007/s10903-018-0730-9 [DOI] [PubMed] [Google Scholar]
- 24.Guigné F, Duke P, Rourke L. Is vitamin D deficiency an underreported issue in refugee health?: two cases of infants presenting with vitamin D-deficiency rickets. Can Fam Physician 2013;59:641–3. [PMC free article] [PubMed] [Google Scholar]
- 25.Green TJ, Li W, Barr SI, et al. Vitamin D supplementation is associated with higher serum 25OHD in Asian and white infants living in Vancouver, Canada. Matern Child Nutr 2015;11:253–9. 10.1111/mcn.12008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lane G, Nisbet C, Whiting SJ, et al. Canadian newcomer children’s bone health and vitamin D status. Appl Physiol Nutr Metab 2019;44:796–803. 10.1139/apnm-2018-0705 [DOI] [PubMed] [Google Scholar]
- 27.MacPherson DW, Zencovich M, Gushulak BD. Emerging pediatric HIV epidemic related to migration. Emerg Infect Dis 2006;12:612–7. 10.3201/eid1204.051025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller KK, Banerji A. Epidemiology of malaria presenting at British Columbia’s children’s hospital, 1984–2001. Can J Public Health 2004;95:245–8. 10.1007/BF03405123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amin M, Perez A. Is the wait-for-patient-to-come approach suitable for African newcomers to Alberta, Canada? Community Dent Oral Epidemiol 2012;40:523–31. 10.1111/j.1600-0528.2012.00698.x [DOI] [PubMed] [Google Scholar]
- 30.Amin MS, Perez A, Nyachhyon P. Parental awareness and dental attendance of children among African immigrants. J Immigr Minor Health 2015;17:132–8. 10.1007/s10903-013-9912-7 [DOI] [PubMed] [Google Scholar]
- 31.Azrak ME, Huang A, Hai-Santiago K. The oral health of preschool children of refugee and immigrant families in Manitoba. J Can Dent Assoc 2017;83:1–10. [PubMed] [Google Scholar]
- 32.Locker D, Clarke M, Murray H. Oral health status of Canadian-born and immigrant adolescents in North York, Ontario. Community Dent Oral Epidemiol 1998;26:177–81. 10.1111/j.1600-0528.1998.tb01947.x [DOI] [PubMed] [Google Scholar]
- 33.Moreau A-M, Hennous F, Dabbagh B, et al. Oral health status of refugee children in Montreal. J Immigr Minor Health 2019;21:693–8. 10.1007/s10903-018-0835-1 [DOI] [PubMed] [Google Scholar]
- 34.Badri P, Wolfe R, Farmer A, et al. Psychosocial determinants of adherence to preventive dental attendance for preschool children among Filipino immigrants in Edmonton, Alberta. J Immigr Minor Health 2018;20:658–67. 10.1007/s10903-017-0599-z [DOI] [PubMed] [Google Scholar]
- 35.Moerman JN, Ratjen F, Subbarao P, et al. The prevalence of asthma in Canadian children of South Asian descent. Pediatr Pulmonol 2014;49:43–8. 10.1002/ppul.22907 [DOI] [PubMed] [Google Scholar]
- 36.Benchimol EI, Mack DR, Guttmann A, et al. Inflammatory bowel disease in immigrants to Canada and their children: a population-based cohort study. Am J Gastroenterol 2015;110:553–63. 10.1038/ajg.2015.52 [DOI] [PubMed] [Google Scholar]
- 37.Philipneri A, Hanna S, Mandhane PJ, et al. Association of immigrant generational status with asthma. Can J Public Health 2019;110:462–71. 10.17269/s41997-019-00201-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bin Yameen TA, Abadeh A, Lichter M. Visual impairment and unmet eye care needs among a Syrian pediatric refugee population in a Canadian City. Can J Ophthalmol 2019;54:668–73. 10.1016/j.jcjo.2019.03.009 [DOI] [PubMed] [Google Scholar]
- 39.Redditt VJ, Graziano D, Janakiram P, et al. Health status of newly arrived refugees in Toronto, ONT: Part 2: chronic diseases. Can Fam Physician 2015;61:e310–5. [PMC free article] [PubMed] [Google Scholar]
- 40.Redditt VJ, Janakiram P, Graziano D, et al. Health status of newly arrived refugees in Toronto, ONT: Part 1: infectious diseases. Can Fam Physician 2015;61:e303–9. [PMC free article] [PubMed] [Google Scholar]
- 41.Maticka-Tyndale E, Barrett M, McKay A. Adolescent sexual and reproductive health in Canada: a review of national data sources and their limitations. Can J Hum Sex 2000;9:41–65. [Google Scholar]
- 42.Salehi R. Indicators of access to sexual health services for Toronto newcomer youth [dissertation]. [Toronto]: York University; 2011. p. 283.
- 43.Georgiades K, Boyle MH, Duku E, et al. Tobacco use among immigrant and nonimmigrant adolescents: individual and family level influences. J Adolesc Health 2006;38:443.e1–443.e7. 10.1016/j.jadohealth.2005.02.007 [DOI] [PubMed] [Google Scholar]
- 44.Hamilton HA, Owusu-Bempah A, Boak A, et al. Ethnoracial differences in cannabis use among native-born and foreign-born high school students in Ontario. J Ethn Subst Abuse 2018;17:123–34. 10.1080/15332640.2017.1312655 [DOI] [PubMed] [Google Scholar]
- 45.Stoll K. Correlates and predictors of tobacco use among immigrant and refugee youth in a Western Canadian City. J Immigr Minor Health 2008;10:567–74. 10.1007/s10903-008-9136-4 [DOI] [PubMed] [Google Scholar]
- 46.Lane G, Farag M, White J, et al. Chronic health disparities among refugee and immigrant children in Canada. Appl Physiol Nutr Metab 2018;43:1043–58. 10.1139/apnm-2017-0407 [DOI] [PubMed] [Google Scholar]
- 47.Shea JM, Beausoleil N. Breaking down 'healthism': barriers to health and fitness as identified by immigrant youth in St. John’s, NL, Canada. Sport, Education and Society 2012;17:97–112. 10.1080/13573322.2011.607914 [DOI] [Google Scholar]
- 48.Quon EC, McGrath JJ, Roy-Gagnon M-H. Generation of immigration and body mass index in Canadian youth. J Pediatr Psychol 2012;37:843–53. 10.1093/jpepsy/jss037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kukaswadia A, Pickett W, Janssen I. Time since immigration and ethnicity as predictors of physical activity among Canadian youth: a cross-sectional study. PLoS One 2014;9:e89509. 10.1371/journal.pone.0089509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wahi G, Boyle MH, Morrison KM, et al. Body mass index among immigrant and non-immigrant youth: evidence from the Canadian community health survey. Can J Public Health 2014;105:e239–44. 10.17269/cjph.105.4288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lane G, Nisbet C, Vatanparast H. Food insecurity and nutritional risk among Canadian newcomer children in Saskatchewan. Nutrients 2019;11:1744–60. 10.3390/nu11081744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Quon E. Effects of generation of immigration on overweight in Canadian youth [thesis]. Montreal (QC): Concordia University, 2010. Available: https://spectrum.library.concordia.ca/979367/1/MR71018.pdf [Accessed 21 Oct 2021].
- 53.Hossain N. A portrait of immigrant children’s health: physical activity and injury prevention. [dissertation]. [Toronto]: York University. 2011. p. 138.
- 54.Evans A, Caudarella A, Ratnapalan S, et al. The cost and impact of the interim federal health program cuts on child refugees in Canada. PLoS One 2014;9:e96902. 10.1371/journal.pone.0096902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beiser M, Taa B, Fenta-Wube H, et al. A comparison of levels and predictors of emotional problems among preadolescent Ethiopians in Addis Ababa, Ethiopia, and Toronto, Canada. Transcult Psychiatry 2012;49:651–77. 10.1177/1363461512457155 [DOI] [PubMed] [Google Scholar]
- 56.Rousseau C, Drapeau A, Platt R. Living conditions and emotional profiles of Cambodian, Central American, and Québécois youth. Can J Psychiatry 2000;45:905–11. 10.1177/070674370004501005 [DOI] [PubMed] [Google Scholar]
- 57.Georgiades K, Boyle MH, Duku E. Contextual influences on children’s mental health and school performance: the moderating effects of family immigrant status. Child Dev 2007;78:1572–91. 10.1111/j.1467-8624.2007.01084.x [DOI] [PubMed] [Google Scholar]
- 58.Kwak K, Rudmin F. Adolescent health and adaptation in Canada: examination of gender and age aspects of the healthy immigrant effect. Int J Equity Health 2014;13:1–10. 10.1186/s12939-014-0103-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kwak K. An evaluation of the healthy immigrant effect with adolescents in Canada: examinations of gender and length of residence. Soc Sci Med 2016;157:87–95. 10.1016/j.socscimed.2016.03.017 [DOI] [PubMed] [Google Scholar]
- 60.Islam F. Immigrating to Canada during early childhood associated with increased risk for mood disorders. Community Ment Health J 2015;51:723–32. 10.1007/s10597-015-9851-y [DOI] [PubMed] [Google Scholar]
- 61.Patterson B, Kyu HH, Georgiades K. Age at immigration to Canada and the occurrence of mood, anxiety, and substance use disorders. Can J Psychiatry 2013;58:210–7. 10.1177/070674371305800406 [DOI] [PubMed] [Google Scholar]
- 62.Yang F-J. Is childhood migration a mental health risk? Exploring health behaviors and psychosocial resources as pathways using the cross-sectional Canadian community health survey. Soc Sci Res 2019;83:102303. 10.1016/j.ssresearch.2019.04.016 [DOI] [PubMed] [Google Scholar]
- 63.Stermac L, Elgie S, Dunlap H, et al. Educational experiences and achievements of war-zone immigrant students in Canada. Vulnerable Child Youth Stud 2010;5:97–107. 10.1080/17450120903440399 [DOI] [Google Scholar]
- 64.Rousseau C, Drapeau A, Rahimi S. The complexity of trauma response: a 4-year follow-up of adolescent Cambodian refugees. Child Abuse Negl 2003;27:1277–90. 10.1016/j.chiabu.2003.07.001 [DOI] [PubMed] [Google Scholar]
- 65.Tulli M, Salami B, Begashaw L, et al. Immigrant mothers’ perspectives of barriers and facilitators in accessing mental health care for their children. J Transcult Nurs 2020;31:598–605. 10.1177/1043659620902812 [DOI] [PubMed] [Google Scholar]
- 66.Author ADA, Ibrahim S, et al. African immigrant parents’ perspectives on the factors influencing their children’s mental health. J Child Fam Stud 2021;31:142–54. [Google Scholar]
- 67.Chow HPH. Sense of belonging and life satisfaction among Hong Kong adolescent immigrants in Canada. J Ethn Migr Stud 2007;33:511–20. 10.1080/13691830701234830 [DOI] [Google Scholar]
- 68.Gagné MH, Shapka JD, Law DM. Moving beyond grades: the social and emotional well-being of Chinese Canadians at school. Asian Am J Psychol 2014;5:373–82. 10.1037/a0038243 [DOI] [Google Scholar]
- 69.Emerson SD, Gagné Petteni M, Guhn M, et al. Social context factors and refugee children’s emotional health. Soc Psychiatry Psychiatr Epidemiol 2022;57:829–41. 10.1007/s00127-021-02173-y [DOI] [PubMed] [Google Scholar]
- 70.George MA, Bassani C. Influence of perceived racial discrimination on the health of immigrant children in Canada. J Int Migr Integr 2018;19:527–40. 10.1007/s12134-018-0539-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rousseau C, Hassan G, Measham T, et al. From the family universe to the outside world: family relations, school attitude, and perception of racism in Caribbean and Filipino adolescents. Health Place 2009;15:751–60. 10.1016/j.healthplace.2008.12.004 [DOI] [PubMed] [Google Scholar]
- 72.Elsayed D, Song J-H, Myatt E, et al. Anger and sadness regulation in refugee children: the roles of pre- and post-migratory factors. Child Psychiatry Hum Dev 2019;50:846–55. 10.1007/s10578-019-00887-4 [DOI] [PubMed] [Google Scholar]
- 73.Choi YR. Chinese immigrant children: predictors of emotional and behavioural problems [thesis]. Montreal, QC: McGill University, 2005. Available: https://escholarship.mcgill.ca/concern/parent/fx719m683/file_sets/f7623c96f [Accessed 21 Oct 2021].
- 74.Brabant LH, Lapierre S, Damant D, et al. Immigrant children: their experience of violence at school and community in host country. Child Soc 2016;30:241–51. 10.1111/chso.12131 [DOI] [Google Scholar]
- 75.Amirali EL, Bezonsky R, McDonough R. Culture and Munchausen-by-proxy syndrome: the case of an 11-year-old boy presenting with hyperactivity. Can J Psychiatry 1998;43:632–5. 10.1177/070674379804300614 [DOI] [PubMed] [Google Scholar]
- 76.Measham T, Guzder J, Rousseau C, et al. Refugee children and their families: supporting psychological well-being and positive adaptation following migration. Curr Probl Pediatr Adolesc Health Care 2014;44:208–15. 10.1016/j.cppeds.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 77.Beiser M, Hamilton H, Rummens JA, et al. Predictors of emotional problems and physical aggression among children of Hong Kong Chinese, mainland Chinese and Filipino immigrants to Canada. Soc Psychiatry Psychiatr Epidemiol 2010;45:1011–21. 10.1007/s00127-009-0140-3 [DOI] [PubMed] [Google Scholar]
- 78.Berman H, Mulcahy GA, Forchuk C, et al. Uprooted and displaced: a critical narrative study of homeless, Aboriginal, and newcomer girls in Canada. Issues Ment Health Nurs 2009;30:418–30. 10.1080/01612840802624475 [DOI] [PubMed] [Google Scholar]
- 79.Kanji Z. Understanding the experiences of Ismaili Afghan refugee children through photo conversations [dissertation]. Edmonton, AB: University of Alberta, 2009. Available: https://era.library.ualberta.ca/items/54a916b9-34ea-4a1e-ba1c-03aa7ee2792a [Accessed 21 Oct 2021].
- 80.de Freitas Girardi J, Miconi D, Lyke C, et al. Creative expression workshops as psychological first aid (Pfa) for asylum-seeking children: an exploratory study in temporary shelters in Montreal. Clin Child Psychol Psychiatry 2020;25:483–93. 10.1177/1359104519891760 [DOI] [PubMed] [Google Scholar]
- 81.Bolduc EL. Engagement into treatment: Comparing immigrants and non-immigrants in youth mental health services in Montreal [master’s thesis]. [Montreal (QC)]: McGill University. 2017. p. 94.
- 82.Khanlou N, Shakya Y, Muntaner C. Mental health services for newcomer youth: exploring needs and enhancing access, 2009. Available: https://accessalliance.ca/wp-content/uploads/2018/06/FINAL-REPORT-RG-No-122-CHEO-July-31-2009.doc.pdf [Accessed 22 Feb 2022].
- 83.Short KH, Johnston C. Stress, maternal distress, and children's adjustment following immigration: the buffering role of social support. J Consult Clin Psychol 1997;65:494–503. 10.1037/0022-006X.65.3.494 [DOI] [PubMed] [Google Scholar]
- 84.Caxaj CS, Berman H. Belonging among newcomer youths. ANS Adv Nurs Sci 2010;33:E17–30. 10.1097/ANS.0b013e3181fb2f0f [DOI] [PubMed] [Google Scholar]
- 85.Pitt RS, Sherman J, Macdonald ME. Low-income working immigrant families in Quebec: exploring their challenges to well-being. Can J Public Health 2015;106:e539–45. 10.17269/CJPH.106.5028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rousseau C, Laurin-Lamothe A, Rummens JA, et al. Uninsured immigrant and refugee children presenting to Canadian paediatric emergency departments: disparities in help-seeking and service delivery. Paediatr Child Health 2013;18:465–9. 10.1093/pch/18.9.465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vang ZM. Infant mortality among the Canadian-born offspring of immigrants and non-immigrants in Canada: a population-based study. Popul Health Metr 2016;14:1–15. 10.1186/s12963-016-0101-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vanthuyne K, Meloni F, Ruiz-Casares M, et al. Health workers' perceptions of access to care for children and pregnant women with precarious immigration status: health as a right or a privilege? Soc Sci Med 2013;93:78–85. 10.1016/j.socscimed.2013.06.008 [DOI] [PubMed] [Google Scholar]
- 89.Petrovskaya O A. The mental health of immigrant and refugee children in Canada: a scoping review. International Health Trends and Perspectives 2021;1:418–57. [Google Scholar]
- 90.Salami B, Mason A, Salma J, et al. Access to healthcare for immigrant children in Canada. Int J Environ Res Public Health 2020;17:3320–12. 10.3390/ijerph17093320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Salami B, Fernandez-Sanchez H, Fouche C, et al. A scoping review of the health of African immigrant and refugee children. Int J Environ Res Public Health 2021;18:3514–21. 10.3390/ijerph18073514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Scott D, Emerson LR, Martin G. A scoping review of associations between ethno-cultural context and mental health in Canada. Can J Commun Ment Health 2021;40:23–48. [Google Scholar]
- 93.Vang ZM, Sigouin J, Flenon A, et al. Are immigrants healthier than native-born Canadians? A systematic review of the healthy immigrant effect in Canada. Ethn Health 2017;22:209–41. 10.1080/13557858.2016.1246518 [DOI] [PubMed] [Google Scholar]
- 94.Lu C, Ng E. Healthy immigrant effect by immigrant category in Canada. Health Rep 2019;30:3–11. 10.25318/82-003-x201900400001-eng [DOI] [PubMed] [Google Scholar]
- 95.Barozzino T. Immigrant health and the children and youth of Canada: are we doing enough? Healthc Q 2010;14:52–9. 10.12927/hcq.2010.21983 [DOI] [PubMed] [Google Scholar]
- 96.Mental health of immigrants and non-immigrants in Canada: evidence from the Canadian health measures survey and service provider interviews in Alberta 2017.
- 97.Baffoe M. The social reconstruction of “home” among African immigrants in Canada. Can Ethn Stud 2010;41:157–73. 10.1353/ces.2010.0026 [DOI] [Google Scholar]
- 98.Ahmed S, Shommu NS, Rumana N, et al. Barriers to access of primary healthcare by immigrant populations in Canada: a literature review. J Immigr Minor Health 2016;18:1522–40. 10.1007/s10903-015-0276-z [DOI] [PubMed] [Google Scholar]
- 99.Kalich A, Heinemann L, Ghahari S. A scoping review of immigrant experience of health care access barriers in Canada. J Immigr Minor Health 2016;18:697–709. 10.1007/s10903-015-0237-6 [DOI] [PubMed] [Google Scholar]
- 100.Page MJ, McKenzie JE, Boutron I, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021. http://www.prisma-statement.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-008189supp001.pdf (67.4KB, pdf)
bmjgh-2021-008189supp002.pdf (759.2KB, pdf)
bmjgh-2021-008189supp003.pdf (56.7KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.