Abstract
Introduction
The impact of the COVID-19 pandemic on cancer screenings and care has yet to be determined. This study aims to investigate the screening, diagnosis, and mortality rates of the top five leading causes of cancer mortality in the United States from 2019 to 2021 to determine the potential impact of the COVID-19 pandemic on cancer care.
Methods
A retrospective cohort study investigating the impact of the COVID-19 pandemic on screening, diagnoses, and mortality rates of the top five leading causes of cancer death (lung/bronchus, colon/rectum, pancreas, breast, and prostate), as determined by the National Institute of Health (NIH) utilizing The United States Healthcare Cost Institute and American Cancer Society databases from 2019 to 2021.
Results
Screenings decreased by 24.98% for colorectal cancer and 16.01% for breast cancer from 2019 to 2020. Compared to 2019, there was a .29% increase in lung/bronchus, 19.72% increase in colorectal, 1.46% increase in pancreatic, 2.89% increase in breast, and 144.50% increase in prostate cancer diagnoses in 2020 (all P < .01). There was an increase in the total number of deaths from colorectal, pancreatic, breast, and prostate cancers from 2019 to 2021.
Conclusion
There was a decrease in the screening rates for breast and colorectal cancer, along with an increase in the estimated incidence and mortality rate among the five leading causes of cancer deaths from 2019 to 2021. The findings suggest that the COVID-19 pandemic is associated with impaired cancer screening, diagnosis, and care, and further emphasizes the need for proactive screening and follow-up to prevent subsequent cancer morbidity and mortality.
Keywords: cancer screening, cancer diagnosis, cancer mortalities, covid-19 pandemic, prevention interventions
Introduction
Throughout the coronavirus disease 2019 (COVID-19), there have been concerns regarding the potential impacts of the pandemic on the delivery of routine care within the United States (U.S.).1-3 According to the Center for Disease Control (CDC), an estimated 41% of adults in the U.S. have avoided both routine (32%) and urgent (12%) care because of COVID-19-related concerns. 2 Most notably, the COVID-19 pandemic has impacted routine cancer screening, diagnosis, and treatment. 4 Due to CDC recommendations to postpone non-urgent medical care along with general public hesitation to enter medical settings, there has been a precipitous drop in cancer screenings throughout the pandemic.3,5
According to the National Institute of Health (NIH), the top five cancers with the greatest mortality in the U.S. include lung, colon, pancreas, breast, and prostate, in descending order. 6 Of these, routine screenings are recommended for lung, colon, and breast cancers. 7 A recent meta-analysis reported significant decreases in both breast and colon cancer screening compared with pre-pandemic levels. 5 The late detection of these aggressive malignancies may result in worse prognoses and sub-optimal treatment options. 4 For example, if detection of colorectal cancer is delayed, cancer may spread and severely limit treatment options and negatively impact patient outcomes. 4
Recent studies investigating the impact of the COVID-19 pandemic on cancer screening, diagnoses, and mortality have been limited in either their scope or population scale.5,8,9 For example, a recent meta-analysis investigating changes in cancer screening revealed lower rates compared to the pre-pandemic reference year but were limited to small patient registries used to collect the original data. 5 Similarly, other studies investigating new diagnoses or mortality during the pandemic were limited to available EMR records from individual health networks or analyzed trends in only one type of cancer.8,9 There is a need for a more comprehensive investigation to understand the broad impact of the COVID-19 pandemic on cancer screening and care. The aim of this study is to investigate screening, diagnosis, and mortality rates of the top five leading causes of cancer mortality in the U.S. between 2019 and 2021 to determine the potential impact of the COVID-19 pandemic on cancer care.
Methods
Study Design and Population Characteristics
A retrospective cohort study using publicly accessible data reported by the American Cancer Society (ACS) of the estimated diagnostic and mortality rates of the top five leading causes of cancer mortality, as determined by the National Cancer Institute (NCI) (lung/bronchus, colon/rectum, pancreas, breast, and prostate), for the years 2019, 2020, and 2021.4,6 The year 2019 is included as a reference year. Cancer screening data were collected from the United States Healthcare Cost Institute (HCCI) for colon/rectum, breast, and prostate cancer for the years 2019 and 2020. 3 Screening rates were determined by cumulative colonoscopies, mammograms, and prostate-specific antigen (PSA) tests for the years 2019 and 2020. U.S. population statistics were provided by the U.S. Census Bureau and used to calculate incidence rates. 10 Mortality rates were reported as total deaths in 2019, 2020, and 2021.
Data Collection Strategy
The United States Healthcare Cost Institute (HCCI) database was used to evaluate changes in cancer screenings for the years 2019 and 2020 for breast, colorectal, and prostate cancer. 11 Lung/bronchus and pancreatic cancer screenings were not reported in the database. The HCCI is an independent, non-profit research institute that gathers data via clearinghouse records systems, a third-party data collection organization between patients and their insurance providers. 11 The data includes 184 million claims from 30 million patients in 18 different states.
The ACS provided an estimate of the total number of new cancer diagnoses and deaths across the U.S. for the following five leading causes of cancer mortality: lung and bronchus, colon and rectum, pancreas, breast, and prostate.
Statistical Analysis
Microsoft Excel was utilized for statistical analysis. Descriptive statistics (mean and frequency) and percent change were performed to determine the difference in screening, diagnosis, and mortality for the top leading causes of cancer mortality. Percent change for the years 2020 and 2021 was compared to the reference year 2019. The incidence rate ratio was computed via Exact Poisson. Significance was defined as P<.05.
Results
Nationwide Cancer Screening
In 2019, there were an estimated 46,718,350 breast, 22,575,550 colorectal, and 49,014,200 prostate cancer screenings. In 2020, there were an estimated 39,238,200 breast, 17,094,800 colorectal, and 49,713,150 prostate cancer screenings. Compared to 2019, there was a 24.98% decrease in colorectal cancer screening, a 16.01% decrease in breast cancer screening, and a 1.43% increase in prostate cancer screening in 2020 (Figure 1).
Figure 1.
Projected number of colorectal, breast, and prostate cancer screenings during the years 2019 and 2020.
Nationwide Cancer Diagnoses
The number of diagnoses of all the top 5 leading causes of cancer mortality increased each consecutive year from 2019 to 2020 and 2021 (Figure 2). The number of lung/bronchus cancer diagnoses increased from 228,150 in 2019 to 228,820 in 2020 (+.29%) and 235,760 in 2021 (+3.34%). Lung/bronchus cancer had an incidence rate of 69.51/100,000 person-years (PY) in 2019, 69.15/100,000PY in 2020, and 70.91/100,000PY in 2021. The incidence rate of lung/bronchus cancer was 1.02 times greater in 2021 than in 2019 (P < .001).
Figure 2.
Estimated total number of cancer diagnoses of the top five leading causes of cancer mortality for the years 2019, 2020, and 2021. All five leading causes of cancer deaths increased in estimated new diagnoses between 2019 and 2021.
The number of colorectal cancer diagnoses increased from 123,580 in 2019 to 147,950 in 2020 (+19.72%) and 149,500 in 2021 (+20.97%). Colorectal cancer had an incidence rate of 37.54/100,000PY in 2019, 44.71/100,000PY in 2020, and 44.97/100,000PY in 2021. The incidence rate of colon/rectum cancer was 1.19 times greater in 2020 than 2019 (P < .001) and 1.19 times greater in 2021 than 2019 (P < .001).
The number of pancreatic cancer diagnoses increased from 56,770 in 2019 to 57,600 in 2020 (+1.46%) and 60,430 in 2021 (+6.45%). Pancreatic cancer had an incidence rate of 17.30/100,000PY in 2019, 17.41/100,000PY in 2020, and 18.18/100,000PY in 2021. The incidence rate of pancreatic cancer was 1.05 times greater in 2021 than in 2019 (P < .001).
The number of breast cancer diagnoses increased from 271,270 in 2019 to 279,100 in 2020 (+2.89%) and 284,200 in 2021 (+4.77%). The incidence rate of breast cancer was 82.64/100,000PY in 2019, 84.35/100,000PY in 2020, and 85.49/100,000PY in 2021. The incidence rate of breast cancer was 1.02 times greater in 2020 than in 2019 (P < .001) and 1.03 times greater in 2021 than in 2019 (P < .001).
The number of prostatic cancer diagnoses increased from 78,500 in 2019 to 191,930 in 2020 (+144.50%) and 248,530 in 2021 (+216.60%). The incidence of prostate cancer was 23.92/100,000PY in 2019, 58.00/100,000PY in 2020, and 74.76/100,000PY in 2021. The incidence rate of prostatic cancer was 2.43 times greater in 2020 than in 2019 (P < .001) and 3.13 times greater in 2021 than in 2019 (P < .001).
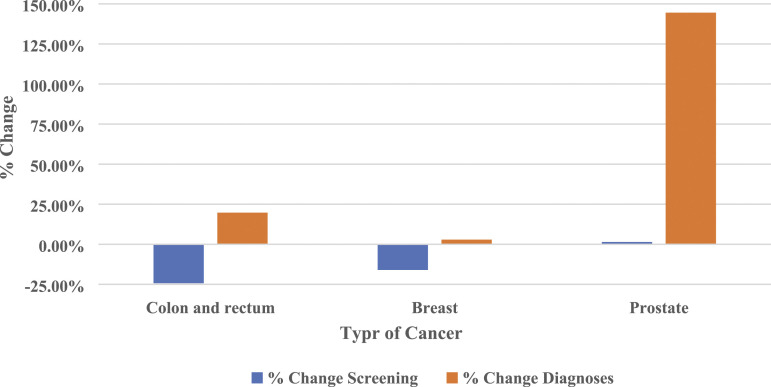
Compared to 2019, there was a .29% increase in lung/bronchus cancer diagnoses, a 19.72% increase in colorectal cancer diagnoses, a 1.46% increase in pancreatic cancer diagnoses, a 2.89% increase in breast cancer diagnoses, and a 144.50% increase in prostate cancer diagnoses in 2020. Compared to the decrease in screening for colorectal and breast cancer, diagnoses for these two cancers increased from 2019 to 2020 (Figure 3).
Figure 3.
Percent change between screening rates and estimated diagnostic rates for colorectal, breast, and prostate cancer for the year 2020 compared to 2019.
Nationwide Cancer Mortality
Four of the top five leading causes of cancer deaths had an estimated increase in the total number of deaths in 2020 and 2021, compared to 2019 (Figure 4). There was an increase in deaths from colorectal cancer from 51,020 in 2019 to 53,200 in 2020 (+4.27%) and 52,980 in 2021 (+3.84%). There was an increase in deaths from pancreatic cancer from 45,750 in 2019 to 47,050 in 2020 (+2.84%) and 48,220 in 2021 (+5.40%). There was an increase in deaths from breast cancer from 42,260 in 2019 to 42,690 in 2020 (+1.02%) and 44,130 in 2021 (+4.42%). There was an increase in deaths from prostate cancer from 31,620 in 2019 to 33,330 in 2020 (+5.41%) and 34,130 in 2021 (+7.94%). There was only a decrease in deaths from lung/bronchus cancer from 142,670 in 2019 to 135,720 in 2020 (−4.87%) and 131,880 in 2021 (−7.56%).
Figure 4.
Estimated total number of cancer deaths for the top five cancers with the highest mortality rate. Colorectal, pancreatic, breast, and prostatic cancers all had an estimated increase in mortality for the years 2020 and 2021, compared to 2019. Lung/bronchus cancer saw a decrease in mortality in 2020 and 2021 compared to 2019.
Four out of the five cancer types showed increases in both new diagnoses and mortality in the years 2020 and 2021, compared to 2019. Only lung and bronchus cancer showed an increase in new cases with a decrease in mortality in the same years. Screening decreased while new diagnoses and mortality increased for colorectal and breast cancer from 2019 to 2020 (Figure 5).
Figure 5.
Percent changes in screening, diagnoses, and mortality in 2020 compared to 2019.
Discussion
This study found a decrease in screening rates by 16.01% and 24.98% for breast and colon cancer, respectively, from 2019 to 2020. All five of the leading causes of cancer mortality (lung/bronchus, colorectal, pancreatic, breast, and prostatic cancer) in the U.S. demonstrated an increase in new diagnoses from 2019 to 2021. Notably, there was a greater increase in diagnoses of prostate, colon, and breast cancer from 2019 to 2020, compared with 2020 to 2021. There was a significant increase of 3.13, 1.19, and 1.03 times the incidence rate of prostate, colon, and breast cancer, respectively, from 2019 to 2021. Correspondingly, there was an increase in mortality from colorectal, pancreas, breast, and prostate cancer from 2019 to 2021.
Our findings indicate that cancer screenings have decreased during the COVID-19 pandemic, supporting the findings of previous studies. A meta-analysis performed by Mayo et al tracked cancer screenings before and during the COVID-19 pandemic, and revealed significantly lower pooled incidence ratios for breast (.63) and colon (.11) cancer screenings during this time. 5 Additionally, a study conducted by Englum et al investigating the rates of cancer screening within the Veterans Affairs Healthcare System during the onset of the pandemic in 2020 found colonoscopies decreased by 45% from 2019. 8 Another study by Patt et al found a precipitous drop in breast, colon, prostate, and lung cancer screenings during 2020 compared with 2019. 12 The findings of our study supports the extensive evidence that cancer screenings have decreased during the COVID-19 pandemic, warranting discussion of rebooting preventive health services during the midst of the ongoing pandemic with special attention to overdue screenings and diagnostic follow-ups.5,8,11,12
The decrease in cancer screening exhibited by our study is likely multifactorial, including widespread closures, financial insecurity and public hesitation to enter medical settings. In 2020, the CDC released a statement recommending postponing non-urgent services including preventive care and screening examinations.3,13 Consequently, many outpatient medical settings experienced closures, particularly in rural areas, creating delays in routine care. 8 Economic pressures from COVID-19 have also left many unemployed and without employer-sponsored health insurance introducing unforeseen challenges to healthcare access. 14 These barriers have continued to persist throughout new outbreaks of COVID-19 variants. 15 While an increase in telehealth services have relatively compensated for some of these challenges, these encounters hinder physical exams, diagnostic tests, and imaging.16,17 Conversely, telehealth services may offer an affordable and efficient platform to conduct some home-based screenings, such as “Cologuard,” to promote colorectal cancer screening despite barriers to colonoscopies. 18
Interestingly, there was an increase in prostate cancer screening from 2020 to 2019. While the literature suggests there has been a uniform decrease in cancer screenings, this finding suggests that the COVID-19 pandemic has had varying impacts on cancer screening tools. PSA tests for prostate cancer were rapidly adopted following the transition to telehealth consultations. 19 During this transition, guidelines were released that discouraged other screening modalities such as digital rectal exams, in accordance with lockdowns and concerns of fecal-oral transmission of COVID-19 infections.20,21 While PSA screenings increased during the pandemic, it is important to note that there have been delays in diagnostic follow-up after a positive screening. 22 This is supported by the increase in prostate cancer diagnoses and corresponding mortality found by our study, indicating that while prostate cancer screenings remain unaffected during the pandemic, subsequent diagnosis and cancer care may have suffered.
We found an increase in the incidence rate for all top five leading causes of cancer deaths in the U.S. from 2019 to 2021. The concurring decrease in cancer screenings during the pandemic likely delayed cancer detection, allowing for pre-cancerous disease progression and more advanced cancer presentations, potentially explaining the increasing cancer diagnoses found by our study.23-26 Contrary to our findings, a cross-sectional analysis found a combined decrease of 46.4% in new weekly cancer diagnoses for breast, colon, lung, pancreatic, gastric, and esophageal cancer in 2020 compared with 2018. 27 The study was conducted utilizing limited EMR records and registries, and our evaluation utilizing the ACS database represents a more comprehensive evaluation of cancer diagnoses across the entire U.S.
Finally, our findings indicate there was an increase in colorectal, breast, prostate, and pancreatic cancer mortality during the pandemic. Considering the rapid progression of some forms of cancer, there have been concerns regarding delays in surgical interventions due to the COVID-19 pandemic. 28 In the midst of the continued healthcare burden from COVID-19, many breast, colon, and prostate cancer surgical interventions have been postponed, even in the setting of aggressive malignancies. 29 These delays likely result from decreased availability of medical equipment, such as ventilators, in order to redirect resources for critical care of COVID-19 patients. 30 Combined with the economic barriers to care and delays in crucial surgical interventions, it is unsurprising that cancer mortality has increased throughout the pandemic.
The findings of our study warrant a discussion of the potential implications of reduced cancer screening and care during the COVID-19 pandemic. According to the World Health Organization (WHO), early cancer care increases the chances of survival and avoids potential treatment complications and subsequent substantial healthcare costs. 31 For example, colon cancer screening procedures such as colonoscopies allow for visualization of pre-cancerous lesions, effectively reducing both colon cancer incidence and mortality. 32 Other screening methods may be conducted through telehealth visits, such as non-invasive fecal immunochemical test (n-FIT), but positive results still require prompt diagnostic follow-up, requiring in-person visits. 33
Similarly, optimal breast cancer screening and diagnostic modalities require the utilization of in-person medical facilities. In contrast to colon cancer screening, less intrusive screening modalities, such as “self-breast exams” are not recommended, limiting opportunities for effective screening during the pandemic. 34 Similarly, the screening and diagnosis of prostate cancers often require physical exams and biopsies for proper staging and treatment guidance. 35
Based on the findings of this study, we offer several recommendations to mitigate the potential negative effects of the COVID-19 pandemic on screening, diagnosis, and mortality for the top 5 leading causes of cancer-related mortality. First, we endorse the suggestions provided by the New England Journal of Medicine to develop clinical registries that notify providers and patients when they are due for preventive services. 36 We also recommend increased distribution of at-home prevention kits (ie, FIT-DNA testing). 36 Subsequently, the development of transport services for pick-up and delivery of patient samples to nearby laboratories may improve compliance with sample collection. 37 Communication systems for diagnostic follow-up after positive screening results should also be strengthened. 38 Additionally, future studies should investigate the stages at which cancers are detected before and during the pandemic to elucidate whether delays in screening have impacted the stage of disease presentation.
Given our findings of increased cancer mortality rates and the scarcity of medical resources throughout the pandemic, we recommend utilizing a triage approach to cancer treatment. This approach was implemented for the management of breast cancer, in order to maximize the number of therapeutic surgeries while minimizing potential exposure to COVID-19. Triage has also been used to identify high-risk patients that may benefit most from at-home FIT tests.9,18 We recommend extending this triage approach to other malignancies where applicable. Furthermore, we advocate for the interprofessional collaboration between hospitals to grant operating privileges to surgeons from nearby medical centers that have been disproportionately impacted by COVID-19 and do not have the adequate resources to perform elective cancer procedures. 39
This study was not without limitations. First, the publicly available data provided by the ACS after the year 2018 included estimates developed from algorithms that may have a multifactorial influence. Second, the cancer screening data was provided by the HCCI database which investigates the electronic medical records of insured patients only, potentially excluding undocumented patients or those who self-pay for their services. Finally, the HCCI database only includes data from 18 states, most of which were predominantly of the western region. Future investigations should investigate the impact of the COVID-19 pandemic on uninsured and vulnerable populations, given that these individuals are often at significant risk for cancer-related disease and mortality.
Conclusion
Our study found decreases in the screening rates for breast and colorectal cancer, along with an increase in the estimated incidence and mortality rate of the five leading causes of cancer deaths from 2019 to 2021. While these changes are likely multifactorial, our findings support the mounting evidence that the COVID-19 pandemic is associated with impaired cancer screening, diagnosis, and care, and further emphasizes the critical need for proactive screening and follow-up to prevent subsequent cancer morbidity and mortality. While screening modalities for some cancers, such as colorectal cancer, can be effectively conducted at home and via telehealth visits, diagnostic follow-up and subsequent treatment have been negatively impacted by the pandemic. Innovative solutions to these unforeseen barriers to cancer screening and care must be implemented to improve cancer detection, treatment, and ultimately patient outcomes during the pandemic.
Footnotes
Author’s contributions: Study design and conception: AE.
Data collection, analysis, and interpretation: JC, SA, MY, and AE.
Manuscript preparation and drafting: JC, MY, SA, KN, TB, JI, and AE.
Critical revisions of the manuscript: JC, MY, SA, KN, TB, JI, and AE.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14(5):965-967. doi: 10.1016/j.dsx.2020.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Czeisler MÉ, Marynak K, Clarke KE, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States. MMWR Morb Mortal Wkly Rep. 2020;69:1250-1257. doi: 10.15585/mmwr.mm6936a4external 10.15585/mmwr.mm6936a4external [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin K, Kurowski D, Given P, Kennedy K, Clayton E. The Impact of COVID-19 on the Use of Preventive Health Care. 2021. Accessed January 6, 2022. https://healthcostinstitute.org/hcci-research/the-impact-of-covid-19-on-the-use-of-preventive-health-care. [Google Scholar]
- 4.American Cancer Society . Cancer facts and statistics. 2022. Accessed January 23, 2022. https://www.cancer.org/research/cancer-facts-statistics.html [Google Scholar]
- 5.Mayo M, Potugari B, Bzeih R, Scheidel C, Carrera C, Shellenberger RA. Cancer screening during the COVID-19 pandemic: A systematic review and meta-analysis. Mayo Clin Proc Innov Qual Outcomes. 2021;5(6):1109-1117. doi: 10.1016/j.mayocpiqo.2021.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Health . Common cancer sites-cancer stat facts. SEER. 2021. Accessed January 17, 2022. https://seer.cancer.gov/statfacts/html/common.html [Google Scholar]
- 7.United States Preventive Services Task Force . Published recommendations. 2022. Accessed January 17, 2022. https://www.uspreventiveservicestaskforce.org/uspstf/topic_search_results?topic_status=P [Google Scholar]
- 8.Englum BR, Prasad NK, Lake RE, Mayorga-Carlin M, Turner DJ, Siddiqui T, et al. Impact of the COVID-19 pandemic on diagnosis of new cancers: A national multicenter study of the veterans affairs healthcare system. Cancer; 2021. doi: 10.1002/cncr.34011 10.1002/cncr.34011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alagoz O, Lowry KP, Kurian AW, et al. Impact of the COVID-19 pandemic on breast cancer mortality in the US: Estimates from collaborative simulation modeling. J Natl Cancer Inst. 2021;113(11):1484-1494. doi: 10.1093/jnci/djab097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.United States Census Bureau . U.S and world population clock; 2022. Accessed January 29, 2022https://www.census.gov/popclock/ [Google Scholar]
- 11.The impact of covid-19 on the use of Preventive Health Care. 2022. HCCI. https://healthcostinstitute.org/hcci-research/the-impact-of-covid-19-on-the-use-of-preventive-health-care. Accessed January 10, 2022 [Google Scholar]
- 12.Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: How the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059-1071. doi: 10.1200/CCI.20.00134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid Services . Non-emergent, elective medical services, and treatment recommendations. 2020. Accessed January 17, 2022. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf [Google Scholar]
- 14.Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19-implications for the health care system. N Engl J Med. 2020;383(15):1483-1488. doi: 10.1056/NEJMsb2021088 [DOI] [PubMed] [Google Scholar]
- 15.American Academy of Family Physicians . Covid-19 continues to cause some people to put off care. 2022. Accessed January 29, 2022. https://www.aafp.org/news/health-of-the-public/20211006delayedcare.html [Google Scholar]
- 16.Cortez C, Mansour O, Qato DM, Stafford RS, Alexander GC. Changes in short-term, long-term, and preventive care delivery in US Office-based and telemedicine visits during the COVID-19 pandemic. JAMA Health Forum. 2021;2(7):e211529. doi: 10.1001/jamahealthforum.2021.1529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Colbert GB, Venegas-Vera AV, Lerma EV. Utility of telemedicine in the COVID-19 era. Rev Cardiovasc Med. 2020;21(4):583-587. doi: 10.31083/j.rcm.2020.04.188 [DOI] [PubMed] [Google Scholar]
- 18.Patel S, Issaka RB, Chen E, Somsouk M. Colorectal cancer screening and COVID-19. Am J Gastroenterol. 2021;116(2):433-434. doi: 10.14309/ajg.0000000000000970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan WS, Wong A, Mahmalji W, Raza A. Is there still a role for digital rectal examination in the prostate cancer diagnostic pathway in the COVID-19 and post COVID-19 era? Aging Male. 2021;24(1):92-94. doi: 10.1080/13685538.2020.1786047 [DOI] [PubMed] [Google Scholar]
- 20.Hindson J. COVID-19: Faecal–oral transmission? Nat Rev Gastroenterol Hepatol. 2020;17:259. doi: 10.1038/s41575-020-0295-7 10.1038/s41575-020-0295-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American cancer society recommendations for prostate cancer early detection. 2022. American Cancer Society. Retrieved from: January 23, 2022. https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/acs-recommendations.html [Google Scholar]
- 22.Obek C, Doganca T, Argun OB, Kural AR. Management of prostate cancer patients during COVID-19 pandemic. Prostate Cancer Prostatic Dis. 2020;23(3):398-406. doi: 10.1038/s41391-020-0258-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Click B, Pinsky PF, Hickey T, Doroudi M, Schoen RE. Association of colonoscopy adenoma findings with long-term colorectal cancer incidence. JAMA. 2018;319(19):2021-2031. doi: 10.1001/jama.2018.5809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D'Ovidio V, Lucidi C, Bruno G, Lisi D, Miglioresi L, Bazuro ME. Impact of COVID-19 pandemic on colorectal cancer screening program. Clin Colorectal Cancer. 2021;20(1):e5-e11. doi: 10.1016/j.clcc.2020.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yong JH, Mainprize JG, Yaffe MJ, et al. The impact of episodic screening interruption: COVID-19 and population-based cancer screening in Canada. J Med Screen. 2021;28(2):100-107. doi: 10.1177/0969141320974711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Haren RM, Delman AM, Turner KM, et al. Impact of the COVID-19 pandemic on lung cancer screening program and subsequent lung cancer. J Am Coll Surg. 2021;232(4):600-605. doi: 10.1016/j.jamcollsurg.2020.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;3(8):e2017267. doi: 10.1001/jamanetworkopen.2020.17267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fu SJ, George EL, Maggio PM, Hawn M, Nazerali R. The consequences of delaying elective surgery: Surgical perspective. Ann Surg. 2020;272(2):e79-e80. doi: 10.1097/SLA.0000000000003998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ProPublica . Cancer surgeries and organ transplants are being put off for coronavirus. Can they wait? 2020. Accessed January 23, 2022. https://www.propublica.org/article/cancer-surgeries-and-open-transplants-are-being-put-off-for-coronavirus-can-they-wait [Google Scholar]
- 30.Richards M, Anderson M, Carter P, et al. The impact of the COVID-19 pandemic on cancer care. Nat Cancer. 2020;1:565-567. doi: 10.1038/s43018-020-0074-y 10.1038/s43018-020-0074-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization . Promoting cancer early diagnosis; 2022. Accessed January 22, 2022. https://www.who.int/activities/promoting-cancer-early-diagnosis [Google Scholar]
- 32.Holme Ø, Bretthauer M, Fretheim A, Odgaard-Jensen J, Hoff G. Flexible sigmoidoscopy versus faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst Rev. 2013;9:CD009259. doi: 10.1002/14651858.CD009259.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zorzi M, Battagello J, Selby K, et al. Non-compliance with colonoscopy after a positive faecal immunochemical test doubles the risk of dying from colorectal cancer. Gut. 2021;71:561-567. gutjnl-2020-322192. doi: 10.1136/gutjnl-2020-322192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Cancer Society . Breast cancer screening guidelines faqs: FAQ breast cancer. 2022. Accessed January 17, 2022. https://www.cancer.org/cancer/breast-cancer/frequently-asked-questions-about-the-american-cancer-society-new-breast-cancer-screening-guideline.htmlhttps://www.cancer.org/cancer/breast-cancer/frequently-asked-questions-about-the-american-cancer-society-new-breast-cancer-screening-guideline.html
- 35.Litwin MS, Tan HJ. The diagnosis and treatment of prostate cancer: A review. JAMA. 2017;317(24):2532-2542. doi: 10.1001/jama.2017.7248 [DOI] [PubMed] [Google Scholar]
- 36.Horn DM, Haas JS. Covid-19 and the mandate to redefine preventive care. N Engl J Med. 2020;383(16):1505-1507. doi: 10.1056/NEJMp2018749 [DOI] [PubMed] [Google Scholar]
- 37.Randel KR, Schult AL, Botteri E, et al. Colorectal cancer screening with repeated fecal immunochemical test versus sigmoidoscopy: Baseline results from a randomized trial. Gastroenterology. 2021;160(4):1085-1096. e5. doi: 10.1053/j.gastro.2020.11.037 [DOI] [PubMed] [Google Scholar]
- 38.Selby K, Senore C, Wong M, May FP, Gupta S, Liang PS. Interventions to ensure follow-up of positive fecal immunochemical tests: An international survey of screening programs. J Med Screen. 2021;28(1):51-53. doi: 10.1177/0969141320904977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ji C, Singh K, Luther AZ, Agrawal A. Is elective cancer surgery safe during the COVID-19 pandemic? World J Surg. 2020;44(10):3207-3211. doi: 10.1007/s00268-020-05720-x [DOI] [PMC free article] [PubMed] [Google Scholar]