Abstract
Background
Gallbladder agenesis is an extremely rare congenital condition in which most patients will remain asymptomatic; nonetheless, a small subset of patients will mimic biliary, urinary, or gastrointestinal disorders. As a result, if these patients are unaware of their condition, an ultrasound may be needed when they present with right upper abdominal pain, which can be misleading or inconclusive, putting the surgeon and the medical team in a diagnostic and intraoperative dilemma.
Case presentation
We present the case of a 36-year-old woman with a history of ventricular septal defect and cleft palate. She presented with abdominal pain to the emergency department. After an ultrasound, cholecystitis was misdiagnosed, and, unfortunately, the medical team did not realize this mistake. As a result, surgery was decided. After additional tests, gallbladder agenesis was diagnosed, and the patient fully recovered.
Clinical discussion
Congenital absence of the gallbladder can often pose a dilemma to surgeons when it is diagnosed during surgery. Preoperative diagnosis is highly challenging as it can mimic other pathologies; therefore, the medical team needs to keep this pathology on their list of differential diagnoses to avoid dangerous procedures.
Conclusions
Congenital absence of the gallbladder can often pose a dilemma to surgeons when it is diagnosed during laparoscopic cholecystectomy. Since preoperative diagnosis is challenging, communication between radiologists and surgeons is critical in order to provide proper care for any patient.
Keywords: Gallbladder, Biliary agenesis, Laparoscopic
Highlights
-
•
Misdiagnosis can occur and it's our duty as physicians to learn from these mistakes.
-
•
Gallbladder agenesis is a rare pathology that must always be among our differentials.
-
•
Congenital absence of the gallbladder can often pose a dilemma to surgeons when it is diagnosed during surgery.
1. Introduction
Gallbladder agenesis is a rare, often asymptomatic, anomaly of the biliary tract [1,2]. However, few patients may present clinically indistinguishable symptoms from other gastrointestinal or urinary pathologies or even from an excluded or atrophic gallbladder; these patients are believed to have a hypertonic biliary sphincter, which would lead to biliary dyskinesia and even choledocholithiasis. [2,3] This can be worsened in developing countries like Ecuador, where healthcare personnel were already weary and flooded in work even in the absence of a pandemic [4,5]. Medical errors will continue to appear, leading to an incorrect preoperative diagnosis and exposing patients to unnecessary surgical procedures. [1,4]
We present the case of a 36-year-old patient with a history of ventricular septal defect and cleft palate in which cholecystitis was misdiagnosed. During surgery, the gallbladder was nowhere to be found. Gallbladder agenesis was suspected and then confirmed in the postoperative period.
This work has been reported in line with the SCARE 2020 criteria [6].
2. Case report
The patient is a 36-year-old woman with a past medical history of ventricular septal defect and cleft palate. She presented to the emergency room with a 2-year history of upper abdominal pain predominantly after eating. At first, the pain was mild; therefore, she did not seek any treatment; however, one week prior to admission, she presented with nausea, asthenia, and fever; thus, her family brought her to the hospital.
On clinical examination, a tachycardic patient with abdominal tenderness in her upper abdomen was identified; Murphy's sign was not present at the time, and she did not have any clinical features of biliary obstruction, including pale stools or jaundice.
Complementary exams revealed leukocytosis, neutrophilia, and an elevated C-reactive protein. Bilirubin, amylase, aspartate aminotransferase, and gamma-glutamyl transferase were normal (Table 1).
Table 1.
Laboratory values of the patient.
| Exam | Value | Range |
|---|---|---|
| White Blood Count (cell/mm3) | 15 | 4.00–11.0 |
| Hb (g/dl) | 13 | 11.5–16 |
| Neutrophils (%) | 78 | 33–64 |
| C-reactive protein (mg/dL) | 10 | 0.8–1.0 |
| Bilirubin (mg/dL) | 1 | 0.2–1.2 |
| Amylase (U/L) | 55 | 40–140 |
| Aspartate aminotransferase U/L | 30 | 0–35 |
| Gamma-glutamyl transferase (U/L) | 25 | 0–40 |
Due to this, an abdominal ultrasound was requested. Unfortunately, as this case happened during midnight, the sonogram was performed by a resident and not an attending due to the limited resources in the hospital. Regretfully, he misinterpreted the images and reported a small gallbladder with an apparent small gallstone and diffuse gallbladder wall thickening. Bile ducts were normal and not dilated. (Fig. 1). Thus, cholecystitis and acute abdomen were suspected.
Fig. 1.
Ultrasound with equivocal diagnosis of cholecystitis.
With these findings, surgical consultation was needed. The on-call surgeon assessed the patient with right upper abdominal pain, leukocytosis, and an incorrect echography report. Without seeing the ultrasound images and relying solely on the information at hand, cholecystitis was misdiagnosed, and surgery was decided.
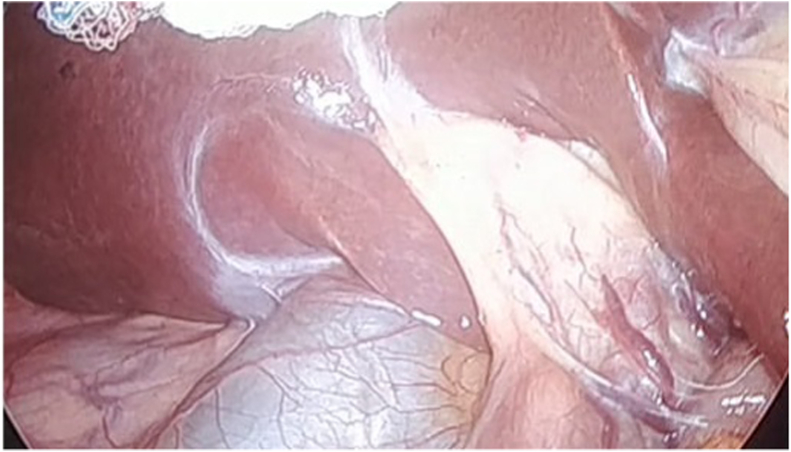
During laparoscopy, the liver and duodenum appeared normal without adhesions, yet the gallbladder was nowhere to be seen. The bile ducts were recognized, and after a thorough examination of the abdominal cavity, the gallbladder was not identified; therefore, the procedure was concluded to avoid any injury (Fig. 2A, Fig. 2BA and B).
Fig. 2A.
Transoperative view of the left and right hepatic ducts.
Fig. 2B.
Transoperatvie view of absence of gallbladder.
On her postoperative period, an abdominal computed tomography was requested since magnetic resonance cholangiopancreatography was not available at that time. The liver appeared normal, and the gallbladder was absent. Slight inflammation around the perirenal fat was also recognized (Fig. 3A).
Fig. 3.
A: Abdominal CT, with absence of gallbladder.
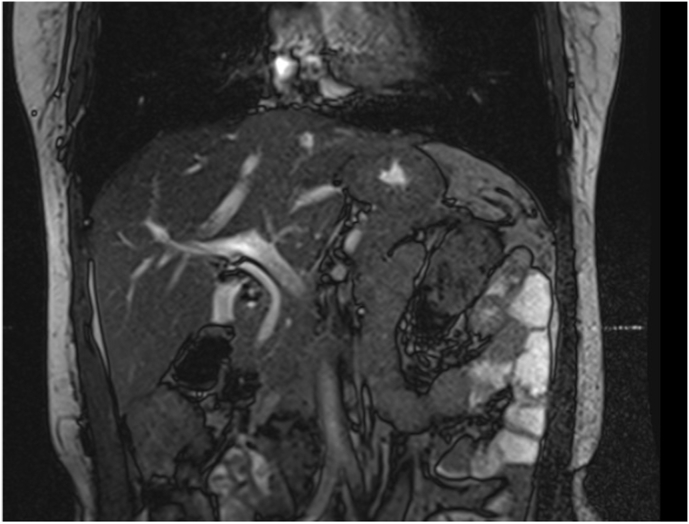
Due to this discrepancy, a magnetic resonance cholangiopancreatography confirmed what was presumed; agenesis of the gallbladder without extrahepatic biliary atresia (Fig. 4A, Fig. 4BA and B). Additional assessment confirmed pyelonephritis and was successfully treated. She was informed of her rare condition and discharged without complications. On follow-ups, she is doing ok.
Fig. 4A.
MRCP reconstruction of the biliary tree without gallbladder.
Fig. 4B.
MRCP, the right and left hepatic ducts are seen, but the gallbladder is absent.
3. Discussion
Lemery first reported agenesis of the gallbladder without extrahepatic atresia in 1701, and since then, less than 500 cases have been reported in the literature [1,2]. It is an extremely rare pathology (0.01 to 0.06% of the adult population) that can occur alone (70–87% of cases) or associated with other anomalies (30%). The etiology is still under research, but it is generally accepted as a congenital malformation. [1,3] Nevertheless, gallbladder agenesis has been associated with many other gastrointestinal, skeletal, cardiovascular, and genitourinary malformations. [2,3] In our case, the patient had multiple malformations treated during her infancy.
Gallbladder agenesis is believed to occur from the failure of the gallbladder bud to develop or failure of the partially formed gallbladder to recanalize during intrauterine life [[1], [2], [3]].
Clinical presentations are varied; most patients will remain asymptomatic and live a normal life, yet, about 20% of patients will develop symptoms clinically indistinguishable from other gastrointestinal or renal disorders, such as right-upper abdominal pain dyspepsia, biliary colic, and sometimes even jaundice [[7], [8], [9]].
The reason why this subgroup of patients experiences pain, nausea, jaundice, and other symptoms is not yet fully understood; nonetheless, previous medical experience in postcholecystectomy syndrome has led to believe that these patients experience a syndrome similar to biliary dyskinesia [1,7]. Additional analyses have demonstrated that the ampullary sphincter contraction in these patients is greater than in normal subjects, leading to an increased risk of choledocholithiasis [8,10]. When the diagnosis is made transoperative, it has a 3:1 female predominance, probably because the diagnosis of cholelithiasis is more common in women. [9,10] As it was found in our patient.
Preoperative diagnosis is now more straightforward since ultrasound, abdominal CT, MRCP, and laparoscopy are now broadly available, yet oversights can still occur. [1,10] After clinical examination, ultrasonography is the usual starting point for diagnosing biliary tract disease (95% sensitivity for cholelithiasis); nevertheless, given the rarity of gallbladder agenesis and the fact that this test is operator-dependent, many radiologists might doubt if they do not find the gallbladder and might mistake it with a shrunken gallbladder or porcelain gallbladder. [1,11] As it happened in our case.
Thus, if doubts exist, further investigations are required, such as radioisotope hepatobiliary scan, MRCP, or CT, to confirm the diagnosis and avoid unnecessary surgeries [1,12]. Despite this, surgery in patients with gallbladder agenesis happens when there is a complaint of biliary symptoms along with a false-positive US study [2,13]. As it occurred in our patient.
If the diagnosis occurs during surgery, the surgeon should first look for ectopics gallbladders (intrahepatic, lesser omentum, retroperitoneum, retrohepatic retroduodenal, or retropancreatic), if unable to identify them; intraoperative cholangiography may be reasonable; however, exhaustive surgical exploration of the extrahepatic bile ducts is not necessary, and additional testing in the postoperative period should be pursued to confirm the diagnosis or help in further preoperative planning if required [1,3,14].
In our case, as the gallbladder could not be identified and to avoid other risks, surgery was completed, and complementary tests were requested.
Given the rarity of this condition, when there is a report of an absent gallbladder or doubts exist about the patient's condition, the medical team must consistently have open communication to avoid exposing the patient to unnecessary surgery [1,13]. In addition, whenever the gallbladder is improperly seen in routine imaging methods, gallbladder agenesis should be kept in mind [1,15].
Medical errors are strongly related to communication breakdowns [4,5]. Hospital staff works hard, long hours, and regularly faces life-and-death situations [4]. Therefore, communication between healthcare professionals is essential to provide adequate care to any patient [4,5]. However, there is a fine line separating dedication from overwork; if unchecked, overwork could lead to counterproductive effects that may affect patient care [5].
4. Conclusion
Congenital absence of the gallbladder can often pose a dilemma to surgeons when it is diagnosed during surgery. Preoperative diagnosis is highly challenging as it can mimic other pathologies; therefore, surgeons and radiologists need to keep this pathology on their list of differential diagnoses to avoid dangerous procedures.
This case also proves that despite its virtues, a career in medicine will bring significant challenges that could lead to considerable emotional distress for any healthcare worker; there is no single formula to overcome these personal and professional difficulties. Nevertheless, all personnel needs to be alert, motivated, and above all, use these rare cases not as punishable offenses but as educational opportunities that will allow us to provide our patients with the best available care.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Patient perspective
At first, the patient was scared about her treatment, whether it would hurt, and whether she could be “ok” nonetheless since surgery was successful, she was grateful to the medical team.
Conflicts of interest
We declare no conflict of interest.
Sources of funding
None.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors and has been approved by the ethics committee of our hospital.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
GM and AA analyzed and interpreted the patient data and did the surgical treatment. AA, GJ & AC was a major contributor in writing the manuscript. EP prepared the figures. AJ y PR revised the manuscript and reviewed all the available data. All authors read and approved the final manuscript.
Registration of research studies
1. NA.
Guarantor
G. A. M. MD, Attending Surgeon at Hospital IESS Quito Sur & Universidad San Francisco de Quito gabomolina32@gmail.com.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103585.
Contributor Information
Gabriel A. Molina, Email: gabomolina32@gmail.com.
Andres V. Ayala, Email: andres_pojkar@hotmail.com.
Alberto C. Arcia, Email: alberto-andrea@hotmail.com.
Galo E. Jiménez, Email: galojimenez1981@yahoo.com.
Estefany J. Proaño, Email: estefany.jp9@gmail.com.
C. Augusto Cadena, Email: augusto94.ac@gmail.com.
Andres Jimenez, Email: andresitosebas@hotmail.com.
Paula M. Raza, Email: paularaza16@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Bani-Hani K.E. Agenesis of the gallbladder: difficulties in management. J. Gastroenterol. Hepatol. 2005;20(5):671–675. doi: 10.1111/j.1440-1746.2005.03740.x. [DOI] [PubMed] [Google Scholar]
- 2.Kabiri H., Domingo O., Tzarnas C. Agenesis of the gallbladder. Curr. Surg. 2006;63(2):104–106. doi: 10.1016/j.cursur.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Frey C., Bizer L., Ernst C. Agenesis of the gallbladder. Am. J. Surg. 1967;114(6):917–926. doi: 10.1016/0002-9610(67)90418-7. [DOI] [PubMed] [Google Scholar]
- 4.Crijns T.J., Kortlever J.T.P., Guitton T.G., Ring D., Barron G.C. Symptoms of burnout among surgeons are correlated with a higher incidence of perceived medical errors. HSS J. 2020;16(Suppl 2):305–310. doi: 10.1007/s11420-019-09727-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clapper T., Ching K. Debunking the myth that the majority of medical errors are attributed to communication. Med. Educ. 2019;54(1):74–81. doi: 10.1111/medu.13821. [DOI] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Bennion R.S., Thompson J.E., Jr., Tompkins R.K. Agenesis of the gallbladder without extrahepatic biliary atresia. Arch. Surg. 1988;123(10):1257–1260. doi: 10.1001/archsurg.1988.01400340083014. [DOI] [PubMed] [Google Scholar]
- 8.Salazar M.C., Brownson K.E., Nadzam G.S., Duffy A., Roberts K.E. Gallbladder agenesis: a case report. Yale J. Biol. Med. 2018;91(3):237–241. Published 2018 Sep 21. [PMC free article] [PubMed] [Google Scholar]
- 9.Gotohda N., Itano S., Horiki S., et al. Gallbladder agenesis with no other biliary tract abnormality: report of a case and review of the literature. J. Hepatobiliary Pancreat Surg. 2000;7(3):327–330. doi: 10.1007/s005340070057. [DOI] [PubMed] [Google Scholar]
- 10.Malde S. Gallbladder agenesis diagnosed intra-operatively: a case report. J. Med. Case Rep. 2010;4:285. doi: 10.1186/1752-1947-4-285. Published 2010 Aug 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pérez Moreiras M., Couselo Villanueva J., Maseda Díaz O., Arija Val F. Una verdadera agenesia vesicular. Cirugía Española. 2007;82(4):246–247. doi: 10.1016/s0009-739x(07)71719-0. [DOI] [PubMed] [Google Scholar]
- 12.Balakrishnan S., Singhal T., Grandy-Smith S., El-Hasani S. Agenesis of the gallbladder: lessons to learn. J. Soc. Laparoendosc. Surg. : J. Soc. Laparoendosc. Surg. 2006;10(4):517–519. [PMC free article] [PubMed] [Google Scholar]
- 13.Castorina S., Scilletta R., Domergue J. Gallbladder agenesis: laparoscopic views of a significant diagnostic challenge. Surg. Radiol. Anat. 2014;36(6):619–620. doi: 10.1007/s00276-014-1263-0. [DOI] [PubMed] [Google Scholar]
- 14.Watemberg S., Rahmani H., Avrahami R., Nudelman I.L., Deutsch A.A. Agenesis of the gallbladder found at laparoscopy for cholecystectomy: an unpleasant surprise. Am. J. Gastroenterol. 1995;90(6):1020–1021. [PubMed] [Google Scholar]
- 15.Peloponissios N., Gillet M., Cavin R., Halkic N. Agenesis of the gallbladder: a dangerously misdiagnosed malformation. World J. Gastroenterol. 2005;11(39):6228–6231. doi: 10.3748/wjg.v11.i39.6228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.