Abstract
Objective
to determine the clinical presentations and histopathological findings of idiopathic granulomatous mastitis, and to evaluate clinical outcomes after management.
Methods
between 2007 and 2021, the files and histopathology reports of 17 patients with idiopathic granulomatous mastitis at Tishreen University Hospital, Latakia, Syria were reviewed. The data were analyzed and a scan through relevant literature was carried out to review related cases.
Results
the age of patients ranged from 23 years to 57 years, and the mean age was 37.2 ± 9.57 years. All patients were female. The most common clinical presentation was breast lumps and the most common mammographic finding was ill-defined masses, which mimics breast carcinoma. Multinucleated giant cells, polymorphonuclear leukocytes, lipogranuloma-like changes and lobulocentric abscesses were the most common histopathological findings. Treatment options include: drainage of abscess along with antibiotics, steroid administration, and surgical excision. Antibiotic treatment was associated with a higher rate of complications, while use of steroids showed complete remission of the disease.
Conclusion
idiopathic granulomatous mastitis is a spectrum of entities that should be differentiated from breast carcinoma and other mastitis conditions, the infectious or the non-infectious ones. The clinical and radiological features resemble those of breast carcinoma and infectious mastitis. The histopathological study is considered as the most crucial element in the multidisciplinary approach to diagnose idiopathic granulomatous mastitis (IGM) and determine the optimal management to be administered.
Keywords: Granulomatous mastitis, Idiopathic granulomatous mastitis, Breast, Mastitis
Highlights
-
•
Granulomatous mastitis (GM) represents a diagnostic and therapeutic challenge.
-
•
Idiopathic granulomatous mastitis is a spectrum of entities that should be differentiated from breast carcinoma and other mastitis conditions.
-
•
The histopathological study is considered as the most crucial element in the multidisciplinary approach to diagnose idiopathic granulomatous mastitis (IGM).
1. Introduction
Granulomatous Mastitis (GM) is a rare benign breast lesion that represents a wide spectrum of entities [1,2]. It is totally essential to distinguish between two main types of GM, the specific (secondary) granulomatous mastitis which occurs as a result of a well-defined cause, and the idiopathic granulomatous mastitis (IGM) which mainly affects women in childbearing age with an incidence between 0.44 and 1.6% of total breast biopsy specimens [[3], [4], [5]]. Since it was first reported in 1972 by Kessler and Wollock, IGM poses a diagnostic and therapeutic challenge [1]. IGM shows various manifestations that may mimic breast carcinomas [1,2,6]. Mostly, IGM presents with a unilateral palpable breast lump that can cause later skin alterations with or without lymphadenopathy [1,2,6]. However, some cases of bilateral lumps were reported [2]. The diagnosis of IGM is established by ruling out other infectious, malignant, and auto-immune pathogenesis. Moreover, No radiological techniques can confirm the diagnosis, besides the real benefit of laboratory tests is only to exclude other differential diagnoses [7]. Hence, the histopathological study is considered the cornerstone in confirming diagnosis and determining the optimal management that should be administered [7]. With the absence of a definite treatment algorithm, management of IGM varies from conservative treatment including observation, antibiotics, steroids and methotrexate to surgery [4,8]. This study was designed to review the clinical presentation and pathological findings of this clinical entity in a series of 17 cases diagnosed in our hospital and to discuss relevant cases published in the literature.
2. Methods
In this retrospective analysis, the records of 17 patients diagnosed with granulomatous mastitis at Tishreen University Hospital, Latakia, Syria, between 2007 and 2021 were reviewed. Collected data include the patient's demography, clinical presentation, laboratory, mammographic and pathological findings. A definitive diagnosis was obtained by an open excisional and tru-cut needle biopsy. All microscopic slides were reviewed. The histochemical stains, Ziehl-Neelsen stain for acid-fast bacilli (AFB), and periodic acid-Schiff (PAS) stain were also revised.
3. Results
The age of patients ranged from 23 to 57 years with a mean of 37.2 ± 9.57 years. All patients were female. In 7 cases (41%), the most frequent complaint at presentation was a palpable lump; followed by axillary lymphadenopathy in 6 cases (35%), breast pain in 5 cases (29%), nipple discharge in 3 cases (18%), and sinus tract in 2 cases (12%). Size of the lesions ranged from 2 to 11 cm; with a mean of 4.9 ± 2.2 cm. At presentation, 2 patients were pregnant and one was a breastfeeding mother. Neither history of smoking nor concurrent systemic findings was reported in all cases. Of the lesions, 7 (41%) were in the left breast and 8 (47%) were in the right breast. 2 (11%) lesions were bilateral. Involvement was limited to the upper external quadrant in 7 cases (41%), upper internal quadrant in 1 case (5%), and central area in 9 cases (54%). Mammographic examination showed an ill-defined mass in 12 patients (70%), and an irregular asymmetric density in 5 patients (30%). 7 out of the 17 cases (41%) had a clinical impression of a not otherwise specified (NOS) breast mass. In 5 cases (30%), breast carcinoma was suspected. The clinical impression of the other lesions was fibrocystic changes. On pathological examination, gross appearance showed an irregular, nodular, gray-tan, and firm mass, (Fig. 1). Microscopic features showed multinucleated giant cells in all cases (100%), lobulocentric abscesses in 9 cases (53%), lipogranuloma-like findings in 9 cases(53%), polymorphonuclear leukocytes in 12 cases (71%), and necrosis in 3 cases (17%), as shown in (Fig. 2). The histochemical stains for AFB and fungus were negative in all cases, (Fig. 3). Five patients (30%) were treated with abscess drainage and antibiotics, 6 patients (35%) were treated with steroids, 5 patients (30%) had surgical excision, and only one patient had spontaneous remission of the mass. Of the surgical excision-treated patients, one had recurrence of the lesion. Moreover, relapse was reported in 3 of the incision and drainage patients, (Table 1).
Fig. 1.
a, b: gross features of idiopathic granulomatous mastitis, the cut surface of the breast lumps shows irregular, gray-tan firm masses with nodularity.c, d: the cut section shows ill-defined nodules with foci of necrosis & abscess formation.
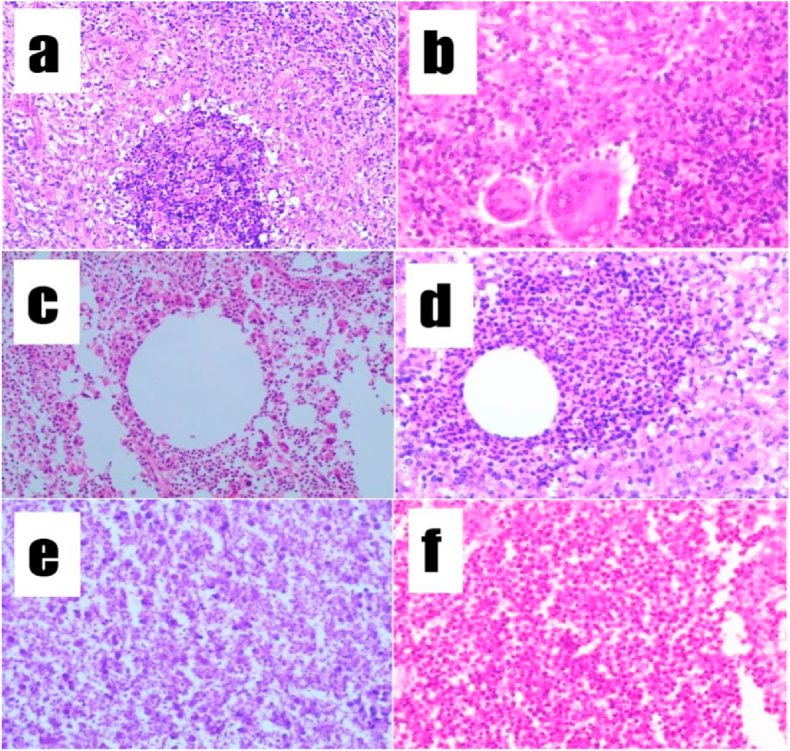
Fig. 2.
microscopic features of IGM:
a: lobulocentric abscesses (hematoxylin and eosin staining x
100). b: multinucleated giant cells (hematoxylin and eosin staining × 200). c,d: lipogranuloma-like changes (hematoxylin and eosin staining x100). e: necrosis (hematoxylin and eosin staining × 200). f: neutrophils (hematoxylin and eosin staining x100).
Fig. 3.
microscopic features for special stains show:
a,b: negativity of Ziehl-Neelsen stain for acid-fast bacilli (
AFB). c,d: negativity of periodic acid-Schiff (PAS) for fungal infection.
Table 1.
Shows the general characteristics of the revised cases.
| Findings | Number of cases, total number: 17 cases | |
|---|---|---|
| Gender | Female | 17 |
| Male | 0 | |
| Age | Less than 25 years | 1 |
| {25 → 45} years | 12 | |
| More than 45 years | 4 | |
| Side | Left breast | 7 |
| Right breast | 8 | |
| Bilateral | 2 | |
| Location | Upper internal quadrant | 1 |
| Upper external quadrant | 7 | |
| Central | 9 | |
| Mammographic examination | Ill-defined mass | 12 |
| Irregular asymmetric density | 5 | |
| Clinical impression | not otherwise specified (NOS) breast mass | 7 |
| Carcinoma | 5 | |
| Fibrocystic changes | 5 | |
| Presenting symptoms | Breast palpable lump | 7 |
| Axillary lymphadenopathy | 6 | |
| Breast pain | 5 | |
| Nipple discharge | 3 | |
| Sinus tract | 2 | |
| Pathological parameters | Lobulocentric abscesses | 9 |
| Lipogranuloma-like changes | 9 | |
| Polymorphonuclear leukocytes | 12 | |
| Multinucleated giant cells | 17 | |
| Necrosis | 3 | |
| Treatment | Drainage of abscess along with antibiotics | 5 |
| Steroid administration | 6 | |
| Surgical excision | 5 | |
| Spontaneous remission | 1 | |
4. Discussion
GM is a rare benign breast lesion that was first defined by Kessler and Wollock in 1972 [1]. Later, there was a tendency to categorize GM into two main types in terms of etiology: specific and idiopathic [3,4]. Specific granulomatous mastitis occurs due to infectious reasons (tuberculosis, leprosy, syphilis, cat scratch disease, histoplasmosis, cryptococcosis, schistosomiasis, fungal or parasitic infection) or noninfectious reasons that vary between systemic diseases (sarcoidosis, diabetes mellitus, Crohn's disease, systemic lupus erythematosus, or vasculitis such as Wegner's granulomatosis, giant cell arteritis, Takayasu's arteritis, and Churg-Strauss syndrome), and breast-localized disorders (fat necrosis, ductal ectasia or foreign body reaction like silicone implants) [3,4,9,10].
Idiopathic Granulomatous Mastitis, as the name indicates, has no clear etiology so far. IGM Diagnosis poses a dilemma, as it depends on exclusion; with an average delay in diagnosis of about 4–5 months [10,11]. Many etiological hypotheses have been postulated in the literature [5,10].
Autoimmunity is the most acceptable one [8,10], as it is supported by some key facts: the premium response to steroids and immunosuppressive agents, with great improvement in patients who had recurrence after surgical excision, and the predominance of T-lymphocytes revealed by histochemical studies. Furthermore, some IGM patients experienced concurrent systemic findings like arthritis and erythema nodosum which were not reported in our patients [3,8,10].
Pregnancy, lactation, and use of oral contraceptive pills (OCP) are the most controversial risk factors discussed among medical reporters, in spite of only three patients in our series were among these categories. Some authors presumed that milk stasis caused by the aforementioned conditions leads to micro-ruptures in mammary ducts resulting in milk extravasation into the interstitial tissue which, in turn, induces an inflammatory process. This could explain the preponderance of women of childbearing age with a history of gestation, lactation, and OCP usage among the patients. However, this relationship is still controversial due to the cases of IGM occurrence in men and nulliparous women, in addition to reports with no history of OCP intake, as most of our cases [2,3,7,8,10].
Smoking, alpha 1-antitrypsin deficiency, galactorrhea, hyperprolactinemia, and antipsychotic medications are additional factors that are claimed to trigger an inflammatory process in the breast [2,3,7,8,10]. Smoking is presumed to be a causative factor to develop the injury into bilateral and delay healing process [2]. However, to date no definitive correlation has been demonstrated between IGM and any of the previously mentioned factors [2,3,7,8,10], as we can see that no history of smoking was reported in our cases. Another causative factor that should be estimated is infection with Corynebacterium. These lipophilic gram-positive bacilli, which exist as normal skin flora, were first isolated within IGM patients in 2002. Thenceforward, many reports presumed a possible correlation between IGM and the most identified species: Corynebacterium kroppenstedtii, Corynebacterium amycolatum, and Corynebacterium tuberculostearicum. On the other hand, infection with Corynebacterium could be misdiagnosed in many cases of IGM because of insufficient routine tests that show the gram-positive bacilli [3,7,8,10]. Recently, a term of “Cystic Neutrophilic Granulomatous Mastitis” has been evolved to define breast infection with Corynebacterium species as a subtype of GM with a distinct entity. This aims to avoid misguided therapy and achieve optimal treatment [7,11]. Hitherto, no ethnic predisposition has been established [5,7,12]. Nonetheless, many studies link the augmentation of reports from Mediterranean countries and the Middle East to underdiagnosing tuberculosis. Hence, performing Ziehl Neelsen stain for AFB, which was negative in our series, is essential especially in endemic regions because steroids, the mainstay treatment in IGM, aggravate tuberculosis (TB) [2,12,13].
IGM can occur at variable ages starting from 11 to 87 years [2,3]. The predominance of occurrence is in women of childbearing age between the 3rd and 4th decades. Mean age of 36 years was identified in a review of 3060 patients which is consistent with our case series (37 years) [5]. Very few cases of men with IGM were reported as well [7]. In regards to clinical manifestations, the most common presentation-as also shown in our case series-is a palpable lump, frequently unilateral and in a few cases bilateral [2]. The mass can be located in any quadrant of the breast but usually, the upper lateral quadrant and retro-areolar region are the most involved areas, the same as what we are reporting in our series [5]. Cases of multiple unilateral small lumps were reported, too [13]. Axillary lymphadenopathy, pain, oedema, breast asymmetry, nipple inversion, nipple discharge, and skin alterations like ulceration and peau d'orange sign are common symptoms as well [7,8,10]. The chronic presentation includes sinus and fistula formation [7,8,10]. Erythema nodosum and arthritis are considered to be concurrent systemic manifestations [7]. Breast carcinoma and inflammatory breast carcinoma are the first clinical impression occasionally, resulting in the patient experiencing serious anxiety and depression during the time of investigation, until the final diagnosis is established [2].
IGM Diagnosis poses a dilemma, as it depends on exclusion; with an average delay in diagnosis of about 4–5 months [5,8]. IGM is radiologically indeterminate, but radiography must be performed to distinguish it from other breast diseases [7]. Mammography shows irregular lumps or nodules with asymmetry between parenchyma and focal density. In some cases, some changes are observed, such as enlarged lymph nodes and inversion of the nipple. Ultrasound is the best method used as it shows in more than 80% of cases the presence of a heterogeneous hypo-echoic lesion, and this method is the most widely used to evaluate and follow up the case. MRI is not routinely used, except for assessing the extent of disease when cancer is suspected [6,7].
Histopathology demonstrates an increase in leukocytes, granulomatous lobulitis, accompanied by necrosis plus multinucleated giant cells [6]. Although it is believed that there is a role for genetic factors, there is no confirmation of this statement [4]. A definitive diagnosis of IGM depends on histopathology. Studies have shown the low sensitivity of fine needle aspiration (FNA) which diagnoses only 21% of cases, and must be often followed by a core needle biopsy, which has the highest diagnostic yield of 94%. As a core needle biopsy may fail in the diagnosis of IGM, an open biopsy is indicated, which may cause scarring, non-healing ulcers, or sinus tracts [8,10]. Macroscopic examination reveals an irregular, gray-tan firm mass with nodularity [4]. Microscopic examination demonstrates non-caseating granuloma with epithelioid histiocytes, multinucleated giant cells, plasma cells, lymphocytes, neutrophils, and eosinophils within and around lobules. Necrosis, fibrosis, and microabscess formation are sometimes seen [12]. The aforementioned microscopic features go with our microscopic ones that have been previously discussed in details. Absence of any microorganisms seen on staining for bacteria and fungi rules out infectious granulomas. Caseous necrosis is not present which rules out tuberculosis [10].
There is no consensus on the treatment algorithm for IGM, but a wide spectrum of treatment options, including observation, antibiotics, steroids, methotrexate, and surgery is suggested [7,8,10]. 50% of cases developed chronic course, recurrence, and complications. However, the others achieved uneventful recovery without any specific therapeutic intervention [8,10,14]. Using antibiotics is controversial, as there is no microbiological proof of a bacterial infection in IGM. Steroid therapy reduces the size of the lesion but also leads to side effects including obesity, hypertension, glucose intolerance, and Cushing's syndrome. In cases that are resistant to steroids, methotrexate or surgery would be indicated [7,8,10]. Surgery should be the last option in order to avoid invasive therapies and complications like breastfeeding problems, scars, asymmetry, and unsatisfactory esthetics. The recurrence rate in steroid therapy is 20%, however, it is 4–6.8% in surgery alone or along with steroids [7]. Finally, we have to mention that this work has been reported in line with the PROCESS 2020 criteria [15].
5. Conclusion
Overall, IGM is a spectrum of entities that has received more attention in recent years to define its characteristics in terms of avoiding unnecessary investigations and misguided therapy. A wide spectrum of diseases should be considered and ruled out before diagnosing IGM including breast carcinoma. SO far, histopathological study is still considered to be the most valuable investigation. Ziehl Neelsen stain and PAS stain ought to be performed to all specimens to exclude TB and fungal infections. Management of IGM poses a significant challenge to specialists as it is still controversial. In this manuscript, we aimed to present a series of 17 cases of IGM from Syria, highlighting the crucial role of histopathological examination to confirm the diagnosis, due to the importance of both early diagnosis and management to avoid its complications.
Ethical approval
Not applicable.
Sources of funding
None.
Author contribution
All authors contributed in all the phases of preparing the paper.
Registration of research studies
Researchregistry7602.
Guarantor
Amjad Soltany, M.D.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103587.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kessler E., Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am. J. Clin. Pathol. 1972;58(6):642–646. doi: 10.1093/ajcp/58.6.642. [DOI] [PubMed] [Google Scholar]
- 2.Velidedeoglu M., Kilic F., Mete B., et al. Bilateral idiopathic granulomatous mastitis. Asian J. Surg. 2016;39(1):12–20. doi: 10.1016/j.asjsur.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Altintoprak F., Kivilcim T., Ozkan O.V. Aetiology of idiopathic granulomatous mastitis. World J Clin Cases. 2014;2(12):852–858. doi: 10.12998/wjcc.v2.i12.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ozsen M., Tolunay S., Gokgoz M.S. Granulomatous lobular mastitis: clinicopathologic presentation of 90 cases. Turk. Patoloji. Derg. 2018;34(3):215–219. doi: 10.5146/tjpath.2018.01431. [DOI] [PubMed] [Google Scholar]
- 5.Martinez-Ramos D., Simon-Monterde L., Suelves-Piqueres C., et al. Idiopathic granulomatous mastitis: a systematic review of 3060 patients. Breast J. 2019;25(6):1245–1250. doi: 10.1111/tbj.13446. [DOI] [PubMed] [Google Scholar]
- 6.Mahmodlou R., Dadkhah N., Abbasi F., Nasiri J., Valizadeh R. Idiopathic granulomatous mastitis: dilemmas in diagnosis and treatment. Electron. Physician. 2017;9(9):5375–5379. doi: 10.19082/5375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolfrum A., Kümmel S., Theuerkauf I., Pelz E., Reinisch M. Granulomatous mastitis: a therapeutic and diagnostic challenge. Breast Care. 2018;13(6):413–418. doi: 10.1159/000495146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathew Thomas V., Alexander S.A., Bindal P., Vredenburgh J. Idiopathic granulomatous mastitis-A mystery yet to be unraveled: a case series and review of literature. Cureus. 2020;12(2) doi: 10.7759/cureus.6895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goulabchand R., Hafidi A., Van de Perre P., et al. Mastitis in autoimmune diseases: review of the literature, diagnostic pathway, and pathophysiological key players. J. Clin. Med. 2020;9(4):958. doi: 10.3390/jcm9040958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benson J.R., Dumitru D. Idiopathic granulomatous mastitis: presentation, investigation and management. Future Oncol. 2016;12(11):1381–1394. doi: 10.2217/fon-2015-0038. [DOI] [PubMed] [Google Scholar]
- 11.Wu J.M., Turashvili G. Cystic neutrophilic granulomatous mastitis: an update. J. Clin. Pathol. 2020;73(8):445–453. doi: 10.1136/jclinpath-2019-206180. [DOI] [PubMed] [Google Scholar]
- 12.Lacambra M., Thai T.A., Lam C.C.F., et al. Granulomatous mastitis: the histological differentials. J. Clin. Pathol. 2011;64(5):405–411. doi: 10.1136/jcp.2011.089565. [DOI] [PubMed] [Google Scholar]
- 13.Vinayagam R., Cox J., Webb L. Granulomatous mastitis: a spectrum of disease. Breast Care. 2009;4(4):251–254. doi: 10.1159/000229541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schelfout K., Tjalma W.A., Cooremans I.D., Coeman D.C., Colpaert C.G., Buytaert P.M. Observations of an idiopathic granulomatous mastitis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2001;97(2):260–262. doi: 10.1016/s0301-2115(00)00546-7. [DOI] [PubMed] [Google Scholar]
- 15.Agha R.A., Sohrabi C., Mathew G., Franchi T., Kerwan A., O'Neill N for the PROCESS Group The PROCESS 2020 guideline: updating consensus preferred reporting of CasE series in surgery (PROCESS) guidelines. Int. J. Surg. 2020;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.