PURPOSE:
People with cancer are at increased risk for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. ASCO's COVID-19 registry promotes systematic data collection across US oncology practices.
METHODS:
Participating practices enter data on patients with SARS-CoV-2 infection in cancer treatment. In this analysis, we focus on all patients with hematologic or regional or metastatic solid tumor malignancies. Primary outcomes are 30- and 90-day mortality rates and change over time.
RESULTS:
Thirty-eight practices provided data for 453 patients from April to October 2020. Sixty-two percent had regional or metastatic solid tumors. Median age was 64 years. Forty-three percent were current or previous cigarette users. Patients with B-cell malignancies age 61-70 years had twice mortality risk (hazard ratio = 2.1 [95% CI, 1.3 to 3.3]) and those age > 70 years had 4.5 times mortality risk (95% CI, 1.8 to 11.1) compared with patients age ≤ 60 years. Association between survival and age was not significant in patients with metastatic solid tumors (P = .12). Tobacco users had 30-day mortality estimate of 21% compared with 11% for never users (log-rank P = .005). Patients diagnosed with SARS-CoV-2 before June 2020 had 30-day mortality rate of 20% (95% CI, 14% to 25%) compared with 13% (8% to 18%) for those diagnosed in or after June 2020 (P = .08). The 90-day mortality rate for pre-June patients was 28% (21% to 34%) compared with 21% (13% to 28%; P = .20).
CONCLUSION:
Older patients with B-cell malignancies were at increased risk for death (unlike older patients with metastatic solid tumors), as were all patients with cancer who smoke tobacco. Diagnosis of SARS-CoV-2 later in 2020 was associated with more favorable 30- and 90-day mortality, likely related to more asymptomatic cases and improved clinical management.
INTRODUCTION
People living with cancer are at increased risk for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, COVID-19, and worse COVID-19-related outcomes.1-5 The ASCO has a mission of helping oncology clinicians through research, education, and promotion of the highest-quality and equitable patient care. Thus, ASCO created a registry to track acute and chronic effects of COVID-19 on cancer care delivery, treatments, and outcomes.
ASCO's Registry collects data from mostly community-based, nonacademic medical oncology practices and supports longitudinal data collection to track outcomes over time. Outcomes of interest include all-cause mortality, COVID-19 symptoms and treatments, cancer treatment at the time of and following COVID-19 diagnosis, and changes to cancer treatment plans. In this initial report, our primary objective is to describe the impact of SARS-CoV-2 infection on patients with cancer undergoing anticancer treatment during 2020.
METHODS
Study Design
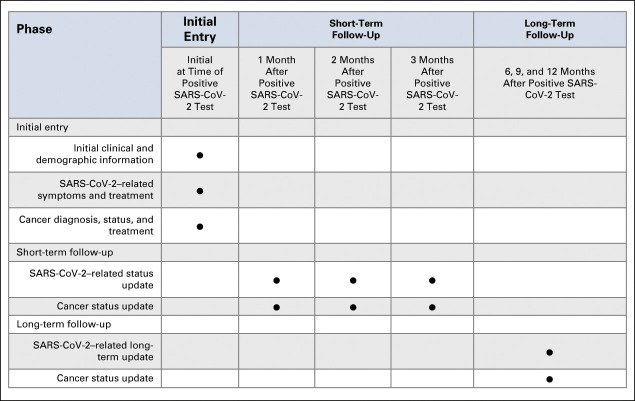
The ASCO Survey on COVID-19 in Oncology Registry is a cohort study launched in April 2020. Participating oncology practices identify patients with a positive SARS-CoV-2 test who are also actively undergoing cancer treatment. The limited identifiers include birth date, home zip code, and event dates. Birth date, home zip code, and practice name are used to link data from the same patient. Electronic health record data are manually entered by staff into REDCap electronic data capture tools (a secure, web-based software platform) hosted at ASCO.6,7 The recommended data entry schedule is at positive SARS-CoV-2 test and then at the following 1, 2, 3, 6, 9, and 12 months, although practices may submit initial data at any time. ASCO is implementing a Registry update that will extend data collection to 18 and 24 months, enabling tracking of additional vaccine doses and SARS-CoV-2 reinfections. Practices joining the registry are asked to submit data retrospectively for eligible patients who experienced illness earlier in the pandemic. The study involves a limited data set and requires data use agreements with participating institutions; WCG institutional review board reviewed the study protocol and determined it was not human subject research. This study (ClinicalTrials.gov identifier: NCT04659135) continues to add data from new and continuing patients (retrospectively and prospectively).
Practice Participation
Seventy-seven practices in the United States are currently participating, with 38 having submitted data on at least one patient at data cutoff (October 24, 2020).
Eligibility
Patients who test positive for SARS-CoV-2 and (1) have active cancer or (2) are receiving adjuvant treatment for a cancer resected within the past 12 months are eligible for registry inclusion. For this analysis, we focused on patients with hematologic malignancies or regional or metastatic solid tumors who were receiving anticancer drug therapy when they tested positive for SARS-CoV-2.
Data Collection
The registry collects information on demographics, risk factors (eg, comorbidities and smoking history), cancer (eg, type, treatments, and treatment delays), SARS-CoV-2 infection (eg, symptoms, treatments, hospitalizations, and long-term sequelae), and mortality at initial data entry. Follow-up information on acute SARS-CoV-2 infection is collected at 1, 2, and 3 months; long-term symptoms and sequelae are collected at 6, 7, and 12 months after a diagnostic SARS-CoV-2 test (Appendix Fig A1, online only). Patients' cancer status and anticancer treatment are collected at all entries.
Outcomes
We focus primarily on 30- and 90-day mortality—all-cause and because of COVID-19. Because of changes in availability of diagnostic testing, clinical experience in managing patients, and revisions to US guidelines in 2020, we hypothesized that we would find differences among patients who tested positive for the virus earlier versus later in 2020. Therefore, we examined patient outcomes before and after June 1, 2020, separately.
Statistical Analysis
Descriptive statistics summarized patient characteristics. Proportions were estimated with exact 95% CIs. Comparisons were made using Fisher's exact test or chi-square test. Hypothesis tests involving categorical variables with unknown categories were performed without including unknown data. Overall survival (OS) is defined as time from SARS-CoV-2–positive test result to death. Kaplan-Meier methods were used to estimate 30- and 90-day mortality estimates within subgroups, with 95% CIs; 90-day mortality was compared using a Z-test. Log-rank tests were used for comparing survival distributions. Cox regression evaluated the association between OS and age and cancer type. Age was included as ordinal with age groups ≤ 60, 61-70, and > 70 years. Interactions between age and cancer type were included to assess differences in association between age and OS by cancer type. Adherence to ordinality was assessed by fitting the model with age groups as nominal. Fit was almost identical based on estimated hazard ratios (HRs) and likelihood statistics; the model with age group as ordinal is reported because of improved precision of estimates. Sample size was not determined based on a power calculation or other justification because of the observational aspect. Therefore, findings are hypothesis-generating. Data cutoff was based on timing of study revisions. Although there was sufficient sample size for some comparisons, certain subgroup analyses were underpowered. As a result, inferences relied primarily on point estimates and 95% CIs with less reliance on P values.
RESULTS
Patient Characteristics
Of the 755 patients entered in the registry by October 24 (one practice provided batched data on November 15), 453 met inclusion criteria for this analysis (Appendix Fig A2, online only). Most patients (76%) were entered by 31 nonacademic practices within hospitals or health systems or free-standing (Table 1). Half of the patients (53%) had metastatic solid tumors; 38% had hematologic malignancies; and 9% had regional solid tumors. The most common cancer diagnosis was multiple myeloma (17%) followed by metastatic lung and metastatic breast cancers (11% each). Half of the patients (53%) have 30 days or more of follow-up data after SARS-CoV-2 test or died ≤ 30 days from SARS-CoV-2 test.
TABLE 1.
Characteristics of Patients Included in the Initial Analysis From the ASCO Registry
Sixty-one percent of patients were White, 27% Black, and 12% other or unknown race. Most patients were female (53%); median age was 64 years (interquartile range: 54-74 years). Most patients had no documented history of tobacco smoking (52%); 43% were current or previous cigarette users (5% unknown). Because of their association with COVID-19,8,9 hypertension, diabetes, and pulmonary disease (not including lung cancer) were examined; 36% of patients had one of these comorbidities; 23% had two comorbidities; no patients had all three. Thirty-five percent of patients had no reported comorbidities (except cancer diagnosis). Most patients were either overweight (34%) or obese (36%) according to body mass index scale.
Impact on Cancer Treatment
At the time of initial data entry, about one third of patients (35%) were continuing their anticancer drug treatments without change; half of the patients (49%) had delayed one or more anticancer drug treatments but did not discontinue any treatments. Seventy-three patients (16%) had discontinued one or more of their anticancer drug treatments, with and without antecedent delays. Most patients without drug treatment changes (72%) and those with delayed treatments (68%) were age ≤ 70 years. In those who had one or more drug discontinuations, 49% were age > 70 years (Appendix Table A2, online only). Most patients with anticancer drug discontinuations were hospitalized for COVID-19 (72%), including 30% who received intensive care. Of patients without drug treatment changes, 41% were hospitalized with only 12% receiving intensive care. A similar percentage of patients with delays were hospitalized (38%; 10% receiving intensive care).
Patient Outcomes
A total of 95 patients in the cohort had died before data cutoff. Most of these deaths (61%) were attributed to COVID-19 or its complications. Cancer progression was the second most common cause of death (22%), with causes of the remaining deaths unknown (8%), unrelated to cancer or COVID-19 (3%), or not reported (5%).
Preliminary analyses showed associations between OS and age (≤ 60, 61-70, and > 70 years, P = .001). There was no significant difference in OS comparing patients with B-cell malignancies versus those with metastatic solid tumors. Looking within cancer types, however, an age association was observed in patients with B-cell malignancies (Fig 1). Among patients with metastatic solid tumors, those age 61-70 years were not at significantly increased risk of death compared with patients ≤ 60 years (HR = 1.29 [95% CI, 0.93 to 1.79]), and similarly for those age > 70 years versus ≤ 60 years (HR = 1.67; 95% CI, 0.87 to 3.19). By contrast, patients with B-cell malignancies age 61-70 years were at more than twice the risk of death (HR = 2.11 [95% CI, 1.34 to 3.32]), and patients age > 70 years were at 4.47 times the risk of death (95% CI, 1.80 to 11.06) compared with patients age ≤ 60 years.
FIG 1.
OS by age in (A) all patients (P = .001), (B) patients with B-cell malignancy (P = .002), and (C) patients with metastatic solid tumors (P = .40). HR, hazard ratio; OS, overall survival.
All-cause mortality rates at the 30- and 90-day timepoints for all patients were 16% (95% CI, 12% to 20%) and 24% (95% CI, 20% to 29%), respectively. Many differences emerged over time in univariable analyses (Appendix Table A1, online only). Before June, testing was limited; the main reason for testing was COVID-19 symptoms (74%). Beginning in June 2020, significantly fewer patients were tested because of symptoms (49%, P < .001), and significantly more patients were tested during routine oncology care (35% after v 7% before, P < .001). Significantly more patients who tested positive before June had COVID-19–related pneumonia compared with those who tested positive in or after June (46% v 23%, P < .001). Hospitalization for COVID-19, with and without intensive care unit admission, decreased for patients diagnosed in or after June compared with those diagnosed before June (P < .001 for both) (Appendix Fig A3, online only). Patients diagnosed before June were significantly more likely to have received supplemental oxygen (44% v 21% P < .001) and been placed on a ventilator (16% v 6%, P = .001) than those diagnosed in or after June.
Figure 2 demonstrates 30- and 90-day mortality rates in patients diagnosed before June and those diagnosed in or after June. Patients diagnosed before June had a 30-day mortality rate of 20% (95% CI, 14% to 25%) compared with 13% (8% to 18%) for those diagnosed in or after June (P = .08). The 90-day mortality rate for patients with pre-June diagnoses was also higher at 28% (21% to 34%) compared with 21% (13% to 28%), although not significant (P = .20). Patients with pre-June diagnosis admitted to the intensive care unit had a 54% (33% to 68%) mortality rate at 30 days and 63% (42% to 76%) at 90 days. Patients with pre-June diagnosis who were hospitalized without intensive care had a 22% (12% to 29%) mortality rate at 30 days and 35% rate (23% to 44%) at 90 days. Mortality rates for patients with a diagnosis in or after June who were hospitalized without intensive care were lower at 30 days (11%; 95% CI, 2% to 19%) and 90 days (23%; 95% CI, 5% to 35%).
FIG 2.

Mortality rates in patients with positive severe acute respiratory syndrome coronavirus 2 test (A) before June (n = 191) or (B) in or after June (n = 262). aFor immunotherapy, at least one component was immunotherapy. For cytotoxic chemotherapy, at least one component was chemotherapy, and none were immunotherapy. For Other, No drug-based components were chemotherapy or immunotherapy. ICU, intensive care unit.
The only patient subgroups diagnosed in or after June whose 30- and 90-day mortality rates were substantially higher than for those diagnosed before June were patients who discontinued anticancer therapy and patients admitted to intensive care. Some comparisons across the periods are limited because of sample size. People with current or past tobacco use had increased mortality rates in both the pre-June and in or after June period. As shown in Appendix Figure A4 (online only), ever having smoked is a risk factor for mortality with a 30-day mortality estimate of 21% compared with only 11% for never smokers (HR = 1.81, P = .005). We found no association between body mass index and mortality, and adjusting for BMI did not diminish the association between tobacco use and mortality (HR = 1.78, P = .008).
DISCUSSION
During 2020, availability of SARS-CoV-2 tests, emerging data on use of antivirals and steroids as COVID-19 therapeutic interventions,10-13 and increasing recognition of asymptomatic transmission as an important element of infection14 led to changes in COVID-19 screening, testing, and care delivery and cancer treatment. We observed temporal differences in COVID-19 symptomatology, as well as COVID-19 and cancer disease management and outcomes in patients receiving treatment for their cancer and COVID-19. Changes in COVID-19 management and patient outcomes also reflect clinicians' growing understanding of the disease and how best to manage severe complications, as well as increasing availability of disease management options. This analysis is among the first to identify these temporal changes in the care of patients with cancer undergoing active cancer therapy, and the first to describe 90-day mortality rates for patients with cancer and COVID-19.
We observed a 30-day mortality rate of 20% for patients diagnosed with SARS-CoV-2 before June 2020, which is greater than other reports. For example, the 30-day mortality rate of 13% reported in a similar period using COVID-19 and Cancer Consortium (CCC19) data likely reflects differences between the registry populations. The ASCO Registry restricts reporting to patients in active cancer treatment and receives most reporting from community or nonacademic practices (76%); a minority (39%) of the CCC19 cohort analyzed were in active anticancer treatment and most (92%) were treated at academic centers where testing might have been more readily available earlier in the pandemic, possibly identifying milder cases. As a result, our respective cohorts may not be directly comparable. Notably, during the same pre-June 2020 interval, the rates of 30-day mortality are similar among those admitted to the hospital, 22% in CCC19 and 23% in the ASCO Registry. For those admitted to intensive care, however, large differences emerge; patients in the ASCO Registry who received intensive care had a 30-day mortality rate of 58% compared with 38% in CCC19,15 likely reflective of clinical care setting and/or impact of active cancer therapy.
This analysis from the ASCO Registry reveals an increased mortality risk with increasing age in patients, especially those with B-cell malignancies. There is nominal (and not significant) increased risk of mortality with age in those with solid tumor malignancies. The identification of more than twice the risk of death (HR = 2.11 and 4.47, respectively) for patients with B-cell malignancies age 61-70 and > 70 years is strengthened by the inclusion of large percentages of patients older than 71 years (33%) and patients with B-cell malignancies (32%). Older age has been established as one of the main risk factors for severe COVID-19,16 and other COVID-19 and cancer registry analyses report an association between increased age and mortality.
Other analyses17-19 have also found an increased risk for COVID-19 mortality among patients with hematologic malignancies with varying findings based on the type of hematologic malignancy.18,20 Passamonti et al observed worse survival among patients with acute myeloid leukemia, indolent non-Hodgkin lymphoma, aggressive non-Hodgkin lymphoma, and plasma cell neoplasms. Mortality association in Dai et al was observed in patients with leukemia, lymphoma, or myeloma. The American Society of Hematology Registry found that those with Hodgkin lymphoma had the highest percentage of deaths, followed by acute leukemia, multiple myeloma or amyloid light chain, and chronic lymphocytic leukemia.19 The biologic basis for increased COVID-19 mortality among patients with hematologic cancers is presumed to be because of decreased SARS-CoV-2–specific antibodies (immunoglobulin M and immunoglobulin G) in response to infection along with quantitative defects in CD4 and B cells (either because of the underlying disease or to its treatment) as compared to patients with solid tumor malignancies.21 Reports from BNT162b2 mRNA SARS-CoV-2 vaccination studies bolster this hypothesis, finding a lower antibody response rate for patients with chronic lymphocytic leukemia22 and older patients with multiple myeloma (median age of 83 years; range: 59-92 years).23 Our analysis found an association of mortality with age for patients with all B-cell malignancies, which included multiple myeloma, non-Hodgkin lymphoma, lymphoid leukemia, and Hodgkin lymphoma. As the number of patients and length of follow-up data grow, we plan to conduct more in-depth analyses within patients with B-cell malignancies.
Our analysis did not find an association between race, sex, and comorbidity index (including hypertension, diabetes, and pulmonary disease) and OS in our cohort of patients with regional or metastatic solid or hematologic malignancies receiving anticancer therapy. Reports from other registries8,17,18 earlier in the pandemic provided different findings across more diverse populations, including those with early-stage disease and survivors. Kuderer et al15 found a mortality association for progressive cancer, smoking (former and current), male sex, race, number of comorbidities, and Eastern Cooperative Oncology Group performance status ≥ two. An international analysis of 650 patients with multiple myeloma found that age, renal disease, and high-risk or poorly controlled multiple myeloma were independent predictors of mortality.24 In this analysis of the ASCO Registry, mortality was only associated with current or former tobacco use and older age in patients with B-cell malignancies. Because all the patients included in our cohort had advanced cancer and were receiving anticancer therapy, advanced cancer and active cancer treatment may have greater impacts than other risk factors in determining patient outcome.
Finally, our analysis offers insight about changes to cancer care delivery for patients diagnosed with COVID-19. We report a high percentage of patients with treatment delays (49%) and discontinuations (16%) with or without delays. Interpretation of these findings is challenging because of limited ability to discern whether the changes were driven by the patient's COVID-19 severity, their cancer status, or both. In addition, practices may have implemented policies to pause anticancer treatment for all patients for one or more periods to reduce exposure risks to other patients and staff within infusion space. We plan more in-depth analysis on delays and discontinuations of cancer therapies, as well as rationale for the delays and discontinuations and associations with COVID-19 symptoms and severity and patient outcomes in future work. In addition, with longer follow-up and a larger sample size, we will have power to perform analyses with greater attention to adjustment for potential confounders, including evaluation of COVID-19–related versus non–COVID-19–related OS.
This observational research study is reliant largely on data collected from ambulatory oncology clinics. As a result, ready access to inpatient and clinical data not directly related to oncology treatment varies. We directed practices to inquire with hospitals to obtain this information. We also recognize that this initial patient cohort is not representative of all patients with cancer, and sample size for this analysis is modest. To improve external validity, we are recruiting practices from additional geographic locations and enhancing inclusion of cases including the most frequent incident cancers. Differential duration of follow-up for those diagnosed early versus later in the pandemic may lead to bias, but most hospitalizations and COVID-19 symptoms are reported on the initial registry form; so, the potential differential follow-up bias is somewhat mitigated. Initial analysis of data collected regarding cancer treatment delays and discontinuations led us to recognize that more detailed data were needed (eg, start dates, stop dates and drug names) to better characterize lengths of delays and identify treatments that were changed or discontinued. Our data collection forms have now been revised to capture this information and will provide greater detail to expand this analysis in future research.
Although US outbreaks have slowed, our findings continue to be relevant in areas with low vaccination rates and surging SARS-CoV-2 variant infections. Additionally, for patients with cancer who exhibit decreased vaccine response, our findings that life can be extended with early diagnosis (testing of asymptomatic individuals) and aggressive care (as implemented after June 2020) are important, as SARS-CoV-2 remains a public health problem in the United States as well as in many countries, especially low- and middle-income countries around the world with limited access to vaccines.
In conclusion, among patients with regional or metastatic solid tumor and hematologic cancers, those with both B-cell malignancies and older age were at increased risk for death, along with people who previously or currently smoke tobacco. Patients in the United States diagnosed with SARS-CoV-2 during the first six months of 2020 were more likely to receive intensive COVID-19 interventions and were at greater mortality risk. Delays and discontinuations of cancer treatment were common, and future analyses will provide more in-depth analysis of these data.
ACKNOWLEDGMENT
The ASCO Registry is supported by Conquer Cancer, the ASCO Foundation's COVID Impacts Cancer Fund (https://p2p.conquer.org/covidresponse?cmpid=learn_more_homepage_secondary_pane). ASCO thanks the oncology practices that are participating in the ASCO Survey on COVID-19 in Oncology (ASCO) Registry (https://www.asco.org/asco-coronavirus-information/coronavirus-registry), taking the time to enter data on their patients' experiences with cancer and COVID-19.
Appendix
FIG A1.
Study calendar for patients in ASCO survey on COVID-19 in Oncology Registry. The Registry was changed in August 2021 to add data collection for at 18 and 24 months after positive SARS-CoV-2 test. The full ASCO Registry protocol schema is available at https://www.asco.org/asco-coronavirus-information/coronavirus-registry. SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
FIG A2.

CONSORT diagram for registry patients selected for analysis.
FIG A3.

COVID-19 interventions in patients diagnosed with severe acute respiratory syndrome coronavirus 2 before or after June 2020. Estimated percentages remove unknown percentages for each category of intervention from the percentage that is reported (Table 1). ICU, intensive care unit.
FIG A4.

Thirty- and 90-day mortality estimates by patient subgroups. ICI, immune checkpoint inhibitor; ICU, intensive care unit.
TABLE A1.
COVID-19 Information, Stratified by Date of COVID-19 Diagnosis
TABLE A2.
Select Baseline Characteristics, Stratified by Patients Who Had No Changes to Their Cancer Treatment(s), Delay(s) in One or More of Their Cancer Treatments, or Discontinuation(s) of One or More of Their Cancer Treatment(s) (possibly in addition to delays)
Kathryn F. Mileham
Honoraria: Bristol Myers Squibb, Regeneron
Consulting or Advisory Role: AstraZeneca, Bayer, Merck
Charu Aggarwal
Consulting or Advisory Role: Genentech, Lilly, Celgene, Merck, AstraZeneca, Blueprint Genetics, Shionogi, Daiichi Sankyo/Astra Zeneca
Speakers' Bureau: AstraZeneca (I), Roche/Genentech (I)
Research Funding: Genentech/Roche (Inst), Incyte (Inst), Macrogenics (Inst), Merck Sharp & Dohme (Inst), AstraZeneca/MedImmune (Inst)
Daniel J. Mesenhowski
Employment: Virginia Cancer Specialists
Alexander Spira
Leadership: NEXT Oncology Virginia (Inst)
Stock and Other Ownership Interest: Lilly
Honoraria: CytomX Therapeutics, AstraZeneca/MedImmune, Merck, Takeda, Amgen, Janssen Oncology, Novartis, Bristol Myers Squibb, Bayer
Consulting or Advisory Role: Array BioPharma (Inst), Incyte, Amgen, Novartis, AstraZeneca/MedImmune (Inst), Mirati Therapeutics, Gritstone Oncology, Jazz Pharmaceuticals, Merck (Inst), Bristol Myers Squibb (Inst), Takeda, Janssen Research & Development
Research Funding: Roche (Inst), AstraZeneca (Inst), Boehringer Ingelheim (Inst), Astellas Pharma (Inst), MedImmune (Inst), Novartis (Inst), Newlink Genetics (Inst), Incyte (Inst), AbbVie (Inst), Ignyta (Inst), LAM Therapeutics (Inst), Trovagene (Inst), Takeda (Inst), Macrogenics (Inst), CytomX Therapeutics (Inst), Astex Pharmaceuticals (Inst), Bristol-Myers Squibb (Inst), Loxo (Inst), Arch Therapeutics (Inst), Gritstone Oncology (Inst), Plexxikon (Inst), Amgen (Inst), Daiichi Sankyo (Inst), ADC Therapeutics (Inst), Janssen Oncology (Inst), Mirati Therapeutics (Inst), Rubius Therapeutics (Inst)
Eric J. Clayton
Employment: US Oncology, HCA Healthcare
Stock and Other Ownership Interests: HCA Healthcare
Research Funding: US Oncology
Travel, Accommodations, Expenses: US Oncology
David Waterhouse
Consulting or Advisory Role: Bristol Myers Squibb, AZTherapies, AbbVie, Amgen, McGivney Global Advisors, Janssen Oncology, Seattle Genetics, Jazz Pharmaceuticals, Exelixis, Eisai, EMD Serono, Merck, Pfizer, Mirati Therapeutics, Regeneron/Sanofi
Speakers' Bureau: Bristol-Myers Squibb, Janssen Oncology, Merck, AstraZeneca, Amgen, EMD Serono
Travel, Accommodations, Expenses: Bristol Myers Squibb
Abdul-Rahman Jazieh
Stock and Other Ownership Interests: Innovative Healthcare Institute
Research Funding: MSD Oncology, AstraZeneca, Pfizer
Travel, Accommodations, Expenses: Bristol Myers Squibb
Other Relationship: MSD (Inst)
Ronald C. Chen
Consulting or Advisory Role: Medivation/Astellas, Accuray, Bayer, Blue Earth Diagnostics, AbbVie, Myovant Sciences, Genentech, Pfizer
Research Funding: Accuray
Julie R. Gralow
Consulting or Advisory Role: Genentech, AstraZeneca, Hexal, Puma Biotechnology, Roche, Novartis, Seagen, Genomic Health
Richard L. Schilsky
Leadership: Clariifi
Consulting or Advisory Role: Cellworks, Scandion Oncology, Bryologyx
Research Funding: AstraZeneca (Inst), Bayer (Inst), Bristol Myers Squibb (Inst), Genentech/Roche (Inst), Lilly (Inst), Merck (Inst), Pfizer (Inst), Boehringer Ingelheim (Inst), Seattle Genetics (Inst)
Open Payments Link: https://openpaymentsdata.cms.gov/physician/1138818/summary
Elizabeth Garrett-Mayer
Consulting or Advisory Role: Deciphera
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Poster presentation and discussion session at 2021 ASCO Annual Meeting.
SUPPORT
Conquer Cancer, the ASCO Foundation, funds the ASCO Registry and had no role in study design, data collection, data analysis, data interpretation, writing of the report, or decision to submit for publication.
K.F.M. and S.S.B. contributed equally as cofirst authors. R.L.S. and E.G.-M. contributed equally as cosenior authors.
AUTHOR CONTRIBUTIONS
Conception and design: Kathryn F. Mileham, Suanna S. Bruinooge, Charu Aggarwal, David Waterhouse, Abdul-Rahman Jazieh, Ronald C. Chen, Richard L. Schilsky, Elizabeth Garrett-Mayer
Financial support: Suanna S. Bruinooge
Administrative support: Suanna S. Bruinooge, Melinda Kaltenbaugh, Jen Hanley Williams, Elizabeth Garrett-Mayer
Provision of study materials or patients: Kathryn F. Mileham, Suanna S. Bruinooge, Charu Aggarwal, Alicia L. Patrick, Daniel J. Mesenhowski, Alexander Spira, Eric J. Clayton, David Waterhouse, Susan Moore
Collection and assembly of data: Kathryn F. Mileham, Suanna S. Bruinooge, Charu Aggarwal, Alicia L. Patrick, Christiana Davis, Daniel J. Mesenhowski, Alexander Spira, Eric J. Clayton, David Waterhouse, Susan Moore, Melinda Kaltenbaugh, Jen Hanley Williams, Elizabeth Garrett-Mayer
Data analysis and interpretation: Kathryn F. Mileham, Suanna S. Bruinooge, Charu Aggarwal, Christiana Davis, Alexander Spira, David Waterhouse, Ronald C. Chen, Julie R. Gralow, Richard L. Schilsky, Elizabeth Garrett-Mayer
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Changes Over Time in COVID-19 Severity and Mortality in Patients Undergoing Cancer Treatment in the United States: Initial Report From the ASCO Registry
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Kathryn F. Mileham
Honoraria: Bristol Myers Squibb, Regeneron
Consulting or Advisory Role: AstraZeneca, Bayer, Merck
Charu Aggarwal
Consulting or Advisory Role: Genentech, Lilly, Celgene, Merck, AstraZeneca, Blueprint Genetics, Shionogi, Daiichi Sankyo/Astra Zeneca
Speakers' Bureau: AstraZeneca (I), Roche/Genentech (I)
Research Funding: Genentech/Roche (Inst), Incyte (Inst), Macrogenics (Inst), Merck Sharp & Dohme (Inst), AstraZeneca/MedImmune (Inst)
Daniel J. Mesenhowski
Employment: Virginia Cancer Specialists
Alexander Spira
Leadership: NEXT Oncology Virginia (Inst)
Stock and Other Ownership Interest: Lilly
Honoraria: CytomX Therapeutics, AstraZeneca/MedImmune, Merck, Takeda, Amgen, Janssen Oncology, Novartis, Bristol Myers Squibb, Bayer
Consulting or Advisory Role: Array BioPharma (Inst), Incyte, Amgen, Novartis, AstraZeneca/MedImmune (Inst), Mirati Therapeutics, Gritstone Oncology, Jazz Pharmaceuticals, Merck (Inst), Bristol Myers Squibb (Inst), Takeda, Janssen Research & Development
Research Funding: Roche (Inst), AstraZeneca (Inst), Boehringer Ingelheim (Inst), Astellas Pharma (Inst), MedImmune (Inst), Novartis (Inst), Newlink Genetics (Inst), Incyte (Inst), AbbVie (Inst), Ignyta (Inst), LAM Therapeutics (Inst), Trovagene (Inst), Takeda (Inst), Macrogenics (Inst), CytomX Therapeutics (Inst), Astex Pharmaceuticals (Inst), Bristol-Myers Squibb (Inst), Loxo (Inst), Arch Therapeutics (Inst), Gritstone Oncology (Inst), Plexxikon (Inst), Amgen (Inst), Daiichi Sankyo (Inst), ADC Therapeutics (Inst), Janssen Oncology (Inst), Mirati Therapeutics (Inst), Rubius Therapeutics (Inst)
Eric J. Clayton
Employment: US Oncology, HCA Healthcare
Stock and Other Ownership Interests: HCA Healthcare
Research Funding: US Oncology
Travel, Accommodations, Expenses: US Oncology
David Waterhouse
Consulting or Advisory Role: Bristol Myers Squibb, AZTherapies, AbbVie, Amgen, McGivney Global Advisors, Janssen Oncology, Seattle Genetics, Jazz Pharmaceuticals, Exelixis, Eisai, EMD Serono, Merck, Pfizer, Mirati Therapeutics, Regeneron/Sanofi
Speakers' Bureau: Bristol-Myers Squibb, Janssen Oncology, Merck, AstraZeneca, Amgen, EMD Serono
Travel, Accommodations, Expenses: Bristol Myers Squibb
Abdul-Rahman Jazieh
Stock and Other Ownership Interests: Innovative Healthcare Institute
Research Funding: MSD Oncology, AstraZeneca, Pfizer
Travel, Accommodations, Expenses: Bristol Myers Squibb
Other Relationship: MSD (Inst)
Ronald C. Chen
Consulting or Advisory Role: Medivation/Astellas, Accuray, Bayer, Blue Earth Diagnostics, AbbVie, Myovant Sciences, Genentech, Pfizer
Research Funding: Accuray
Julie R. Gralow
Consulting or Advisory Role: Genentech, AstraZeneca, Hexal, Puma Biotechnology, Roche, Novartis, Seagen, Genomic Health
Richard L. Schilsky
Leadership: Clariifi
Consulting or Advisory Role: Cellworks, Scandion Oncology, Bryologyx
Research Funding: AstraZeneca (Inst), Bayer (Inst), Bristol Myers Squibb (Inst), Genentech/Roche (Inst), Lilly (Inst), Merck (Inst), Pfizer (Inst), Boehringer Ingelheim (Inst), Seattle Genetics (Inst)
Open Payments Link: https://openpaymentsdata.cms.gov/physician/1138818/summary
Elizabeth Garrett-Mayer
Consulting or Advisory Role: Deciphera
No other potential conflicts of interest were reported.
REFERENCES
- 1.Wang Q, Berger NA, Xu R: Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol 7:220-227, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He W, Chen L, Chen L, et al. : COVID-19 in persons with haematological cancers. Leukemia 34:1637-1645, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robilotti EV, Babady NE, Mead PA, et al. : Determinants of COVID-19 disease severity in patients with cancer. Nat Med 26:1218-1223, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang W, Guan W, Chen R, et al. : Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol 21:335-337, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta V, Goel S, Kabarriti R, et al. : Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov 10:935-941, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377-381, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Minor BL, et al. : The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95:103208, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ejaz H, Alsrhani A, Zafar A, et al. : COVID-19 and comorbidities: Deleterious impact on infected patients. J Infect Public Health 13:1833-1839, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao YD, Ding M, Dong X, et al. : Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 76:428-455, 2021 [DOI] [PubMed] [Google Scholar]
- 10.Holshue ML, DeBolt C, Lindquist S, et al. : First case of 2019 novel coronavirus in the United States. N Engl J Med 382:929-936, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grein J, Ohmagari N, Shin D, et al. : Compassionate use of remdesivir for patients with severe Covid-19. N Engl J Med 382:2327-2336, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanders JM, Monogue ML, Jodlowski TZ, et al. : Pharmacologic treatments for coronavirus disease 2019 (COVID-19): A review. JAMA 323:1824-1836, 2020 [DOI] [PubMed] [Google Scholar]
- 13.WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC Murthy S et al. : Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: A meta-analysis. JAMA 324:1330-1341, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gandhi M, Yokoe DS, Havlir DV: Asymptomatic transmission, the Achilles' heel of current strategies to control Covid-19. N Engl J Med 382:2158-2160, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuderer NM, Choueiri TK, Shah DP, et al. : Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 395:1907-1918, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Derosa L, Melenotte C, Griscelli F, et al. : The immuno-oncological challenge of COVID-19. Nat Cancer 1:946-964, 2020 [DOI] [PubMed] [Google Scholar]
- 17.Passamonti F, Cattaneo C, Arcaini L, et al. : Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: A retrospective, multicentre, cohort study. Lancet Haematol 7:e737-e745, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dai M, Liu D, Liu M, et al. : Patients with cancer appear more vulnerable to SARS-CoV-2: A multicenter study during the COVID-19 outbreak. Cancer Discov 10:783-791, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang K, Sheng Y, Huang C, et al. : Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: A multicentre, retrospective, cohort study. Lancet Oncol 21:904-913, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wood WA, Neuberg DS, Thompson JC, et al. : Outcomes of patients with hematologic malignancies and COVID-19: A report from the ASH Research Collaborative Data Hub. Blood Adv 4:5966-5975, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang A, Bange E, Han N, et al. : CD8 T cells compensate for impaired humoral immunity in COVID-19 patients with hematologic cancer. Res Sq. 2021. 10.21203/rs.3.rs-162289/v1 [DOI] [Google Scholar]
- 22.Herishanu Y, Avivi I, Aharon A, et al. : Efficacy of the BNT162b2 mRNA COVID-19 vaccine in patients with chronic lymphocytic leukemia. Blood 137:3165-3173, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Terpos E, Trougakos IP, Gavriatopoulou M, et al. : Low neutralizing antibody responses against SARS-CoV-2 in elderly myeloma patients after the first BNT162b2 vaccine dose. Blood 137:3674-3676, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chari A, Samur MK, Martinez-Lopez J, et al. : Clinical features associated with COVID-19 outcome in multiple myeloma: First results from the international myeloma society data set. Blood 136:3033-3040, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]