Abstract
Background:
The direction toward incorporating clinical pharmacy services is increasing worldwide but there are many barriers that hinder its implementation in many countries. The types of barriers vary among countries according to their culture, population, education & economic status.
Objective:
This study aims to investigate factors hindering the implementation of clinical pharmacy practice in Egyptian hospitals.
Methods:
Hundred hospital pharmacists working in various reputable hospitals in Egypt participated in a descriptive cross-sectional survey designed as a questionnaire representing the main factors previously reported in the literature to hinder clinical pharmacy implementation in different countries around the world. Cronbach alpha was calculated to test the reliability of the questionnaire. Likert plot was used to graphically present the participants’ responses.
Results:
The most significant factors that participants reported to hinder the implementation of clinical pharmacy practice in Egyptian hospitals were the lack of clear career path, financial resources, and leadership support. The percentage of participants who agreed that such factors were key players in hindering the implementation of clinical pharmacy practice was 76%, 74%, and 57% respectively.
Conclusion:
A number of factors were found to impede clinical pharmacy implementation in Egyptian hospitals. Taking corrective measures to resolve such hindrances should ensure proper hospital pharmacy practice and should positively reflect on patient healthcare services provided at the national level.
Keywords: Clinical pharmacy, Factors, Hindering, Career path, Egypt
INTRODUCTION
Pharmacy practice evolved worldwide from dispensing medication to stressing the role of the pharmacist as an essential member of the healthcare team.1 Nowadays, full-spectrum clinical pharmacy services are established in many countries, associated with reduced adverse drug events, medication errors, mortality rates, and treatment costs. Such pharmaceutical services provide patient care by optimizing medication therapy, promoting health, wellness, and disease prevention.2 Clinical pharmacists are specialized in therapeutic knowledge, experience, and skills that can help ensure optimum patient care by applying the best available clinical evidence and interventions in collaboration with the healthcare team.3 Despite such importance of clinical pharmacy practice, many factors prevent its implementation in many countries worldwide. Such types of barriers have been found to vary according to the culture, population, education, and economic status of each country.4 The barriers can be classified into two groups, the first group includes external factors that are out of the pharmacists’ control such as governmental support, national policies, and laws. While the second group includes internal factors such as lack of experience, low salaries, lack of clear career pathway, and difficulties in communication between pharmacists and other healthcare team members.5-7
Many studies were conducted to determine the most significant factors hindering proper implementation of clinical pharmacy in different countries; mainly the United Arab Emirates (UAE), Brazil, India, Pakistan, Philippines, Kuwait, Nigeria, Ethiopia, China, and Portugal. The main barriers in the UAE were found to be high workload, insufficient staff numbers, and lack of time and motivation of pharmacists to pursue a career in clinical practice.5 Most of the “Bachelor of Pharmacy” degree programs in the UAE have recently undergone noticeable changes to accommodate recent international developments in the field of pharmacy. The curriculum of such programs incorporated more clinical and social science courses related to pharmacy practice and even many faculties of pharmacy started to offer Pharm D as their undergraduate program.8 The barriers in Brazil were found to be poor facility layout in addition to healthcare team workers’ resistance, fear, and frustration due to lack of clinical and communication skills. The Pharmacy undergraduate programs in Brazil have a median duration of ten semesters with diversity in the context of internships which require from students a median of six internships. The post-graduate programs include a residency for two years, a Master’s degree for two years & a Ph.D. program of three years.9-11
In India and Pakistan, the profession is more industry-oriented rather than patient-oriented and the role of the clinical pharmacist is still unclear among the healthcare professionals and community.12-14 In addition, experienced and qualified staff needed for practicing and upgrading the B Pharm to a Pharm D program are lacking and there is limited acceptance of the role of pharmacists as healthcare team members by medical and paramedical staff in clinical settings. In 2008, the Pharmacy Council of India introduced a two-year post-graduate Pharm D program intending to prepare clinically oriented pharmacists with rigorous training in clinical aspects for providing pharmaceutical care services to patients.13 In 2005, the Pakistan Pharmacy Council (PPC) upgraded the B Pharm program to a Pharm D program and many pharmacy schools have expanded their pharmacy curriculum to five or six years that lead to a Pharm D degree.14
In the Philippines, the primary factors hindering the implementation of clinical pharmacy practice were reported to be lack of support by physicians and other healthcare professionals, lack of information technology support needed for data collection and documentation, lack of incentives, and the need for updating the pharmacy curriculum.15,16 In addition, there are no standard guidelines for pharmaceutical care practice,7,17 and the undergraduate pharmacy program in the Philippines is extended from 4 years to 5 year B pharm program while also offering a 2-year post-graduate Pharm D program.18
In Kuwait, the main factors hindering the implementation of clinical pharmacy include insufficient staff, lack of proper clinical training, lack of appreciation for pharmacy services by physicians, and the limited time allowed for pharmacists to provide patient care services.19 To face this problem, authorities tried to improve the clinical pharmacy practice by enhancing the quality of education provided to locally-trained clinical pharmacists, approving a post-Bachelor Pharm D degree program that provides clinical training during which pharmacists develop the requisite clinical skills to provide standard pharmaceutical care, and sending pharmacists abroad for additional training and providing up-to-date continuous medical education opportunities to practicing pharmacists.20
Deficiency of funds, difficulty in accessing patients’ clinical and laboratory data, lack of motivation, compromised clinical knowledge, lack of time & space for private counseling, shortage of financial incentives, and low community expectations of the pharmacy profession are the factors that hinder the implementation of clinical pharmacy in Nigeria.7 Other barriers also included pharmacists’ lack of confidence, shortage of pharmacy staff, underutilization of pharmacy technicians, lack of specialization and clinical career structure, medical dominance & opposition, and lack of policies that support clinical pharmacy practice.21 It was not until 2016 that the overall regulatory government agency for all university degree programs in Nigeria, formally approved the Pharm D degree program as a six-year undergraduate program but still most universities offer a five-year B Pharm degree program.22
Lack of sufficient training & awareness, shortage of skilled manpower, lack of incentives, and the need to update the curriculum are the factors that are facing the Ethiopian pharmacists toward the proper implementation of clinical pharmacy.3,23 After a long track record of product-oriented pharmacy practice in Ethiopia, a shift towards a patient-oriented practice is recently introduced by the implementation of a 5-year B Pharm curriculum which includes a one-year clerkship program.23 In China, the factors that impede clinical pharmacy implementation are classified into three categories; one is external that need governmental and upper management support, the second is related to the financial resources available for the incentives and the clinical training, and the third one is related to the expectations and attitudes of clinical pharmacists.4 Until 2008, pharmacy education in China used to focus on pharmaceutical sciences, with the “Bachelor of Science in Pharmacy” as the entry-level degree.24 In 2011, the Ministry of Health directed the pharmacy education toward clinical pharmacy by issuing a policy that all secondary and tertiary hospitals should have at least three and five full-time clinical pharmacists, respectively and in 2018, it indicated that pharmacists have the ultimate responsibility for prescription review.25,26 Barriers to the implementation of advanced clinical pharmacy services identified by Portuguese hospital pharmacists included only the predetermined attitudes and mindsets of pharmacists.27 The Master in Pharmaceutical Sciences is the undergraduate degree offered by faculties of pharmacy in Portugal which allows pharmacists to work in diverse professional areas including community pharmacy, hospital pharmacy, clinical biology, pharmaceutical industry, and regulatory affairs.28 This program is equivalent to the Pharm D program which comprises a six-year rigorous study after which the academic title of Doctor of Pharmacy is issued. Currently, the regulatory body of the pharmacy profession in Portugal; the Portuguese Pharmaceutical Society, does not endorse clinical pharmacy as a specialty since they consider that both hospital and community pharmacists may qualify as clinical pharmacists, but primary care pharmacists with advanced competencies in clinical pharmacy have been incorporated into the healthcare multidisciplinary teams.29
In 1995, the majority of faculties of pharmacy in Egypt used to offer the traditional 5-year undergraduate “BSc in Pharmacy” program stressing the old dispensing pharmacist model, but over time a tendency emerged to develop the role of the pharmacist to be more patient-oriented in an advanced healthcare system.30,31 After 2001, many faculties of pharmacy started to offer additional 5-year undergraduate “BSc in Clinical Pharmacy” program. In 2012, some Faculties of Pharmacy such as Cairo University, Ain Shams University, Alexandria University, and Beni Suef University also started to offer a two-year postgraduate Pharm D degree to satisfy the needs of the BSc in Pharmacy graduates. The first year of this postgraduate Pharm D program includes many didactic courses mainly pharmacotherapy, pharmacokinetics, and pharmaceutical care of many diseases. The second-year consists of clinical rotations in different specialties including ambulatory care, oncology, cardiology, nephrology, pediatrics, and others. In 2019, All faculties of pharmacy in Egypt were required, by the Pharmacy Sector Committee of the Supreme Council of Universities, to offer two 6-year (5+1) Pharm D programs; one replacing the “BSc in Pharmacy” and the other replacing the “BSc in Clinical Pharmacy”, to be followed by a national pre-licensure exam as the minimum requirement for licensure as a pharmacist in Egypt. The first Pharm D program has diversity in the context of internships which allows graduates to work in diverse professional areas including community pharmacy, hospital pharmacy, pharmaceutical industry, regulatory affairs, academia, and research. The second Pharm D program focuses mainly on Clinical/hospital pharmacy with one year of Clinical internships. Although the Egyptian Ministry of Health mandated that all hospitals must implement clinical pharmacy practices, till now clinical pharmacy practice is either not implemented at all or not ideally implemented in many Egyptian hospitals due to several factors.32 These barriers are not studied at the national level yet. We hereby designed a survey to investigate different factors hindering the implementation of clinical pharmacy practice in Egyptian hospitals.
OBJECTIVE
This study aims to investigate factors hindering the implementation of clinical pharmacy practice in Egyptian hospitals.
METHODS
This is a prospective multiple-site study where a descriptive cross-sectional survey was designed to investigate factors hindering clinical pharmacy practice in Egyptian hospitals. Such descriptive research design involves the process of recording, describing, interpreting, and analyzing the events where a questionnaire was made available, either as a hardcopy or as an electronic version, to hundred hospital pharmacists who have more than one year of experience and are working in seven reputable hospitals in Egypt. These hospitals started applying clinical pharmacy services and are facing some obstacles toward proper implementation. Hospital pharmacists with less than one year of experience and those who do not have direct contact with the patient such as quality or warehouse pharmacists were excluded from the study. The questionnaire has ten questions with an ordinal scale from one to five covering the common factors previously reported in the literature as hindering factors for the implementation of clinical pharmacy in different countries around the world. The questionnaire was validated by the “Academic Residency Program Committee’ and the study protocol was approved by the Institution Review Board (IRB) of CCHE 57357 (IRB No. 42/2021). Descriptive statistics for the questionnaire were summarized as mean, standard deviation, and range for continuous data as well as frequency and percentage for categorical data. Likert plot was used to graphically present the participants’ responses to each item of the questionnaire. Cronbach alpha was calculated to test the reliability of the questionnaire. R Foundation for Statistical Computing, Vienna, Austria version 3.6.0 was used for the analysis. The packages “sjPlot” version 2.6.3 was used for plotting Likert plots and the package “psych” version 1.8.12 was used for Cronbach alpha calculation.
RESULTS
Results showed that more than half of the participants graduated between the years 2016 and 2018. Around third of the participants graduated between the years 2011 and 2015. On the other hand, about a tenth of the participants graduated between the years 2000 and 2010 (see Table 1).
Table 1.
Frequency of different categories of participants according to graduation year. Descriptive statistics for the questionnaire were summarized as frequency and percentage for categorical data
| Graduation year | Percentage |
|---|---|
| 2000 to 2010 | 12 |
| 2011 to 2015 | 35 |
| 2016 to 2018 | 53 |
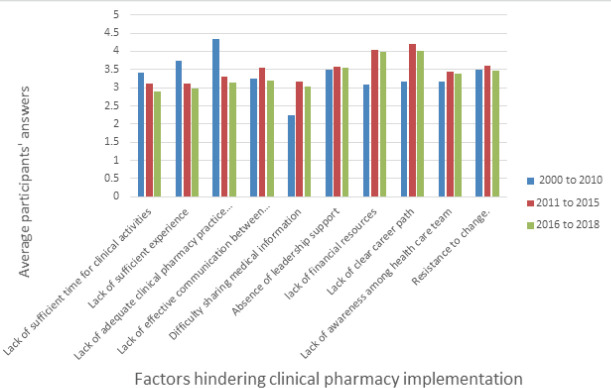
The top three factors that participants reported as factors impeding clinical pharmacy implementation were lack of clear career path, lack of financial resources, and lack of leadership support. The percentage of participants who agreed on these factors to be the main players in clinical pharmacy implementation was 76%, 74%, and 57% respectively. The fourth, fifth, sixth, and seventh-most influencing factors on clinical pharmacy implementation were found to be the “lack of adequate clinical pharmacy practice training”, “resistance to change”, “lack of awareness among healthcare team about the importance of clinical pharmacy”, and “lack of effective communication among healthcare team members” with 49%, 48%, 45% and 40% of participates votes respectively. The least influencing factors were “lack of sufficient experience and information required for clinical pharmacy practice”, “difficulty sharing medical information and patient files among healthcare team” and “lack of sufficient time for clinical activities due to the overload with routine work” which accounted for 39%, 36%l, and 30% of the participants’ votes respectively (see Figure 1).
Figure 1.
Perception of hospital pharmacists about factors that impede implementation of clinical pharmacy practice in Egyptian hospitals. Likert plot was used to graphically represent the participants’ response to each item of the questionnaire where Score 5 = most agree & Score 1= least agree. The packages “sj Plot” version 2.6.3 was used for plotting Likert plots.
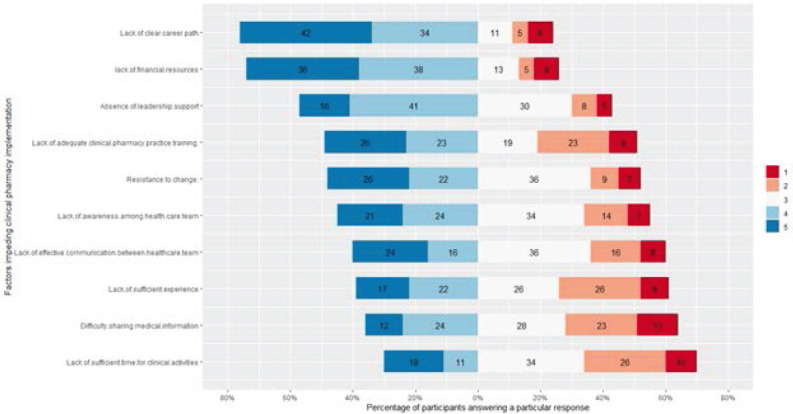
Answers of each participant to all questions are added and divided by 10; the number of questions, to get the average scores for the 10 questions. The possible range for the scores is from 1 to 5. The minimum average for a survey was 1.1 while the maximum average was 5. A summary of the actual responses to questions is available in Table 2 which shows that both Cronbach alpha and standardized Cronbach alpha values are good reflecting the reliability of the questionnaire. A mean of 3.41 indicates that participants, in general, are considering these ten factors as potential barriers to the implementation of the clinical pharmacy practice. In general, the responses of participants between 2016 and 2018 and between 2011 and 2015 are quite similar. However, these responses are quite different from those with graduation years between 2000 and 2010. Figure 2 demonstrates that lack of sufficient time, experience, and training are especially reported by participants with graduation years between 2000 and 2010. On the other hand, difficultly sharing information, lack of career path, or financial resources are considered to be less important barriers for clinical pharmacy implementation among the same category of participants.
Table 2.
Results of Cronbach alpha test as a measure of reliability as well as mean±SD and range of participants’ responses
| Cronbach alpha | Standardized Cronbach alpha | mean | sd | min | max |
|---|---|---|---|---|---|
| 0.803 | 0.806 | 3.410 | 0.723 | 1.100 | 5.000 |
Descriptive statistics for the questionnaire were summarized as mean, standard deviation, and range for continuous data. The package “psych” version 1.8.12 was used for Cronbach alpha calculation.
Figure 2.
Participants’ answers for each questionnaire item grouped by graduation year. The questionnaire has ten questions with an ordinal scale from one to five covering the common factors previously reported in the literature as hindering factors for the implementation of clinical pharmacy in different countries around the world.
The average score of each participant was calculated across all questions. Next, participants were grouped according to their graduation year. The percentage of participants scoring 4 or more is plotted in Figure 3. In general, only a minority (less than 10%) of participants with the graduation year of 2000 to 2010 had an average answer of 4 or more. On the other hand, more than 30% of participants with experience between 2011 and 2015 had an average score of 4 or more. More than 15% of the category of participants with graduation years between 2016 and 2018 had an average score of 4 or more.
Figure 3.
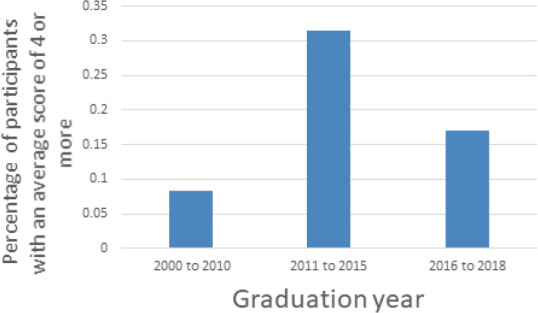
Participants’ average responses to the whole questionnaire grouped by their graduation year
R Foundation for Statistical Computing, Vienna, Austria version 3.6.0 was used for the analysis.
DISCUSSION
The findings of this study demonstrated some common factors as the main obstacles to the implementation of clinical pharmacy practice in Egyptian hospitals. The majority of participating pharmacists perceived the “lack of career pathway of clinical pharmacists” as the most important factor impeding the proper implementation of clinical pharmacy. “Lack of financial resources for establishing appropriate clinical pharmacy units” was considered the second most important factor by participating pharmacists which is expected given that Egypt is one of the world’s developing countries. The third most influencing factor was found to be the “Absence of the hospital leadership support”. Other influencing factors reported were “lack of adequate clinical pharmacy practice training”, “resistance to change”, “lack of awareness among healthcare team about the importance of clinical pharmacy”, and “lack of their effective communication. It is to be noted that the resistance to change from the physicians’ side is well known in some hospitals in Egypt.
The results of our study have some similarities with other studies in different countries. The “lack of career path of clinical pharmacists” was also reported as an important factor impeding the proper implementation of clinical pharmacy in the UAE and Nigeria. The “Lack of financial resources” was also reported as an important factor impeding the proper implementation of clinical pharmacy in the Philippines, Nigeria, Ethiopia, Brazil, and China. The “Absence of leadership support” was also reported as an important factor impeding the proper implementation of clinical pharmacy in India, Pakistan, the Philippines, Kuwait, China, and Nigeria. The results of this study also have some similarities with other studies in different countries concerning the fourth, fifth, sixth, and seventh-most influencing factors on clinical pharmacy implementation. The “lack of adequate clinical pharmacy practice training” was also reported to hinder clinical pharmacy implementation in Kuwait and Ethiopia. The “resistance to change” was also reported to hinder clinical pharmacy implementation in Brazil, India, Pakistan, the Philippines, Kuwait, and Nigeria. The “lack of awareness among healthcare teams about the importance of clinical pharmacy” was also found to hinder clinical pharmacy implementation in Brazil, India, Pakistan, Kuwait, Nigeria, and Ethiopia. The “lack of effective communication among healthcare team members” was also reported to hinder clinical pharmacy implementation in Brazil.
Comparing the barriers in Egypt with the other Arab countries; UAE and Kuwait, reveals that Egypt and UAE share common barriers which are “lack of motivation for pharmacists” or lack of vision on pharmacists’ professional development and “high workload” that affect the time needed for good patient counseling. But the two countries differ in that, contrary to UAE, insufficient staff numbers do not constitute a barrier to clinical pharmacy implementation in Egypt. Indeed, according to a report released in 2019 by the “Pharmacy Sector Committee” of the “Supreme Council of Egyptian University”, the number of pharmacists in Egypt reached 216,072 having one pharmacist for every 438 citizens which is more than four times the international standards, and also the number of pharmacies reached 75,165 having one pharmacy for every 1,261 citizens which are about 3-fold the international standards. From another perspective, comparing the barriers in Egypt with those in Kuwait reveals that Egypt and Kuwait share common barriers which are lack of proper clinical training, lack of appreciation for pharmacy services by some physicians, and the limited time allowed for pharmacists to provide patient care services. But again the two countries differ in that, contrary to Kuwait, insufficient staff numbers do not constitute a barrier to clinical pharmacy implementation in Egypt.
Comparing the barriers in Egypt with the other African countries; Nigeria and Ethiopia, reveals that Egypt and Nigeria share common barriers which are lack of career pathway of clinical pharmacists reflecting on their motivation, deficiency of funds, lack of time for private counseling, and resistance to change by some medical staff. The two countries differ though, in that, some other barriers found in Nigeria are not reported as barriers for the implementation of clinical pharmacy in Egypt such as; difficulty in accessing patients’ clinical and laboratory data, compromised clinical knowledge, lack of space for private counseling, low community expectations of the pharmacy profession, pharmacists’ lack of confidence, shortage of pharmacy staff, underutilization of pharmacy technicians, medical dominance, and lack of policies that support clinical pharmacy practice. The common barriers between Egypt and Ethiopia are the lack of sufficient training & awareness and lack of financial incentives, while in Egypt, and contrary to Ethiopia, shortage of skilled manpower and the need to update the curriculum is not reported as a barrier to the implementation of clinical pharmacy.
Regarding the participants’ answers for each questionnaire item grouped by graduation year, it is to be noted that although lack of sufficient time, experience, and training are especially reported by participants with graduation years between 2000 and 2010 as shown in Figure 2, such results may not have scientific reflections since this category of participants constitute only about a tenth of the total participants in this study as demonstrated in Table 1. The responses of the category of participants with graduation year between 2016 and 2018, who constitute more than half of the whole participants, did not significantly differ from the responses of the other category of participants with graduation year between 2011 and 2015, who represent about a third of the whole participants. This indicates that graduation year did not affect the participants’ responses for each questionnaire item. On the other hand, as indicated in Figure 3, the percentage of participants with an average score of 4 or more to the whole questionnaire was higher in the category with graduation year between 2011 and 2015 representing more than 30% of the total participants indicating that such category of participants believe that many challenges are facing the proper implementation of clinical pharmacy in Egypt, compared to the other two categories of participants.
In a recently published review, fifty-three factors were identified as barriers to the implementation of clinical pharmacy in different hospitals around the world, and the most cited influencing factors were distributed across four domains; attitudinal, political, technical, and administrative.33 The barriers reported in this study fall within the technical and administrative domains and the results of this study are in agreement with the conclusion of such review in that the factors are mainly related to the level of the “pharmacist” group (pharmacist, healthcare team, patient, institution, and national organization), and that “clinical skills” and “time to implement clinical pharmacy services” are influencing factors.
CONCLUSION
Some factors are key players in the implementation of clinical pharmacy in Egyptian hospitals. Working on resolving such barriers, should improve clinical pharmacy practice which will positively reflect on patient care services at the national level.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector.
CONFLICTS OF INTEREST
The authors declare not relevant conflicts of interest or financial relationships.
AUTHOR’S CONTRIBUTIONS
Amani E. Khalifa: Project idea, design, management, conceptualization, methodology, writing-review and editing; Mohamed Kamal Eldin: Principle investigation, data collection, writing-review and editing. Marwan MohyEldin: investigation, data collection, writing-review; Gehad Amgad Zaytoun: investigation, data collection, writing-review; Mahmoud Abo Elmaaty: investigation, data collection, writing-review and editing; Mahmoud Hamza: data processing, statistical analysis, and graphical presentation; Sally Fikry: administration, writing-review and editing; Sherif Kamal: administration, writing-review and editing; Sherif Abouelnaga: supervision, review.
Contributor Information
Mohamed Kamal Eldin, Former Resident in the International Pharmacy Practice Residency (IPPR) program, currently Clinical Pharmacist at the Children Cancer Hospital in Egypt 57357 (CCHE 57357), Cairo, Egypt. mohamed.kamaleldin@57357.org.
Marwan Mohyeldin, Former Resident in the International Pharmacy Practice Residency (IPPR) program, currently Clinical Pharmacist at the Children Cancer Hospital in Egypt 57357 (CCHE 57357), Cairo, Egypt. marwan.mohyi@57357.org.
Gehad Amgad Zaytoun, Former Resident in the International Pharmacy Practice Residency (IPPR) program, currently Clinical Pharmacist at the Children Cancer Hospital in Egypt 57357 (CCHE 57357), Cairo, Egypt. gehadzaitoon@ymail.com.
Mahmoud Abo Elmaaty, Former Resident in the International Pharmacy Practice Residency (IPPR) program, Researcher in Beni-Suef University, currently Clinical Pharmacist at the Children Cancer Hospital in Egypt 57357 (CCHE 57357), Cairo, Egypt. mahallawy_90@yahoo.com.
Mahmoud Hamza, Biostatistician at CCHE 57357, Cairo, Egypt. mahmoud.hamza@57357.org.
Sally Fikry, Director of Residency Program at CCHE 57357, Cairo, Egypt. sally.fikry@57357.org.
Sherif Kamal, Chief Clinical Pharmacist at CCHE 57357, Cairo, Egypt. sherif.kamal@57357.org.
Amani E. Khalifa, Former Acting Dean and Vice Dean, Faculty of Pharmacy, Ain Shams University (ASU). Currently, the Advisor to the President of ASU for the New Nonprofit ASU Project, Cairo, Egypt. advisorp.newuniv@asu.edu.eg ; aekhalifa@hotmail.com
Sherif Abouelnaga, Professor of Pediatric Oncology, the National Cancer Institute, Cairo University, and the CEO of CCHE 57357, Cairo, Egypt. snaga@57357.com.
References
- 1.Preslaski CR, Lat I, MacLaren R, et al. Pharmacist contributions as members of the multidisciplinary ICU team. Chest. 2013;144(5):1687–1695. doi: 10.1378/chest.12-1615. [DOI] [PubMed] [Google Scholar]
- 2.Berenguer B, La Casa C, de la Matta MJ, et al. Pharmaceutical care:past, present and future. Curr Pharm Des. 2004;10(31):3931–3946. doi: 10.2174/1381612043382521. [DOI] [PubMed] [Google Scholar]
- 3.Tegegn HG, Abdela OA, Mekuria AB, et al. Challenges and opportunities of clinical pharmacy services in Ethiopia:A qualitative study from healthcare practitioners'perspective. Pharm Pract. 2018;16(1):1121. doi: 10.18549/PharmPract.2018.01.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Penm J, Moles R, Wang H, et al. Factors affecting the implementation of clinical pharmacy services in China. Qual Health Res. 2014;24(3):345–356. doi: 10.1177/1049732314523680. [DOI] [PubMed] [Google Scholar]
- 5.Ghazal R, Hassan NAG, Ghaleb O, et al. Barriers to the implementation of Pharmaceutical Care into the UAE community pharmacies. IOSR J Pharm. 2014;4(05):68–74. doi: 10.9790/3013-0405068074. [DOI] [Google Scholar]
- 6.Al-azzam SI, Shara M, Alzoubi KH, et al. Implementation of clinical pharmacy services at a university hospital in Jordan. Int J Pharm Pract. 2013;21(5):337–340. doi: 10.1111/ijpp.12009. [DOI] [PubMed] [Google Scholar]
- 7.Agaceta C, Diano G, Lintag M, et al. Perceived barriers to the implementation of pharmaceutical care among pharmacists in private and government hospitals in Metro Manila. Int J Mol Sci Res. 2014;5(08):436–440. [Google Scholar]
- 8.Abu-Gharbieh E, Fahmy S, Rasool BA, et al. Attitudes and perceptions of healthcare providers and medical students towards clinical pharmacy services in the United Arab Emirates. Trop J Pharm Res. 2010;9(5):421–430. doi: 10.4314/tjpr.v9i5.61050. [DOI] [Google Scholar]
- 9.Alcântara TDS, Onozato T, Araújo Neto FC, et al. Perceptions of a group of hospital pharmacists and other professionals of the implementation of clinical pharmacy at a high complexity public hospital in Brazil. BMC Health Serv Res. 2018;18(1):242. doi: 10.1186/s12913-018-3036-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santos Júnior GAD, Onozato T, Rocha KSS, et al. Integration of clinical pharmacy services into the Brazilian health system using Problematization with Maguerez Arc. Res Social Adm Pharm. 2019;15(2):173–181. doi: 10.1016/j.sapharm.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Foppa AA, Martins GA, Nascimento RF, et al. Experiential education in the pharmacy undergraduate curricula in Brazil. Pharm Pract. 2020;18(1):1738. doi: 10.18549/PharmPract.2020.1.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhagavathula AS, Sarkar BR, Patel I. Clinical pharmacy practice in developing countries:focus on India and Pakistan. Arch Pharma Pract. 2014;5(2):91–94. doi: 10.4103/2045-080X.132661. [DOI] [Google Scholar]
- 13.Patel H, Gurumurthy P. Implementation of clinical pharmacy services in academic oncology practice in India. J Oncol Pharm Pract. 2017;25(2):369–381. doi: 10.1177/1078155217739684. [DOI] [PubMed] [Google Scholar]
- 14.Khan TM. Challenges to pharmacy and pharmacy practice in Pakistan. Australas Med J. 2011;4(4):230–235. doi: 10.4066/AMJ.2011.488. [DOI] [Google Scholar]
- 15.Faller EM, Cruz–Bacayo MFD, Abustan AB. Competency assessment of clinical pharmacy education in the Philippines:a basis for curriculum framework. World J Pharm Pharmaceut Sci. 2016;5(3):215–226. [Google Scholar]
- 16.Ongpoy Jr RC, David PP, Capistrano NB, et al. Revisiting the Philippine BS Pharmacy Curriculum After 13 Years:A Survey on Pharmacist Practitioners for the Upcoming Curriculum Revision. Eur J Edu Stud. 2019;6(4):38–52. doi: 10.5281/zenodo.3293680. [DOI] [Google Scholar]
- 17.Zairina E, Khotib J, Ardianto C, et al. Unity in Diversity and the Standardisation of Clinical Pharmacy Services:Proceedings of the 17th Asian Conference on Clinical Pharmacy (ACCP 2017) Yogyakarta, Indonesia:CRC Press. 2017 [Google Scholar]
- 18.Faller EM, Hernandez MT, Hernandez AM, et al. Perception towards the Standardization of Competency Assessment Tools among Clinical Pharmacists in the Philippines. Indian J of Pharmaceut Edu Res. 2019;53(1):48–53. doi: 10.5530/ijper.53.1.7. [DOI] [Google Scholar]
- 19.Lemay J, Waheedi M, Al-Taweel D, et al. Clinical pharmacy in Kuwait:Services provided, perceptions and barriers. Saudi pharmaceut J. 2018;26(4):481–486. doi: 10.1016/j.jsps.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katoue MG, Awad AI, Schwinghammer TL, et al. Pharmaceutical care in Kuwait:hospital pharmacists'perspectives. Int J Clin Pharm. Int J Clin Pharm. 2014;36(6):1170–1178. doi: 10.1007/s11096-014-0013-z. [DOI] [PubMed] [Google Scholar]
- 21.Auta A, Strickland-Hodge B, Maz J. Challenges to clinical pharmacy practice in Nigerian hospitals:a qualitative exploration of stakeholders'views. J Eval Clin Pract. 2016;22(5):699–706. doi: 10.1111/jep.12520. [DOI] [PubMed] [Google Scholar]
- 22.Ekpenyong A, Udoh A, Kpokiri E, et al. An analysis of pharmacy workforce capacity in Nigeria. J Pharm Policy Pract. 2018;11:20. doi: 10.1186/s40545-018-0147-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bilal AI, Tilahun Z, Gebretekle GB, et al. Current status, challenges and the way forward for clinical pharmacy service in Ethiopian public hospitals. BMC Health Serv Res. 2017;17(1):359. doi: 10.1186/s12913-017-2305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryan M, Shao H, Yang L, et al. Clinical pharmacy education in China. Am J Pharm Educ. 2008;72(6):129. doi: 10.5688/aj7206129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Penm J, Li Y, Zhai S, et al. The impact of clinical pharmacy services in China on the quality use of medicines:a systematic review in the context of China's current healthcare reform. Health Policy Plan. 2014;29(7):849–872. doi: 10.1093/heapol/czt067. [DOI] [PubMed] [Google Scholar]
- 26.Qin SB, Zhang XY, Fu Y, et al. The impact of the clinical pharmacist-led interventions in China:A systematic review and Meta-Analysis. Int J of Clin Pharm. 2020;42(2):366–377. doi: 10.1007/s11096-020-00972-y. [DOI] [PubMed] [Google Scholar]
- 27.Brazinha I, Fernandez-Llimos F. Barriers to the implementation of advanced clinical pharmacy services at Portuguese hospitals. Int J Clin Pharm. 2014;36(5):1031–1038. doi: 10.1007/s11096-014-9991-0. [DOI] [PubMed] [Google Scholar]
- 28.Aperta J, Batista A. Education, and training for hospital pharmacists in Portugal. Eur J Hosp Pharm. 2012;19(4):409–410. doi: 10.1136/ejhpharm-2012-000151. [DOI] [Google Scholar]
- 29.Ribeiro N, Mota-Filipe H, Guerreiro MP, et al. Primary health care policy and vision for community pharmacy and pharmacists in Portugal. Pharm Pract. 2020;18(3):2043. doi: 10.18549/PharmPract.2020.3.2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sabry NA, Farid SF. The role of clinical pharmacists as perceived by Egyptian physicians. Int J Pharm Pract. International Journal of Pharmacy Practice. 2014;22(5):354–359. doi: 10.1111/ijpp.12087. [DOI] [PubMed] [Google Scholar]
- 31.Elmaaty MA, Elberry AA, Hussein RR, et al. Applicability of American College of Clinical Pharmacy (ACCP) competencies to clinical pharmacy practice in Egypt. Pharm Pract (Granada) 2020;18(3):1951. doi: 10.18549/PharmPract.2020.3.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdel-Latif MM, Sabra K. Clinical pharmacy practice in Egyptian hospitals. Am J Health-Syst Pharm. 2016;73(1):e63–e66. doi: 10.2146/ajhp150250. [DOI] [PubMed] [Google Scholar]
- 33.Onozato T, Francisca DSCC, Milhome da CFAG, et al. Factors influencing the implementation of clinical pharmacy services for hospitalized patients:A mixed-methods systematic review. Res Social Adm Pharm. 2020;16(4):437–449. doi: 10.1016/j.sapharm.2019.06.018. [DOI] [PubMed] [Google Scholar]