Pediatric heart diseases (HD) affect 1% of school-age children, who experience increased risk of neuropsychological issues linked to poor educational outcomes.1 In children with HD, common neuropsychological delays occur in areas of cognition, learning, language, executive functioning, attention, behavior, social-emotional adjustment, and motor skills.1 These delays often limit final educational attainment, employment, lifelong earnings, and overall quality of life among children with HD.1 Unlike medical conditions with obvious physical effects, HD is an invisible condition where surgery scars hide beneath clothing. Without medical knowledge about a child’s particular illness, school staff may overlook subtle neuropsychological deficits, academic limitations, and school support needs.
To identify neurocognitive concerns and provide recommendations for schools about the cardiac patients’ educational challenges, serial neuropsychological evaluations are recommended.1 However, schools do not always implement recommendations for academic supports from hospital-based psychologists, suggesting a gap in appropriate care coordination and delivery.2
To address such gaps, some hospitals add school liaison responsibilities to the role of social work or case management, who use a consultation-based approach to respond to school concerns raised by patients’ families. While hospital clinic staff have substantial knowledge in their professional disciplines, they often lack sufficient expertise in the field of education to provide comprehensive school recommendations.3 Although some hospitals offer school intervention programs for disease populations such as childhood cancer, effective intervention protocols, and published standards for these services are lacking.4 Most traditional programs focus services on school reentry postdisease onset or hospitalization4 but rarely provide follow-up support postschool reintegration. Meanwhile, neuropsychological deficits may arise at different stages from birth to adulthood in association with medical changes and increasing school expectations.1
Goals and Vision of the Program
The Educational Achievement Partnership Program’s (EAPP) goal is to improve long-term health and academic outcomes of children with HD by integrating health care management and education planning into multidisciplinary care teams. As a novel health service led by experienced educators, the EAPP is uniquely positioned to transform medical and educational paradigms by identifying health and academic problems in a clinical environment and conducting consultative interventions with schools. The EAPP’s mission is to advance long-term educational achievement in children with HD through collaboration, knowledge, advocacy, and commitment and provide every child the opportunity to reach their optimal potential.
Local Challenges in Implementation
The fundamental challenges in building a cardiac EAPP included lack of an effective care coordination protocol, published standards, and validated tools for hospital-based school support services.4 Without available references for hospital-based EAPP structure, clinical operations, and outcome measures, the essential components of an EAPP needed to be developed and tested.
Design of the Initiative
Each phase of program development (structure, operations, and outcomes) involved several key steps: investigation, solution, trial, optimization, data analysis, refinement, standardized implementation, and identification of new challenges. These steps were conducted while providing school support services to >700 referred patients over a 7-year period from 2015 to 2021.
Implementation of the Initiative
Program Structure
Program structure development aimed to establish staffing needs and define EAPP’s role within patient care. Because EAPP advances academic achievement by providing recommendations for school health and education supports, the program is staffed by high level educators who balance expertise in identifying child HD-related needs with educational knowledge and credibility. EAPP specialists hold master’s degrees in education and receive training in cardiac conditions and related neuropsychological deficits. A single specialist serves ≈75 new patients annually with a total intervention cost per patient of ≈$1000 (based on a specialist annual salary of ≈$75 000).
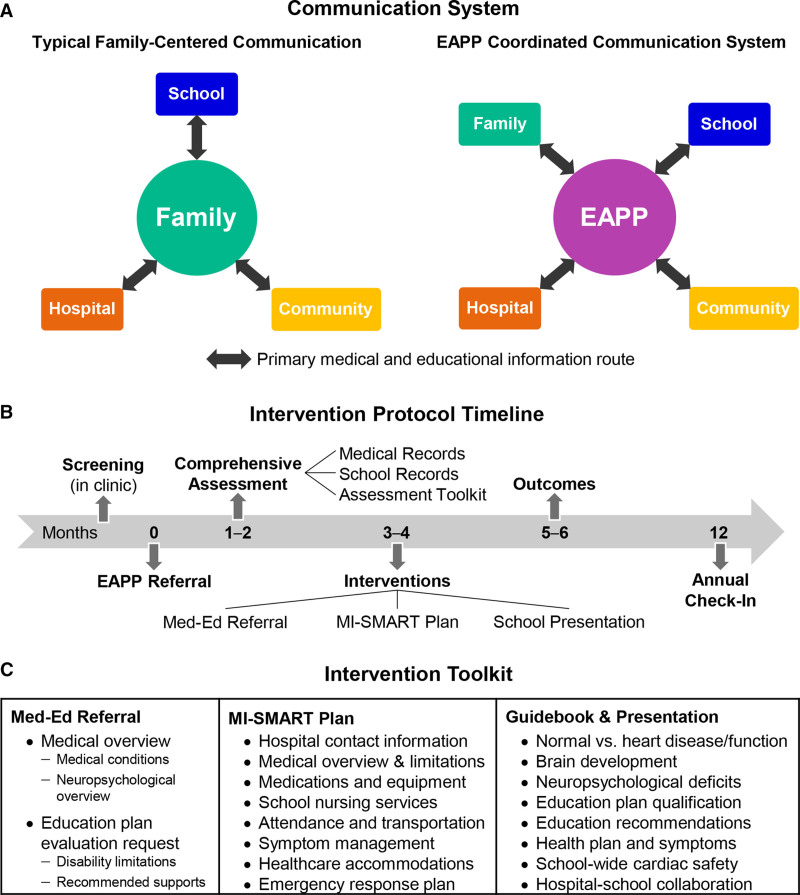
EAPP was conceptualized to address the lack of an effective school support platform in traditional hospital and school models. Under a typical family centered communication model (Figure [A], left), patients’ families are burdened with the responsibility of communicating their child’s medical and educational needs among key stakeholders (ie, school, hospital, and community personnel). While families have expertise in their children’s health and learning, they can be ill-equipped to communicate technical medical terminology and connect neuropsychological sequelae when navigating the complexities of education plan qualification. Under the EAPP’s novel coordinated communication system (Figure [A], right), the EAPP functions as the central information hub, translating medical reports into language understandable and actionable by schools, and aiding school implementation of medically recommended learning, behavior, and health supports.
Figure.
Key components of building an Educational Achievement Partnership Program (EAPP). A, Communication system. B, Intervention protocol timeline. C, Intervention toolkit: Medically-Informed Education Plan Referral Letter (Med-Ed Referral), Medically-Informed School Healthcare and Recommended Treatment Plan (MI-SMART Plan), and School Care Guidebook for Pediatric Heart Disease (Guidebook) and Presentation.
Clinical Operations
Clinical operations development focused on service protocol, assessment, and intervention procedures. The EAPP’s intervention protocol timeline (Figure [B]) includes a comprehensive assessment, a series of intervention steps, and outcome evaluation. Once improvement in school plans and performance is achieved, patients transition into annual follow-up.
The EAPP’s standardized assessment toolkit includes 2 internal tracking tools (intervention status and school impact), 4 structured phone interviews (2 family, 1 patient, and 1 teacher), and 1 school nurse survey. Patient data collected through these assessments is stored in a Research Electronic Data Capture database, a HIPAA-compliant web-based application. Collectively, assessment tools are used to comprehensively evaluate school support needs across 18 key intervention domains (Supplemental Material I) that span school health, developmental progress, psychosocial adjustment, and academic skills.
The EAPP’s intervention toolkit includes: a Medically-Informed Education Plan Referral (Med-Ed Referral) Letter, Medically-Informed School Healthcare Management and Recommended Treatment Plan (MI-SMART Plan), and School Care Guidebook Presentation (Figure [C]). The Med-Ed Referral Letter describes the impact of the patient’s cardiac condition on 4 areas of functioning (health, brain development, risk of neuropsychological deficits, and educational challenges). These letters contain 2 key sections: a medical overview (in laymen’s terms) and an education plan evaluation request (with support recommendations). Importantly, Med-Ed Referrals follow education plan format/language and are sent directly to schools for patients who need education supports.
All cardiac patients are provided recommendations for an Individualized School Health Plan (ISHP) via the EAPP’s MI-SMART Plan. MI-SMART Plans include guidelines for cardiac symptom management, health care accommodations, and other critical supports. For patients requiring both education plans and ISHPs, the Med-Ed Referral and MI-SMART Plan are combined into a single document (see Supplemental Material II for template).
The EAPP’s education and ISHP recommendations are further explained during presentations at patients’ schools, supplemented by a customized visual aid—the EAPP’s School Care Guidebook for Pediatric Heart Disease (Supplemental Material III). The Guidebook Presentation uses images to explain the difference between normal heart function and the patient’s specific type of HD and highlight the impact of pediatric HD on the 4 areas of patient functioning.
Outcome Measures
The EAPP developed measures to evaluate intervention outcomes. The EAPP’s Impact Tracking tool stores key data from preintervention and postintervention school health and education plans, report cards, and attendance records, which are compared to objectively measure school plan and performance changes. The EAPP’s outcome toolkit has 4 surveys that are completed by the family, patient, teacher, and school nurse. The survey questions collect subjective feedback about the impact of the intervention, present level of challenges, and performance across the same 18 key intervention domains that were evaluated during the assessment phase.
Success of the Initiative
Several operational analyses were conducted from 2017 to 2020 to examine the relationship between EAPP services and outcomes in children with HD. Preliminary data from a 2020 cohort of 75 cardiac patients suggests families and schools were motivated to partner with the EAPP: 99% of families and 97% of school staff completed assessment interviews and surveys.
Pilot data from a 2017 cohort of 61 cardiac patients who received complete interventions was evaluated to determine the impact of EAPP services on education plans and school performance. Preintervention, 13 patients (21%) had education plans. The EAPP identified 58 patients (95%) as needing new/expanded education plans; postintervention results indicate this was achieved for 56/58 patients (97%). Additionally, the EAPP identified 50/61 patients (82%) with school performance challenges in areas of attendance, attitude, grades, and psychosocial skills. Postintervention 48/50 patients (96%) improved in ≥1 area assessed. Results suggest the EAPP’s Med-Ed Referral Letters and Guidebook Presentations were associated with improved education plans and school performance.
A 2019 cohort of 74 cardiac patients who received complete interventions and MI-SMART Plan recommendations was evaluated to determine the impact of EAPP services on ISHPs. While only 37 patients (50%) had preintervention ISHPs, all patients needed these plans, and 70 patients (95%) had ISHPs postintervention, with 67/70 of the ISHPs (96%) including recommendations from the EAPP’s MI-SMART Plans. Results support the MI-SMART Plan format as a feasible and useful method for real-world school implementation of hospital-based school health recommendations.
Preliminary outcome survey subjective feedback from a 2020 cohort of 75 cardiac patients has been largely positive. Most stakeholders reported a better understanding the child’s school health and learning support needs. And, many schools requested EAPP services for additional children with HD and other chronic illnesses.
Translation to Other Settings and Future Directions
EAPP services were extended to Complex Care, Oncology, Primary Care, and Neurosciences in 2021. Future expansion will focus on extending EAPP services hospital-wide. The EAPP also plans to seek funding support from state agencies and pursue options for insurance billing to offset costs.
Summary of the Experience, Future Directions, and Challenges
Mere survival of children with HD is not enough; best practices must also improve quality of life and functional outcomes. Over 7 years of program development, EAPP architects created a blueprint for program structure, clinical operations, and outcome measures that can be replicated in other service lines. School support services that follow the EAPP protocol have shown improvements in patients’ school plans and performance. Although the nonbillable nature of this work remains a persisting challenge, the average cost of EAPP services is relatively minor in comparison to the overall benefit. While relatively small sample sizes may limit replication of the initiative’s reported successes, as the EAPP expands, future analyses will target larger cohorts. Taken together, the success of this initiative and the EAPP blueprint offer direction for other hospital-based centers to establish similar school support programs.
Article Information
Acknowledgments
We thank the patients, families, and providers for their participation in this program, and thank the leadership at Children’s Wisconsin’s Herma Heart Institute for their support and dedication to innovations in cardiac care.
Sources of Funding
The project described was supported by the National Center for Advancing Translational Sciences, National Institute of Health. The Educational Achievement Partnership Program is funded by Children's Wisconsin and the Herma Heart Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The project is also funded by the Research and Education Program Fund (a component of the Advancing a Healthier Wisconsin Endowment at the Medical College of Wisconsin), the Children’s Research Institute, and the Herma Heart Institute Innovation Fund at Children’s Wisconsin.
Disclosures
None.
Supplementary Material
Footnotes
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCOUTCOMES.121.008531.
For Sources of Funding and Disclosures, see page 297.
Contributor Information
Christie A. Ruehl, Email: cruehl@chw.org.
Karen C. Stoiber, Email: kstoiber@uwm.edu.
Cheryl L. Brosig, Email: CBrosig@chw.org.
References
- 1.Marino BS, Lipkin PH, Newburger JW, Peacock G, Gerdes M, Gaynor JW, Mussatto KA, Uzark K, Goldberg CS, Johnson WH, Jr, et al. ; American Heart Association Congenital Heart Defects Committee, Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, and Stroke Council. Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management: a scientific statement from the American Heart Association. Circulation. 2012;126:1143–1172. doi: 10.1161/CIR.0b013e318265ee8a [DOI] [PubMed] [Google Scholar]
- 2.Brosig C, Yang K, Hoffmann RG, Dasgupta M, Mussatto K. The role of psychology in a pediatric outpatient cardiology setting: preliminary results from a new clinical program. J Clin Psychol Med Settings. 2014;21:337–346. doi: 10.1007/s10880-014-9404-5 [DOI] [PubMed] [Google Scholar]
- 3.Karpook J, Werner M. Five keys to success: advancing care models for children with complex medical needs. Accessed online August 27, 2020 at: http://www.chartis.com/resources/files/Advancing-Care-Models-for-Children-with-Complex-Medical-Needs-Final-indd-002.pdf.
- 4.Canter KS, Roberts MC. A systematic and quantitative review of interventions to facilitate school reentry for children with chronic health conditions. J Pediatr Psychol. 2012;37:1065–1075. doi: 10.1093/jpepsy/jss071 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.