Abstract
The aim of this study was to evaluate the clinical need and impact of socket preservation to protect the bone for future dental implant placement. Moreover, we aimed to list down various methods of socket preservation by going through randomized clinical trials. We searched PubMed, Google Scholar, and Cochrane databases for all relevant publications, where researchers compared various methods and tools for socket preservation. All eight randomized controlled trials mentioned several methods that are helpful in preserving bone levels both horizontally and vertically. The studies included in this systematic review demonstrate that each material has certain efficacy in preserving the socket after tooth extraction for future implant placement. Socket preservation methods and materials are effective in preparing patients for future prostheses.
Keywords: implant, randomized controlled trial, socket, tooth extraction
INTRODUCTION
Tooth extraction affects masticatory efficiency and causes homeostatic and structural changes in periodontal tissues, leading to alveolar ridge atrophy. Alveolar ridge preservation (ARP) is carried out to avoid ridge resorption after extraction [1, 2]. In the past two decades, many treatment choices were mentioned, such as socket grafting with a biomaterial alone interposing a barrier element. However, there is no resolution regarding the best method for socket preservation: autogenous, allogenic, or alloplastic [2]. Conserving the alveolar ridge is effective but technically delicate, requiring specific surgical skills [1–3]. Still, there is insufficient proof regarding the success of these techniques and the advantages of one method over the other. Presently conflicting observations are reported by researchers regarding the use of grafting material for ARP to prevent alveolar ridge resorption [2, 4, 5].
Our research question aims to identify the effect of various socket preservation materials and methods on the maintenance of ridge levels among patients requiring future prostheses.
This systematic review was carried out to evaluate the clinical need for socket preservation to preserve bone for future placement of a dental implant. Moreover, we aimed to list down various methods of socket preservation by going through randomized clinical trials (RCT). The target audience of this systematic review includes periodontists as well as prosthodontists.
MATERIAL AND METHODS
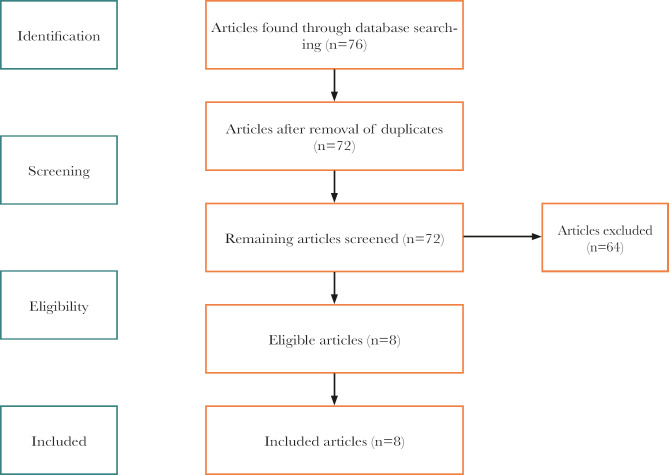
PubMed, Google Scholar, and Cochrane were searched for all relevant publications where the researchers compared various methods and tools for socket preservation. The keywords used were “socket preservation”, “alveolar ridge preservation”, and “bone grafts”. The following search resulted in a total of 76 citations found. After adjusting for duplicates, 72 publications remained. Next, the abstracts of the articles were reviewed, after which 64 studies were removed.
Inclusion criteria: The following criteria were considered essential for the inclusion into the systematic review: (1) randomized control trials, (2) human studies, (3) included the previously mentioned keywords, (4) English language of publication, (5) trials focusing on socket preservation methods and results.
Exclusion criteria: (1) case-control studies, (2) cross-sectional studies, (3) article language other than English, (4) in vitro studies, (5) cohort studies, (6) animal studies.
We used the PRISMA flowchart to report the information received during the examination. Selçuk (2019) [5] highlights that PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) is used to improve transparency in systematic reviews. Therefore, this systematic review adhered to the PRISMA guidelines to eliminate bias and ensure successful completion. Figure 1 represents the PRISMA chart demonstrating various phases of the systematic review.
Figure 1.
PRISMA flowchart.
RESULTS
All studies included (n=8) were thoroughly reviewed, and their findings will be presented in detail in this section. The first study discussed was performed by Avila-Ortiz et al. [1], who completed alveolar ridge preservation using bone allografts and non-absorbable membrane vs. extraction only. Their findings suggest that the ARP method was better than the extraction-only option. As far as the linear bone outcomes were concerned, a mean horizontal crestal width change of 1.07 mm (95% CI, −1.49 to −0.64; P<0.0001). In the same way, there was a noteworthy change in ΔBRH (Buccal Ridge Height) as the median ΔBRH was 0.61 mm (IQR, 0.46 to 0.94) in ARP.
The second study [6] used a full thickness mucoperiosteal flap and a flapless procedure. The results revealed that the changes of the buccolingual bone width were 3.5±0.9 mm for the flap group and 1.7±0.6 mm for the flapless group (p<0.001). In what concerns the vertical bone (VB), the statistical analysis showed only one significant comparison (p=.0105) for VB in the flapless group (1.1±0.9 mm), whereas, in the flapped group, the value obtained for VB was 0.6±0.7 mm. The third study was conducted by Meloni et al. [7], who suggested that the epithelial connective tissue graft led to 0.26 mm bone loss vertically and 1.60 mm horizontally. The porcine collagen matrix led to a vertical loss of 0.31 mm bone and 1.47 mm horizontally.
The study conducted by Guarnieri et al. [8] used three techniques, including extraction sockets with spontaneous bleeding (S), extraction sockets covered by collagen membrane alone (M), and extraction sockets grafted with porcine-derived bone (GM). Results showed that the S group observed 2.13 mm vertically and 3.96 mm horizontally; the M group observed 0.58 mm vertically and 0.91 mm horizontally; the GM group observed 0.31 mm vertically and 0.91 mm horizontally.
Maiorana et al. [9] used demineralized bovine bone mineral and covered it with a porcine-derived non-crosslinked collagen matrix. The findings revealed resorption of 1.21 mm horizontally and 0.46 mm vertically.
Machtei et al. [10] used biphasic calcium sulfate/hydroxyapatite (BCS/HA); bovine-derived xenograft (BDX), or no grafting (control group). Their results showed resorption of 0.65 mm in BCS/HA, 0.25 mm in BDX, and 1.71 mm in the control group were observed vertically. At the same time, 0.5 mm in BCS/HA, 1.56 mm in BDX, and 6 mm in the control group were observed horizontally.
The study by de Carvalho Formiga et al. [11] used dense PTFE membranes with and without xenograft material. Results revealed changes in the buccal plate: control group 0.46 mm, test group 0.91 mm; and alveolar height: control group −0.41 mm, test group 0.35 mm were observed.
Finally, the study by Cardaropoli et al. [12] used extraction alone vs. bovine bone mineral and collagen membrane. Findings revealed that 1.04 mm (width) and 0.46 mm (height) were observed in the experiment group. In contrast, 4.48 mm (width) and 1.54 mm (height) were observed in the extraction alone group. The summary of the studies is described in Table 1.
Table 1.
Summary of the studies included in the systematic review.
| NO | Article (Reference) | Inclusion criteria | Methodology | Results and findings |
|---|---|---|---|---|
| 1. | Avila-Ortiz et al. [1] | RCT, human studies, socket preservation methods, and results | Alveolar Ridge Preservation (ARP) using bone allograft, non-absorbable membrane vs. only tooth extraction | Horizontal crestal width change: -1.07mm Median ΔBRH was 0.61 mm Median ΔLRH was 0.47 mm |
| 2. | Barone et al. [6] | RCT, human studies, socket preservation methods, and results | Full-thickness mucoperiosteal flap vs. a flapless procedure | Epithelial connective tissue graft: Vertical bone loss: 0.26 mm Horizontal: 1.60 mm Porcine collagen matrix: Vertical: 0.31 mm Horizontal: 1.47 mm |
| 3. | Meloni et al. [7] | RCT, human studies, socket preservation methods, and results | Epithelial connective tissue graft vs. porcine collagen matrix | Epithelial connective tissue graft: Vertical bone loss: 0.26 mm Horizontal: 1.60 mm Porcine collagen matrix: Vertical: 0.31 mm Horizontal: 1.47 mm |
| 4. | Guarnieri et al. [8] | RCT, human studies, socket preservation methods, and results | Porcine-derived collagen membrane vs. natural spontaneous healing | Extraction sockets with spontaneous bleeding (S): -2.13 mm vertically and -3.96 mm horizontally Extraction sockets covered by collagen membrane alone (M): -0.58 mm vertically and -0.91 mm horizontally Extraction sockets grafted with porcine-derived bone (GM): -0.31 mm vertically and -0.91 mm horizontally. |
| 5. | Maiorana et al. [9] | RCT, human studies, socket preservation methods, and results | Demineralized bovine bone mineral covered with a porcine-derived non-crosslinked collagen matrix | 1.21 mm horizontally 0.46 mm vertically. |
| 6. | Machtei et al. [10] | RCT, human studies, socket preservation methods, and results | Biphasic calcium sulfate/hydroxyapatite bovine-derived xenograft | 0.65 mm in BCS/HA, 0.25 mm in BDX, and 1.71 mm in the control group (vertically). 0.5 mm in BCS/HA, 1.56 mm in BDX, and 6 mm in the control group were observed horizontally. |
| 7. | de Carvalho Formiga M et al. [11] | RCT, human studies, socket preservation methods, and results | Bone graft vs. blood clots | Buccal plate: control group 0.46 mm, test group 0.91 mm; Alveolar height: control group −0.41 mm, test group 0.35 mm |
| 8. | Cardaropoli et al. [12] | RCT, human studies, socket preservation methods, and results | Extraction alone vs. bovine bone mineral | Experiment group: 1.04 mm (width) and 0.46 mm (height) Extraction alone group: 4.48 mm (width) and 1.54 mm (height) |
Quality assessment
The Cochrane risk of bias assessment method was used to assess the quality of the studies included (Table 2).
Table 2.
Cochrane Risk of bias assessment.
| Random sequence generation | Allocation concealment | Participant and personnel blinding | Outcome Assessment Blinding | Incomplete outcome data | Selective reporting | Other bias | |
|---|---|---|---|---|---|---|---|
| Avila-Ortiz et al., (2020) [1] | |||||||
| Barone et al., (2014) [6] | |||||||
| Meloni et al., (2015) [7] | |||||||
| Guarnieri et al., (2017) [8] | |||||||
| Maiorana et al., (2017) [9] | |||||||
| Machtei et al., (2019) [10] | |||||||
| De Carvalho Formiga et al., (2019) [11] | |||||||
| Cardaropoli et al., 2012 [12] | |||||||
| Low | Unclear | High |
DISCUSSION
This study aimed to list various methods and materials used to preserve the sockets and report the effectiveness of materials and methods discussed. It can be noted from the findings that almost all the methods mentioned produced positive outcomes, especially when the authors compared the findings of the experimental group with the control group. In addition, it was noted that methods such as non-absorbable membrane (dPTFE) and porcine-derived collagen membrane showed positive outcomes when the horizontal bone loss was measured. However, other mentioned materials and methods were effective in preserving vertical bone loss, but not when it comes to horizontal bone loss preservation [9–12]. RCTs using xenografts displayed a considerable diminution of the alveolar bone [1, 7, 13]. It was shown that even the most careful extraction bone resorption results necessitate bone augmentation [14].
CONCLUSIONS
The studies included in this systematic review demonstrate that each material has a certain amount of efficacy in preserving the socket. The methods mentioned above can be used to provide adequate bone preservation both horizontally and vertically, considering the needs of each patient and cost-bearing capability.
ACKNOWLEDGMENTS
Conflict of interest
The authors declare no conflict of interest.
Authorship
AA contributed to conceptualizing and methodology. AAA contributed to methodology and data collection. YA contributed to writing the draft, and NRA contributed to the literature search and data analysis.
REFERENCES
- 1.Avila-Ortiz G, Gubler M, Romero-Bustillos M, Nicholas CL, et al. Efficacy of Alveolar Ridge Preservation: A Randomized Controlled Trial. J Dent Res. 2020 Apr;99(4):402–409. doi: 10.1177/0022034520905660. [DOI] [PubMed] [Google Scholar]
- 2.Faria-Almeida R, Astramskaite-Januseviciene I, Puisys A, Correia F. Extraction Socket Preservation with or without Membranes, Soft Tissue Influence on Post Extraction Alveolar Ridge Preservation: a Systematic Review. J Oral Maxillofac Res. 2019 Sep 5;10(3):e5. doi: 10.5037/jomr.2019.10305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pang C, Ding Y, Hu K, Zhou H, et al. Influence of preservation of the alveolar ridge on delayed implants after extraction of teeth with different defects in the buccal bone. Br J Oral Maxillofac Surg. 2016 Feb;54(2):176–80. doi: 10.1016/j.bjoms.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 4.Hosny MS, Radi IA. Evidence Is Unclear About the Best Material and Technique Required for Alveolar Ridge Preservation for Dental IMPLANT SITE Development. J Evid Based Dent Pract. 2019 Sep;19(3):295–297. doi: 10.1016/j.jebdp.2019.101338. [DOI] [PubMed] [Google Scholar]
- 5.Selçuk AA. A Guide for Systematic Reviews: PRISMA. Turk Arch Otorhinolaryngol. 2019;57(1):57–58. doi: 10.5152/tao.2019.4058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barone A, Toti P, Piattelli A, Iezzi G, et al. Extraction socket healing in humans after ridge preservation techniques: comparison between flapless and flapped procedures in a randomized clinical trial. J Periodontol. 2014 Jan;85(1):14–23. doi: 10.1902/jop.2013.120711. [DOI] [PubMed] [Google Scholar]
- 7.Meloni SM, Tallarico M, Lolli FM, Deledda A, et al. Postextraction socket preservation using epithelial connective tissue graft vs. porcine collagen matrix. 1-year results of a randomised controlled trial. Eur J Oral Implantol. 2015 Spring;8(1):39–48. [PubMed] [Google Scholar]
- 8.Guarnieri R, Stefanelli L, De Angelis F, Mencio F, et al. Extraction Socket Preservation Using Porcine-Derived Collagen Membrane Alone or Associated with Porcine-Derived Bone. Clinical Results of Randomized Controlled Study. J Oral Maxillofac Res. 2017 Sep 30;8(3):e5. doi: 10.5037/jomr.2017.8305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maiorana C, Poli PP, Deflorian M, Testori T, et al. Alveolar socket preservation with demineralised bovine bone mineral and a collagen matrix. J Periodontal Implant Sci. 2017 Aug;47(4):194–210. doi: 10.5051/jpis.2017.47.4.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Machtei EE, Mayer Y, Horwitz J, Zigdon-Giladi H. Prospective randomized controlled clinical trial to compare hard tissue changes following socket preservation using alloplasts, xenografts vs. no grafting: Clinical and histological findings. Clin Implant Dent Relat Res. 2019 Feb;21(1):14–20. doi: 10.1111/cid.12707. [DOI] [PubMed] [Google Scholar]
- 11.de Carvalho Formiga M, Dayube URC, Chiapetti CK, de Rossi Figueiredo D, Shibli JA. Socket Preservation Using a (Dense) PTFE Barrier with or without Xenograft Material: A Randomized Clinical Trial. Materials (Basel) 2019 Sep 8;12(18):2902. doi: 10.3390/ma12182902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L, Cardaropoli G. Socket preservation using bovine bone mineral and collagen membrane: a randomized controlled clinical trial with histologic analysis. Int J Periodontics Restorative Dent. 2012 Aug;32(4):421–30. [PubMed] [Google Scholar]
- 13.Jung RE, Sapata VM, Hämmerle CHF, Wu H, et al. Combined use of xenogeneic bone substitute material covered with a native bilayer collagen membrane for alveolar ridge preservation: A randomized controlled clinical trial. Clin Oral Implants Res. 2018 May;29(5):522–529. doi: 10.1111/clr.13149. [DOI] [PubMed] [Google Scholar]
- 14.Stumbras A, Kuliesius P, Januzis G, Juodzbalys G. Alveolar Ridge Preservation after Tooth Extraction Using Different Bone Graft Materials and Autologous Platelet Concentrates: a Systematic Review. J Oral Maxillofac Res. 2019 Mar 31;10(1):e2. doi: 10.5037/jomr.2019.10102. [DOI] [PMC free article] [PubMed] [Google Scholar]