Abstract
Aims
During the Covid‐19 epidemic, many countries imposed population lockdown. This study aimed to analyse diabetic foot ulcer (DFU) evolution of outpatients between the lockdown period and 1 month after its end.
Materials and Methods
We conducted a prospective, observational, single‐centre study without modification of care. All patients who followed up for a DFU in the study centre between 15 April 2020 and 11 May 2020 were included. The baseline assessment occurred 4 weeks after the beginning of lockdown and the follow‐up visit 4–6 weeks after easing of lockdown. The primary analysis was based on the Site, Ischaemia, Neuropathy, Bacterial infection, Area, Depth (SINBAD) classification.
Results
Twenty‐seven patients were included, median 69.4 years, and 25 were followed‐up at easing of lockdown. The median SINBAD score was 2 (interquartile range 1; 3) at inclusion and 1 (1; 2) at easing of lockdown, with a mean change of −0.32 (95% confidence interval −0.93; 0.29). Seventy‐two percent of the population had a stable or improved score between the two visits. The proportion of patients using off‐loading footwear was higher among those whose SINBAD score improved compared to those whose score worsened or remained stable (72%, 44% and 28%, respectively). Diabetes type was linked to DFU prognosis. Five patients (20%) were hospitalized during the follow‐up period.
Conclusion
Lockdown appears to have had a positive effect on DFU if patients remain under the care of their expert wound centre. We believe this effect is related to better compliance with offloading. The wide use of tele‐medicine seems relevant for the follow‐up of DFU.
Keywords: Covid‐19, diabetes, diabetic foot ulcer, healing, lockdown, SINBAD
1. INTRODUCTION
The Covid‐19 epidemic is an unprecedented challenge for the medical profession. Because of its contagiousness, mortality and emerging nature, it has mobilized the medical resources of most developed countries. Many states, in order to contain and control the progression of the disease, have imposed population containment. However, other diseases particularly chronic ones, have not disappeared. Among them, the management of diabetic foot ulcers (DFUs) has represented a logistical and therapeutic challenge. 1 , 2 , 3 , 4
Diabetic foot is a public health problem in its own right, 5 as it is still the leading cause of non‐traumatic amputation in Western countries, 6 DFU's prognosis in terms of mortality and amputation remains reserved. 7 Within multidisciplinary approach, offloading has a central place. 8 Indeed, failure to respect offloading is significantly associated with delayed healing but also with an increased risk of local bacterial infection. 9 However, making compliance with this difficult treatment is an important constraint for patients. 10
The over‐risk of poor evolution, first suspected and then confirmed in people with diabetes people infected with SARS‐Cov‐2, 11 has obliged our expert centre to limit as much as possible the exposure of patients to intra‐hospital travel. In accordance with international recommendations 12 , 13 , 14 and as many other centres, 15 our foot clinic has therefore continued to follow patients via teleconsultation, and for the most serious cases, by face‐to‐face emergency consultations. These protocols have been shown to be effective in reducing the contamination to SARS‐Cov‐2 of patients with DFU. 2 For people with DFU, this period of containment in the midst of a viral pandemic was a plunge into the unknown. As much as the effect of a reduction in the possibilities of mobility may give hope for better compliance with offloading, the restriction of movement also raises fears of less good nursing care and less support from life‐support workers or any other outside helpers. 16 The elements related to good compliance with offloading are known to be complex to analyse. 17
The effect of lockdown on the evolution of DFU is still insufficiently studied. 18 The decrease in the number of hospitalizations for DFU is widely observed. However, the rate of major amputations has not decreased. 19 , 20 , 21
To our knowledge, no study has reported the evolution of DFU or offloading during this period of lockdown. Therefore, this study aimed to analyse the healing status of patients followed by our foot clinic for DFU 1 month after lockdown and 1 month after the end of it. We included a study of offloading compliance.
2. MATERIALS AND METHODS
2.1. Study design and population
This prospective, monocentric, observational study was carried out at the diabetic foot clinic of Montpellier University Hospital, France. All patients who followed up for a DFU in the study centre between 15 April 2020 and 11 May 2020 were included. A DFU was defined as a trophic ulcer of the lower limb in a patient with diabetes. Exclusion criteria were patients with guardianship, patients unable to understand or answer the physician's interview, and refusals to participate. Patients' care was not modified. The study protocol was approved by the Institutional Review board of Montpellier University Hospital (#202000475). Participants were informed about the study and were free to refuse to take part in the research.
2.2. Follow‐up
The baseline assessment took place during lockdown, at least 4 weeks after the beginning of this period which lasted from 16 March to 11 May 2020 in France. Patients were followed up by our centre before the lockdown began. No follow‐up was started via teleconsultation. Such an initiation could be linked to an increase in mortality. 22 They had a normal follow‐up with no change in management until the baseline assessment when they were included in the study. Appointments have been changed into teleconsultation or maintaining face‐to‐face visits by minimizing cancellations or delays in follow‐up. Due to the movement restrictions, visits were mainly teleconsultations or in person in case of an emergency or if it was impossible to carry out a teleconsultation. The follow‐up visit took place 4–6 weeks after easing of lockdown restrictions. The visits and wound assessment were standardized and made by the same operator. Others were collected from electronic medical records and from consultation or teleconsultation reports.
2.3. Outcomes
Analysis was based on the ulcer classification using the SINBAD (Site, Ischaemia, Neuropathy, Bacterial infection, Area, Depth) score 23 as recommended by the International Working Group for Diabetic Foot (IWGDF) in the follow‐up of DFU. 9 This classification is based on six items, each scored with 0 or 1 point: ulcer site (forefoot [0] or midfoot and hindfoot [1]), ischaemia (intact [0] or reduced [1] pedal blood flow), neuropathy (intact [0] or lost [1] protective sensation), bacterial infection (none [0] or present [1]), area (ulcer <1 cm2 [0] or ≥1 cm2 [1]), and depth (ulcer confined to skin and subcutaneous tissue [0] or reaching muscle, tendon or deeper [1]). The total score ranged from 0 (healed ulcer) to 6 (more severe ulcer).
Off‐loading was evaluated through the use of off‐loading footwear. Patients were asked whether the therapeutic shoes were used for more than half of movements, both indoors and outdoors. Physical activity was assessed by indoor and outdoor walking time. Sedentary time was measured as the mean daily time spent watching screens or reading. Patients were also asked whether they were in charge of household tasks (shopping, cooking, cleaning), alone or not, and whether they had home help. Driving time was also collected. Hospitalizations occurring between the two visits were recorded. Other collected data included the number of persons living in the household, professional activity before lockdown and type of activity, dressing type, and treatments (insulin, oral antidiabetics, antibiotics within the past 2 months, revascularisation in the past 2 months).
2.4. Statistical analysis
Continuous variables were described with means and standard deviation (SD) or median and interquartile range (IQR), depending on the distribution. Qualitative variables were described with numbers and percentages. Mean variation in the SINBAD score between the two visits was calculated, along with its 95% confidence interval (95% CI). To compare qualitative variables between the two visits, we used a Fisher test for paired samples or a CHI‐2 when it was not possible. A Wilcoxon–Mann–Whitney was used for continuous variables. The statistical analysis was performed using the SAS statistical software (version 9.4; SAS Institute).
3. RESULTS
3.1. Population
A total of 27 patients were included during lockdown, and 25 had a follow‐up visit at easing of lockdown restrictions, while 2 patients were lost to follow‐up (Figure 1). Median age was 69.4 years, most patients were males (77.8%) and had type 2 diabetes (81.5%). History of ulcer (77.8%) and of amputation (40.7%) was relatively frequent. Patients' characteristics are described in Table 1. Regarding the personal situation, 27% lived alone while 73% lived with at least another person, and 27%, 50% and 35% of patients, respectively, were in charge of shopping, cooking and cleaning at home.
FIGURE 1.
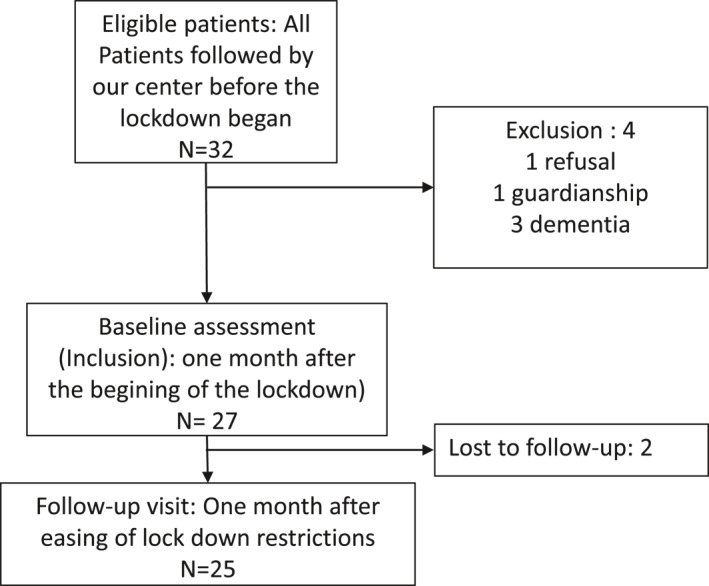
Flow chart of the population
TABLE 1.
Baseline characteristics of the study population
| Variable | N = 27 |
|---|---|
| Age (years), median (IQR) | 69.4 (62.1–75.5) |
| Gender, male | 21 (77.8) |
| BMI (kg/m2), median (IQR) | 29.2 (25.3–34.0) |
| Diabetes type | |
| Type 1 | 3 (11.1) |
| Type 2 | 22 (81.5) |
| Other | 2 (7.4) |
| Diabetes duration (years), median (IQR) | 24 (14–34) |
| Insulin | 21 (77.8) |
| HbA1c (%), median (IQR) | 7.7 (6.9–9.0) |
| eGFR ml/min/1.73 m,2 median (IQR) | 57.5 (28.4–68.0) |
| SINBAD score | |
| 0 | 2 (7) |
| 1 | 9 (33) |
| 2 | 8 (30) |
| 3 | 7 (26) |
| 4 | 1 (4) |
| 5 or 6 | 0 (0) |
| History of ulcer | 21 (77.8) |
| History of amputation | 11 (40.7) |
| Ulcer site | |
| Hindfoot | 5 (18.5) |
| Forefoot | 17 (63.0) |
| Midfoot | 4 (14.8) |
| Stump | 1 (3.7) |
| Dressing type | |
| Alginate | 8 (30) |
| Sucrose octasulfate | 6 (22) |
| Hydrocellular | 5 (19) |
| Others | 6 (22) |
| None | 2 (7) |
| Tobacco (n = 23) | |
| Weaned | 8 (34.8) |
| Active | 7 (30.4) |
| Alcohol | 2 (7.4) |
| High blood pressure (n = 24) | 19 (79.17) |
| Dyslipidaemia (n = 23) | 18 (78.3) |
| Peripheral arterial disease | 24 (88.8) |
| Ischaemic heart disease (n = 22) | 14 (64.6) |
| Colorectal cancer | 4 (14.8) |
Note: Values are numbers (percentages) unless otherwise stated.
Abbreviation: IQR. interquartile range.
3.2. Clinical evolution
Median SINBAD score was 2 (IQR 1; 3) at the baseline visit and 1 (1; 2) at the easing of lockdown restrictions visit, with a mean variation of −0.32 (95% CI −0.93; 0.29) (Table 2). Overall, 72% of the population had a stable or improved score between the two visits. At the lockdown visit, 7% of patients (2/27) had a SINBAD score of 0, while they were 24% (6/25) at the easing of lockdown restrictions visit (Figure S1).
TABLE 2.
SINBAD score during lockdown and easing of lockdown restrictions, and individual variation between the two visits
| SINBAD score | |
|---|---|
| At lockdown (visit 1), median (IQR) | 2 (1; 3) |
| At easing of lockdown restrictions (visit 2), median (IQR) | 1 (1; 2) |
| Individual variation (Δ), mean (95% CI) | −0.32 (−0.93; 0.29) |
| Stable (Δ = 0), n (%) | 7 (28) |
| Improvement, n (%) | 11 (44) |
| Small worsening, n (%) | 7 (28) |
Less patients required antibiotics at easing of lockdown restrictions (n = 3, 13%) than at lockdown (n = 11, 41%) (p = 0.03), while one patient (5%) required revascularization, both at lockdown and at easing of lockdown restrictions. Five patients (20%) were hospitalized during the follow‐up period, including one patient (4%) who required amputation.
The type of diabetes appears as a factor related to the prognosis. Intact protective sensation was related to a worse prognosis according to the SINBAD score (Table 3).
TABLE 3.
Characteristics of the patients according to the evolution of the wound (Improvement of the SINBAD score)
| Improvement (n = 11) | Deterioration or no improvement (n = 14) | p | |
|---|---|---|---|
| Age (years), median (IQR) | 69.9 (55.7–80.6) | 69.6 (63.6–74.7) | 0.64 |
| Gender, male, n (%) | 8 (72.7) | 12 (85.7) | 0.62 |
| BMI (kg/m2), median (IQR) | 28.4 (25.3–30.6) | 29.4 (24.7–34.0) | 0.97 |
| HbA1c (%), median (IQR) | 8.7 (7.5–9.0) | 7.35 (6.9–8.4) | 0.45 |
| eGFR ml/min/1.73 m2, median (IQR) | 63.0 (51.0–76.0) | 56.0 (24.0–65.0) | 0.45 |
| Diabetes type, n (%) | 0.04 | ||
| Type 1 | 3 (12.0) | 0 (0.0) | |
| Type 2 | 8 (32.0) | 12 (48.0) | |
| Other | 0 (0.0) | 2 (8.0) | |
| Diabetes duration (years), median (IQR) | 24.0 (20.0–35.0) | 26.0 (15.0–34.0) | 0.74 |
| Insulin, n (%) | 8 (72.7) | 11 (78.6) | 1 |
| History of ulcer, n (%) | 8 (72.7) | 12 (85.7) | 0.62 |
| History of amputation, n (%) | 6 (54.5) | 3 (21.4) | 0.12 |
| Tobacco (n = 23) | 0.14 | ||
| Weaned | 2 (20.0) | 6 (46.2) | |
| Active | 2 (20.0) | 5 (38.5) | |
| Alcohol | 5 (45.5) | 8 (57.1) | 0.54 |
| Peripheral arterial disease | 9 (81.8) | 13 (92.9) | 0.56 |
| Ischaemic heart disease (n = 22) | 6 (60.0) | 8 (66.7) | 1 |
| SINBAD score | |||
| Ulcer site, n (%) | 0.41 | ||
| Forefoot | 8 (72.7) | 7 (50.0) | |
| Upper | 3 (27.27) | 7 (50.0) | |
| Pedal blood flow intact, at least one palpable pulse, n (%) | 5 (45.45) | 8 (57.14) | 0.85 |
| Protective sensation intact, n (%) | 1 (9.1) | 10 (71.4) | 0.004 |
| Bacterial infection, n (%) | 4 (27.3) | 5 (35.7) | 1 |
| Ulcer ≥1 cm2, n (%) | 2 (18.2) | 5 (35.7) | 0.41 |
| Ulcer reaching muscle, tendon, or deeper, n (%) | 2 (18.2) | 1 (7.1) | 0.56 |
| Exposed bone | 0 (0.0) | 1 (7.14) | 1 |
| Off‐loading footwear, n (%) | |||
| Used | 8 (72.7) | 5 (35.7) | 0.11 |
| Driving, n (%) | 4 (36.4) | 5 (42.9) | 1 |
| Daily walking time (hours), median (IQR) | 1 (0.5; 2) | 0.75 (0–1.5) | 0.39 |
| People living alone, n (%) | 3 (27.3) | 4 (28.6) | 1 |
| Professional activity, n (%) | 3 (27.3) | 2 (14.3) | 0.62 |
| Assistance at home, n (%) | 0.31 | ||
| None | 3 (27.3) | 4 (28.6) | |
| Family | 2 (18.2) | 6 (42.9) | |
| Life assistant | 6 (54.6) | 4 (28.6) | |
| Help with household errands, n (%) | 4 (36.4) | 3 (21.4) | 0.66 |
| Help with cooking, n (%) | 6 (54.6) | 7 (50.0) | 1 |
| Help with cleaning, n (%) | 6 (54.6) | 3 (21.4) | 0.11 |
3.3. Off‐loading and activities
A majority of patients used off‐loading footwear, both at lockdown (73%) and at easing of lockdown restrictions (89%) (p = 0.27), and about half of the patients used them for more than half of their movements (both indoors and outdoors) (Table 4). The proportion of patients using off‐loading footwear tended to be higher among those whose SINBAD score improved compared to those whose score worsened or remained stable (72%, 44% and 28%, respectively; p = 0.11) (Table 3). On the contrary, all seven patients whose ulcer worsened were sedentary for more than 6 h/day during easing of lockdown restrictions, while they were 43% (3/7) among those who were stable and 45% (5/11) among those whose ulcer improved. Patients tended to be slightly more active at easing of lockdown restrictions than at lockdown, although no significant difference was observed (Table 4). The number of patients driving, working and in sick leave did not change between the two visits.
TABLE 4.
Off‐loading and activities
| Lockdown (n = 26) | Easing of lockdown restrictions (n = 18) a | p | |
|---|---|---|---|
| Off‐loading footwear, n (%) | |||
| Used | 19 (73) | 16 (89) | 0.27 |
| Used for more than half of indoor movements | 12 (46) | 10 (56) | 0.54 |
| Used for more than half of outdoor movements | 13 (50) | 10 (56) | 0.72 |
| Driving, n (%) | 10 (39) | 10 (56) | 0.26 |
| Daily walking time (hours), median (IQR) | 1 (0.5; 2) | 1 (0.8–4.5) | 0.48 |
| Sedentary time (reading/screens), n (%) | 0.48 | ||
| <3 h/day | 2 (8) | 4 (22) | |
| 3–6 h/day | 9 (34) | 8 (45) | |
| 6–10 h/day | 7 (27) | 2 (11) | |
| >10 h/day | 8 (31) | 4 (22) | |
| Professional activity, n (%) | 5 (19) | 5 (28) | 1.00 |
| Of which, sick leave | 3 (60) | 3 (60) | 1.00 |
Of the 25 patients followed up at the follow‐up visit, 2 were hospitalized in critical care, 1 passed through hospitalization and was transferred to a rehabilitation centre, 2 had a diagnosis of complete healing prior to the follow‐up visit and had been cleared for off‐loading by the physician, 2 did not have a standardized assessment during their follow‐up visit.
4. DISCUSSION
We report here for the first time the evolution of DFU during the lockdown and the easing of lockdown restrictions periods. We observed an improving trend in the SINBAD score during follow‐up. The proportion of patients wearing an off‐loading shoe seemed to be higher among patients whose SINBAD score improved.
The mechanism of COVID‐19 with its cytokine storm and hypercoagulability in the inflammatory and ischaemic context of DFU was a cause for concern, urging us to exercise caution. 16 The use of high doses of corticosteroids in patients with an infected diabetic foot is also a cause for worry. 24 Thus, COVID‐19 has induced a strong development of tele‐medicine and home care. Shin et al. report, for instance, on their experience in the choice of oral versus intravenous antibiotic therapies, 25 in the application of OVIVA study findings. 26
Our results showed that 72% of patients with a DFU improved or remained stable. This differs from previous observations during the pandemic that didn't show a decrease in major amputation rate. 19 In Caruso et al.'s observation of 25 patients, the risk of amputation among patients admitted into their tertiary care centre for DFU was threefold higher. 19 Hospitalized patients during lockdown had more severe infections, they were more likely to be in emergency care and, finally, the rate of major amputations versus minor amputations seemed to be higher. 21 Furthermore, the return to ‘business as usual’ in terms of the number of hospitalizations for DFUs has been described by Liu et al. as immediate after the end of lockdown. 27
This may be due to the fact that we focussed on a cohort of patients previously followed before the lockdown period. These patients were indeed included in our multidisciplinary approach and follow‐up. For them, management strategies with extensive use of telemedicine do not appear to have challenged their wound healing prognosis. It should be remembered that patients with acute ischaemia or infections, especially soft tissue infections, had closer face‐to‐face visits. Theses ulcers should be managed by a close control to avoid an early deterioration. It also should be noted that all patients had been previously evaluated in a face‐to‐face visit by our team. Telemedicine may represent a risk in the absence of this initial assessment. 22 Therefore, the most urgent situations had already been taken care of. We consequently only studied chronic wounds with a significant impact of offloading on ulcer's prognosis. However, it is likely that there was a delay in the management of patients outside our care network. In this regard, it is noteworthy that foot screening by the general practitioner in patients with diabetes appears to have been one of the elements of monitoring that decreased the most during lockdown. 28 This may suggest a second epidemic at a distance from the reopening of the care system for non‐Covid patients. Interestingly, contrary to the medical community, patients with DFU were much more concerned about the evolution of their DFU than about COVID‐19. 29
Unfortunately, we were not able to measure the evolution of wound size. Due to teleconsultations, wound measurement on photographs was imprecise. However, we used the SINBAD score, which is the score recommended by the IWGDF for monitoring DFU. 9 The main limitation of our study is the small size of the cohort and the absence of comparison to a control group of patients treated during the ‘no lockdown period’. This is a bias unfortunately shared by the cohorts published on this subject to date. 19 Finally, our population is mainly composed of people with peripheral arterial disease. Therefore, we were not able to individualize the ischaemic ulcers from the others. We were not able to conduct a multivariate analysis. This is compensated by its exhaustive nature in our centre and by the fact that all patients had active wounds. It should be noted, however, that our population involved mainly patients with a history of ulcer or amputation, a known factor associated with a higher mortality and amputation rate. In our cohort, patients whose SINBAD score did not improve had a better preserved protective sensation than those who improved. This atypical result is probably due to the high proportion of patients with peripheral arterial disease.
The two analysis moments, 1 month after the beginning of the lockdown and 1 month after the easing of lockdown restrictions, highlight the delayed impact of the lockdown on the evolution of the DFU wounds. The fact that wounds continue to improve despite easing of lockdown restrictions may suggest a memory effect of increased offloading during the lockdown period. Indeed, the proportion of patients using off‐loading footwear was higher among those whose SINBAD score improved compared to those whose score worsened or remained stable. We hypothesize that the lockdown limited the mobility of patients and their relatives. This reduction in mobility may have increased compliance with offloading and thus played a role in the improved prognosis of DFU that we observed in this cohort. However, compliance with offloading at the first visit was not a prognosis factor.
New episodes of lockdown are being ordered all over the world. They are likely to be repeated until we achieve vaccination coverage for the world's population. In any case, the management of this epidemic is a textbook case of the clinical consequences obtained when a population is confined. Lockdown that can occur in the eventuality of a new pandemic, 30 or more classically, anywhere in the world, in the event of a social phenomenon (war, political situation, climatic disaster, etc.) that induces a massive control and lockdown of populations. Lockdown does not appear to compromise DFU prognosis if patients remain under the care of their expert wound centre after a first face‐to‐face evaluation. The wide use of tele‐medicine seems relevant for the follow‐up of DFU. A more in‐depth study of the impact of delays in the initial assessment during the lockdown period, particularly on ischaemic or infected wounds should be conducted. Late referral is known to increase the risk of amputation and mortality due to DFU. 31
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
The study was approved by the ethics committee of Montpellier University Hospital (project number: #202000475) and was realized in accordance with the Helsinki declaration.
AUTHOR CONTRIBUTIONS
Study concept and design: Jean‐Baptiste Bonnet, Ariane Sultan. Acquisition of data: Jean‐Baptiste Bonnet, Abdulkader Jalek, Cécile Elleau, Marie‐Françoise Gras‐Vidal, Julie Pochic, Ariane Sultan. Statistical analysis: Jean‐Baptiste Bonnet, Abdulkader Jalek, Karim Bouchdoug. Study supervision: Antoine Avignon, Ariane Sultan. Writing of the manuscript: Jean‐Baptiste Bonnet, Valérie Macioce, Ariane Sultan. All authors read and approved the final version of the manuscript.
TRANSPARENT PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/dmrr.3520.
Supporting information
Supporting Information S1
ACKNOWLEDGEMENT
The authors wish to thank all the professionals of the diabetic foot unit of Montpellier University Hospital. This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
Bonnet J‐B, Macioce V, Jalek A, et al. Covid‐19 lockdown showed a likely beneficial effect on diabetic foot ulcers. Diabetes Metab Res Rev. 2022;38(4):e3520. 10.1002/dmrr.3520
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Urbančič‐Rovan V. Diabetic foot care before and during the COVID‐19 epidemic: what really matters? Diabetes Care. 2021;44(2):e27‐e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Meloni M, Izzo V, Giurato L, Gandini R, Uccioli L. Management of diabetic persons with foot ulceration during COVID‐19 health care emergency: effectiveness of a new triage pathway. Diabetes Res Clin Pract. 2020;165:108245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jaly I, Iyengar K, Bahl S, Hughes T, Vaishya R. Redefining diabetic foot disease management service during COVID‐19 pandemic. Diabetes Metab Syndr Clin Res Rev. 2020;14(5):833‐838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kelahmetoglu O, Camlı MF, Kirazoglu A, et al. Recommendations for management of diabetic foot ulcers during COVID‐19 outbreak. Int Wound J. 2020;17(5):1424‐1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367‐2375. [DOI] [PubMed] [Google Scholar]
- 6. Lazzarini PA, Pacella RE, Armstrong DG, van Netten JJ. Diabetes‐related lower‐extremity complications are a leading cause of the global burden of disability. Diabetes Med. 2018;35(9):1297‐1299. [DOI] [PubMed] [Google Scholar]
- 7. Ghanassia E, Villon L, Thuan dit Dieudonné J‐F, Boegner C, Avignon A, Sultan A. Long‐term outcome and disability of diabetic patients hospitalized for diabetic foot ulcers. Diabetes Care. 2008;31(7):1288‐1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lazzarini PA, Jarl G, Gooday C, et al. Effectiveness of offloading interventions to heal foot ulcers in persons with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36(S1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schaper NC, van Netten JJ, Apelqvist J, et al. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36:e3266. [DOI] [PubMed] [Google Scholar]
- 10. Macfarlane DJ, Jensen JL. Factors in diabetic footwear compliance. J Am Podiatr Med Assoc. 2003;93(6):485‐491. [DOI] [PubMed] [Google Scholar]
- 11. Wargny M, Potier L, Gourdy P, et al. Predictors of hospital discharge and mortality in patients with diabetes and COVID‐19: updated results from the nationwide CORONADO study. Diabetologia. 2021;64(4):778‐794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. COVID‐19 and Diabetic Foot Disease [Internet]. IWGDF Guidelines. [Cited 2021 Feb 21]. https://iwgdfguidelines.org/covid‐19/ [Google Scholar]
- 13. Oropallo A, Lantis J, Martin A, Al Rubaiay A, Wang N. Wound care during the COVID‐19 pandemic: improving outcomes through the integration of telemedicine. J Wound Care. 2021;30(Sup2):S12‐S17. [DOI] [PubMed] [Google Scholar]
- 14. Meloni M, Bouillet B, Ahluwalia R, et al. Fast‐track pathway for diabetic foot ulceration during COVID‐19 crisis: a document from International Diabetic Foot Care Group and D‐Foot International. Diabetes Metab Res Rev. 2021;37(3):e3396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schmidt BM, Munson ME, Rothenberg GM, Holmes CM, Pop‐Busui R. Strategies to reduce severe diabetic foot infections and complications during epidemics (STRIDE). J Diabet Complicat. 2020;34(11):107691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lipscomb D, Smith AS, Adamson S, Rezazadeh EM. Diabetic foot ulceration in COVID‐19 lockdown: cause for concern or unexpected benefit? Diabet Med. 2020;37(8):1409‐1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jarl G. Methodological considerations of investigating adherence to using offloading devices among people with diabetes. Patient Prefer Adherence. 2018;12:1767‐1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kavitha KV, Deshpande SR, Pandit AP, Unnikrishnan AG. Application of tele‐podiatry in diabetic foot management: a series of illustrative cases. Diabetes Metab Syndr Clin Res Rev. 2020;14(6):1991‐1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Caruso P, Longo M, Signoriello S, et al. Diabetic foot problems during the COVID‐19 pandemic in a tertiary care center: the emergency among the emergencies. Diabetes Care. 2020;43(10):e123‐e124. [DOI] [PubMed] [Google Scholar]
- 20. Lancaster EM, Wu B, Iannuzzi J, et al. Impact of the coronavirus disease 2019 pandemic on an academic vascular practice and a multidisciplinary limb preservation program. J Vasc Surg. 2020;72(6):1850‐1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Casciato DJ, Yancovitz S, Thompson J, et al. Diabetes‐related major and minor amputation risk increased during the COVID‐19 pandemic. J Am Podiatr Med Assoc. 2020. [DOI] [PubMed] [Google Scholar]
- 22. Rasmussen BSB, Froekjaer J, Bjerregaard MR, et al. A randomized controlled trial comparing telemedical and standard outpatient monitoring of diabetic foot ulcers. Diabetes Care. 2015;38(9):1723‐1729. [DOI] [PubMed] [Google Scholar]
- 23. Ince P, Abbas ZG, Lutale JK, et al. Use of the SINBAD classification system and score in comparing outcome of foot ulcer management on three continents. Diabetes Care. 2008;31(5):964‐967. [DOI] [PubMed] [Google Scholar]
- 24. Gutierrez‐Ortiz C, Garcia‐Villasante E, Pinedo‐Torres I. COVID‐19 and diabetic foot: will the lamp burn bright? Int J Low Extremy Wound. 2020;19(2):111. [cited 2021 Feb 22] https://journals.sagepub.com/doi/10.1177/1534734620948764 [DOI] [PubMed] [Google Scholar]
- 25. Shin L, Bowling FL, Armstrong DG, Boulton AJM. Saving the diabetic foot during the COVID‐19 pandemic: a tale of two cities. Diabetes Care. 2020;43(8):1704‐1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Li H‐K, Rombach I, Zambellas R, et al. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019;380(5):425‐436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu C, You J, Zhu W, et al. The COVID‐19 outbreak negatively affects the delivery of care for patients with diabetic foot ulcers. Diabetes Care. 2020;43(10):e125‐e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Coma E, Mora N, Méndez L, et al. Primary care in the time of COVID‐19: monitoring the effect of the pandemic and the lockdown measures on 34 quality of care indicators calculated for 288 primary care practices covering about 6 million people in Catalonia. BMC Fam Pract. 2020;21(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Iacopi E, Pieruzzi L, Goretti C, Piaggesi A. I fear COVID but diabetic foot (DF) is worse: a survey on patients’ perception of a telemedicine service for DF during lockdown. Acta Diabetol. 2021;58(5):587‐593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leong Tan GW, Chandrasekar S, Lo ZJ, et al. Early experience in the COVID‐19 pandemic from a vascular surgery unit in a Singapore tertiary hospital. J Vasc Surg. 2020;72(1):12‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meloni M, Lazaro‐Martínez JL, Ahluwalia R, et al. Effectiveness of fast‐track pathway for diabetic foot ulcerations. Acta Diabetol. 2021;58(10):1351‐1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


