Abstract
Background
Early maladaptive schemas (EMS), as lifelong psychological structures, tend to be associated with psychopathological symptomatology. Previous research has suggested that schemas act as psychological vulnerabilities to stressful life situations, such as the present worldwide COVID‐19 pandemic. In this context, anxiety and psychological distress have been documented as two of the main psychological symptoms associated with the COVID‐19 pandemic. However, the associations between specific EMS and COVID‐19 anxiety remain unexplored. Therefore, this study aims to explore the relationships between EMS, COVID‐19 anxiety as well as other mental health variables such as psychological well‐being, distress and life satisfaction.
Methods
In a cross‐sectional design, 249 individuals (M = 34.2, SD = 12.0) completed several self‐report measures.
Results
EMS from different schematic domains were positively associated with COVID‐19 anxiety and psychological distress and negatively associated with psychological well‐being and life satisfaction. An EMS hierarchical regression model predicted COVID‐19 anxiety. Mistrustfulness and vulnerability to harm and illness mediated the relationships between COVID‐19 anxiety, psychological distress and life satisfaction.
Conclusions
According to these results, mistrustfulness and vulnerability to harm and illness can act as underlying variables for the decrease in mental health associated with the COVID‐19 pandemic.
Keywords: COVID‐19 anxiety, early maladaptive schemas, life satisfaction, mistrustfulness, psychological distress, vulnerability to harm and illness
Key Practitioner Message.
Early Maladaptive Schemas are associated with COVID‐19 Anxiety, Mental Health and Life Satisfaction;
Mistrustfulness and Vulnerability to Harm and Illness schemas and mediate COVID‐19 Anxiety and Mental Health;
Mistrustfulness and Vulnerability to Harm and Illness schemas and mediate COVID‐19 Anxiety and Life Satisfaction;
Mistrustfulness, Vulnerability to Harm and Illness and Pessimism schemas may be viewed as a Core Vulnerability Triad to COVID‐19 Anxiety;
Early Maladaptive Schemas mat be viewed as longitudinal vulnerability factors regarding COVID‐19 Anxiety, Life Satisfaction and Mental Health;
1. INTRODUCTION
The severe acute respiratory syndrome‐related coronavirus 2 (SARS‐CoV‐2) is responsible for the COVID‐19 disease, which was declared on 11 March 2020 by the World Health Organization (WHO, 2020a) as a worldwide pandemic. Flu‐like symptoms, such as fever, shortness of breath, fatigue and cough, were systematically observed by physicians, ranging from moderate to severe (Alimohamadi et al., 2020; Grant et al., 2020; Lopez‐Leon et al., 2021). Severe respiratory failure caused by the COVID‐19 disease has already caused millions of deaths worldwide (WHO, 2020b), expressing difficulties for governments and health agencies in dealing with the rapid spread of a new coronavirus unknown to science. However, several vaccines have by now been developed, and most countries are involved in complete national vaccination programmes (Lindholt et al., 2021; Taylor et al., 2020). In addition to somatic symptoms (e.g., fever and fatigue), COVID‐19 has also been systematically associated to a wide array of psychopathological symptoms, such as depression (Bueno‐Notivol et al., 2021; Qiu et al., 2020), anxiety (Albery et al., 2021; Lee, 2020; Lee et al., 2020), depression and anxiety (Porter et al., 2021; Rondung et al., 2021; Woon et al., 2021), stress (Gasteiger et al., 2021; Varma et al., 2021) and post‐traumatic stress symptoms (PTSS) related to COVID‐19 (Janiri et al., 2021; Tu et al., 2021). Neuropsychiatric sequelae of COVID‐19 related to olfactory impairment (Ho et al., 2021), depression (Ceban et al., 2021) and post‐traumatic stress disorder (PTSD) (Hao et al., 2020) have also been identified. Also, COVID‐19 has been associated with other variables related to mental health, such as social isolation, psychological distress, psychological well‐being and psychological needs (Faustino et al., 2021a; Wang et al., 2021). A recent study on attitudes towards vaccination found that individuals with higher levels of depression and anxiety were more willing to pay for the COVID‐19 vaccine than healthy controls, suggesting a higher susceptibility for COVID‐19‐related distress in vulnerable populations (Hao et al., 2021). Taken together, these evidences represent the harmful impacts of the COVID‐19 pandemic on psychological health, generating an expectation of lasting effects in the coming years (Holmes et al., 2020).
Anxiety is one of the most prevalent psychological symptoms described as COVID‐19 related (Santabárbara et al., 2021). In this sense, Nikčević and Spada (2020) stated that there is a COVID‐19 anxiety syndrome characterized by internal and external actions related to avoidance, checking, worrying and threat monitoring. The authors developed the COVID‐19 Anxiety Syndrome Scale (C‐19ASS) focused on the assessment of these constructs. Solid psychometric properties of the C‐19ASS were described with adequate predictive values regarding generalized anxiety and depression, controlling for age, gender, employment and risk status, as well as personality traits (Nikčević et al., 2021). Another instrument was developed based on the notion of the prevalence of anxiety related to COVID‐19. Faustino and colleagues (2021b) developed the COVID‐19 Inventory, with a focus on the assessment of anxiety and the perceived severity of COVID‐19. The instrument presented satisfactory psychometric properties regarding convergent validity between the COVID‐19 anxiety subscale and somatization, anxiety, phobic anxiety, paranoid ideation and psychological distress (Faustino et al., 2021b) ). It is important to stress that the development of assessment measures regarding COVID‐19 symptomatology is extremely valuable, due to the lack of valid instruments. Concomitantly, it is also important to explore which psychological variables may be associated with COVID‐19 anxiety, as existing studies are sparse. The Anxiety Syndrome is characterized by avoidance, checking, worrying and threat monitoring (Nikčević & Spada, 2020). These psychological constructs may be seen as coping strategies through which people deal with anxiety and stress. But these variables do not represent the core maladaptive psychological structures that underlie the use of such strategies.
Those long‐standing psychological structures may be described as early maladaptive schemas (EMS) (Young et al., 2003). EMS are experience‐based psychological structures with representational (e.g., cognition and images) and experiential meanings (e.g., bodily sensations and feelings) developed in childhood or adolescence due to the frustration of core emotional needs (Young et al., 2003). EMS are stable, inflexible, generalized and impermeable to change, leading to life‐long psychological suffering, partially maintained by dysfunctional schematic coping behaviours (avoidance, surrender and overcompensation). Young et al. (2003) elaborated on 18 EMS based on five domains of emotional needs (e.g., attachment, autonomy and identity). However, this model has been updated (see Arntz et al., 2021). Schema domains and EMS are described in Table 2. There is a substantial body of research supporting theoretical claims regarding EMS. As representative examples, previous studies documented the associations between EMS and transdiagnostic symptomatology (van Vreeswijk et al., 2014), depression (Tariq et al., 2021; Wegener et al., 2013), anxiety (Cockram et al., 2010; Hawke & Provencher, 2011), personality disorders (Carr & Francis, 2010; Kunst et al., 2020; Tan et al., 2018), psychological needs (Faustino & Vasco 2020a), cognitive fusion (Faustino & Vasco, 2020b) and emotional processing difficulties (Faustino & Vasco 2020c). Mediational models emphasized the critical role of EMS in psychopathology. Roelofs et al. (2011) showed that schema domains of disconnection and rejection (as well as other domains) mediated the relationship between quality of attachment and depressive symptomatology. Lewin et al. (2015) showed that EMS of vulnerability to harm mediated the relationship between recollections of maternal bonding and current depression. Calvete et al. (2018) found that EMS of disconnection and rejection domain mediated the relationship between family abuse and social anxiety with bullying victimization during a 6‐month period. Lim et al. (2018) suggested that temperamental traits of high harm avoidance, high neuroticism, low self‐directedness and low cooperativeness exerted a direct and/or an indirect effect on the relationship between EMS and depressive symptoms. Recently, Faustino and Vasco (2020c) described a mediational model where schema domains of disconnection and rejection, impaired autonomy and impaired limits mediated the relationship between emotional processing difficulties and psychological needs. In this sense, EMS act as latent factors that augment or diminish the relationships between psychological variables, namely, psychopathological symptomatology.
EMS are regarded as transdiagnostic variables, because each individual may develop a specific cluster of schemas based on his/her life history, which in turn may foster different kinds symptomatic profiles EMS shape how individuals see themselves, the world and others, and this is associated with autobiographical life experiences (Young et al., 2003). EMS are thematically related with one or several emotional core needs that were frustrated in childhood and adolescence, facilitating the emergence of depression and anxiety. While previous research suggests that all EMS are associated with anxiety disorders, it is possible to observe that the disconnection and rejection and impaired autonomy domains tend to be associated with anxiety symptoms and anxiety disorders (Hawke & Provencher, 2011, 2013; Shorey et al., 2015). Narrowly, the Vulnerability to Harm and Illness schema has been consistently found to be associated with Panic Disorder (Hinrichsen et al., 2004; Hinrichsen et al., 2007; Kwak & Lee, 2015) and PTSD (Cockram, 2009), while the Mistrustfulness schema tends to be associated with PTSD (Dutra et al., 2008; LaMotte et al., 2016) and paranoid ideation (Karatzias et al., 2016). The Vulnerability to Harm and Illness schema leads individuals to believe that they lack the internal control to deal with an imminent health catastrophe (e.g., COVID‐19 pandemic), which is felt as unbearable. The Mistrustfulness schema leads individuals to have core beliefs about others and the world as untrustworthy, unfair and manipulative. Thus, the triggering of these two EMS in combination may act as a psychological template to interpret the situational events related to the COVID‐19 pandemic from two different but associated/complementary perspectives. On one hand, the Vulnerability to Harm and Illness schema may facilitate catastrophic perceptions of the COVID‐19 pandemic with extreme consequences for the self and others, which are experienced with stress, tension, anxiety and angst. On the other hand, the Mistrustfulness schema may increase the lack of trust in the official authorities, regarding quarantine measures, official pandemic numbers and vaccine efficacy, which may also facilitate feelings of psychological distress and loss of life satisfaction. The disbelief in the official authorities and conspiracy theories were/are a significant problem that should be addressed worldwide (De Coninck et al., 2021).
Tailoring psychotherapy to the specific characteristics of the individual (e.g., schemas), communication styles, coping responses and psychological needs should be the objective of conceptualizing each clinical case (Faustino & Vasco, 2020a, 2020b, 2020c). As stated earlier, EMS are thematic specific, meaning they may facilitate different/same symptoms despite their origins. Different EMS may promote the same symptoms; however, the underlying need is different. The frustrated core need embedded in EMS (e.g., emotional neglect and trauma‐related fears) is different, which suggests different clinical strategies. Thus, schema restructuring follows different therapeutic paths based on schema specifications. For example, individuals with a Mistrust/Abuse schema require emphasis on relational strategies, while individuals with a Vulnerability to Harm and Illness schema require more cognitive and behavioural tasks (Young et al., 2003). In this sense, understanding individual differences in responses to COVID‐19 anxiety is crucial to understanding the core frustrated emotional need underlying schema manifestations.
Despite these theoretical claims, the predictive and the mediational roles of EMS on the relationships between COVID‐19 anxiety and mental health variables remain unexplored. Therefore, the present work has four exploratory aims: (1) to explore the associations between EMS, COVID‐19 anxiety, psychological well‐being and distress, and life satisfaction; (2) to explore the predictive value of EMS in COVID‐19 anxiety and; (3) to explore the mediational role of Vulnerability to Harm and Illness and Mistrustfulness schemas on the relationships between COVID‐19 anxiety, psychological well‐being and distress, and life satisfaction.
Hypothesis
EMS are positively correlated with COVID‐19 anxiety, as well as with psychological distress (H1);
EMS are negatively correlated with psychological well‐being and life satisfaction (H2);
EMS are significant predictors of COVID‐19 anxiety (H3); and
Vulnerability to Harm and Illness and Mistrustfulness schemas mediate the relationships between COVID‐19 anxiety, psychological well‐being (H4a), psychological distress (H4b) and life satisfaction (H4c).
2. METHODS
2.1. Participants and procedures
Participants of this study were recruited from the general population, using a link disseminated through social media (e.g., Facebook and LinkedIn) that accompanied an announcement of the study. Subjects could enrol if they were older than 18 years old and younger than 90, if they were in self‐quarantine for more than 15 days and if they did not suffer from a major neurocognitive disorder. All individuals were tested individually in the period between the 20th of April and the 30th of December of 2020, in which Portugal was under severe quarantine measures. A maximum period of 6 days was given to finalization of the research protocol and there was no compensation for participating. Informed consent was obtained from all individuals, after being presented with an explanation of the study. The present research was approved by the ethics committee of the Faculty of Psychology of the University of Lisbon.
First quarantine measures started in Portugal on the 22nd of March and started to be raised in middle June. Recommended confinement was required for (1) individuals who were infected or ill with COVID‐19 and (2) risk group individuals (e.g., chronic diseases and older adults). Physical or in person work, cultural, religious, sports and academic activities were suspended and replaced by online modalities where possible. There were also restrictions on public circulation (exceptions included, e.g., police officers, health workers and firemen) and on commerce, which was obligated to have reduced schedules.
The sample consisted of 249 participants, 56 males (22.5%) and 193 females (77.7%). The age of men varied between 18 and 72 years (M = 37.2, SD = 13.6), and the age of women ranged from 18 to 72 years (M = 33.3, SD = 11.3). Education frequencies were 3 (1.2%) with 9 years of education, 33 (13.3%) with 12 years, 95 (38.2%) with bachelor's degree, 111 (44.6%) with master's degree and 7 (2.8%) with a doctoral degree—see Table 1.
TABLE 1.
Descriptive statistics
| n | % | M | SD | |
|---|---|---|---|---|
| Age | 249 | 100 | 34.2 | 12.0 |
| Gender | ||||
| Men | 56 | 22.5 | ||
| Women | 193 | 77.7 | ||
| Educational level | ||||
| <9 years | 3 | 1.2 | ||
| Secondary | 33 | 13.3 | ||
| Bachelor's degree | 95 | 38.2 | ||
| Master's degree | 111 | 44.6 | ||
| Doctoral degree | 7 | 2.8 | ||
| Occupation | ||||
| Working | 44 | 17.7 | ||
| Telework | 87 | 34.9 | ||
| Lay‐off | 16 | 6.4 | ||
| Unemployed | 32 | 12.8 | ||
| Student | 56 | 22.5 | ||
| Student‐worker | 8 | 3.2 | ||
| Retired | 6 | 2.4 | ||
| Marital status | ||||
| Single | 148 | 59.4 | ||
| Married | 44 | 17.7 | ||
| Civil union | 37 | 14.9 | ||
| Divorced | 18 | 7.2 | ||
| Widow | 2 | 0.8 | ||
| Psychological treatment | ||||
| Yes | 34 | 13.7 | ||
| No | 215 | 86.3 | ||
| Self‐reported diagnosis | ||||
| Yes | 14 | 41.2 | ||
| No | 20 | 58.8 | ||
2.2. Measures
2.2.1. COVID‐19 Inventory
The COVID‐19 Inventory (Faustino et al., 2021b) is a self‐report instrument focused on the assessment of beliefs about the severity of COVID‐19 and the intensity of their anxiety, divided into two subscales: COVID‐19 Anxiety and COVID‐19 Severity. It has 8 items with a 5‐point Likert. In the present study, only COVID‐19 Anxiety scale was used and Cronbach's alpha was considered adequate (α = .84).
2.2.2. Young Schema Questionnaire (YSQ‐S3)
The YSQ‐S3 (Young, 2005; Portuguese version by Rijo, 2009, 2017) is a self‐report questionnaire focused on the assessment of EMS. It has 90 items rated on a 6‐point Likert scale. This instrument assesses five schema domains (e.g., Disconnection and Rejection, Impaired Autonomy and Performance) which contain 18 schemas (e.g., Abandonment/Instability, Mistrustfulness and Defectiveness/Shame) grouped by thematic similarity. In the present study, Cronbach's alphas ranged between medium in Impaired Autonomy and Performance (α = .88) and high in the Disconnection and Rejection domain (α = .95).
2.2.3. Mental Health Inventory (MHI‐5)
The MHI‐5 (Derogatis, 1993; Portuguese version by Ribeiro, 2001) is a self‐report instrument focused on the assessment of psychological well‐being and distress. It has 6 items rated on a 5‐point Likert scale. This self‐report instrument is used as a fast screening regarding mental health indexes. In the present study, Cronbach's alpha was considered adequate for Psychological Distress (α = .86) and Psychological Well‐being (α = .81).
2.2.4. Satisfaction with Life Scale (SWLS)
The SWLS (Diener et al., 1985; Portuguese version by Laranjeira, 2009) is a self‐report scale focused on the assessment of global cognitive judgements of one's life satisfaction. It has 5 items rated on a 7‐point Likert scale. In the present study, Cronbach's alpha was considered adequate (α = .89),
2.3. Data analysis
All statistical analyses were conducted using IBM's SPSS Statistics 24. Descriptive statistics were used to obtain the sample characterization ‐ see Table 1. Although the Kolmogorov–Smirnov test on our data pointed to it not following a normal distribution (p < .05), the Skewness and Kurtosis values were between −2 to +2 and between −7 to +7, respectively, which means that data can be considered normal (Byrne, 2010)—see Table 2. We also analysed multicollinearity, which showed to be adequate for all analyses |VIF < 5; T < 2| (Pallant, 2007). In this sense, parametric statistics were used. The Pearson product–moment correlation coefficient was used to study the associations between variables. Finally, a stepwise analysis was performed to explore predictive power, and the macro process for SPSS (Hayes, 2013) was used when conducting the mediation analysis.
TABLE 2.
Descriptive statistics of the variables under study (N = 249)
| Mean | SD | Min | Max | SK | K–S | |
|---|---|---|---|---|---|---|
| COVID‐19 Anxiety | 2.32 | 0.73 | 1.00 | 6.00 | −0.47 | −0.20 |
| Life Satisfaction | 4.66 | 1.05 | 0.00 | 4.00 | −0.59 | −0.05 |
| Psychological Distress | 2.44 | 0.86 | 1.00 | 4.67 | 0.39 | 0.68 |
| Psychological Well‐being | 2.82 | 0.57 | 1.00 | 8.50 | 0.20 | −0.19 |
| Disconnection and rejection | 2.13 | 0.95 | 1.00 | 5.48 | 0.90 | 1.15 |
| Emotional Deprivation | 1.88 | 1.07 | 1.00 | 5.80 | 0.03 | 1.54 |
| Abandonment/Instability | 2.60 | 1.26 | 1.00 | 6.00 | −0.40 | 0.68 |
| Mistrustfulness | 2.23 | 1.07 | 1.00 | 5.80 | 0.36 | 0.95 |
| Social Isolation | 2.31 | 1.17 | 1.00 | 6.00 | 0.51 | 1.04 |
| Defectiveness/Shame | 1.65 | 1.04 | 1.00 | 6.00 | 3.17 | 1.89 |
| Impaired autonomy and performance | 1.95 | 0.74 | 1.00 | 4.40 | −0.09 | 0.74 |
| Failure | 1.97 | 1.13 | 1.00 | 6.00 | 1.24 | 1.30 |
| Functional Dependence | 1.74 | 0.81 | 1.00 | 5.00 | 1.04 | 1.21 |
| Vulnerability to Harm and Illness | 2.26 | 1.05 | 1.00 | 5.20 | −0.34 | 0.69 |
| Underdeveloped Self | 1.84 | 0.83 | 1.00 | 4.80 | 1.07 | 1.18 |
| Impaired limits | 2.45 | 0.84 | 1.00 | 5.00 | −0.45 | 0.23 |
| Entitlement | 2.48 | 0.91 | 1.00 | 5.40 | −0.27 | 0.37 |
| Impaired Self‐control | 2.42 | 0.99 | 1.00 | 5.80 | 0.27 | 0.66 |
| Others domain | 2.52 | 0.80 | 1.00 | 5.47 | 0.04 | 0.41 |
| Subjugation | 1.97 | 0.96 | 1.00 | 5.40 | 0.72 | 1.09 |
| Self‐sacrifice | 2.89 | 1.10 | 1.00 | 5.80 | −0.52 | 0.35 |
| Recognition‐seeking | 2.71 | 1.01 | 1.00 | 5.60 | −0.48 | 0.23 |
| Overvigilance and inhibition | 2.73 | 0.82 | 1.00 | 5.10 | −0.19 | 0.39 |
| Emotional Inhibition | 2.21 | 1.07 | 1.00 | 5.60 | 0.29 | 0.91 |
| Unrelenting Standards/Hypercritical | 3.70 | 1.03 | 1.00 | 6.00 | −0.37 | −0.22 |
| Pessimism | 2.60 | 1.26 | 1.00 | 6.00 | −0.32 | 0.66 |
| Punitiveness | 2.40 | 0.96 | 1.00 | 5.40 | 0.20 | 0.71 |
| YSQ‐S3 total index | 2.32 | 0.73 | 1.00 | 4.50 | −0.21 | 0.56 |
Abbreviations: K–S, Kolmogorov–Smirnov; SD, standard deviation; SK, skewness, kurtosis.
3. RESULTS
3.1. Correlational analyses
As expected, several associations were found between EMS and COVID‐19 Anxiety, Life Satisfaction, Psychological Distress and Psychological Well‐being. Several schemas correlated positively with COVID‐19 Anxiety, with the most strongly correlated being Mistrustfulness (r = .20, p < .01), Vulnerability to Harm and Illness (r = .29, p < .01) and Pessimism (r = .21, p < .01). Furthermore, all EMS correlated negatively with Life Satisfaction, for which the highest correlation was with Emotional Deprivation (r = −.47, p < .01) and the lowest was with Unrelenting Standards/Hypercritical (r = −.07, p < .05). The correlational pattern between EMS, Psychological Well‐being and Psychological Distress was also expected, wherein all schemas correlated negatively with Psychological Well‐being and positively with Psychological Distress (p < .05)—see Table 3.
TABLE 3.
Pearson correlations between early maladaptive schemas and mental health variables (N = 249)
| COVID‐19 Anxiety | Life Satisfaction | Psychological Well‐being | Psychological Distress | |
|---|---|---|---|---|
| Disconnection and rejection | .10 | −.47 ** | −.32 ** | .44 ** |
| Emotional Deprivation | .00 | −.47 ** | −.20 ** | .36 ** |
| Abandonment/Instability | .16 * | −.25 ** | −.33 ** | .35 ** |
| Mistrustfulness | .20 ** | −.33 ** | −.25 ** | .30 ** |
| Social Isolation | .01 | −.52 ** | −.28 ** | .38 ** |
| Defectiveness/Shame | .03 | −.45 ** | −.26 ** | .45 ** |
| Impaired autonomy and performance | .15 * | −.44 ** | −.32 ** | .39 ** |
| Failure | −.01 | −43 ** | −.27 ** | .42 ** |
| Functional Dependence | .01 | −37 ** | −.22 ** | .28 ** |
| Vulnerability to Harm and Illness | .29 ** | −.32 ** | −.32 ** | .33 ** |
| Underdeveloped Self | .17 ** | −.23 ** | −.16 ** | .18 ** |
| Impaired limits | −.03 | −.33 ** | −.29 ** | .27 ** |
| Entitlement | −.02 | −.23 ** | −.26 ** | .16 * |
| Impaired Self‐control | −.03 | −.35 ** | −.26 ** | .31 ** |
| Others domain | .16 * | −.37 ** | −.28 ** | .38 ** |
| Subjugation | .13 * | −.43 ** | −.20 ** | .39 ** |
| Self‐sacrifice | .16 * | −.25 ** | −.16 * | .25 ** |
| Recognition‐seeking | .01 | −.19 ** | −.29 ** | .25 ** |
| Overvigilance and inhibition | .20 ** | −.29 ** | −.33 ** | .35 ** |
| Emotional Inhibition | .19 ** | −.21 ** | −.23 ** | .23 ** |
| Unrelenting Standards/Hypercritical | .13 * | −.07 * | −.27 ** | .17 ** |
| Pessimism | .21 ** | −.34 ** | −.29 ** | .37 ** |
| Punitiveness | .06 | −.22 ** | −.19 ** | .27 ** |
| YSQ‐S3 total index | .13 * | −.45 ** | −.35 ** | .43 ** |
p < .01.
p < .05.
3.2. Stepwise regression analysis
Using a stepwise regression analysis, a composite model was found with seven predictors that explain 22% of the variance of COVID‐19 Anxiety (b = 0.27, p < .01)—see Table 4 (Hypothesis 2).
TABLE 4.
Stepwise regression analysis with early maladaptive schemas as predictors of COVID‐19 anxiety (N = 249)
| B | Error | St beta | R 2 | t | Sig | |
|---|---|---|---|---|---|---|
| Vulnerability to Harm | .42 | .07 | .41 | .09 | 5.659 | .00 |
| Social Isolation | −.24 | .07 | −.27 | .11 | −3.183 | .00 |
| Mistrustfulness | .35 | .08 | .35 | .14 | 4.028 | .00 |
| Entitlement | −.21 | .08 | −.17 | .18 | −2.346 | .02 |
| Impaired Self‐control | −.16 | .08 | −.15 | .20 | −1.931 | .05 |
| Emotional Inhibition | .15 | .06 | −.15 | .21 | 2.258 | .02 |
| Punitiveness | −.16 | .08 | −.16 | .22 | −1.974 | .05 |
3.3. Mediation models
Three mediation models were tested to explore Hypotheses 4a, 4b, and 4c. Confidence intervals of 95% and 10,000 bootstrap computations were used. In the first model, the direct effect between COVID‐19 Anxiety and Psychological Distress was not significant. Nevertheless, the relationship between COVID‐19 Anxiety and Psychological Distress (indirect effect) was mediated by Vulnerability to Harm and Illness (b = 0.03, |.03, .09|, p < .05) and Mistrustfulness (b = 0.01, |.01, .04|, p < .05) schemas. In the second model, the direct effect between COVID‐19 Anxiety and Psychological Well‐being was also not significant. The relationship between COVID‐19 Anxiety and Psychological Well‐being (indirect effect) was mediated by Vulnerability to Harm and Illness (b = 0.08, |.02, .16|, p < .05) and was not mediated by the Mistrustfulness schema. In the third model, the direct effect between COVID‐19 Anxiety and Life Satisfaction was not significant. However, the relationship between COVID‐19 Anxiety and Life Satisfaction (indirect effect) was mediated by Vulnerability to Harm and Illness (b = −0.05, |−.09, −.01|, p < .05) and Mistrustfulness (b = −0.03, |−.07, −.01|, p < .05) schemas (Figures 1, 2, 3).
FIGURE 1.
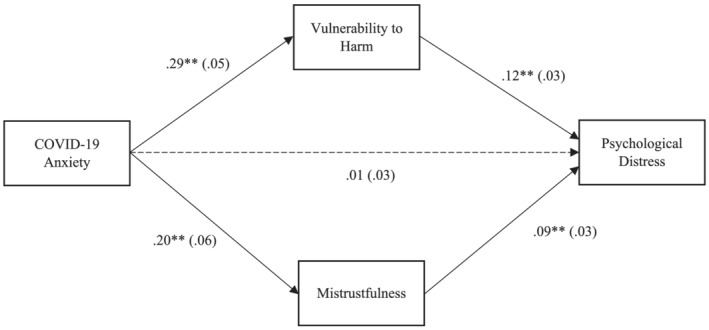
Mediation analysis between COVID‐19 Anxiety and Psychological Distress, with Vulnerability to Harm and Illness and Mistrustfulness schemas as significant mediators (b = 2.27, p < .05)
FIGURE 2.
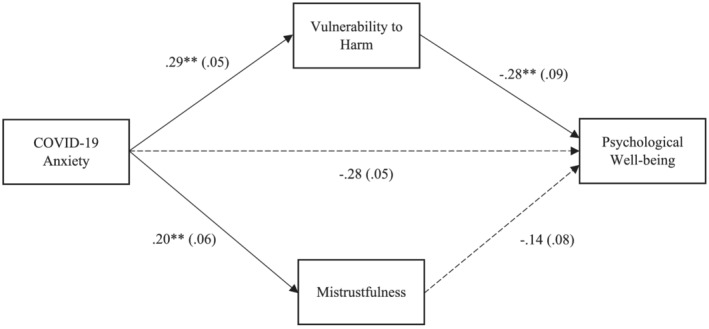
Mediation analysis between COVID‐19 Anxiety and Psychological Well‐being, with Vulnerability to Harm and Illness and Mistrustfulness schemas as significant mediators (b = 3.00, p < .05)
FIGURE 3.
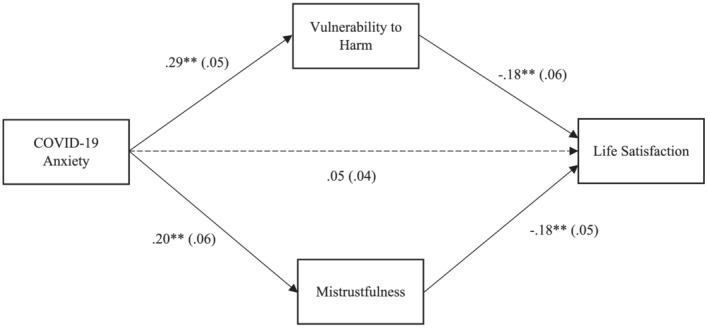
Mediation analysis between COVID‐19 Anxiety and Life Satisfaction with Vulnerability to Harm and Illness and Mistrustfulness schemas as significant mediators (b = 3.04, p < .05)
4. DISCUSSION
The primary aims of the present study were achieved. The exploration of the relationships between EMS and COVID‐19 Anxiety and mental health variables was conducted using several statistical analyses. In sum, the results largely supported theoretical predictions, solidifying the relevance of EMS in the understanding of mental health variables. Also, our results emphasize the particular relevance of the Vulnerability to Harm and Illness and the Mistrustfulness schemas on the relationships between COVID‐19 and Psychological Well‐being and Distress, as well as Life Satisfaction. Some considerations should be discussed.
Hypotheses 1 and 2 were confirmed. EMS were positively correlated with COVID‐19 Anxiety and Psychological Distress and negatively correlated with Psychological Well‐being and Distress, as well as Life Satisfaction. Moreover, all EMS correlated with mental health variables (e.g., Psychological Distress), which suggests that all EMS, regardless of their core thematic significance, may play a dysfunctional role in psychological functioning. This result is in line with previous studies (Faustino & Vasco, 2020a, 2020b, 2020c). However, only specific EMS were associated with COVID‐19 Anxiety, which supports the notion that several clusters of specific EMS may facilitate specific symptomatology. Based on the highest correlations between EMS and COVID‐19, it appears that the Vulnerability to Harm and Illness, Pessimism and Mistrustfulness schemas may be seen as a Core Vulnerability Triad for COVID‐19 Anxiety. Individuals who consider themselves fragile, vulnerable and/or weak and see the world as a dangerous/suspicious place tend to be prone to experience COVID‐19 anxiety because they feel they are not able to deal with ‘expected fears and disasters’ associated with the pandemic. Associated with these distressing appraisals and perceptions of not being able to cope may be an underlying sense of pessimism which expects the worst possible outcomes. Thus, EMS such as Abandonment/Instability, Mistrustfulness, Vulnerability to Harm and Illness and Underdeveloped Self were previously associated with Anxiety symptomatology (Dutra et al., 2008; Hawke & Provencher, 2011; Price, 2007). One likely explanation may be that these specific EMS, when triggered by life situations such as the COVID‐19 pandemic, may lead individuals to expect the worse outcome possible, which in turn prompts a feeling of anxiety. When anxious, individuals may engage in avoidance, checking, worrying and threat monitoring behaviours that tend to exacerbate emotional disturbances (Nikčević & Spada, 2020) and to confirm the veracity of beliefs of weakness, impotence, unworthiness and vulnerability embedded in the EMS (Young et al., 2003). Also, a pessimistic view of the world may be associated with beliefs of vulnerability and weakness (Beck, 2008).
A set of complex EMS predicted COVID‐19 Anxiety, which is in alignment with previous findings (Dutra et al., 2008; Hawke & Provencher, 2011), confirming Hypothesis 3. In spite of discrepant empirical findings regarding which specific EMS is the best predictor of anxiety disorders, our results suggest that a combination of EMS may postpone core vulnerabilities in dealing with the COVID‐19 pandemic. Thus, a cluster of EMS may be viewed as a vulnerability cognitive profile, with specific thematic associations that would be of great interest to be assessed by psychotherapists who apply schema healing strategies. Another aspect is the recurrence of EMS of Disconnection and Rejection (e.g., Social Isolation and Mistrustfulness) and the Impaired Autonomy and Performance (e.g., Vulnerability to Harm and Illness) in regression models regarding anxiety disorders (Gewelt, 2017). These domains reflect vulnerabilities associated with core emotional needs of attachment, trust, performance, confidence and self‐efficacy. For instance, if individuals do not develop a sense of basic trust and confidence in themselves and others, events such as the COVID‐19 pandemic may elicit several distressing thoughts and emotions that confirm that the world is not a safe place, leading to stress, tension, anguish and anxiety.
Hypothesis 4 was divided into three related but distinct models. The sub‐hypotheses A and C were confirmed, while the sub‐hypothesis B was not. The Vulnerability to Harm and Illness and Mistrustfulness schemas mediated relationships between COVID‐19 Anxiety, Psychological Distress and Life Satisfaction. Previous studies showed that COVID‐19 Anxiety was a significant predictor of Psychological Distress and different psychopathological symptoms (Faustino et al., 2020b; Gasteiger et al., 2021; Janiri et al., 2021; Tu et al., 2021; Varma et al., 2021). This result suggests that the relationship between COVID‐19 Anxiety and Psychological Distress may not be linear but instead mediated by specific EMS. Individuals who have exaggerated fears regarding medical issues and environmental catastrophes (Vulnerability to Harm and Illness) and lack basic trust and confidence in others and the world (Mistrustfulness) are prone to Psychological Distress experiencing stress, tension, angst and anxiety. These schemas facilitate one's self‐view as weak, inadequate and vulnerable to harm and a view of the world as a dangerous and mistrustful place. By viewing themselves and the world through these EMS, it is understandable that Life Satisfaction levels may be lower than those of individuals with more adaptive core beliefs. In Sub‐hypothesis B, the Mistrustfulness schema was not a significant mediator of the relationship between COVID‐19 Anxiety and Psychological Well‐being, which may be explained in different ways. First, the Vulnerability to Harm and Illness schema tends to be recurrently associated with anxiety symptoms, which means that it may be a more central EMS than Mistrustfulness regarding COVID‐19 Anxiety. Second, the correlational pattern and the regression analyses show a slightly stronger association between the Vulnerability to Harm and Illness schema and COVID‐19 Anxiety than with the Mistrustfulness schema. Third, Psychological Distress and Well‐being are differentiated but concomitant constructs in the context of the COVID‐19 pandemic. According to these results, individuals who are vulnerable and mistrustful tend to experience increasing levels of Psychological Distress, while individuals who are ‘only’ vulnerable to harm tend to decrease Psychological Well‐being associated with COVID‐19 Anxiety. A mediation model with the Pessimism EMS was not tested. However, based on the correlational pattern, it is likely that Pessimism schema may be a part of the Core Vulnerability Triad which may be viewed as a vulnerability factor to COVID‐19 Anxiety. Despite these new insights regarding EMS and COVID‐19 Anxiety, more research is required in order to continue to explore and replicate these results in other countries and with different samples.
Finally, symptom‐focused psychological intervention during the pandemic can be performed via the Internet, regarding insomnia (Derose et al., 2021; Soh et al., 2020), psychological distress (Aminoff et al., 2021), anxiety and depression (Mahoney et al., 2021). These interventions seem also cost‐effective (Zhang & Ho, 2017) and individuals with high levels of anxiety and mistrust seem to benefit from this type of intervention (Ho et al., 2020). In this way, it is possible, on the one hand, to maintain the psychological intervention centred on hypothetical schema‐driven symptoms and, on the other hand, to avoid physical proximity for long periods of time, which can potentiate contagion between the therapist and the patient.
4.1. Limitations and future directions
The study's online cross‐sectional design may limit some causal explanations about the variables under study, and future studies could aim for a replication using a clinical sample. It could also be argued that the use of self‐report instruments may limit our data to the individuals' self‐awareness. In general, future research could benefit from a bigger sample, in order to improve generalization and statistical power. Our sample was mainly comprised by young adults with a high education level, mostly single and with a predominance of female subjects, which lead the conclusions to be based on a particular layer of the general population. In the future, COVID‐19 anxiety and severity should be explored with other schema instruments. The YSQ‐S3 does not clearly differentiate cognitions and emotions about the self and others, which may be relevant to case conceptualization. Thus, Faustino (2021) suggested that core schemas may have an intrinsic dialectical nature regarding the adaptive and maladaptive views of the self and others. It would be interesting to explore how COVID‐19 anxiety and severity relate to cognitions about the self and others.
5. CONCLUSIONS
EMS may play a significant role in the relationships between COVID‐19 Anxiety and mental health variables. Vulnerability to Harm and Illness as well as Mistrustfulness schemas mediated the relationships between COVID‐19 Anxiety, Psychological Distress and Well‐being and Life Satisfaction. These new results may not only contribute to the exploration of the impacts of the COVID‐19 pandemic on mental health but also inform transtheoretical conceptualization and clinical decision‐making.
CONFLICT OF INTEREST
The authors state that there is no conflict of interest.
INFORMED CONSENT
Informed consent was obtained from all individuals.
ETHICS STATEMENT
This study was approved by BLINDED.
ACKNOWLEDGEMENT
No funding was received on the present study.
Faustino, B. , Vasco, A. B. , Delgado, J. , Farinha‐Fernandes, A. , & Guerreiro, J. C. (2022). Early maladaptive schemas and COVID‐19 anxiety: The mediational role of mistrustfulness and vulnerability to harm and illness. Clinical Psychology & Psychotherapy, 29(4), 1297–1308. 10.1002/cpp.2706
Melissa Furtado and Briar E. Inness are equally second authors.
DATA AVAILABILITY STATEMENT
Data are not shared.
REFERENCES
- Albery, I. P. , Spada, M. M. , & Nikčević, A. V. (2021). The COVID‐19 anxiety syndrome and selective attentional bias towards COVID‐19‐related stimuli in UK residents during the 2020–2021 pandemic. Clinical Psychology & Psychotherapy, 28(6), 1367–1378. 10.1002/cpp.2639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimohamadi, Y. , Sepandi, M. , Taghdir, M. , & Hosamirudsari, H. (2020). Determine the most common clinical symptoms in COVID‐19 patients: A systematic review and meta‐analysis. Journal of Preventive Medicine and Hygiene, 61(3), E304–E312. 10.15167/2421-4248/jpmh2020.61.3.1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aminoff, V. , Sellén, M. , Sörliden, E. , Ludvigsson, M. , Berg, M. , & Andersson, G. (2021). Internet‐based cognitive behavioral therapy for psychological distress associated with the COVID‐19 pandemic: A pilot randomized controlled trial. Frontiers in Psychology, 12, 684540. 10.3389/fpsyg.2021.684540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arntz, A. , Rijkeboer, M. , Chan, E. , Fassbinder, E. , Karaosmanoglu, A. , Lee, C. W. , & Panzeri, M. (2021). Towards a reformulated theory underlying schema therapy: Position paper of an international workgroup. Cognitive Therapy and Research, 45, 1007–1020. 10.1007/s10608-021-10209-5 [DOI] [Google Scholar]
- Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. The American Journal of Psychiatry, 165(8), 969–977. 10.1176/appi.ajp.2008.08050721 [DOI] [PubMed] [Google Scholar]
- Bueno‐Notivol, J. , Gracia‐García, P. , Olaya, B. , Lasheras, I. , López‐Antón, R. , & Santabárbara, J. (2021). Prevalence of depression during the COVID‐19 outbreak: A meta‐analysis of community‐based studies. International Journal of Clinical and Health Psychology, 21(1), 100196. 10.1016/j.ijchp.2020.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne, B. M. (2010). Structural equation modeling with AMOS: Basic concepts, applications, and programming, 2nd Edition. Routledge Taylor & Francis Group. [Google Scholar]
- Calvete, E. , Fernández‐González, L. , González‐Cabrera, J. M. , & Gámez‐Guadix, M. (2018). Continued Bullying Victimization in Adolescents: Maladaptive Schemas as a Mediational Mechanism. Journal of Youth and Adolescence, 47(3), 650–660. 10.1007/s10964-017-0677-5 [DOI] [PubMed] [Google Scholar]
- Carr, S. N. , & Francis, A. J. (2010). Early maladaptive schemas and personality disorder symptoms: An examination in a non‐clinical sample. Psychology and Psychotherapy, 83(4), 333–349. 10.1348/147608309X481351 [DOI] [PubMed] [Google Scholar]
- Ceban, F. , Nogo, D. , Carvalho, I. P. , Lee, Y. , Nasri, F. , Xiong, J. , Lui, L. , Subramaniapillai, M. , Gill, H. , Liu, R. N. , Joseph, P. , Teopiz, K. M. , Cao, B. , Mansur, R. B. , Lin, K. , Rosenblat, J. D. , Ho, R. C. , & McIntyre, R. S. (2021). Association between mood disorders and risk of COVID‐19 infection, hospitalization, and death: A systematic review and meta‐analysis. JAMA Psychiatry, 78(10), 1079–1091. 10.1001/jamapsychiatry.2021.1818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockram, D. M. (2009). Role and treatment of early maladaptive schemas in Vietnam veterans with PTSD. Murdoch University: Professional Doctorate thesis. [DOI] [PubMed] [Google Scholar]
- Cockram, D. M. , Drummond, P. D. , & Lee, C. W. (2010). Role and treatment of early maladaptive schemas in Vietnam veterans with PTSD. Clinical Psychology & Psychotherapy, 17(3), 165–182. 10.1002/cpp.690 [DOI] [PubMed] [Google Scholar]
- De Coninck, D. , Frissen, T. , Matthijs, K. , d'Haenens, L. , Lits, G. , Champagne‐Poirier, O. , & Généreux, M. (2021). Beliefs in conspiracy theories and misinformation about COVID‐19: Comparative perspectives on the role of anxiety, depression and exposure to and trust in information sources. Frontiers in Psychology, 12, 646394. 10.3389/fpsyg.2021.646394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. R. (1993). The Brief Symptom Inventory (BSI): Administration, scoring and procedures manual. National Computer Systems. [Google Scholar]
- Derose, S. F. , Rozema, E. , Chen, A. , Shen, E. , Hwang, D. , & Manthena, P. (2021). A population health approach to insomnia using internet‐based cognitive behavioral therapy for insomnia. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 17(8), 1675–1684. 10.5664/jcsm.9280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener, E. , Emmons, R. A. , Larsen, R. J. , & Griffin, S. (1985). The Satisfaction with Life Scale. Journal of Personality Assessment, 49, 71–75. [DOI] [PubMed] [Google Scholar]
- Dutra, L. , Callahan, K. , Forman, E. , Mendelsohn, M. , & Herman, J. (2008). Core schemas and suicidality in a chronically traumatized population. The Journal of Nervous and Mental Disease, 196(1), 71–74. 10.1097/NMD.0b013e31815fa4c1 [DOI] [PubMed] [Google Scholar]
- Faustino, B . (2021). Confirmatory factor analysis of the European Portuguese version of the Brief Core Schemas Scale. Psychological Reports. 10.1177/00332941211063602 [DOI] [PubMed] [Google Scholar]
- Faustino, B. , & Vasco, A. B . (2020a). Schematic functioning, interpersonal dysfunctional cycles and cognitive fusion in the complementary paradigmatic perspective: Analysis of a clinical sample. Journal of Contemporary Psychotherapy, 1(50), 47–55. 10.1007/s10879-019-09422-x [DOI] [Google Scholar]
- Faustino, B. , & Vasco, A. B . (2020b). Early maladaptive schemas and cognitive fusion on the regulation of psychological needs. Journal of Contemporary Psychotherapy, 1(50), 105–112. 10.1007/s10879-019-09446-3 [DOI] [Google Scholar]
- Faustino, B. , & Vasco, A. B . (2020c). Relationships between emotional processing difficulties and early maladaptive schemas on the regulation of psychological needs. In Clinical Psychology and Psychotherapy. Advance online publication. 10.1002/cpp.2464 [DOI] [PubMed] [Google Scholar]
- Faustino, B., Vasco, A. B., Delgado, J., Farinha‐Fernandes, A., & Guerreiro, J. C . (2021a). Exploring the impacts of COVID‐19 related social distancing on loneliness, psychological needs and symptomatology. Research in Psychotherapy (Milano), 23(3), 492. 10.4081/ripppo.2020.492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faustino, B., Vasco, A. B., Delgado, J., Farinha‐Fernandes, A., Guerreiro, J. C., & Matos, M . (2021b). COVID‐19 inventory and mental health: Preliminary analysis. American Journal of Psychotherapy, appipsychotherapy20210004. Advance online publication. 10.1176/appi.psychotherapy.20210004 [DOI] [PubMed] [Google Scholar]
- Gasteiger, N. , Vedhara, K. , Massey, A. , Jia, R. , Ayling, K. , Chalder, T. , Coupland, C. , & Broadbent, E. (2021). Depression, anxiety and stress during the COVID‐19 pandemic: Results from a New Zealand cohort study on mental well‐being. BMJ Open, 11(5), e045325. 10.1136/bmjopen-2020-045325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewelt, S. E. (2017). Early Maladaptive Schemas in Anxiety Disorders ‐ An Investigation of Schemas' Relation to Symptoms in a Complex Sample.Master Degree. University of Oslo: Deparment of Psychology. [Google Scholar]
- Grant, M. C. , Geoghegan, L. , Arbyn, M. , Mohammed, Z. , McGuinness, L. , Clarke, E. L. , & Wade, R. G. (2020). The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS‐CoV‐2; COVID‐19): A systematic review and meta‐analysis of 148 studies from 9 countries. PLoS ONE, 15(6), e0234765. 10.1371/journal.pone.0234765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao, F. , Tam, W. , Hu, X. , Tan, W. , Jiang, L. , Jiang, X. , Zhang, L. , Zhao, X. , Zou, Y. , Hu, Y. , Luo, X. , McIntyre, R. S. , Quek, T. , Tran, B. X. , Zhang, Z. , Pham, H. Q. , Ho, C. , & Ho, R. (2020). A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID‐19 inpatients in isolation facilities. Translational Psychiatry, 10(1), 355. 10.1038/s41398-020-01039-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao, F. , Wang, B. , Tan, W. , Husain, S. F. , McIntyre, R. S. , Tang, X. , Zhang, L. , Han, X. , Jiang, L. , Chew, N. , Tan, B. Y. , Tran, B. , Zhang, Z. , Vu, G. L. , Vu, G. T. , Ho, R. , Ho, C. S. , & Sharma, V. K. (2021). Attitudes toward COVID‐19 vaccination and willingness to pay: Comparison of people with and without mental disorders in China. BJPsych Open, 7(5), e146. 10.1192/bjo.2021.979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawke, L. D. , & Provencher, M. D. (2011). Schema theory and schema therapy in mood and anxiety disorders: A review. Journal of Cognitive Psychotherapy, 25(4), 257–276. 10.1891/0889-8391.25.4.257 [DOI] [PubMed] [Google Scholar]
- Hawke, L. D. , & Provencher, M. D. (2013). Early maladaptive schemas: Relationship with case complexity in mood and anxiety disorders. Journal of Cognitive Psychotherapy, 27(4), 359–369. 10.1891/0889-8391.27.4.359 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach. Guilford Press. [Google Scholar]
- Hinrichsen, H. , Waller, G. , & Dhokia, R. (2007). Core beliefs and social anxiety in the eating disorders. Eating and Weight Disorders ‐ Studies on Anorexia Bulimia and Obesity, 12(1), E14–E18. 10.1007/BF03327776 [DOI] [PubMed] [Google Scholar]
- Hinrichsen, H. , Waller, G. , & Emanuelli, F. (2004). Social anxiety and agoraphobia in the eating disorders: Associations with core beliefs. The Journal of Nervous and Mental Disease, 192(11), 784–787. 10.1097/01.nmd.0000144698.69316.02 [DOI] [PubMed] [Google Scholar]
- Ho, C. S. , Chee, C. Y. , & Ho, R. C. (2020). Mental health strategies to combat the psychological impact of coronavirus disease 2019 (COVID‐19) beyond paranoia and panic. Annals of the Academy of Medicine, Singapore, 49(3), 155–160. 10.47102/annals-acadmedsg.202043 [DOI] [PubMed] [Google Scholar]
- Ho, R. C. , Sharma, V. K. , Tan, B. , Ng, A. , Lui, Y. S. , Husain, S. F. , Ho, C. S. , Tran, B. X. , Pham, Q. H. , McIntyre, R. S. , & Chan, A. (2021). Comparison of brain activation patterns during olfactory stimuli between recovered COVID‐19 patients and healthy controls: A functional near‐infrared spectroscopy (fNIRS) study. Brain Sciences, 11(8), 968. 10.3390/brainsci11080968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A. , O'Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , Ballard, C. , Christensen, H. , Silver, R. C. , Everall, I. , Ford, T. , John, A. , Kabir, T. , King, K. , Madan, I. , Michie, S. , Przybylski, A. K. , Shafran, R. , Sweeney, A. , … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet: Psychiatry, 7(6), 547–560. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janiri, D. , Carfì, A. , Kotzalidis, G. D. , Bernabei, R. , Landi, F. , & Sani, G. (2021). Posttraumatic stress disorder in patients after severe COVID‐19 infection. JAMA Psychiatry, 78(5), 567–569. 10.1001/jamapsychiatry.2021.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatzias, T. , Jowett, S. , Begley, A. , & Deas, S. (2016). Early maladaptive schemas in adult survivors of interpersonal trauma: Foundations for a cognitive theory of psychopathology. European Journal of Psychotraumatology, 7, 30713. 10.3402/ejpt.v7.30713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunst, H. , Lobbestael, J. , Candel, I. , & Batink, T. (2020). Early maladaptive schemas and their relation to personality disorders: A correlational examination in a clinical population. Clinical Psychology & Psychotherapy, 27(6), 837–846. 10.1002/cpp.2467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwak, K. H. , & Lee, S. J. (2015). A comparative study of early maladaptive schemas in obsessive‐compulsive disorder and panic disorder. Psychiatry Research, 230(3), 757–762. 10.1016/j.psychres.2015.11.015 [DOI] [PubMed] [Google Scholar]
- LaMotte, A. D. , Taft, C. T. , & Weatherill, R. P. (2016). Mistrust of others as a mediator of the relationship between trauma exposure and use of partner aggression. Psychological Trauma Theory Research Practice and Policy, 8(4), 535–540. 10.1037/tra0000157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laranjeira, C. A. (2009). Preliminary validation study of the Portuguese version of the Satisfaction With Life Scale. Psychology, Health & Medicine, 14(2), 220–226. 10.1080/13548500802459900 [DOI] [PubMed] [Google Scholar]
- Lee, S. A. (2020). Coronavirus anxiety scale: A brief mental health screener for COVID‐19 related anxiety. Death Studies, 44, 393–401. 10.1080/07481187.2020.1748481 [DOI] [PubMed] [Google Scholar]
- Lee, S. A. , Jobe, M. C. , Mathis, A. A. , & Gibbons, J. A. (2020). Incremental validity of coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. Journal of Anxiety Disorders, 74, 102268. 10.1016/j.janxdis.2020.102268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin, M. R. , Garcia, L. M. , Limon, A. M. , & Ojeda, A. (2015). Dysfunctional parenting and depression: The mediational role of schemas. Journal of Experimental Psychopathology, 6(1), 2–12. 10.5127/jep.035513 [DOI] [Google Scholar]
- Lim, C. R. , Barlas, J. , & Ho, R. (2018). The effects of temperament on depression according to the schema model: A scoping review. International Journal of Environmental Research and Public Health, 15(6), 1231. 10.3390/ijerph15061231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindholt, M. F. , Jørgensen, F. , Bor, A. , & Petersen, M. B. (2021). Public acceptance of COVID‐19 vaccines: Cross‐national evidence on levels and individual‐level predictors using observational data. BMJ Open, 11(6), e048172. 10.1136/bmjopen-2020-048172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez‐Leon, S. , Wegman‐Ostrosky, T. , Perelman, C. , Sepulveda, R. , Rebolledo, P. , Cuapio, A. , & Villapol, S. (2021). More Than 50 Long‐Term Effects of COVID‐19: A Systematic Review and Meta‐Analysis. Research square, rs.3.rs‐266574. 10.21203/rs.3.rs-266574/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney, A. , Li, I. , Haskelberg, H. , Millard, M. , & Newby, J. M. (2021). The uptake and effectiveness of online cognitive behaviour therapy for symptoms of anxiety and depression during COVID‐19. Journal of Affective Disorders, 292, 197–203. 10.1016/j.jad.2021.05.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikčević, A. V. , & Spada, M. M. (2020). The COVID‐19 Anxiety Syndrome Scale: Development and psychometric properties. Psychiatry Research, 292, 113322. 10.1016/j.psychres.2020.113322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikčević, A. V. , Marino, C. , Kolubinski, D. C. , Leach, D. , & Spada, M. M. (2021). Modelling the contribution of the Big Five personality traits, health anxiety, and COVID‐19 psychological distress to generalised anxiety and depressive symptoms during the COVID‐19 pandemic. Journal of Affective Disorders, 279, 578–584. 10.1016/j.jad.2020.10.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallant, J. (2007). SPSS survival manual: A step by step guide to data analysis using SPSS for Windows (version 15). McGrow Hill Education: Berkshire: Open University Press. [Google Scholar]
- Porter, C. , Favara, M. , Hittmeyer, A. , Scott, D. , Sánchez Jiménez, A. , Ellanki, R. , Woldehanna, T. , Duc, L. T. , Craske, M. G. , & Stein, A. (2021). Impact of the COVID‐19 pandemic on anxiety and depression symptoms of young people in the global south: Evidence from a four‐country cohort study. BMJ Open, 11(4), e049653. 10.1136/bmjopen-2021-049653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price, J. P. (2007). Cognitive schemas, defence mechanisms and post‐traumatic stress symptomatology. Psychology and Psychotherapy: Theory, Research and Practice, 80(3), 343–353. 10.1348/147608306x144178 [DOI] [PubMed] [Google Scholar]
- Qiu, J. , Shen, B. , Zhao, M. , Wang, Z. , Xie, B. , & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID‐19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro, J. L. P. (2001). Mental Health Inventory: Um estudo de adaptação à população portuguesa. Psicologia, Saúde & Doenças, 2(1), 77–99. [Google Scholar]
- Rijo, D. (2017). O Questionário de Esquemas de Young (YSQ‐S3). In Gonçalves M., Simões M. R., & Almeida L. (Eds.), Psicologia clínica e da saúde: Instrumentos de avaliação (pp. 159–173). PACTOR. [Google Scholar]
- Roelofs, J. , Lee, C. , Ruijten, T. , & Lobbestael, J. (2011). The mediating role of early maladaptive schemas in the relation between quality of attachment relationships and symptoms of depression in adolescents. Behavioural and Cognitive Psychotherapy, 39(4), 471–479. 10.1017/S1352465811000117 [DOI] [PubMed] [Google Scholar]
- Rondung, E. , Leiler, A. , Meurling, J. , & Bjärtå, A. (2021). Symptoms of depression and anxiety during the early phase of the COVID‐19 pandemic in Sweden. Frontiers in Public Health, 9, 562437. 10.3389/fpubh.2021.562437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara, J. , Lasheras, I. , Lipnicki, D. M. , Bueno‐Notivol, J. , Pérez‐Moreno, M. , López‐Antón, R. , De la Cámara, C. , Lobo, A. , & Gracia‐García, P. (2021). Prevalence of anxiety in the COVID‐19 pandemic: An updated meta‐analysis of community‐based studies. Progress in Neuro‐Psychopharmacology & Biological Psychiatry, 109, 110207. 10.1016/j.pnpbp.2020.110207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey, R. C. , Elmquist, J. , Anderson, S. , & Stuart, G. L. (2015). The relationship between early maladaptive schemas, depression, and generalized anxiety among adults seeking residential treatment for substance use disorders. Journal of Psychoactive Drugs, 47(3), 230–238. 10.1080/02791072.2015.1050133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh, H. L. , Ho, R. C. , Ho, C. S. , & Tam, W. W. (2020). Efficacy of digital cognitive behavioural therapy for insomnia: A meta‐analysis of randomised controlled trials. Sleep Medicine, 75, 315–325. 10.1016/j.sleep.2020.08.020 [DOI] [PubMed] [Google Scholar]
- Tan, Y. M. , Lee, C. W. , Averbeck, L. E. , Brand‐de Wilde, O. , Farrell, J. , Fassbinder, E. , Jacob, G. A. , Martius, D. , Wastiaux, S. , Zarbock, G. , & Arntz, A. (2018). Schema therapy for borderline personality disorder: A qualitative study of patients' perceptions. PLoS ONE, 13(11), 0206039. 10.1371/journal.pone.0206039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tariq, A. , Reid, C. , & Chan, S. (2021). A meta‐analysis of the relationship between early maladaptive schemas and depression in adolescence and young adulthood. Psychological Medicine, 51(8), 1233–1248. 10.1017/S0033291721001458 [DOI] [PubMed] [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020). COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety, 37(8), 706–714. 10.1002/da.23071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu, Y. , Zhang, Y. , Li, Y. , Zhao, Q. , Bi, Y. , Lu, X. , Kong, Y. , Wang, L. , Lu, Z. , & Hu, L. (2021). Post‐traumatic stress symptoms in COVID‐19 survivors: A self‐report and brain imaging follow‐up study. Molecular Psychiatry. 10.1038/s41380-021-01223-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Vreeswijk, M. F. , Spinhoven, P. , Eurelings‐Bontekoe, E. H. , & Broersen, J. (2014). Changes in symptom severity, schemas and modes in heterogeneous psychiatric patient groups following short‐term schema cognitive‐behavioural group therapy: A naturalistic pre‐treatment and post‐treatment design in an outpatient clinic. Clinical Psychology & Psychotherapy, 21(1), 29–38. 10.1002/cpp.1813 [DOI] [PubMed] [Google Scholar]
- Varma, P. , Junge, M. , Meaklim, H. , & Jackson, M. L. (2021). Younger people are more vulnerable to stress, anxiety and depression during COVID‐19 pandemic: A global cross‐sectional survey. Progress in Neuro‐Psychopharmacology & Biological Psychiatry, 109, 110236. 10.1016/j.pnpbp.2020.110236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegener, I. , Alfter, S. , Geiser, F. , Liedtke, R. , & Conrad, R. (2013). Schema change without schema therapy: The role of early maladaptive schemata for a successful treatment of major depression. Psychiatry, 76(1), 1–17. 10.1521/psyc.2013.76.1.1 [DOI] [PubMed] [Google Scholar]
- Woon, L. S. , Leong Bin Abdullah, M. , Sidi, H. , Mansor, N. S. , & Nik Jaafar, N. R. (2021). Depression, anxiety, and the COVID‐19 pandemic: Severity of symptoms and associated factors among university students after the end of the movement lockdown. PLoS ONE, 16(5), e0252481. 10.1371/journal.pone.0252481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2020b). Coronavirus disease 2019 (COVID‐19) situation report—69. World Health Organization. https://apps.who.int/iris/handle/10665/331615 [Google Scholar]
- World Health Organization (WHO) . (2020a). Mental health and psychosocial considerations during the COVID‐19 outbreak, 18 March 2020. World Health Organization. https://apps.who.int/iris/handle/10665/331490 [Google Scholar]
- Young, J. (2005). The Young Schema Inventory, Standardized Items (3rd version). Schema Therapy Institute. [Google Scholar]
- Young, J. E. , Klosko, J. S. , & Weishaar, M. E. (2003). Schema therapy: A practitioner's guide. Guilford Press. [Google Scholar]
- Zhang, M. W. , & Ho, R. C. (2017). Moodle: The cost effective solution for internet cognitive behavioral therapy (I‐CBT) interventions. Technology and Health Care: Official Journal of the European Society for Engineering and Medicine, 25(1), 163–165. 10.3233/THC-161261 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are not shared.


