Abstract
Background
Coronavirus disease 2019 (COVID‐19) disrupted pediatric oncology care globally, increasing demands on health care providers (HCPs) who adapted to continue care. This study sought to characterize the pandemic's impact on pediatric oncology HCPs worldwide.
Methods
A 60‐item survey focused on changes to clinical care, resources, and effects on clinicians. A diverse subgroup of institutions was purposefully selected for focus groups that explored teamwork, communication, and changes to care delivery.
Results
The survey included 311 responses from 213 institutions representing 79 countries. Sixteen institutions participated in 19 multidisciplinary focus groups in 8 languages. Decreased clinical staff availability was cited by 51% of institutions as a major impact. Staffing modifications included decreased provider availability (66% of institutions), roles or responsibility changes, and transfer outside the specialty. Physical effects included frequent COVID‐19 illness; 8% of respondents reported HCP deaths. Fifty percent of providers did not have the necessary personal protective equipment. HCPs also experienced psychological distress and financial concerns. Findings indicated more frequent impact on nurses than other providers. Impacts were described across all hospital resource levels, with staffing modifications more frequent in countries with higher COVID‐19 incidence (P < .001) and mortality rate (P = .004). Focus groups revealed negative impacts were stabilized by increased teamwork, communication, contributions outside usual roles, policies aimed at optimizing safety, and feeling that they were contributing.
Conclusions
COVID‐19 had a profound impact on the pediatric oncology workforce, creating challenging modifications to staffing and resulting in physical, psychological, and financial distress. Despite these challenges, HCPs caring for children with cancer came together to continue to provide high‐quality care.
Keywords: coronavirus disease 2019 (COVID‐19), delivery of health care, global, health care personnel, pediatric oncology, workforce
Short abstract
This mixed‐methods study reveals the impact that the coronavirus disease 2019 (COVID‐19) pandemic has had on pediatric oncology providers globally, and it highlights the importance of implementing strategies to protect the health care workforce during challenging situations.
Introduction
Since severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) was identified in December of 2019, health care providers (HCPs) have been called to care for those affected by coronavirus disease 2019 (COVID‐19) and continue to provide care to all patients. The adaptations required to provide high‐quality care caused enormous stress on human resources for health around the world. 1 Organizations are reporting a parallel pandemic among clinicians risking their lives through exposure to the virus and the detrimental effects on their mental health. 2 Thousands of health care workers have lost their lives due to COVID‐19, with hundreds of thousands of infections worldwide. 3 , 4 Furthermore, studies have characterized the psychological toll of the pandemic and resulting trauma, burnout, and mental health disorders. 5 , 6 , 7 , 8 , 9 , 10 Other burdens affecting HCPs include fear of transmitting the virus, isolation from families, lost income, interrupted training, and increased workload. 1
A critical shortage of specialized pediatric oncology providers existed before the pandemic, especially in low‐ and middle‐income countries (LMICs) where greater than 90% of the world's children with cancer live. 11 , 12 , 13 , 14 These shortages contribute to high levels of burnout and attrition in LMICs, further diminishing the available workforce. 11 , 12 , 15 During the pandemic, lockdowns and restrictions aimed at curbing the spread of COVID‐19 led to widespread disruptions to pediatric cancer care. 16 , 17 Such adaptations presented new challenges for pediatric oncology providers. This study sought to characterize the impacts of the COVID‐19 pandemic on pediatric oncology providers globally.
Materials and Methods
Study Design and Sample
An explanatory sequential mixed‐methods design was used for this study. First, a cross‐sectional survey with 60 multiple‐choice items sought to elucidate the effect of COVID‐19 on the care of children with cancer globally, focusing on changes to clinical care, availability of resources, and effects on clinical staff. Survey questions were developed with input from multidisciplinary stakeholders, reviewed for face and content validity with the study team and iteratively revised. Questions related to impacts on clinical staff aimed to explore changes in roles or responsibilities, interdisciplinary communication, and reductions in staffing availability. The final item on the survey offered participants an opportunity to opt in to the qualitative portion of the study. Based on this item, a geographically and socioeconomically diverse range of respondents was purposefully selected to host focus groups. These respondents identified multidisciplinary providers and stakeholders from their institutions to include in the focus groups to assess impact and adaptations to COVID‐19 across a range of experiences. The focus‐group guide was written in English, reviewed with a panel of experts, and iteratively revised before translation to Spanish. Pilot focus groups were conducted in both English and Spanish, after which additional revisions were incorporated. The guide was then translated into additional languages by bilingual members of the research team. Questions in the focus‐group guide were related to teamwork, communication, and changes to care of patients and families.
This study was reviewed and approved by the institutional review board at St. Jude Children's Research Hospital. Additional approval was obtained as required by local institutional review boards.
Data Collection
The survey was distributed through the Global COVID‐19 Observatory and Resource Center for Childhood Cancer, 18 the St. Jude Global Alliance, 19 and International Society of Paediatric Oncology 20 listservs. Data were collected from June 22 to August 21, 2020.
Focus groups were held between September 4 and October 27, 2020. All focus groups were conducted in the official language of the participating country. A semi‐structured focus‐group guide was developed in English, translated into seven other languages, and reviewed by bilingual members of the research team to ensure that the initial intent of the questions was maintained. Focus groups were conducted virtually via a video‐conferencing platform, audio recorded, and professionally transcribed and translated into English. 21 Two bilingual facilitators moderated each focus group, including at least 1 native speaker. Bilingual facilitators reviewed translated transcripts for clarity and accuracy before analysis.
Data Analysis
Survey responses were included for analysis if at least two‐thirds of the items were completed. To evaluate frequency of effects and balance institutions with multiple answers, responses were analyzed at an institutional level. If multiple responses from the same institution existed, the pediatric cancer unit director's responses were used in the analysis. If no unit director completed the survey, responses were selected on the basis of participant role, with responses from oncologists included for cancer‐associated questions and answers from infectious‐disease specialists for questions specific to COVID‐19. If multiple providers with the same role responded from an institution, the mean or mode of their responses was used for numerical and categorical data, respectively. Descriptive statistics was used to analyze all items. Comparisons between groups were analyzed using Fisher exact and chi‐square tests. National indicators obtained from the World Bank Open Data platform were used to define country characteristics. 22 Data regarding SARS‐CoV‐2 incident cases and mortality from July 22, 2020 (midpoint of the survey timeframe) were extracted from the World Health Organization Coronavirus Disease Dashboard. 23
Focus‐group transcripts were analyzed using rapid turnaround analysis. 24 Quantitative and qualitative findings on HCPs were analyzed together in broad categories derived from survey domains and thematic content analysis: modifications to staffing and workload, including reductions in staffing, reassignment of providers, and changes in roles, responsibilities, or work hours, and impacts on providers, including physical, psychological, and financial impacts. Stabilizing elements were discussed as aspects that helped minimize negative impacts.
Results
Survey responses from 311 providers at 213 unique institutions in 79 countries were included for analysis. Of these, 167 were interested in providing additional information; participants from 16 institutions were selected to conduct 19 focus groups (Supporting Fig. 1). Participants represented countries from all World Health Organization regions and World Bank income groups (Fig. 1) and included pediatric hematologist/oncologists, infectious‐disease physicians, trainees, other physicians, nursing directors, nurses, social workers, pharmacists, psychologists, researchers, data managers, other health care providers, volunteers, and nongovernmental agency officials caring for children with cancer (Table 1).
Figure 1.
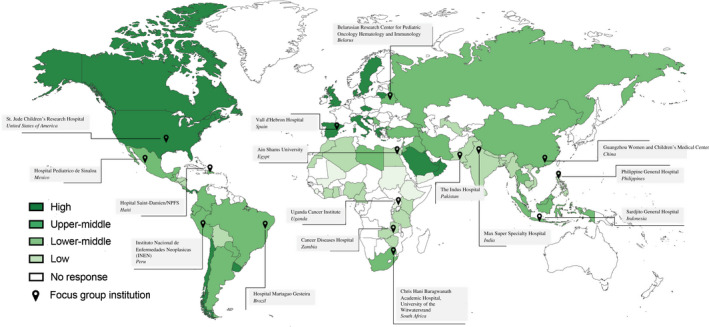
Survey respondents and focus‐group institutions. Countries represented by survey respondents (green, categorized by country income classification) and focus groups. Responses were received from 79 countries; focus groups were held in 16 countries.
TABLE 1.
Demographics of Survey Respondents and Focus Groups
| Survey, No. (%) | Focus Groups, No. (%) | |
|---|---|---|
| World Bank group of responding institutions (n = 213) | ||
| Low‐income countries | 13 (6) | 2 (13) |
| Lower‐middle‐income countries | 58 (27) | 5 (31) |
| Upper‐middle‐income countries | 105 (49) | 7 (44) |
| High‐income countries | 37 (17) | 2 (13) |
| Type of hospital (n = 213) | ||
| Public or governmental | 151 (71) | 15 (94) |
| Private or for‐profit | 62 (29) | 1 (6) |
| Average number of children diagnosed with cancer annually at institution (n = 213) | ||
| <20 | 21 (10) | 0 (0) |
| 20‐49 | 47 (22) | 1 (6) |
| 50‐99 | 48 (23) | 3 (19) |
| 100‐299 | 59 (28) | 6 (38) |
| ≥300 | 31 (15) | 6 (38) |
| Unsure | 7 (3) | 0 (0) |
| Individual respondent/focus‐group participant role (n = 311) | ||
| Pediatric hematologist/oncologist | 220 (71) | 50 (30) |
| Infectious‐disease physician | 12 (4) | 7 (4) |
| Trainee physician (resident, fellow) | 8 (3) | 3 (2) |
| Other physician | 36 (12) | 28 (17) |
| Nurse | 23 (7) | 28 (17) |
| Nurse director | 4 (1) | 9 (5) |
| Other a | 8 (3) | 39 (24) |
Other participant roles include data manager, head of infection control, surveillance officer, volunteer team lead, nongovernmental agency officer, pharmacist, social worker, epidemiologist, psychologist, patient navigator, child life specialist, dietician, patient safety officer, administrator, quality manager, patient experience manager, researcher, clinical trials coordinator, and cytogeneticist.
Modifications to Staffing and Workload
Respondents cited decreased availability of clinical staff most frequently when asked about major impacts on pediatric cancer care during the pandemic, with providers from 108 of 213 institutions (51%) reporting this effect (Fig. 2). When directly asked about reductions in staffing availability, 66% of institutions (141 of 213) described experiencing this effect of the pandemic. Of these institutions, the most frequent reasons for staff shortages were quarantine (105 of 141; 74%) and COVID‐19 infection (85 of 141; 60%). There was no difference in the occurrence of reductions in clinical staff based on country income group (P = .202). However, reductions in staffing availability were more frequently reported by institutions in countries with increased COVID‐19 incidence (P < .001) and mortality rate (P = .004) (Table 2). During the focus groups, all institutions discussed the effect of the pandemic on the availability of staff. A nurse manager in Peru stated: “I've had up to 12 people in quarantine in the same month. I don't have staff.” Some institutions hired additional staff to cover shortages: “We had a good amount of employees that needed to be hired on a temporary contract to be able to meet the needs of the professionals that were away due to COVID” (nurse in Brazil).
Figure 2.
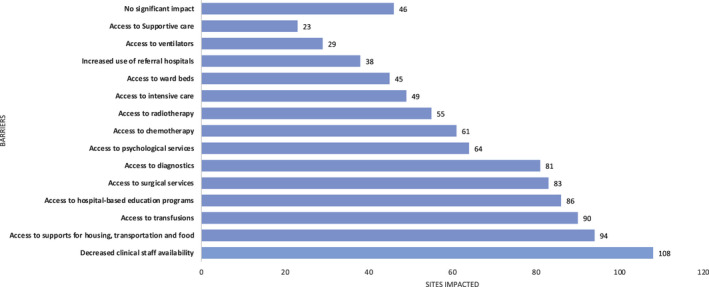
Coronavirus disease 2019 (COVID‐19) had a major impact on the care of children with cancer. The frequency of responses of the main source of effects of the COVID‐19 pandemic on pediatric cancer care (n = 213) are shown.
TABLE 2.
Effect of Country Income Status and COVID‐19 Burden on Staff Reduction and Deaths
| World Bank Group | P | ||||
|---|---|---|---|---|---|
| LIC (n = 13) No. (%) | LMIC (n = 58) No. (%) | UMIC (n = 105) No. (%) | HIC (n = 37) No. (%) | ||
| Reduction in clinical staff | 7 (54) | 42 (72) | 67 (64) | 25 (68) | .202 |
| Death of staff | 1 (8) | 6 (10) | 10 (10) | 1 (3) | .748 |
| COVID‐19 Incidence Rate Quartiles (cases/million) | |||||
| Q1 (29) | Q2 (36) | Q3 (77) | Q4 (71) | ||
| Reduction in clinical staff | 11 (38) | 19 (53) | 58 (75) | 53 (75) | <.001 |
| Death of staff | 1 (4) | 4 (11) | 6 (8) | 7 (10) | .555 |
| COVID‐19 Mortality Rate Quartiles (deaths/million) | |||||
| QI (28) | Q2 (36) | Q3 (57) | Q4 (92) | ||
| Reduction in clinical staff | 10 (36) | 22 (61) | 41 (72) | 68 (74) | .004 |
| Death of staff | 0 (0) | 5 (14) | 2 (4) | 11 (12) | .211 |
Abbreviations: COVID‐19, coronavirus disease 2019; LIC, low‐income country; LMIC, low‐ and middle‐income country; UMIC, upper‐ and middle‐income country; HIC, high‐income country.
Responses were categorized based on World Bank group, COVID‐19 incidence, and mortality rate. Fisher exact tests are used for comparison.
Lockdowns limited transportation and impacted staff's ability to report to work. This was described by 34 of 141 of institutions (24%) with reduced staffing. A nurse in a focus group in Uganda further characterized this: “You couldn't move from your house before 6:00 AM and … after 6:00 PM. And so that affected the health workforce in terms of presenting to duty.”
Sixty‐two percent of institutions (133 of 213) reported shift schedules had been modified for medical teams. These modifications were described by focus‐group participants as a strategy to minimize cross‐exposure, with “rosters” or “rotations” of staff who worked in the hospital for an extended period of time and remained away for some time: “We make a roster … they don't need to come on the daily basis, they have to come on every other day or every Thursday or every fourth day, … to minimize the exposure to the COVID‐19” (oncologist in Pakistan).
Providers were frequently transferred to other services to support the COVID‐19 response. This was noted by 45% of institutions (64 of 141) that experienced reduced staffing availability. Nurses were reassigned in 52% of these institutions (73 of 141), while 15% (21 of 141) reported reassignment of pediatric hematologists/oncologists. Figure 3 presents the frequency of reassignment and representative quotes. Staff transfer was compounded by closure of pediatric hematology/oncology units (15 of 213; 7%) and shifting dedicated pediatric hematology/oncology beds to other purposes (41 of 213; 19%). A nurse manager in the Philippines described this compound effect: “The nurses in our unit were also deployed at the other pediatric units, including the COVID pediatric wards. So, up to now, our unit is still closed.”
Figure 3.
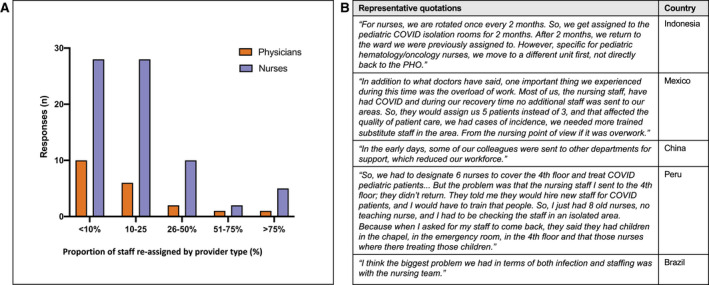
Pediatric hematology/oncology staff reassignment by provider type: quantitative and qualitative results. (A) Frequency of reassignment of hematology/oncology physicians and nurses as reported by survey respondents (n = 213). (B) Representative quotes describing the reassignment of providers.
Other changes in roles, responsibilities, or scope of work were reported by 47% of institutions (101 of 213), related to increased workload to cover for providers who were reassigned, sick, quarantined, or working remotely. This was described by focus‐group participants in both low‐ and high‐income countries. A nurse in Zambia noted: “We have to work extra hard because let's say … there are four of you, two have got to take time off, and then the two of you have to cover,” while in the United States, an oncologist expressed: “The team dynamics hasn't changed significantly, we just had to work much harder.”
Impacts on Providers
Pediatric oncology providers experienced physical impacts, such as contracting the virus; psychological impacts, such as burnout, stress, and stigmatization; and financial impacts, including unpaid leave and decreased salary. Table 3 includes quotes describing the physical, psychological, and financial impacts of COVID‐19 on providers.
TABLE 3.
Impact of COVID‐19 on Pediatric Hematology/Oncology Providers: Representative Quotes by Impact Area
| Impact Area | Representative Quotes |
|---|---|
| Physical | “We just had to bring everybody into the COVID response so running those 400 beds required four times more people than it used to and that's because we have a lot of critical care patients and then we used to just really max out the number of hours that each person had to put in like for example our residents, they wouldn't blink an eye at 24 hours on duty even more.” (Philippines) |
| “Maybe a point that I think we still have a deficit is the issue of the PPE, that I don't know if we're going to talk about that later, it is still a weak point in the services, especially in the surgical area.” (Spain) | |
| Psychological | “Without a doubt there is stress, without a doubt there is exhaustion, and sometimes, there really is a lack of this type of support.” (Belarus) |
| “So, it has been a very stressful at times … we have been trying to go and speak to mothers, patients themselves and it is frightening for ourselves because we're exposing ourselves so much, so it has been a very difficult time.” (Zambia) | |
| “I think there was a lot of fear about the disease and older colleagues were afraid.” (South Africa) | |
| “Honestly I think that sometimes we put aside the mental health of all of us involved, myself included, I think we were all on the verge of collapse … practically all the residents who were rotating here told us that they had anxiety attacks, panic attacks, they could not sleep, many of them needed psychiatric medicine.” (Mexico) | |
| “[Parents] don't comply with the rules, so the technical nurses must be like babysitters, repeating constantly, Sir, please, keep your distance. Sir please, stay on your seat. And we even had some cases where they disrespected the staff.” (Peru) | |
| “… the psychological trauma that comes along with the COVID. Sometimes staff wherever I would hear, oh, there is a staff, who is affected, everyone shakes, everyone becomes timid.” (Uganda) | |
| Financial | “People don't really want to admit that they don't feel well … they know, that if infected, unpaid self‐isolation is waiting for them. Either, you don't go to work for two weeks, unpaid, or you go to work for two weeks, paid, and endanger all of your colleagues with your infection … Because, obviously, people don't want to sit at home hungry, for two weeks' time.” (Belarus) |
| “And also, the staffs that were working with us, some of them were from very far until they couldn't afford that transport to come and work.” (Uganda) |
Physical
During the pandemic, many staff members were infected with COVID‐19. Eight percent of institutions (18 of 213) had HCPs die because of COVID‐19, with no significant impact on deaths due to country income, COVID‐19 incidence, or mortality (Table 2). In focus groups, participants across all country income groups discussed providers falling ill with COVID‐19. In the United States, an oncologist remarked: “With … 100‐ish positive symptomatic staff, nobody's been desperately ill. But we've had a couple of people hospitalized and need oxygen and out for a prolonged amount of time.” Focus‐group participants described nurses falling ill more than other providers: “The hospital nursing staffs, the service staff, I can tell you most of them have gone home with COVID or have had clinical manifestation” (oncologist in Mexico). Physical exhaustion from additional workload was felt by many providers: “We had a great rate of illness of the professionals and … the hospital refused to make new hires of professionals and so it was very challenging” (nurse in Brazil).
Providers with direct patient contact were at risk of contracting the virus due to a lack of minimally necessary personal protective equipment (PPE) needed to prevent transmission. Only 50% of institutions (106 of 213) responded they always had the minimally necessary PPE. This was noted across all country income groups, with no difference in availability of PPE between income groups (P = .463). Staff who did have access to PPE described physical discomfort experienced during long shifts: “Sometimes the person can say I want to wear the gown, I want to wear the equipment but it's too hot I can't stand it” (oncologist in Haiti).
Psychological
In focus groups, providers repeatedly discussed the psychological impact of providing care during the COVID‐19 pandemic. An oncologist in Peru summarized these feelings: “The burnout topic is a reality in our health care system, even before, and now it has intensified with the pandemic.” Feelings of fear were common, including fear of getting sick or getting family members sick: “The anxiety of the COVID infection among the health care workers … and the concern about the COVID infection on health care workers” (nurse in Pakistan). Some providers faced stigma or harassment from the public for precautions taken to curb the spread of the virus: “We are even assaulted in the streets when we wear the masks. Some people … become very aggressive” (oncologist in Haiti). Many were isolated from their families due to transportation restrictions or to reduce exposure, as described by a nurse in China: “It was stressful psychologically that many of our nurses or our colleagues were unable to return [to] their hometown.” Finally, providers across income settings described feelings of regret for not being able to provide the holistic care they had previously prided themselves on. In South Africa, an oncologist reflected: “We were so afraid that if our children got COVID that they would have died … many children were very, very isolated in this period … they sat huddled up at home without going outside, without being with friends or going to school.” This was echoed by an oncologist in the United States: “This was a major stress for many providers because feeling unable to provide the same level of care which we used to provide. And this is what eventually takes a toll.”
Despite these stressors, psychological support was available to staff in only 46% of institutions (99 of 213), and the mental health needs of staff, patients, or families received decreased attention or resources in 37% of institutions (79 of 213). The importance of psychological support for staff was emphasized in focus groups: “There are many professionals who … have many consequences and are having a very bad time emotionally … we must take care of professionals in that regard, so they can feel protected, not only with PPEs but on an emotional level” (social worker in Spain).
Financial
Financial impacts on providers occurred in 27% of institutions (58 of 213) and were described by focus‐group participants as resulting from staff needing to take unpaid leave for illness or quarantine. This was exacerbated by medical costs for providers who did not have employer‐ or government‐provided medical insurance, as explained by a nurse in Zambia: “At least we need medical insurance because we show during the pandemic that a lot of medical staff have lost their lives.” Some providers described unexpected costs, such as purchasing their own PPE or increased costs of transportation during the pandemic: “We have had to provide our own PPE through self‐financing” (nurse in Indonesia).
Stabilizing Elements
Despite many challenges, focus‐group participants described an increased sense of teamwork and collegiality experienced while responding to the pandemic. This manifested through supporting one another, covering for ill or quarantined colleagues, and sharing the workload: “The support and encouragement of each other, because when a person gets tired and they have no more enthusiasm, it's easy to give up and say ‘I can't do this anymore.’ But when you see a colleague, who tries … to share the work, and help each other, then you get extra strength” (infection‐control physician in Belarus). Focus‐group participants also described the importance of increased communication among colleagues and from hospital administration: “This has been one of the best experiences I have had. I have been working in this hospital for … 25 years, I have never had the feeling of being so informed at all levels” (oncologist in Spain). New communication channels between providers were reported by 65% of institutions (139 of 213). In focus groups, providers discussed how new ways of communicating aided in discussing patient needs between providers in different locations: “We were mostly using telephone conversations or WhatsApp video calls or WhatsApp chats to actually maintain the continuum of care” (oncologist in India). New policies were also communicated via new methods, as described by an oncologist in Egypt: “We created a WhatsApp group with … each head of … unit. All staff and managers in a WhatsApp group to follow up any decision or any notification. Then it is officially shared in the general departments of hospitals.”
Providers found meaning in positive changes in roles, responsibilities, or scope of work allowing them to contribute outside of their usual duties to continue care, as reported in 49 of 213 (23%) of surveyed institutions. An oncologist in South Africa described “everyone has got their sleeves rolled up and are doing the work … and that's a testament to everyone that we work with. There was no one that shied away from work or use this as an excuse to do less work.” Other elements that counter‐balanced negative impacts of the pandemic included debriefing, institutional algorithms or policies aimed at ensuring staff safety, and a feeling of making a difference or contributing to control the pandemic. Additional quotes illustrating stabilizing elements are included in Table 4.
TABLE 4.
Stabilizing Elements: Representative Quotes
| Teamwork and collegiality | “… The team spirit is excellent. So I think that although it was difficult in challenging times … but then you had every member of the team that was willing to assist.” (South Africa) |
| “And second good thing was everyone was concerned for the colleague's health.” (Pakistan) | |
| “Those who are here who are giving like 300%, not even 100% or 50%.” (Mexico) | |
| Debriefing | “… We've always had that culture of debriefing talking about things other than oncology finding out how we coping with whatever is happening. So when we moved into the pandemic I personally felt that we just were carrying on with the unit culture.” (South Africa) |
| “We're all pretty nervous at first and so we texted each other constantly. It was like we had this group chat going on 24 hours a day for probably the first couple of weeks because we're all like, really nervous. And we shared like every bit of information and discussed every article that came out and we were kind of all over it.” (United States) | |
| Institutional algorithms or policies | “I have felt that not only patient but staff safety has really been a priority.” (United States) |
| “So‐‐ but I think the level we manage well and the algorithm, the policies and the SOP were very helpful when people are contacting us and reaching us to how to manage COVID‐19 at home or at office level or at, if any, anyone colleague or family member are infected with the COVID in their home or in their office to help manage.” (Pakistan) | |
| Making a difference | “Despite the anxiety, stress, fear, doctors, nurses, auxiliaries, the other type of staff of the hospital, everyone … was motivated to come to work because we knew that there was a problem and that it was going to affect not only the hospital but the health system.” (Haiti) |
Abbreviations: COVID‐19, coronavirus disease 2019; SOP, standard operating procedures.
Discussion
Health care providers are a cornerstone of pediatric cancer care, providing care to patients with highly specialized management needs. Before the pandemic, the global pediatric oncology workforce faced many challenges, including staff shortages, 25 occupational safety concerns, and burnout. 12 , 13 , 14 , 26 , 27 This study highlights additional obstacles faced by providers during the COVID‐19 pandemic, including modifications to staffing and physical, psychological, and financial impacts. Despite these barriers, HCPs caring for children with cancer across the world were shown to be incredibly resilient, coming together to continue to provide care even in the direst circumstances.
This study describes staffing changes that led to decreased availability of specialized providers, felt equally across country income groups. However, incidence and mortality rates of COVID‐19 were significantly related to reductions in staffing. This indicates that, despite preexisting inequalities in human resources for health care, institutions and providers needed to adapt to respond to the local burden of the pandemic. However, additional strains caused by the pandemic may be felt more acutely in LMICs, where poorly resourced health care systems and overstretched specialties are less able to absorb and recover. 1 , 25 Ultimately, decreased availability of pediatric oncology providers during the pandemic could lead to a long‐term scarcity in the workforce, particularly in LMICs where multidisciplinary staff and specialty training opportunities are limited. 14 , 28 To mitigate this, health care organizations should consider implementing policies to retain professionals in their trained specialty 29 and build a relief pool of providers. 30 Enacting such policies will both lessen the effect of acute shortages due to illness or quarantine and prevent long‐term deficiencies.
Effective care for children with cancer requires a robust nursing workforce; however, shortages, recruitment, and retention challenges in the oncology specialty contribute to nursing shortfalls. 13 Worryingly, we found COVID‐19 had a heavy burden on nurses with higher illness rates, quarantine, and reassignment to manage patient surges on other units. This may be exacerbated by PPE shortages, as nurses spend proportionately higher time in direct contact with patients. Nurses in lower paid roles 31 are susceptible to the financial effects described, while increased workload, fatigue, and stress contribute to burnout and psychological distress. 13 Hospitals and health care systems must take special care to protect this vulnerable group. Policies, guidelines, and positive support from families and society can contribute to increased resilience, adaptation, and coping. 32 Our findings on stabilizing elements further substantiate strategies for supporting nurses and mitigating negative effects.
To protect pediatric oncology providers and their patients, organizations must pay attention to interventions that increase physical, psychological, and financial safety. Provision of adequate PPE, 33 vaccines, and ensuring adequate rest breaks and time off 34 can mitigate physical impacts. Providing hospitalization leave rather than deducting hours from annual sick leave can increase compliance with quarantine. 35 Previous work has described the importance psychological supports and access to professional psychology services for HCPs, 36 , 37 , 38 including peer‐support programs, 39 but in our study only half of staff had access to these resources. Our study demonstrated changes in care delivery caused an inability to provide the usual level of care to patients, leading to feelings of guilt and anxiety. Without psychological support, feelings of guilt, anxiety, and burnout have been shown to increase attrition of HCPs, 40 further amplifying described shortages. Health care systems should provide paid leave for illness and quarantine, 35 health insurance, childcare services, 41 and job security to ensure providers' financial security.
Finally, teamwork, interpersonal interactions, frequent communication, clear leadership, and a sense of purpose were found to protect health care workers. 42 High levels of collegiality, cooperation, and positive coworker relationships were noted as positive impacts in an international study of oncologists. 29 Our findings support these tenets and suggest implementing frequent communication, structured debriefing, policies to protect staff safety, procedural algorithms, and psychological support can balance out negative impacts on HCPs across resource settings.
Our study has several limitations. As the data collection was conducted in the second half of 2020, the results may not reflect the full impact of the pandemic. We hope that by including institutions that experienced various waves of infection we collected meaningful information that can be applied to a variety of settings. Additionally, cross‐sectional survey methodology and purposeful sampling for focus groups allow for the potential of selection bias. To address this, we ensured sampling from across all world regions and country income groups to capture a variety of experiences. Data from the survey were collected at an institutional level, prioritizing responses from physician leaders. This may have excluded perspectives from other providers and skewed data that may have been reported differently by other providers. We attempted to offset this potential imbalance by including a range of multidisciplinary providers in the focus groups. Finally, some findings may have been impacted by language barriers, as the survey was only available in English, and focus groups held in languages other than English were transcribed and translated before analysis, which could alter meaning. To mitigate this possibility, translated transcripts and analyzed data underwent a review process with bilingual facilitators and native speakers to verify accuracy and intended meaning was maintained.
In conclusion, this study revealed that COVID‐19 had a profound effect on the world's pediatric oncology health care workforce, with deleterious effects felt across all country income groups, reflecting the truly global nature of the pandemic's impact. To prevent potentially devastating impacts, it is imperative that health care organizations around the world implement measures that support providers, both as the current pandemic evolves and in planning for future catastrophic events. Special attention should be paid to the nursing workforce, who were particularly vulnerable yet are often not included in high‐level institutional response committees. The global pediatric oncology community possesses preexisting strengths in collaboration, advocacy, respect for multidisciplinary teams, and a strong sense of meaning in our work. We must utilize these strengths and come together to respond to challenges posed by the pandemic and protect the well‐being of the workforce and the children they care for.
Funding Support
This work was supported by the American Lebanese Syrian Associated Charities.
Conflict of Interest Disclosures
The authors made no disclosures.
Author Contributions
Elizabeth R. Sniderman: Writing–initial manuscript and table and figure development. Dylan E. Graetz: Idea development. Asya Agulnik: Idea development. Carlos Rodriguez‐Galindo: Idea development. Daniel C. Moreira: Idea development and table and figure development. All authors contributed to data collection, interpretation of the findings, editing of the article, and approval of the final submitted version.
Supporting information
Fig S1
Supplementary Material
Sniderman ER, Graetz DE, Agulnik A, Ranadive R, Vedaraju Y, Chen Y, Devidas M, Chantada GL, Hessissen L, Dalvi R, Pritchard‐Jones K, Rodriguez Galindo C, Moreira DC. Impact of the COVID‐19 pandemic on pediatric oncology providers globally: A mixed‐methods study. Cancer.2022. 10.1002/cncr.34090
See editorial on pages 1363‐1364, this issue.
The second and last authors contributed equally to this article.
The authors thank the COVIMPACT Study Group Collaborators for their support.
The COVIMPACT Study Group Collaborators were Nancy S. Bolous, MD, Cyrine E. Haidar, PharmD, Laure Bihannic, PhD, Diana Sa da Bandeira, PhD, Jade Xiaoqing Wang, PhD, Dongfang Li, PhD, Flavia Graca, PhD, Aksana Vasilyeva, PhD, and Harry Lesmana, MD.
Contributor Information
Dylan E. Graetz, Email: dylan.graetz@stjude.org.
Daniel C. Moreira, Email: daniel.moreira@stjude.org.
References
- 1. Mehta S, Machado F, Kwizera A, et al. COVID‐19: a heavy toll on health‐care workers. Lancet Respir Med. 2021;9:226‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dzau VJ, Kirch D, Nasca T. Preventing a parallel pandemic—a national strategy to protect clinicians' well‐being. N Engl J Med. 2020;383:513‐515. [DOI] [PubMed] [Google Scholar]
- 3. Erdem H, Lucey DR. Healthcare worker infections and deaths due to COVID‐19: a survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis. 2021;102:239‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gholami M, Fawad I, Shadan S, et al. COVID‐19 and healthcare workers: a systematic review and meta‐analysis. Int J Infect Dis. 2021;104:335‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen R, Sun C, Chen JJ, et al. A large‐scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID‐19 pandemic. Int J Ment Health Nurs. 2021;30:102‐116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gainer DM, Nahhas RW, Bhatt NV, Merrill A, McCormack J. Association between proportion of workday treating COVID‐19 and depression, anxiety, and PTSD outcomes in US physicians. J Occup Environ Med. 2021;63:89‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID‐19. Article in Chinese. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38:192‐195. [DOI] [PubMed] [Google Scholar]
- 8. Lai J, Ma S, Wang Y, et al. factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin K, Yang BX, Luo D, et al. The mental health effects of COVID‐19 on health care providers in China. Am J Psychiatry. 2020;177:635‐636. [DOI] [PubMed] [Google Scholar]
- 10. Tsan SEH, Kamalanathan A, Lee CK, Zakaria SA, Wang CY. A survey on burnout and depression risk among anaesthetists during COVID‐19: the tip of an iceberg? Anaesthesia. 2021;76(suppl 3):8‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodriguez‐Galindo C, Friedrich P, Alcasabas P, et al. Toward the cure of all children with cancer through collaborative efforts: pediatric oncology as a global challenge. J Clin Oncol. 2015;33:3065‐3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Morrissey L, Lurvey M, Sullivan C, et al. Disparities in the delivery of pediatric oncology nursing care by country income classification: international survey results. Pediatr Blood Cancer. 2019;66:e27663. [DOI] [PubMed] [Google Scholar]
- 13. Challinor JM, Alqudimat MR, Teixeira TOA, Oldenmenger WH. Oncology nursing workforce: challenges, solutions, and future strategies. Lancet Oncol. 2020;21:e564‐e574. [DOI] [PubMed] [Google Scholar]
- 14. Israels T, Challinor J, Howard S, Arora RH. Treating children with cancer worldwide–challenges and interventions. Pediatrics. 2015;136:607‐610. [DOI] [PubMed] [Google Scholar]
- 15. Nukpezah RN, Khoshnavay Fomani F, Hasanpour M, Nasrabadi AN. A qualitative study of Ghanaian pediatric oncology nurses' care practice challenges. BMC Nurs. 2021;20:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Graetz D, Agulnik A, Ranadive R, et al. Global effect of the COVID‐19 pandemic on paediatric cancer care: a cross‐sectional study. Lancet Child Adolesc Health. 2021;5:332‐340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gonzalez‐Montero J, Valenzuela G, Ahumada M, Barajas O, Villanueva L. Management of cancer patients during COVID‐19 pandemic at developing countries. World J Clin Cases. 2020;8:3390‐3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moreira DC, Sniderman E, Mukkada S, et al. The Global COVID‐19 Observatory and Resource Center for Childhood Cancer: a response for the pediatric oncology community by SIOP and St. Jude Global. Pediatr Blood Cancer. 2021:e28962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. St. Jude Children's Research Hospital St. Jude Global Alliance. Accessed July 4, 2021. https://global.stjude.org/en‐us/
- 20. International Society of Paediatric Oncology SIOP Organisation. Accessed July 4, 2021. https://siop‐online.org/about/
- 21. Squires A. Methodological challenges in cross‐language qualitative research: a research review. Int J Nurs Stud. 2009;46:277‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. World Bank Country and Lending Groups. World Bank Data Help Desk . Accessed November 21, 2019. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519‐world‐bank‐country‐and‐lending‐groups
- 23. World Health Organization WHO Coronavirus Disease (COVID‐19) Dashboard. Accessed September 24, 2020. https://covid19.who.int/
- 24. Vindrola‐Padros C, Chisnall G, Cooper S, et al. Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID‐19. Qual Health Res. 2020;30:2192‐2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scheffler RM, Campbell J, Cometto G, et al. Forecasting imbalances in the global health labor market and devising policy responses. Hum Resour Health. 2018;16:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aristizabal P, Fuller S, Rivera‐Gomez R, et al. Addressing regional disparities in pediatric oncology: results of a collaborative initiative across the Mexican‐North American border. Pediatr Blood Cancer. 2017;64. doi: 10.1002/pbc.26387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Friedrich P, Ortiz R, Fuentes S, et al. Barriers to effective treatment of pediatric solid tumors in middle‐income countries: can we make sense of the spectrum of nonbiologic factors that influence outcomes? Cancer. 2014;120:112‐125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mathew A. Global survey of clinical oncology workforce. J Global Oncol. 2018;4:1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jazieh AR, Coutinho AK, Bensalem AA, et al. Impact of the COVID‐19 pandemic on oncologists: results of an international study. JCO Global Oncol. 2021;7:242‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hick JL, Biddinger PD. Novel coronavirus and old lessons—preparing the health system for the pandemic. N Engl J Med. 2020;382:e55. [DOI] [PubMed] [Google Scholar]
- 31. Delivered by Women, Led by Men: A Gender and Equity Analysis of the Global Health and Social Workforce. World Health Organization; 2019. [Google Scholar]
- 32. Balay‐Odao EM, Alquwez N, Inocian EP, Alotaibi RS. Hospital preparedness, resilience, and psychological burden among clinical nurses in addressing the COVID‐19 crisis in Riyadh, Saudi Arabia. Front Public Health. 2021;8:573932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Campbell J, Koca F. Financing and protection for the health and care workforce. Bull World Health Org. 2021;99:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. JAMA. 2020;323:1439‐1440. [DOI] [PubMed] [Google Scholar]
- 35. Wee LE, Sim XYJ, Conceicao EP, et al. Containment of COVID‐19 cases among healthcare workers: the role of surveillance, early detection, and outbreak management. Infect Control Hosp Epidemiol. 2020;41:765‐771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dewey C, Hingle S, Goelz E, Linzer M. Supporting clinicians during the COVID‐19 pandemic. Ann Intern Med. 2020;172:752‐753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID‐19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9:241‐247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chirico F, Nucera G, Magnavita N. Protecting the mental health of healthcare workers during the COVID‐19 emergency. BrJPsych Int. 2021;18:1‐2. [Google Scholar]
- 39. Kinman G, Teoh K, Harriss A. Supporting the well‐being of healthcare workers during and after COVID‐19. Occup Med (Lond). 2020;70:294‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Labrague LJ, de Los Santos JAA. Fear of COVID‐19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. 2020;29:395‐403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Fraher EP, Pittman P, Frogner BK, et al. Ensuring and sustaining a pandemic workforce. N Engl J Med. 2020;382:2181‐2183. [DOI] [PubMed] [Google Scholar]
- 42. De Leo A, Cianci E, Mastore P, Gozzoli C. Protective and risk factors of Italian healthcare professionals during the COVID‐19 pandemic outbreak: a qualitative study. Int J Environ Res Public Health. 2021;18:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Supplementary Material


