Abstract
Introduction Competency-based medical education (CBME) approach in the medical curriculum has been introduced globally with the goal of providing flexibility, accountability, and learner-centeredness among medical learners. Traditional surgical skill training in most places has relied on “see one, do one, teach one model,” while simulation model-based training has been shown to improve competencies in surgical trainees. We wanted to assess the usefulness of a hydrophilic barrier adhesive foam wound dressing as a novel skin simulation model for learning biomechanics and practice of cutaneous flaps among plastic surgical resident trainees at our institute.
Materials and Methods An absorbent, soft polyurethane foam pad located centrally upon a larger polyurethane membrane, coated with a hydrocolloid adhesive, forming an island dressing, was used as a simulation model for this study. It was obtained from the hospital store either after or nearing their expiry dates of clinical use. Plastic surgery residents in different years of training were invited to participate in a simulation workshop, using this novel model, and give their feedback.
Results Seventeen residents in different plastic surgery training levels participated in the workshop and gave their feedback on the skin flap simulation model. The simulation model received extremely high (100%) scores on two parameters, namely, utility for flap and suture practice and high scores (88%–94%) for texture, ability to mark, and improving confidence among trainees.
Conclusions Adhesive bilayer polyurethane foam can be used as a novel cutaneous skin flap simulation model for understanding the biomechanics of skin flaps and cutaneous flap practice.
Keywords: residents training, CBME, facial plastic surgery, flaps, surgical simulation
Introduction
Traditional surgical skill training in most places has relied on “see one, do one, teach one” model where the surgical trainee is expected to see procedural skills from an experienced practitioner, memorize the skills, replicate these when the opportunity arises, and further teach it to a new trainee who then carries the tradition forward. 1 With increasing patient awareness and advocacy, ethical and legal issues have come to the fore in these training schemes. This, combined with a lack of confidence among trainees due to inadequate exposure and practice, has led to the promotion of simulation-based surgical skill training in newer surgical curricula. Cutaneous surgical procedures, including suturing techniques, biopsy techniques, and skin flap procedures, are amenable to simulation-based skill training.
Aim
We aim to assess the usefulness of a hydrophilic barrier adhesive foam wound dressing as a novel skin simulation model for learning biomechanics as well as the practice of cutaneous flaps among plastic surgical resident trainees at our institute.
Materials and Methods
An absorbent, soft polyurethane foam pad located centrally upon a larger polyurethane membrane, coated with a hydrocolloid adhesive ( Fig. 1 ), forming an island dressing (Biatain Adhesive), was used as a simulation model for this study. These dressing materials were obtained from the hospital store as they were nearing their expiry or were in postexpiry dates of clinical use. They were thought of as materials to be used for teaching purposes. A skin simulation model feedback sheet was designed for this study, and items were validated for content with the help of experts. It was designed to capture participant opinion on simulation model characteristics on a Likert scale. The simulation model was assessed for four characteristics parameters: texture, pliability, ability to mark, and handling with instruments. It was also evaluated for four utility parameters, namely, suture practice, flap practice, confidence improvement, and novel flap designing. The feedback scores per item and overall scores were then captured from this sheet. Trainees from the department of plastic surgery were invited to participate in a cutaneous flap workshop. After delivering an overview of cutaneous flaps in practice to the participants, they were provided with a skin simulation board (created by fixing the hydrophilic barrier adhesive foam wound dressing to a rigid rubber board), skin marking pen, measuring scale, surgical instruments, and sutures (4'0 prolene). A list of activities was provided to participants to execute on the skin simulation board. Defects were created on the simulation model, and the participants were allowed to recreate skin flaps for coverage of the defects. All participants were then invited to complete the feedback form at the end of the workshop.
Fig. 1.
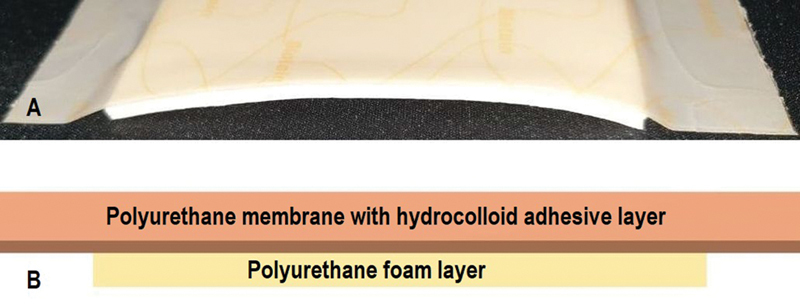
Figure showing cross-section through simulation model ( A ) with a schematic representation ( B ).
Demographic data of participants and feedback scores for each participant were collected from the feedback form and expressed in percentage of the total score. Item-wise scores for all participants were also collected.
Results
Video 1 Video demonstrating the utility of skin simulation model.
Seventeen plastic surgery residents in the first, second, and third year of training participated in a one-day cutaneous flap simulation workshop. They provided feedback in the skin simulation model feedback sheet. The participants performed different activities, as assigned to them in the worksheet ( Fig. 2A ), including performing Z-plasties, bilobed flaps, hatchet flap, Limberg flaps, linear suturing, purse-string suturing, etc. ( Fig. 3 ) ( Video 1 ). Participant feedback scores for all parameters were captured from the feedback form ( Fig. 2B ) ( Table 1 ). Nearly 30% of participants responded that the simulation model did not feel similar to normal skin during instrumentation and was not useful for designing novel flaps, while 40% of residents thought it was not pliable enough. The simulation model, however, received extremely high (100%) scores on two parameters, namely, utility for flap and suture practice, and high scores (88%–94%) for texture, ability to mark ( Fig. 4 ), and improving confidence.
Fig. 2.
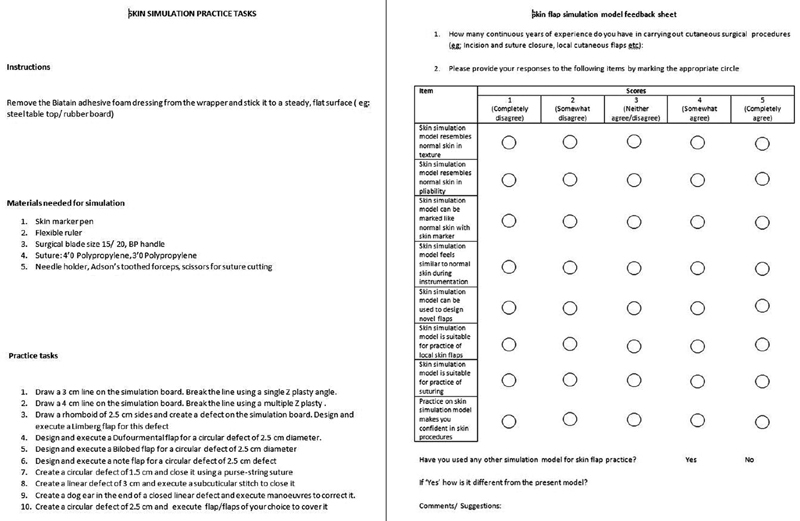
Simulation practice tasks ( A ) and feedback form ( B ).
Fig. 3.
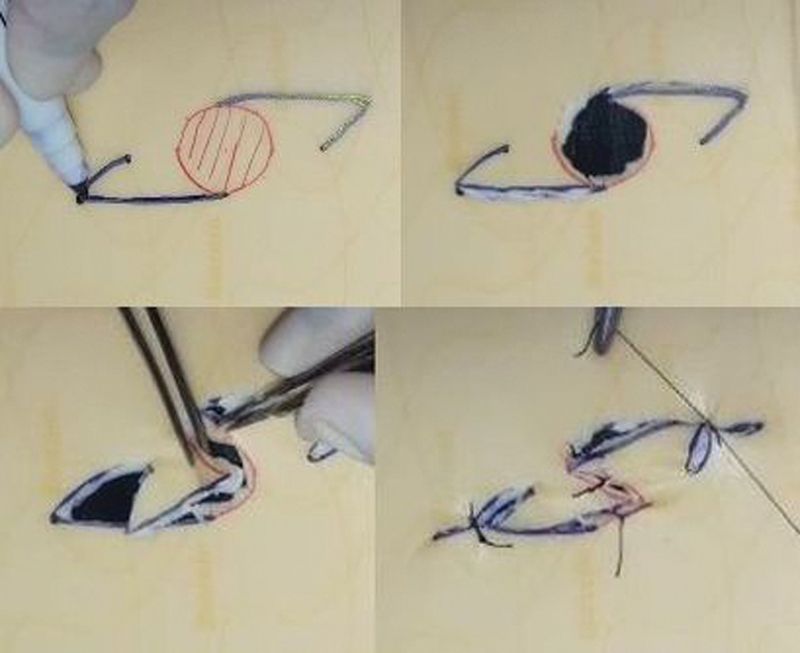
Marking, designing, and execution of hatchet flap on simulation model.
Table 1. Table showing feedback scores.
| Parameters | Score (Mean ± SD) | Score (Median [IQR]) | Percentage of ⅘ score |
|---|---|---|---|
| 1. Texture | 3.94 ± 0.66 | 4 (0) | 15/17 (88%) |
| 2. Pliability | 3.23 ± 1.20 | 4 (2) | 10/17 (59%) |
| 3. Markability | 4.76 ± 0.56 | 5 (0) | 16/17 (94%) |
| 4. Similarity | 3.82 ± 0.95 | 4 (1.5) | 12/17 (70.58%) |
| 5. Utility (novel flaps) | 4.06 ± 1.14 | 4 (1.5) | 13/17 (76.47%) |
| 6. Practicality (skin flaps) | 4.56 ± 0.50 | 5 (1) | 17/17 (100%) |
| 7. Practicality (suturing) | 4.82 ± 0.39 | 5 (0) | 17/17 (100%) |
| 8. Utility (confidence) | 4.29 ± 0.68 | 4 (1) | 15/17 (88%) |
Abbreviations: IQR, interquartile range; SD, standard deviation.
Fig. 4.
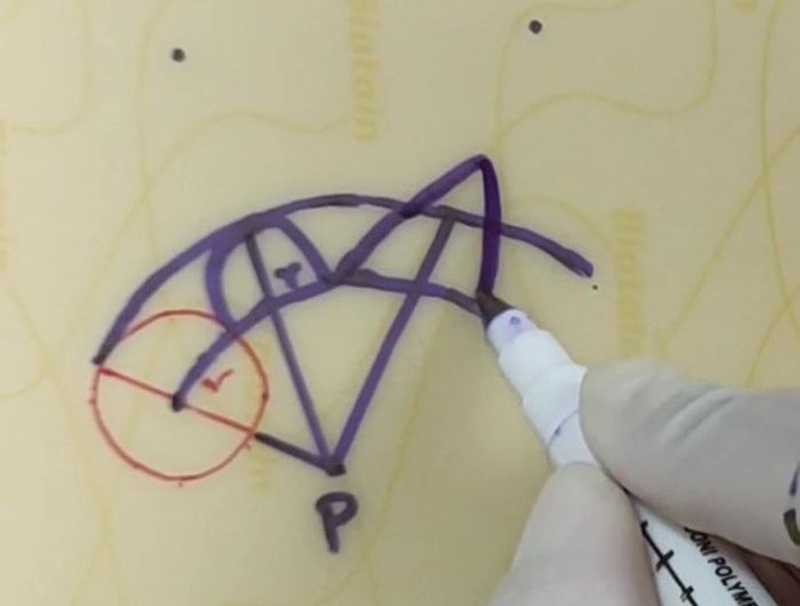
Showing the excellent marking ability nature of simulation model.
Discussion
Simulation models have been known to improve competencies in surgical trainees. 2 The Oxford dictionary has defined competency as “the ability to do something successfully and efficiently.” 3 Keeping the goal of learner competence in mind, competency-based medical education (CBME) is being widely adopted across the globe as well as India. Traditional surgical training has followed Halstedian pattern of residency, which is based on timed exposure and knowledge assessment (loosely translated into on “see one, do one, teach one” model) and aided by the maintenance of operative case logs and board/university examinations. 4 5
The CBME approach in the medical curriculum, which includes flexibility, accountability, and learner-centeredness, was proposed by the erstwhile Medical Council of India (MCI) to improve learners' skills. 6 This approach becomes essential for surgical trainees where a time variable but competency-based learning and assessment will help trainees develop the competencies expected of them once their training is completed. Simulation models in facial plastic surgery, such as shown in this study, will help residents improve cognitive and psychomotor skills and help provide instructors an opportunity to supervise, assess closely, and guide trainee development. 7
Accurate designing and execution of skin flaps are essential, particularly over the face, where the presence of important landmarks interposed with varying areas of lax and taut skin determine flap design and outcomes. An understanding of skin's biomechanical qualities, namely, normal skin tension and directional properties, extensibility and contractility of skin, and viscoelastic properties of skin, help surgeons design and execute skin flaps. 8 For a senior plastic surgeon, this understanding comes from experience, while it is usually a “trial and error” for beginners. Simulation-based learning is a well-accepted active learning process. It is now integrated into undergraduate and postgraduate medical curricula worldwide. 9 The use of simulation in plastic surgery training has been in practice for the last few years. 10 Simulation practice of flap procedures provides trainees a relaxed learning environment, with an opportunity to practice several times and improve upon their mistakes, ultimately building up on their self-confidence. Simulation-based flap learning contributes to patient safety, autonomy, and patient ethics such as social justice. It also prepares the resident with necessary surgical and error management skills. 11
Numerous models have been adopted for cutaneous surgical skill simulation, including dry models such as silicon-based models, foam-based models, hybrid models, and wet models including banana peel, goatskin, pigskin, fresh cadaver, soft embalmed cadaver, etc. Innovative uses of discarded abdominoplasty specimens have also been described. 12 An ideal skin simulation model for surgical skill practice should have the following: viscoelastic properties and color similar to normal skin, odorless, readily available, should not have special storage requirements, be inexpensive, nonmessy during handling and, finally, should not involve ethical or legal issues. A review of the literature reveals that a suitable skin simulation model having the qualities mentioned above for the practice of geometrical skin flaps by learners has been restricted by availability, cost, and other issues. 13 While the commercially designed simulators are expensive, indigenously designed skin models have limitations of availability and standardization. 14 15
Formalin-preserved cadavers have been used traditionally for practice of skin flaps, but these are limited by their availability, need to visit cadaver dissection hall, and a pungent odor that persisted for quite some time after completion of the practice session. Formalin also causes irritation to the eyes. An accurate understanding of the biomechanics of skin flaps is restricted in formalin-preserved skin, owing to the mummification effect of formalin, which makes the skin hard and leathery. This was overcome to some extent by the introduction of soft embalmed cadavers in our institute, which is a specialized process and incurs substantial expenses. The skin textures in soft embalmed cadavers and fresh cadavers resemble natural skin and provide a surgical experience closest to natural. 16 These are, however, again limited by availability and a need to visit the dissection hall. Both these techniques provide the closest anatomical experience, which is essential while designing and executing flaps in various subunits of the face where landmark distortions need to be kept into consideration. Wet skin simulation models described in the literature include goatskin, pigskin, and chicken skin. 17 Although they provide realistic skin experience, termed as “high fidelity,” the use of these is marred by need for a special wet laboratory for practice and proper waste disposal management. Ethnic and cultural issues may also inhibit the use of these among learners. Commercially available skin simulation models have been found to be expensive. They cannot be recommended for routine and repeated practice by residents, although these provide the best models in a workshop setting, where participants may bear the expenses to some extent through registration fees. Foam-based models not unlike ours have been described in literature for suturing practice by surgical trainees, however their use as simulation model for geometrical cutaneous flaps has not been described earlier. 18 19
We have tried to utilize “the best out of waste” from the hospital-based available dressing material either nearing or postclinical use expiry dates, such as the bilayer foam-based adhesive dressing material, as a skin simulation model, for the practice of suturing and flap procedures. The tensile strength and acceptable pliability of the material make it easy to replicate many cutaneous flaps. Although the participants felt a lack of haptic feedback, and the pliability was not as good as normal skin, yet sixty percent of the participants were satisfied during use. It is available in two sizes (10 cm × 10 cm and 15 cm × 10 cm), so small flaps, as well as larger rotation and transposition flaps, could be demonstrated to learners. The outer layer's texture mimics natural skin; hence, it was suitable to practice specialized suturing techniques like purse-string closure, subcuticular stitches, and Gilles A stitch. The adhesive portion of the model helped fix the model to a firm base and mimic fixed zones and boundaries of the face. This made it easier to demonstrate the limits of flap boundaries and the formation of dog ears during flap movements. Although we have used some of the old stock from the hospital pharmacy, the price of each adhesive simulation model is in the range of Rs 300 (4 USD) to Rs 600 (8 USD) and available easily compared with commercial simulation models, which may cost around Rs 2000 (30 USD) to Rs 7000 (900 USD) per piece and are also not readily available locally. Obtaining regular supply of this material may be difficult for routine use. However, these can be procured directly from the manufacturer and utilized for flap training workshop sessions at periodic intervals. One way to address the regular supply of high-fidelity simulation models in a cost-effective manner, particularly in teaching institutes, is the possibility of in-hospital fabrication of simulation models, according to user needs. 20 Till such systems are in place, we believe our low-cost, moderate-fidelity model may address the needs of plastic surgery trainees.
Conclusions
Adhesive bilayer polyurethane foam can be used as a novel cutaneous skin flap simulation model for understanding the biomechanics of skin flaps and cutaneous flap practice. This model is easily available and provides occasions for departments to institute competency-based training in their facial plastic surgery curriculum and allows plastic surgical trainees to improve their surgical skills.
Conflicts of Interests No conflicts of interests.
Source(s) of Support
None.
References
- 1.Kotsis S V, Chung K C. Application of the “see one, do one, teach one” concept in surgical training. Plast Reconstr Surg. 2013;131(05):1194–1201. doi: 10.1097/PRS.0b013e318287a0b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomson J E, Poudrier G, Stranix J T, Motosko C C, Hazen A. Current status of simulation training in plastic surgery residency programs: a review. Arch Plast Surg. 2018;45(05):395–402. doi: 10.5999/aps.2017.01585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soanes C, Stevenson A. Revised Edition. Oxford, UK: Oxford University Press; 2005. The Oxford Dictionary of English. [Google Scholar]
- 4.Nguyen V T, Losee J E. Time- versus competency-based residency training. Plast Reconstr Surg. 2016;138(02):527–531. doi: 10.1097/PRS.0000000000002407. [DOI] [PubMed] [Google Scholar]
- 5.Motola I, Devine L A, Chung H S, Sullivan J E, Issenberg S B. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Med Teach. 2013;35(10):e1511–e1530. doi: 10.3109/0142159X.2013.818632. [DOI] [PubMed] [Google Scholar]
- 6.Shah N, Desai C, Jorwekar G, Badyal D, Singh T. Competency-based medical education: An overview and application in pharmacology. Indian J Pharmacol. 2016;48 01:S5–S9. doi: 10.4103/0253-7613.193312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hopmans C J, den Hoed P T, Wallenburg I. Surgeons' attitude toward a competency-based training and assessment program: results of a multicenter survey. J Surg Educ. 2013;70(05):647–654. doi: 10.1016/j.jsurg.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Gibson T, Kenedi R M. Biomechanical properties of skin. Surg Clin North Am. 1967;47(02):279–294. doi: 10.1016/s0039-6109(16)38180-4. [DOI] [PubMed] [Google Scholar]
- 9.Ericsson K A.Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains Acad Med 200479(10, Suppl)S70–S81. [DOI] [PubMed] [Google Scholar]
- 10.Rosen J M, Long S A, McGrath D M, Greer S E. Simulation in plastic surgery training and education: the path forward. Plast Reconstr Surg. 2009;123(02):729–738. doi: 10.1097/PRS.0b013e3181958ec4. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell N M, Cutting C B, King T W, Oliker A, Sifakis E D. A real-time local flaps surgical simulator based on advances in computational algorithms for finite element models. Plast Reconstr Surg. 2016;137(02):445e–452e. doi: 10.1097/01.prs.0000475793.38984.7e. [DOI] [PubMed] [Google Scholar]
- 12.Gupta S, Mohapatra D P, Chittoria R K. Innovative use of abdominoplasty specimen. J Cutan Aesthet Surg. 2018;11(02):88–90. doi: 10.4103/JCAS.JCAS_55_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khunger N, Kathuria S. Mastering surgical skills through simulation-based learning: Practice makes one perfect. J Cutan Aesthet Surg. 2016;9(01):27–31. doi: 10.4103/0974-2077.178540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delletec Surgical Procedure Simulators (Home page on the internet)Accessed January 25, 2021 at:http://www.delletec.com/Skin%20Closure%202.htm
- 15.Erler-Zimmer Simulators (Home page on the internet)Accessed January 25, 2021 at:https://www.erler-zimmer.de/shop/en/medical-simulators/skin-suture/
- 16.Reddy R, Iyer S, Pillay M, Thankappan K, Ramu J. Soft embalming of cadavers for training purposes: optimising for long-term use in tropical weather. Indian J Plast Surg. 2017;50(01):29–34. doi: 10.4103/ijps.IJPS_219_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denadai R, Toledo A P, Martinhão Souto L R. Basic plastic surgery skills training program on inanimate bench models during medical graduation. Plast Surg Int. 2012;2012:651863. doi: 10.1155/2012/651863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olson J, Kalina C, Berg D. Foam dressing as a suturing model. Dermatol Surg. 2013;39(06):952–953. doi: 10.1111/dsu.12169. [DOI] [PubMed] [Google Scholar]
- 19.Yag-Howard C. Making and using a mouse pad model of skin to practice suturing techniques. Dermatol Surg. 2013;39(12):1947–1949. doi: 10.1111/dsu.12347. [DOI] [PubMed] [Google Scholar]
- 20.Williams T P, Snyder C L, Hancock K J. Development of a low-cost, high-fidelity skin model for suturing. J Surg Res. 2020;256:618–622. doi: 10.1016/j.jss.2020.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]


