Abstract
Purpose
The coronavirus disease-2019 (COVID-19) pandemic had affected the visiting or communicating policies for family members. We surveyed the intensive care units (ICUs) in South Asia and the Middle East to assess the impact of the COVID-19 pandemic on visiting and communication policies.
Materials and method
A web-based cross-sectional survey was used to collect data between March 22, 2021, and April 7, 2021, from healthcare professionals (HCP) working in COVID and non-COVID ICUs (one response per ICU). The topics of the questionnaire included current and pre-pandemic policies on visiting, communication, informed consent, and end-of-life care in ICUs.
Results
A total of 292 ICUs (73% of COVID ICUs) from 18 countries were included in the final analysis. Most (92%) of ICUs restricted their visiting hours, and nearly one-third (32.3%) followed a “no-visitor” policy. There was a significant change in the daily visiting duration in COVID ICUs compared to the pre-pandemic times (p = 0.011). There was also a significant change (p <0.001) in the process of informed consent and end-of-life discussions during the ongoing pandemic compared to pre-pandemic times.
Conclusion
Visiting and communication policies of the ICUs had significantly changed during the COVID-19 pandemic. Future studies are needed to understand the sociopsychological and medicolegal implications of revised policies.
How to cite this article
Chanchalani G, Arora N, Nasa P, Sodhi K, Al Bahrani MJ, Al Tayar A, et al. Visiting and Communication Policy in Intensive Care Units during COVID-19 Pandemic: A Cross-sectional Survey from South Asia and the Middle East. Indian J Crit Care Med 2022;26(3):268–275.
Keywords: Communication barrier, Do not resuscitate orders, End-of-life care, Family communication, Informed consent, Informed consent document, Patient visitors, Terminal care, Visitors to patients
Keypoints
The pandemic of coronavirus disease-2019 has significantly changed the visiting and communication policies in intensive care units of South Asian and Middle East countries.
Most of the ICUs have restricted visitors in ICU, and communication with family members has changed from in-person to virtual.
There was also a significant change in the process of informed consent and end-of-life discussions during the ongoing pandemic compared to pre-pandemic times.
Introduction
Healthcare professionals (HCPs) in intensive care units (ICUs) find communication with family members of critically ill patients often challenging. The ICU environment has an immense impact on the family members and is linked to higher anxiety, stress, and depression.1,2 An effective communication between HCPs and family members on various aspects of the patient care plan can mitigate the psychological stress and increase satisfaction.3 Other circumstances where family member–physician communication is pivotal include informed consent for emergency surgery or ICU procedures, end-of-life (EOL) decisions, and medical incidents or errors. Azoulay et al. proposed a two-step model to improve family–physician interactions in ICU, providing early and adequate information to family members and their involvement in decision-making.4
Historically, visiting hours in ICU were restricted on the grounds of infection control, emotional stress to the patient, or smooth functioning of ICU.5 The stay of patients in ICU is stressful for their family members. Staying close to their loved ones and periodic communication with HCPs are essential measures that can reduce anxiety and distress among family members. The open-door policy, flexible visiting hours, effective communication with family members, and their involvement in clinical decision-making or EOL decisions have been a matter of intense discussion in the last few years. There has been an intense effort on “humanizing care” in ICU with various innovative initiatives.6,7 The evidence has started emerging on the benefits of flexible visiting policy in ICU for reduction of posttraumatic stress, delirium, and enhanced patient safety.1,8 A recent meta-analysis on flexible vs restricted visiting hours found a reduction of anxiety and delirium in patients and an improved satisfaction rate among family members with flexible visiting hours.9
The pandemic of COVID-19 from its inception brought a considerable strain to the healthcare resources, and various adaptations were made to mitigate this challenge.10,11 ICU visiting policy was either changed to “no-visitors” or restricted by frequency or number of visitors. Restrictions on visiting hours were placed in the context of public health safety to protect patients, family members, and HCPs.12–14 The unprecedented surge of critically ill patients during waves of pandemic inundated ICUs and affected the process of communication. The effects of these measures were expected to be exponential in resource-limited countries.
The countries of South Asia and the Middle East have a combined population of 2.37 billion or nearly one-third of the world population. Besides a long history of trade, the relations among these countries are deeply rooted because of religion and sociocultural linkages.15 Religion and culture have considerable influence on shared decision-making between HCPs and family members. This is pertinent to EOL decisions such as withdrawing and withholding treatment, medical futility, and do not attempt to resuscitate (DNAR) orders.16 We conducted a multicenter survey across South Asia and the Middle East to assess the visiting and communication policies in ICU during pre-pandemic times and their changes after the onset of the pandemic of COVID-19.
Materials and Methods
An online cross-sectional survey was conducted across South Asia and Middle East countries between March 22, 2021 and April 7, 2021. The investigators GC, PN, and NA performed a literature search on “Google Scholar” and “PubMed” electronic databases using search terms “communication” OR “family members” OR “family-physician communication” OR “informed consent” OR “visiting hours” AND “COVID-19” OR “SARS-CoV-2”. We reviewed all English language published research, including regional or national guidance, recommendations from World Health Organization (WHO) or Centre for Disease Control and Prevention (CDC) published between January 1, 2020 and March 10, 2021.
Participant Recruitment
Seventeen members representing different countries in the region with a background in intensive care medicine, anesthesiology, internal medicine, or public health were invited into the steering committee.
The country coordinator from the steering committee was responsible for collecting regional data on ICUs and inviting participants through e-mail or social media. The survey was circulated among eligible participants through snowball sampling. We made a concerted effort to invoke participation from all the countries across the region based on confirmed cases of COVID-19. Only one response per ICU was allowed from either senior physician, nurse, or administrator. Any duplicate entries were deleted after a discussion with the country coordinator. Different responses were collected for ICUs admitting patients with COVID-19 (COVID ICU) and ICUs admitting other patients (non-COVID ICU). There is no information available on number of ICUs in this region, so target sample population could not be calculated.
Survey Questionnaire
The survey questionnaire was prepared from the literature search and feedback from members of the steering committee.10,11,17,18 The questionnaire consisted of two sections, besides information on the demographics of the participants and their ICUs. Information on the model of ICUs based on the extent of intensivist involvement, like open, closed, or semi-closed was also collected.19 Section one collected data on the communication and visitor policies in ICU during the pre-pandemic time (before March 11, 2020), and section two collected information on current policies. Multiple-choice questions on visiting hours in the ICU, method of HCP–family member interactions, informed consent, and EOL discussion or DNAR were used to collect information in the survey (Supplement 1: Original survey). We also collected information on the HCPs responsible for communication with family members before and during the pandemic. The comments and opinions on current policies were collected through a free text option at the end of the survey. We conducted a dry run of the survey among the steering committee members to correct typographical errors and to include regional, cultural, or practice variations.
The survey did not invoke any patient information. The consent for participation and publication of the results was obtained from the responders. The ethics approval was obtained from the hospital ethics committee of principal investigators, KS and GC, and wherever required by the country coordinators. The approval was obtained from the institutional clinical research and ethics committee (CREC-2133/2021) by the principal investigators: KS and GC. The steering committee members took necessary ethics approval from their respective countries. The survey was registered in clinicaltrials.gov (Identifier: NCT04602351). We used Consensus-based Checklist for Reporting of Survey Studies (CROSS) (Supplement 2: CROSS checklist).20
Statistical Analysis
Categorical data were summarized using frequencies and percentages. The comparison between two categorical variables was made using Chi-square Pearson's test. All tests were two-tailed, and p <0.05 was taken for statistical significance. Missing data were not imputed for the analysis. The analysis was performed using Statistical Package for the Social Sciences (SPSS) software (version 25) (IBM Corp., Armonk, New York, USA).
Results
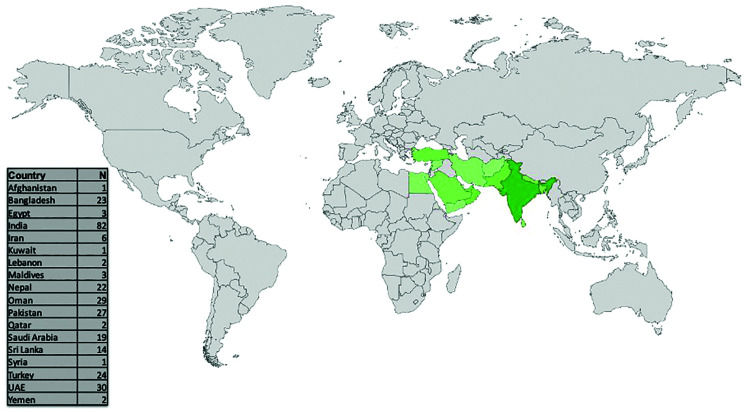
A total of 331 responses were received from 18 countries across South Asia and the Middle East (Fig. 1). After excluding 39 duplicate entries, 292 responses representing an equal number of ICUs were included in the final analysis. Most (99.1%) of the responses were received through HCPs working in ICU. Out of 292 ICUs, 213 (72.9%) were COVID ICUs, 69.7% were closed, or semi-closed ICU models, and 65.9% were mixed, receiving medical and surgical patients.
Fig. 1.
Geographical representation of the number of ICUs who participated in the cross-sectional survey. N represents the number of ICUs from each country; ICU, intensive care units
From the inception of the COVID-19 pandemic, 92% of ICUs had changed their policy to restricted visiting hours, while only 7.2% reported no change compared to pre-pandemic times (Table 1). Restriction of visiting hours included “no-visitor” policy for 32.3% of ICUs and visitors only for vulnerable patients or in exceptional circumstances like EOL care for 35.4% of ICUs. Most of the ICUs (79.5%) in the region have a visiting policy of fixed hours in the pre-pandemic times. The daily duration of the visit by family members or friends was limited to less than 6 hours in 82.2% of ICUs during pre-pandemic times. During the ongoing pandemic, fixed visiting hours were further reduced in 65.3% of ICUs. There was a nonsignificant change in the duration of visiting family members before vs during the pandemic (p = 0.16). However, there was a significant change in the daily visiting duration when only COVID ICUs were compared to the pre-pandemic times (p = 0.01) (Table 2). Multiple HCPs, like primary admitting physicians (51.4%), ICU consultants (79.8%), or specialist trainees/residents (55.3%), were responsible for communication with family members in ICUs (Table 3). There was a significant change in the HCPs responsible for handling the communication during the ongoing pandemic compared to the pre-pandemic time in COVID ICUs (p = 0.01), but it was nonsignificant overall (p = 0.27) (Table 3). During pre-pandemic times, most of the ICUs (94.5%) allowed in-person communication, and the place for communication was a dedicated room (44.7%), ICU corridor (26.6%), or patient's bedside (24.5%).
Table 1.
Descriptive statistics of multiple-choice questions used in the survey
| Questions in the survey, n (%) | Responses (%) | ||||||
|---|---|---|---|---|---|---|---|
| Type of ICUs | Open: 88 (30.2%) | Closed: 104 (35.6%) | Semi-closed: 100 (34.1%) | ||||
| Type of patients in ICU | Medical: 50 (17.2%) | Surgical: 11 (3.6%) | Mixed: 191 (65.9%) | Cardiac: 11 (3.6%) | Neurology: 6 (2.1%) | New COVID: 5 (1.6%) | Others: 18 (6%) |
| Pre-pandemic time | |||||||
| Visiting policy | Fixed visiting hours: 232 (79.5%) | Flexible visiting hours: 28 (9.7%) | No visiting: 16 (5.4%) | Flexible visiting for vulnerable and EOL: 64 (21.8%) | Other: 5 (1.8%) | ||
| Visiting (hours/day) | 24 hours: 18 (6.3%) | 12–24 hours: 5 (1.8%) | 6–12 hours: 13 (4.5%) | 3–6 hours: 5 (17.8%) | <3 hours: 188 (64.4%) | Other: 15 (5.2%) | |
| HCP responsible for family communication | Admitting physician: 150 (51.4%) | ICU consultant: 233 (79.8%) | Specialist trainee: 161 (55.3%) | Nurse: 72 (24.8%) | Dedicated team: 11 (3.9%) | Other: 20 (6.9%) | |
| Place for HCP-family communication | Bedside: 72 (24.5%) | Dedicated room: 131 (44.7%) | Corridor/ad-hoc space: 78 (26.6%) | Other: 12 (4.2%) | |||
| Procedure of informed consent | In-person and documentation: 272 (93.1%) | In-person under video/audio recording and documentation: 17 (5.9%) | Recorded video/audio: 2 (0.7%) | Recorded video/audio and documentation by physician: 1 (0.3%) | |||
| Procedure for DNAR or EOL discussions with family members | In-person: 239 (81.8%) | In-person or video, audio recording: 8 (2.7%) | Video/audio calling to family members: 2 (0.7%) | Other: 43 (14.8%) | No DNAR: 38 (13%) | ||
| HCP responsible for DNAR or EOL discussions | Consultant: 145 (49.7%) | Specialist trainee: 17 (5.8%) | Combined: 91 (31.2%) | Nurse 0 | Dedicated team: 1 (0.3%) | Other (Public relation officer/administrator/nontreating consultant) 38 (13%) | No DNAR: 38 (13%) |
| During COVID-19 pandemic | |||||||
| Visiting restricted more than pre-pandemic time | Yes: 269 (92.1%) | No change: 22 (7.2%) | Liberal: 1 (0.7%) | ||||
| Visiting policy | Daily: 70 (23.9%) | Alternate day: 2 (0.6%) | On request: 91 (31.1%) | Only during EOL care: 65 (22.1%) | Vulnerable patients: 39 (13.3%) | Never: 94 (32.3%) | Other: 11 (3.6%) |
| Are families being communicated? | Yes: 274 (94%) | No: 18 (6%) | |||||
| Frequency of communication | Once/day: 140 (48%) | Twice/day: 90 (30.8%) | During any significant change in patient condition: 133 (45.6%) | Every time family members want to know: 93 (31.7%) | Other: 8 (2.7%) | ||
| Method of family communications | Audio calls by ICU team: 197 (67.4%) | Audio calls made by family members: 78 (26.6%) | Video conference: 59 (20.2%) | In-person: 131 (45%) | Other: 7 (2.4%) | ||
| HCP responsible for family members communication | Admitting physician: 132 (45.3%) | ICU consultant: 221 (75.8%) | Specialist trainee: 168 (57.4%) | Nurse: 69 (23.6%) | Dedicated team: 13 (4.5%) | Other: 18 (6.3%) | |
| Type of ICUs | Open: 88 (30.2%) | Closed: 104 (35.6%) | Semi-closed: 100 (34.1%) | ||||
| Type of patients in ICU | Medical: 50 (17.2%) | Surgical: 11 (3.6%) | Mixed: 191 (65.9%) | Cardiac: 11 (3.6%) | Neurology: 6 (2.1%) | New COVID: 5 (1.6%) | Others: 18 (6%) |
| Procedure of informed consent | In-person and documentation: 120 (41%) | In-person under video/audio recording and documentation: 44 (14.8%) | Recorded video/audio: 25 (8.6%) | Recorded video/audio and documentation by physician: 104 (35.5%) | |||
| Procedure for DNAR or EOL discussion with family members | In-person: 133 (45.5%) | In-person under video, audio recording: 69 (23.6%) | Video/audio calling to family members: 49 (16.8%) | Other: 41 (14.1%) | No DNAR: 40 (14%) | ||
| HCP responsible for DNAR or EOL discussion | Consultant: 122 (41.8%) | Specialist trainee: 21 (7.2%) | Combined: 105 (36%) | Nurse: 1 (0.3%) | Dedicated team: 1 (0.3%) | Other (Public relation officer/administrator/nontreating consultant): 42 (14.4%) | No DNAR: 40 (14%) |
N, number of ICUs; ICU, intensive care unit; DNAR, do not attempt to resuscitate; HCP, healthcare professional; EOL, end-of-life-care; COVID-19, coronavirus disease-2019. Dedicated team: designated team of physician, nurse, and social worker for communication on EOL or DNAR
Table 2.
Change in visiting policy from pre-pandemic times for all ICUs and COVID ICUs
| Visiting policy | Liberal | Same as before | Restricted | Chi-square p value | |
|---|---|---|---|---|---|
| All ICUs | |||||
| Fixed visiting hours only | 3 (60%) | 9 (50%) | 175 (65.3%) | 0.156 | |
| Fixed visiting hours except for vulnerable patients and EOL care | 0 | 1 (5.6%) | 42 (15.7%) | ||
| No-visitor policy | 1 (60%) | 2 (11.0%) | 14 (5.2%) | ||
| No-visitor policy except for vulnerable patients and EOL care | 0 | 1 (5.6%) | 14 (5.2%) | ||
| Open visiting (at any time) | 1 (20%) | 5 (27.8%) | 21 (7.8%) | ||
| COVID ICUs | |||||
| Fixed visiting hours only | 3 (100%) | 5 (45.5%) | 128 (64.3%) | 0.011 | |
| Fixed visiting hours except for vulnerable patients and EOL care | 0 | 0 | 32 (16.1%) | ||
| No-visitor policy | 0 | 0 | 11 (5.5%) | ||
| No-visitor policy except for vulnerable patients and EOL care | 0 | 0 | 10 (5%) | ||
| Open visiting (at any time) | 0 | 6 (54.5%) | 16 (8%) | ||
p <0.05 is significant, EOL, end-of-life; ICU, intensive care unit. Liberal: Visiting policy was changed to either increased duration or number of visitors compared to pre-pandemic times. Restricted: Visiting policy was changed to either restriction in duration or number of visitors compared to pre-pandemic times
Table 3.
Comparison of communication policy, DNAR, or EOL care discussion with family members pre-pandemic time and during pandemic of COVID-19
| Policy or process compared | Variables | Pre-pandemic times | During pandemic | Chi-square (p value) |
|---|---|---|---|---|
| Process of communication with family members | In-person counseling and documentation | 269 (93.1%) | 119 (41%) | <0.001 |
| In-person under video/audio recording and documentation | 17 (5.9%) | 43 (14.8%) | ||
| Recorded video/audio (no in-person) | 2 (0.7%) | 25 (8.6%) | ||
| Recorded video/audio and physician documentation in medical records | 1 (0.3%) | 103 (35.5%) | ||
| Healthcare professional responsible for communication with family members | Primary treating team | 23 (7.9%) | 19 (6.5%) | 0.27 |
| ICU consultant | 64 (22.1%) | 56 (19.2%) | ||
| Specialist trainee | 15 (5.2%) | 25 (8.6%) | ||
| Nursing | 3 (1%) | 7 (2.4%) | ||
| Any of the above | 180 (61.1%) | 183 (62.6%) | ||
| Others (dedicated team) | 5 (1.7%) | 2 (0.7%) | ||
| DNAR or EOL care discussion with family members | No DNAR policy | 38 (13%) | 41 (14%) | <0.001 |
| In-person | 239 (81.8%) | 133 (45.5%) | ||
| In-person, video, and audio | 8 (2.7%) | 69 (23.6%) | ||
| Video and audio | 2 (0.7%) | 49 (16.8%) | ||
| Healthcare professional responsible for DNAR or EOL care discussion with family members | Consultant | 145 (49.7%) | 122 (41.8%) | 0.459 |
| Specialist trainee | 17 (5.8%) | 21 (7.2%) | ||
| Combined | 91 (31.2%) | 106 (36.0%) | ||
| Dedicated team | 1 (0.3%) | 1 (0.3%) | ||
| Nursing | 0 (%) | 1 (0.3%) | ||
| No DNAR policy | 38 (13%) | 41 (14%) |
p <0.05 is significant. COVID-19, coronavirus disease-2019; DNAR, do not attempt to resuscitate; EOL, end-of-life-care
Before the COVID-19 pandemic, the process of informed consent for nonemergent or a surgical procedure was performed in-person in 93.1% of ICUs, and 5.9% of ICUs were additionally video or audio recording the process. There was a significant change (p <0.001) during the ongoing pandemic, with only 41% of ICUs were obtaining informed consent through family members in-person, while 35.5% obtaining consent through a telephone or video call (Table 3). The change in process for informed consent was significant in COVID ICUs (p = 0.01) (Table 4). Around 13% of ICUs in the region do not have a DNAR policy (Table 1). During the pre-pandemic time, nearly all ICUs (99.1%) involved family members in-person for EOL decisions. There was a significant change in the process of communication during the pandemic, with only 45.5% of ICUs agreed to have such discussions in-person (p <0.001) (Table 3). The ICU consultant was primarily responsible for handling communication about EOL decisions with family members with no significant change (p = 0.46) during pandemic (41.8%) compared to pre-pandemic times (49.7%) (Tables 1 and 3).
Table 4.
Comparison of COVID ICUs and non-COVID ICUs for counseling team and process of informed consent
| Variable | Change in policy | COVID ICU | Non-COVID ICU | Chi-square p value |
|---|---|---|---|---|
| Counseling team | No change | 87 (41%) | 39 (49.4%) | 0.012 |
| Complete change | 24 (11.3%) | 7 (8.9%) | ||
| Partial change | 101 (47.6%) | 33 (41.8%) | ||
| Informed consent | No change | 74 (34.7%) | 41 (51.9%) | 0.008 |
| Complete change | 134 (62.9%) | 34 (43%) | ||
| Partial change | 5 (2.3%) | 4 (5.1%) |
p <0.05 significant. COVID-19, coronavirus disease-2019; ICU, intensive care unit
The qualitative comments from the participants were allowed on their problems, satisfaction, and concerns related to visiting policies during the COVID-19 pandemic. Many respondents expressed their discontent on “breaking bad news,” documentation of verbal consent, and laborious communication efforts during the surge of patients. Few of these comments are mentioned in the following.
The communication during COVID-19 pandemic is considerably compromised in the absence of direct contact, and telephonic or video communication was insufficient to convey critical conditions to family members.
The physicians were busy in clinical work, and communication is usually pushed to a lower priority.
The change in visiting policy is traumatic from the patient's perspective. In the absence of family members, the anxiety, stress, and fear of own health are amplified.
Making the patient and attendants understand the risk and need for isolation was tiring.
It is a very sensitive and emotional issue and patient relatives often become aggressive if not communicated well.
Communication with all relatives of patient with COVID-19 is a difficult task as they are not visiting the patient and insecurity feelings are there.
The absence of family members made them worry about the family and fear social stigmata after discharge.
Discussion
The COVID-19 pandemic has imposed unique challenges to the healthcare systems globally. Infection control measures requiring social distancing and restricted movements developed barriers to communication between family members and HCPs. This cross-sectional study was conducted in ICUs of South Asia and the Middle East countries on visiting policy, informed consent, and communication with family members during COVID-19 pandemic and change from pre-pandemic times. During pre-pandemic times, most of the ICUs allowed visitors for less than 6 hours, and the visiting policy was significantly restricted during the ongoing pandemic. Nearly two-thirdd of ICUs changed their visiting policies to a “no-visitor” policy, or visitors only in extraordinary circumstances. ICUs allowing in-person communication with family members nearly dropped by half during pandemic compared to pre-pandemic times. There was a significant change in communication with family members on informed consent and EOL decisions.
Majority (79.5%) of the ICUs in our study followed a limited (fixed) visiting policy even during pre-pandemic times. There is an open debate regarding humanizing ICUs with greater involvement of patients and their family members in the care process.6 Despite its benefits, the adoption of flexible or open visiting policy in ICUs faced various challenges.21 The research on adopting an open visiting policy in ICU is largely done in Europe, North America, or Australia.22 Few studies before the COVID-19 pandemic also reported a fixed duration visitation policy in South Asia and the Middle East. Sociocultural and religious differences, shortage of nursing staff, impact on ICU functioning, and absence of research were some of the perceived barriers to open visiting policy.22,23
Most of the (92.1%) ICUs in the region changed the visiting policy during COVID-19 pandemic to restrict the visitors compared to pre-pandemic times. The COVID-19 pandemic had considerably affected the visiting policy with restriction of visitors in ICUs.11,17,18 The alteration in visiting policy also affected communication and made the process stressful and demanding for HCPs. Nearly one-third ICUs completely stopped visitors to the ICUs. At the same time, another one-third allowed visitors only for exceptional situations like for vulnerable patients (e.g., pediatric or elderly) or EOL care of a terminally ill patient. Though non-COVID ICUs also adopted a more-restricted visiting policy, it was statistically significant only for COVID ICUs. Only few ICUs (7.2%) which were non-COVID ICUs did not change visiting policy during the pandemic. We could not collect information on any additional precautions which were considered for these ICUs with unchanged policy. The alteration of visiting policy in COVID ICUs is also in line with the recommendations of public health agencies to limit visitors in ICUs to reduce the risk of cross-infection.13,14
Informed consent for an invasive procedure has medicolegal implications and engenders trust in the physician, with a higher satisfaction rate among family members. The consent for a nonemergent procedure in a critically ill patient in ICU is commonly obtained from a proxy (usually a family member). In our study, there was a significant change observed in the process of informed consent, with many ICUs resorting from in-person documentation to audio/video-based verbal consent. Even during pre-pandemic times, there was a considerable gap in the informed consent process. In a multicenter cross-sectional survey, more than half (51%) of next-of-kin failed to identify the procedures, which they consented.24
The DNAR directive is a core component of EOL decisions. The DNAR directive to preserve the dignity of a dying patient has an established place in ICUs of different parts of the world. Around 13% of ICUs in our survey did not have a policy of DNAR in pre-pandemic times. The process of communication with family members on EOL decisions and DNAR directives is challenging and requires an open face-to-face discussion. However, there is wide variation in EOL care in South Asia and the Middle East because of social, cultural, and religious beliefs.25–29 Recently, Indian government guidelines on DNAR directives proposed to include family members in close communication with treating physicians to facilitate EOL decisions in the patient's best interests.2 The pandemic has altered the involvement of family members, with nearly half the number of ICUs employed audio or video communication instead of in-person. This change again was seen more prominently in COVID ICUs as compared to non-COVID ICUs. This is expected to compromise the trust and confidence of the family members in such crucial decisions. However, systematic remote counseling of family members on EOL decisions during COVID-19 in a single-center study reported significantly improved ratings by the bereaved family members.30
The qualitative comments highlighted the challenges and higher personal dissatisfaction among HCPs with the altered communication process during the COVID-19 pandemic. Many participating physicians appreciated that the remodeling of current communication processes during the COVID-19 pandemic is required and may improve the physician–family member relation, satisfaction level, and reduced risk of medical error. Many others felt an urgent need to improve communication to avoid litigations or medicolegal problems.
Strength and Limitations
Our study has many strengths. Firstly, to our knowledge, this cross-sectional survey from the third world in South Asia and the Middle East region with culture and social similarities reflect the visiting and communication policy for family members during COVID-19 pandemic. Secondly, in the absence of limited previous research from this region on such policies, we also collated information on pre-pandemic times to understand baseline practices. Thirdly, we tried to include ICUs from all major countries in the region simultaneously over 2 weeks to capture a snapshot of visiting and communication policies. Finally, we included COVID ICUs and non-COVID ICUs to understand the practice variation during the COVID-19 pandemic.
There are a few limitations of our study:
The clubbed question on EOL and DNAR policy questions may have affected the responses, as few countries did not have legal DNAR directives.
The exclusion of patients and family members from the survey may have missed crucial information on the impact of these policies on their social and psychological well-being.
The survey results may not be representing. Without information on the number of ICUs from the region, we could not analyze the response rate.
Inherent limitations of a cross-sectional survey, snowball recruitment, and recall bias may affect the generalizability of our results.
The survey demonstrates a snapshot (point prevalence) and does not reflect the trend in the policies over the course of the pandemic. However, we provided a free text section in the survey to collect practice variations throughout the pandemic.
Conclusion
There was a significant change in the visiting policy of the ICUs during the COVID-19 pandemic. Most ICUs restricted visitors, with nearly one-third of ICUs, resorted to a “no-visitor” policy. In-person communication with family members nearly dropped by half during the pandemic compared to pre-pandemic times. There was a significant change in communication with family members on informed consent and discussion related to EOL decisions. There is an urgent need for future research to understand the effect of these altered policies on the satisfaction or psychological well-being of patients and family members.
Footnotes
Source of support: Nil
Conflict of interest: None
Orcid
Gunjan Chanchalani https://orcid.org/0000-0001-8429-8526
Nitin Arora https://orcid.org/0000-0001-9941-8340
Prashant Nasa https://orcid.org/0000-0003-1948-4060
Kanwalpreet Sodhi https://orcid.org/0000-0002-7377-9225
Maher J Al Bahrani https://orcid.org/0000-0002-9177-521X
Ashraf Al Tayar https://orcid.org/0000-0002-2897-7417
Madiha Hashmi https://orcid.org/0000-0002-7332-0692
Vinod Jaiswal https://orcid.org/0000-0001-8365-6758
Sandeep Kantor https://orcid.org/0000-0002-4491-6198
Ahsina J Lopa https://orcid.org/0000-0002-5336-4217
Bassam Mansour https://orcid.org/0000-0002-5640-0631
Anushka D Mudalige https://orcid.org/0000-0002-5264-1585
Rashid Nadeem https://orcid.org/0000-0003-3785-2832
Gentle S Shrestha https://orcid.org/0000-0003-0385-2340
Ahmed R Taha https://orcid.org/0000-0001-7901-9553
Melda Türkoğlu https://orcid.org/0000-0003-4043-7082
Dameera Weeratunga https://orcid.org/0000-0002-5899-3741
Supplementary Material
All the supplementary material are available online on the website of www.IJCCM.org
References
- 1.Kynoch K, Chang A, Coyer F, McArdle A. The effectiveness of interventions to meet family needs of critically ill patients in an adult intensive care unit: a systematic review update. JBI Database System Rev Implement Rep. 2016;14(3):181–234. doi: 10.11124/JBISRIR-2016-2477. [DOI] [PubMed] [Google Scholar]
- 2.Alfheim HB, Hofsø K, Småstuen MC, Tøien K, Rosseland LA, Rustøen T. Post-traumatic stress symptoms in family caregivers of intensive care unit patients: a longitudinal study. Intensive Crit Care Nurs. 2020;50:5–10. doi: 10.1016/j.iccn.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 3.CoBaTrICE Collaboration. The views of patients and relatives of what makes a good intensivist: a European survey. Intensive Care Med. 2007;33:1913–1920. doi: 10.1007/s00134-007-0799-4. [DOI] [PubMed] [Google Scholar]
- 4.Azoulay E, Sprung CL. Family-physician interactions in the intensive care unit. Crit Care Med. 2004;32(11):2323–2328. doi: 10.1097/01.ccm.0000145950.57614.04. [DOI] [PubMed] [Google Scholar]
- 5.Lee MD, Friedenberg AS, Mukpo DH, Conray K, Palmisciano A, Levy MM. Visiting hours policies in New England intensive care units: strategies for improvement. Crit Care Med. 2007;35(2):497–501. doi: 10.1097/01.CCM.0000254338.87182.AC. [DOI] [PubMed] [Google Scholar]
- 6.Heras La Calle G, Oviés ÁA, Tello VG. A plan for improving the humanisation of intensive care units. Intensive Care Med. 2017;43(4):547–549. doi: 10.1007/s00134-017-4705-4. [DOI] [PubMed] [Google Scholar]
- 7.Pollard K, Wessman BT. Development of a standardized communication intervention bundle for use at a medical training hospital intensive care unit. Indian J Crit Care Med. 2019;23(5):234–235. doi: 10.5005/jp-journals-10071-23168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosa RG, Falavigna M, Robinson CC, da Silva DB, Kochhann R, de Moura RM, et al. Study protocol to assess the effectiveness and safety of a flexible family visitation model for delirium prevention in adult intensive care units: a cluster-randomised, crossover trial (The ICU Visits Study). BMJ Open. 2018;8(4):e021193. doi: 10.1136/bmjopen-2017-021193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nassar Junior AP, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: a systematic review and meta-analysis. Crit Care Med. 2018;46(7):1175–1180. doi: 10.1097/CCM.0000000000003155. [DOI] [PubMed] [Google Scholar]
- 10.Auerbach A, O'Leary KJ, Greysen SR, Harrison JD, Kripalani S, Ruhnke GW, et al. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483–488. doi: 10.12788/jhm.3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valley TS, Schutz A, Nagle MT, Miles LJ, Lipman K, Ketcham SW, et al. Changes to visitation policies and communication practices in Michigan ICUs during the COVID-19 pandemic. Am J Respir Crit Care Med. 2020;202(6):883–885. doi: 10.1164/rccm.202005-1706LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201(11):1337–1344. doi: 10.1164/rccm.202004-1037CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC. Management of visitors to healthcare facilities in the context of COVID-19: non-US healthcare settings. 2020. [Accessed July 29, 2021]]. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html/ Available from:
- 14.WHO. Infection prevention and control of epidemic-and pandemic prone acute respiratory infections in health care. 2020. [[Accessed July 29, 2021]]. https://www.who.int/publications/i/item/infection-prevention-and-control-of-epidemic-and-pandemic-prone-acute-respiratory-infections-in-health-care/ Available from: [PubMed]
- 15.Pillalamarri A. South Asia: tethered to the Middle East; Southeast Asia: tethered to China. The Diplomat. 2020. [[Accessed July 24, 2021]]. https://thediplomat.com/2016/03/south-asia-tethered-to-the-middle-east-southeast-asia-tethered-to-china/ Available from:
- 16.Jahn Kassim PN, Alias F. Religious, ethical and legal considerations in end-of-life issues: fundamental requisites for medical decision making. J Relig Health. 2016;55(1):119–134. doi: 10.1007/s10943-014-9995-z. [DOI] [PubMed] [Google Scholar]
- 17.Rose L, Yu L, Casey J, Cook A, Metaxa V, Pattison N, et al. Communication and virtual visiting for families of patients in intensive care during COVID-19: a UK National Survey. Ann Am Thorac Soc. 2021;18(10):1685–1692. doi: 10.1513/AnnalsATS.202012-1500OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boulton AJ, Jordan H, Adams CE, Polgarova P, Morris AC, Arora N. Intensive care unit visiting and family communication during the COVID-19 pandemic: a UK survey. J Intensive Care Soc. 2021. [DOI] [PMC free article] [PubMed]
- 19.Chowdhury D, Duggal AK. Intensive care unit models: do you want them to be open or closed? A critical review. Neurol India. 2017;65(1):39–45. doi: 10.4103/0028-3886.198205. [DOI] [PubMed] [Google Scholar]
- 20.Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, et al. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Intern Med. 2021;36(10):3179–3187. doi: 10.1007/s11606-021-06737-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olding M, McMillan SE, Reeves S, Schmitt MH, Puntillo K, Kitto S. Patient and family involvement in adult critical and intensive care settings: a scoping review. Health Expect. 2016;19(6):1183–1202. doi: 10.1111/hex.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ning J, Cope V. Open visiting in adult intensive care units–a structured literature review. Intensive Crit Care Nurs. 2020;56:102763. doi: 10.1016/j.iccn.2019.102763. [DOI] [PubMed] [Google Scholar]
- 23.Khaleghparast S, Joolaee S, Ghanbari B, Maleki M, Peyrovi H, Bahrani N. A review of visiting policies in intensive care units. Glob J Health Sci. 2015;8(6):267–276. doi: 10.5539/gjhs.v8n6p267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Modra LJ, Hart GK, Hilton A, Moore S. Informed consent in the intensive care unit: the experiences and expectations of patients and their families. Crit Care Resusc. 2014;16(4):262–268. 25437219 [PubMed] [Google Scholar]
- 25.Immad SQ. DNAR decisions in Pakistan, Middle East, and UK: an emergency physician's perspective. South Asian J Emerg Med. 2018;2(1):1–5. doi: 10.5455/sajem.020107. [DOI] [Google Scholar]
- 26.Madadin M, Alsaffar GM, AlEssa SM, Khan A, Badghaish DA, Algarni SM, et al. Clinicians’ attitudes towards do-not-resuscitate directives in a teaching hospital in Saudi Arabia. Cureus. 2019;11:e6510. doi: 10.7759/cureus.6510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baykara N, Utku T, Alparslan V, Arslantaş MK, Ersoy N. Factors affecting the attitudes and opinions of ICU physicians regarding end-of-life decisions for their patients and themselves: a survey study from Turkey. PLoS One. 2020;15(5):e0232743. doi: 10.1371/journal.pone.0232743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mathur R. ICMR consensus guidelines on ‘do not attempt resuscitation’. Indian J Med Res. 2020;151(4):303–310. doi: 10.4103/ijmr.IJMR_395_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choudhuri AH, Sharma A, Uppal R. Effects of delayed initiation of end-of-life care in terminally ill intensive care unit patients. Indian J Crit Care Med. 2020;24(6):404–408. doi: 10.5005/jp-journals-10071-23454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ersek M, Smith D, Griffin H, Kinder D, Thorpe JM, Kutney-Lee A. End-of-life care in the time of COVID-19: communication matters more than ever. J Pain Symptom Manage. 2021;S0885-3924(20):30975-1. doi: 10.1016/j.jpainsymman.2020.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]