Abstract
Background
The French government issued national COVID-19-related confinement and stay-at-home orders depending on different epidemic levels in a bid to stem the coronavirus pandemic and its resurgence. The long-term impact of lockdown measures on the general population may vary. We aimed to identify and characterize self-reported mental and physical health trajectories in the French population from pre-lockdown to the first and second COVID-19 lockdowns and to identify factors associated with health status variation patterns.
Methods
We did a secondary analysis of the MAVIE cohort in France. Volunteers of this national cohort were recruited between November 2014 and December 2019, and information was collected at recruitment (pre-lockdown), April–May 2020 (the first lockdown), and October–December 2020 (the second lockdown). Latent class mixed models were built to identify distinct anxiety (as measured by GAD-7) and depressive (as measured by PHQ-9) symptoms, and self-perceived mental and physical health trajectories. Factors associated with status variation were identified by logistic or multinomial regression.
Results
A total of 613 participants with data in all three data collection waves were included. Respondents spent almost half as much time on traditional media, websites and social media during the second lockdown as during the first. Mean anxiety scores were 1.96, 2.37 and 2.82 at pre-lockdown, and the first and second lockdowns, respectively. Mean depressive scores were 3.12, 3.36 and 3.95, respectively. Latent class mixed models fitted two and three distinct trajectory classes respectively for anxiety symptoms (‘no pre-pandemic anxiety, slightly increase’, 58.9%; ‘consistently fair’, 41.1%) and depressive symptoms (‘consistently very low’, 34.6%; ‘consistently low’, 56.1%; ‘increasing and clinically significant at the second lockdown’, 9.3%), and four classes for self-perceived mental and physical health. Females were more likely to belong to trajectories of the most vulnerable one as regard to the symptoms of anxiety and depression, and self-perceived mental and physical health. The younger participants were also more vulnerable to anxiety symptoms and those with a clinical diagnosis or a positive COVID-19 test for the participant or relatives were more likely to belong to vulnerable trajectories for depressive symptoms and self-perceived mental health.
Conclusion
A continuing increase in the mean scores of anxiety and depression symptoms was observed throughout the two lockdown periods in France. Further analyses revealed distinct patterns with a small fraction of volunteers experiencing worsening mental and physical health symptoms. This vulnerable small part of the population requires targeted support.
Keywords: COVID-19 lockdown, Latent class trajectory, Anxiety symptoms, Depression symptoms, Mental health, Physical health
1. Introduction
The COVID-19 pandemic has alarming implications for collective and individual health and social and emotional functioning (Pfefferbaum and North, 2020). The COVID-19-related confinement and stay-at-home orders issued by governments resulted in the largest enforced isolation period in human history (Fancourt et al., 2021). Over the past year, there has been an outpouring of studies reporting the mental health status of people who contracted the disease in the general population or in a specific population such as health care workers (Vindegaard and Benros, 2020). One review of 23 studies only 7 of which reported data from pre-pandemic time points found an increase in mental health problems in the general population from pre-pandemic assessments through the first lockdown phase (Richter et al., 2021).
The long-term effects of lockdown measures may, however, vary with the local characteristics of the epidemic and the public health response. Besides, because some individuals may be more vulnerable than others (Pfefferbaum and North, 2020), the average temporal trend of mental health for the whole population could cover up some discriminate trajectories. Notably, few studies have reported the different trajectories of mental health status across distinct lockdown phases (Batterham et al., 2021; Bu et al., 2020; Herle et al., 2021; Pierce et al., 2021; Saunders et al., 2021; Shevlin et al., 2021; Tan et al., 2020). For example, the ‘UCL COVID-19 Social Study’ (Fancourt et al., 2021) observed with latent growth modeling the highest levels of depression and anxiety symptoms at the early stages of lockdown, with a strong decline thereafter. Further, socially-supportive coping was associated with a faster decrease in anxiety and depressive symptoms (Fluharty et al., 2021). The same research group also identified four trajectory classes of perceived loneliness during the early period of the pandemic (23/03/2020–10/05/2020), with 51.7% of the sample who experienced a relatively stable and high level of loneliness (Bu et al., 2020). Another study based on the ‘Understanding Society, the UK Household Longitudinal Study (UKHLS)’ study identified five distinct mental health trajectories across the first 6 months of the pandemic in 19,763 adults, 11.1% of whom were characterized by poor mental health throughout the observation period, and most participants had either consistently good (39.3%) or consistently very good (37.5%) mental health (Pierce et al., 2021). Among 1296 Australian adults, three and four distinct trajectories for depression and anxiety symptoms were respectively identified from the beginning of COVID-19-related restrictions in late March 2020 to mid-June 2020, with 9.0% of participants showing initially severe and then declining depressive symptoms and 7.8% presenting initially mild and then increasing anxiety symptoms (Batterham et al., 2021). Only one study analyzed whether adverse trajectories were associated with the experience of COVID-19 diagnosis or testing (Pierce et al., 2021). No attempt was made to describe the evolution of the perception of physical health over the period.
France experienced its first and second COVID-19 lockdowns from 17 March 2020 to 11 May 2020 and from 30 October 2020 to 15 December 2020, respectively, in a bid to stem the coronavirus pandemic and its resurgence. Several research teams undertook to monitor the mental health of the population from the first lockdown. For instance, cross-sectional surveys conducted during the first lockdown showed that the prevalence of symptoms of emotional difficulties and hyperactivity/inattention among French children were 7.1% and 24.7%, respectively (Castro et al., 2021); the prevalence of high levels of anxiety, severe depression, severe distress and suicidal thoughts among 69,054 French university students were 27.5%, 16.1%, 22.4% and 11.4%, respectively (Wathelet et al., 2020); and 19.1% of French adults met the diagnostic criteria of clinical insomnia (Kokou-Kpolou et al., 2020). Repeated measures studies found that in the French general population the prevalence of sleep problems significantly decreased during the last weeks of lockdown (Beck et al., 2021), and that the proportion of individuals reporting trouble sleeping (Edjolo et al., 2020) and anxiety symptoms (Ramiz et al., 2021) increased from pre-lockdown to the first lockdown (Ramiz et al., 2021). One survey conducted during the last four days of the first lockdown reported that 12.2% of adults perceived a need for psychological support (Alleaume et al., 2021). Large public support for the national lockdown was fragile in France and was first a critical consensus anchored in current controversies and recent social struggles; second, it was weaker among individuals with a low socioeconomic status, especially since lockdown exacerbated pre-existing social inequalities (Peretti-Watel et al., 2020).
However, it is difficult to quantify and characterize the population that suffered over time because of the scarcity of cohort follow-ups with detailed data including the pre-epidemic period. We took advantage of the existence of a cohort set up before the pandemic to conduct a study of the evolution of mental and physical health levels among the French population over the two lockdowns. The aims of this study were to identify the potential distinct trajectories of physical and mental health outcomes across the two COVID-19 lockdown periods in France and to explore the sociodemographic characteristics profiles of participants of those different classes of trajectories.
2. Methods
2.1. Study design and data collection
This study is based on the ‘MAVIE’ project, which is a web-based cohort established in 2014 for the surveillance and study of HLIs (Home, Leisure and Sports Injuries) among the French population (including those from overseas territories) and has been described in detail previously (Castro et al., 2021; Ramiz et al., 2021). Cohort management was entirely online, including invitations, registration, and data collection. The largest share of participants was recruited through email invitations sent by three mutual insurance companies (MAAF, MACIF and MAIF) to their insurees. A smaller proportion of the participants were informed of the MAVIE cohort and invited to participate through press releases, social media, posters, and flyers (Castro et al., 2021).
Individuals meeting the following criteria were included in this cohort: 1) residing in France; 2) being able to understand and answer the questionnaires in French; 3) having access to and being able to use the internet. A specific questionnaire was designed and proposed to all active volunteers in the cohort to collect information concerning their living conditions and health (the “lockdown questionnaire”). We invited by email the 9598 participants recruited between November 2014 and December 2019 (baseline pre-pandemic data) to participate in this study with an online questionnaire proposed on April 2020 (during the first lockdown) (Ramiz et al., 2021) and October 2020 (during the second lockdown). A total of 1237 and 1161 volunteers completed the questionnaire, respectively. Data from the pre-pandemic period, the first and the second lockdown were available for 613 adult participants.
2.2. Assessment
The following information was collected and analyzed.
2.2.1. Socio-demographic characteristics
Socio-demographic characteristics at pre-lockdown analyzed in the present study included: age, sex, marital status, highest educational degree obtained, place of residence, frequency of alcohol use and tobacco consumption.
2.2.2. Pandemic- and lockdown-related characteristics
Information with regard to living status during the first lockdown including outdoor space (yes/no) and living area (30 m2 or less/more than 30 m2) were collected. Participants were asked whether they, or a family member, or close friends or acquaintances had been affected by COVID-19. The time spent seeking epidemic information on traditional media (television, radio, and printed press), websites and social media was also collected. We further created new variables (‘clinical diagnosis or positive COVID-19 test (the participants, family members, friends or acquaintances)’ during the first lockdown and during the second lockdown) in logistic or multinomial models to indicate whether or not the participant, family members, their friends or acquaintances were diagnosed with or tested positive for COVID-19.
2.2.3. Health outcomes of interest
2.2.3.1. Anxiety symptoms
We used the validated 7-item Generalized Anxiety Disorder Scale (GAD-7) (Cronbach's α: 0.888) to assess the anxiety symptoms experienced during the last two weeks (Löwe et al., 2008; Spitzer et al., 2006). Response options for each item ranged from “not at all” (0) to “nearly every day” (3). The total score ranges from 0 to 21, and higher scores indicate more severe clinical impairment. In our study, those who had a score of 10 or greater were considered to have moderate or severe anxiety symptoms, i.e., possible anxiety (Spitzer et al., 2006).
2.2.3.2. Depressive symptoms
Depression symptoms were collected using the Patient Health Questionnaire-9 (PHQ-9) (Kocalevent et al., 2013; Kroenke et al., 2001). Participants indicated how often they had been bothered by each symptom over the past two weeks using a four-point Likert scale ranging from 0 (Not at all) to 3 (Nearly every day), summing up to an overall score that ranges from 0 to 27. Those who had a score of 10 or greater were considered to have moderate or severe depression symptoms (possible depression) (Kroenke et al., 2001).
2.2.3.3. Self-perceived mental and physical health
Self-perceived mental health and self-perceived physical health over the past week were assessed separately using a visual analogue scale (1 = Poor health, 10 = Excellent health).
2.3. Statistical analyses
The normality of continuous variables was tested using the Shapiro-Wilk test. Univariate analyses were performed using the Chi-square test, Mann-Whitney U test or Kruskal–Wallis test when applicable.
Latent class mixed models offer a way of incorporating additional heterogeneity which can be used to uncover distinct subpopulations (McCulloch et al., 2002; Muthén and Asparouhov, 2008). The latent class mixed models (LCMM) were fitted using the R ‘lcmm’ package (Proust-Lima et al., 2015) to identify distinct classes of individuals sharing similar trajectories of health markers of interest across the three time points: pre-lockdown, first and second lockdowns. This was done separately for the four scores describing anxiety symptoms, depression symptoms, self-perceived mental health and self-perceived physical health. We estimated successive models with an increasing number of latent classes (G) for each health marker starting with a one-class solution with a quadratic term for time. The initial values for models with more than 1 class were drawn from the asymptotic distribution of the estimates of the 1-class model; as recommended, a gridsearch function was used to run an automatic grid search (Proust-Lima et al., 2015) with a maximum of 50 iterations from 100 random vectors of initial values. The final models were selected considering goodness of fit indices of models including lowest Bayesian information criteria (BIC) and higher posterior probabilities of class membership, but also the visual figures, clinical relevance and interpretability. In our study, the maximum number of classes introduced in the models was 6. The posterior probabilities of class membership in each latent class were computed; the closer the mean value is to 1, the more discriminating the model is, and the less ambiguous the individual classifications are (Proust-Lima et al., 2015; Proust-Lima et al., 2014). To further characterize the trajectories, we described socio-demographic and lockdown-related characteristics of health outcomes of interest in each identified class. We reported the latent class mixed model in line with the Guidelines for Reporting on Latent Trajectory Studies (GRoLTS) (Van De Schoot et al., 2017).
In order to explore the associations between socio-demographic, pandemic- and lockdown-related characteristics and class-specific trajectories of each health outcome, we used logistic regression models or the “nnet” R package (Venables and Ripley, 2002) to fit multinomial regression models. In each model, the class-specific trajectory of each health outcome was set as the dependent variable. The following variables were introduced in the model: age group, sex, marital status, education, place of residence, alcohol use, tobacco consumption, outdoor space and living area during the first lockdown and clinical diagnosis or positive COVID-19 test (for the participants, family members, friends or acquaintances) during the first and second lockdowns. Note that COVID-19 clinical diagnosis or testing was restricted to the participant him/herself when assessing factors of self-perceived physical health. The adjusted odds ratio (OR) and 95% confidence interval (95% CI) were used to express the potential correlations. Missing values were handled by employing multiple imputation by chained equations (the “mice” R package) to generate 50 imputed datasets (van Buuren and Groothuis-Oudshoorn, 2010). We performed data analyses using R version 3.6.3 (R Core Team, 2020) via RStudio software (RStudio Team, 2020) with a significant level of 0.05 (two-tailed).
2.4. Ethics statement and confidentiality
The French Data Protection Authority (CNIL) approved the protocol of the MAVIE project (No. 912292). Identifying data were stored on servers at a different location from those hosting the main database. All adult participants provided electronic informed consent. Child participants took part under the responsibility and with the consent of a legal guardian.
3. Results
3.1. Basic descriptions
There were 613 adult participants with data in all three phases (pre-lockdown, the first and second lockdowns), the mean age was 58.1 years (SD = 12.1) and 309 (50.4%) of them were female. There were 403 (65.7%) in a couple relationship (marriage, civil union or cohabitation with a spouse/partner), 66.1% (n = 405) of the participants had a monthly household income of 2500 euros or more and nearly 20% (n = 121) were living in rural areas (fewer than 5000 inhabitants).
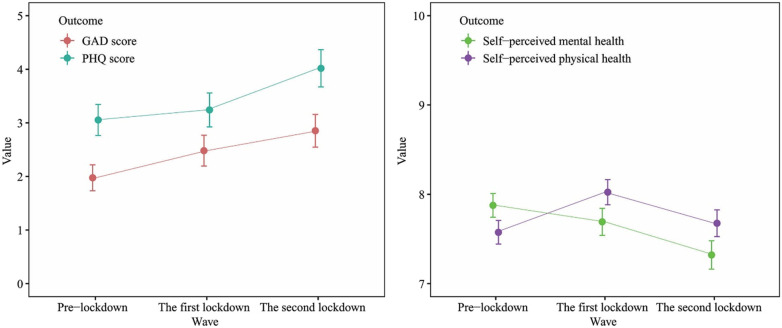
Descriptions of health outcomes of interest pre-lockdown and during the first and second lockdowns and pandemic- and lockdown-related characteristics are shown in Table 1 . Both anxiety and depressive scores increased over these periods: the mean GAD-7 scores were 1.96, 2.37 and 2.82 pre-lockdown, and during the first and second lockdowns, respectively; the corresponding figures for mean PHQ-9 scores were 3.12, 3.36 and 3.95, respectively (Fig. 1 ). The average self-perceived mental health status also worsened over time. The mean self-perceived physical health score improved from pre-lockdown to the first lockdown period and then decreased at the second lockdown (Fig. 1). The reported average time spent obtaining epidemic information halved from the first to the second lockdown. This was the case for traditional media (1.47 vs. 0.86 h/day), websites (0.59 vs. 0.32 h/day) and social media (0.82 vs. 0.60 h/day).
Table 1.
Descriptions of health outcomes of interest and lockdown-related characteristics.
| Variables | Pre-lockdown |
1st lockdown |
2nd lockdown |
P |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| GAD-7 score (n = 469) | 1.96 (2.87) | 2.37 (3.47) | 2.82 (3.60) | <0.001a |
| PHQ-9 score (n = 462) | 3.12 (3.47) | 3.36 (3.83) | 3.95 (4.12) | 0.005a |
| Self-perceived physical health (1−10) (n = 535) | 7.56 (1.64) | 8.06 (1.72) | 7.67 (1.85) | <0.001a |
| Self-perceived mental health (1–10) (n = 530) | 7.88 (1.63) | 7.74 (1.86) | 7.33 (1.94) | <0.001a |
| Time spent seeking epidemic information (in hours/day) | ||||
| Traditional media (n = 541) | – | 1.47 (1.53) | 0.86 (1.27) | <0.001b |
| Websites (n = 540) | – | 0.59 (0.93) | 0.32 (0.53) | <0.001b |
| Social media (n = 545) | – | 0.82 (1.12) | 0.60 (0.93) | <0.001b |
| N (%) | N (%) | N (%) | ||
| Anxiety symptoms (n = 469) | 0.168c | |||
| No | 454 (96.8) | 447 (95.3) | 442 (94.2) | |
| Yes (GAD score ≥ 10) | 15 (3.2) | 22 (4.7) | 27 (5.8) | |
| Depressive symptoms (n = 462) | 0.024c | |||
| No | 436 (94.4) | 428 (92.6) | 414 (89.6) | |
| Yes (PHQ score ≥ 10) | 26 (5.6) | 34 (7.4) | 48 (10.4) | |
| Clinical diagnosis or positive COVID-19 test (multiple-choice question) | ||||
| The participant (n = 613) | – | 7 (1.1) | 23 (3.8) | 0.006c |
| Family members (n = 613) | – | 56 (9.1) | 141 (23.0) | <0.001c |
| Close friends (n = 613) | – | 28 (4.6) | 61 (10.0) | <0.001c |
| Acquaintances (n = 613) | – | 74 (12.1) | 122 (19.9) | <0.001c |
GAD-7: Generalized Anxiety Disorder Scale-7; PHQ-9: Patient Health Questionnaire-9; SD: Standard deviation.
Kruskal–Wallis test.
Mann-Whitney U test.
Chi-square test.
Fig. 1.
Plots of health outcomes of interest before and during the first and second lockdowns (mean, 95% CI).
3.2. Health outcomes trajectories
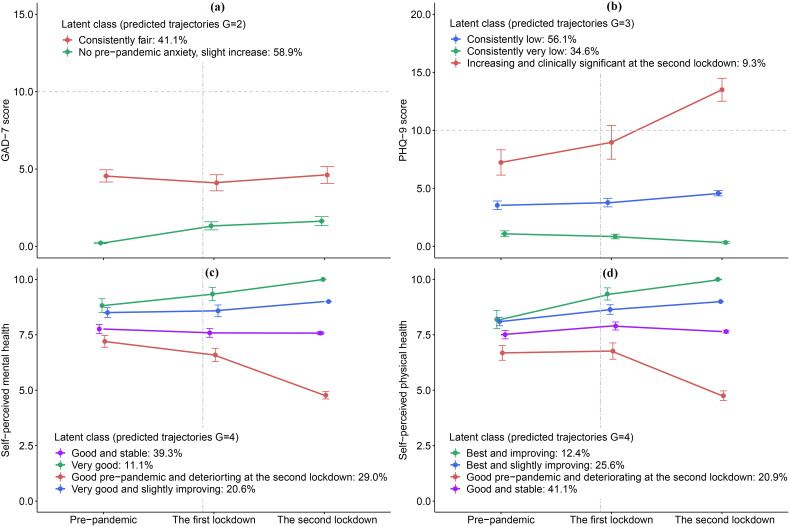
We fitted LCMM models with up to six latent classes (see supplemental Table 1 for the goodness of fit indices and supplemental Figs. 1–4), and selected the 2-class model as the optimal solution for GAD score, the 3-class for PHQ score and the 4-class models for self-perceived mental health and physical health scores. Fig. 2 shows the identified class-specific trajectories of the observed scores for the four health outcomes. Most of the proportions of subjects classified in each latent class in all models with a posterior probability above 0.7 were >80% (supplemental Table 1).
Fig. 2.
Observed average GAD-7 score (a), PHQ-9 score (b), self-perceived mental health (c) and self-perceived physical health (d) status from different class-specific trajectories over time among the French population.
Note: Error bars represent 95% CIs.
Dashed line: The corresponding clinical significance level. Two-dash line: COVID-19 being declared a pandemic.
Anxiety symptoms
As regard to the anxiety score (Fig. 2a), the first class accounted for 58.9% of the total participants with a very good pre-lockdown level (no pre-pandemic anxiety) and a slight increase over time (the ‘no pre-pandemic anxiety, slight increase’ trajectory). The second class included 41.1% of the participants with a ‘consistently fair’ trajectory.
Depressive symptoms
Of the total participants, 34.6% belonged to the ‘consistently very low’ depressive score class (Fig. 2b). The ‘consistently low’ class included 56.1% of the participants, with slightly greater depressive scores than those of the first class. A proportion of 9.3% of the participants followed a trajectory with ‘increasing and clinically significant depressive symptoms (PHQ-9 score ≥ 10) with a slight increase from pre-lockdown to the first lockdown and a sharp increase from the first lockdown to the second lockdown.
Self-perceived mental health
A proportion of 11.1% of the participants belonged to the ‘very good’ self-perceived mental health class, with a very good initial status, and a slight increase over time (Fig. 2c). There were 20.6% following a ‘very good and slightly improving’ trajectory, with a very good pre-lockdown status, then a slight improvement from the first lockdown to the second. A class of 39.3% of the participants showed a ‘good and stable’ trajectory. Besides, 29.0% of the participants had a good pre-pandemic status, then a slight deterioration from pre-pandemic to the first lockdown and then a sharp deterioration from the first lockdown to the second (the ‘good pre-pandemic and deteriorating at the second lockdown’ trajectory class).
Self-perceived physical health
A proportion of 12.4% of the participants belonged to the ‘best and improving’ trajectory with the best initial status and improving (Fig. 2d). There were 25.6% with a ‘best and slightly improving’ trajectory, with a lower improving rate than observed in the first class. Individuals in a ‘good and stable’ trajectory class accounted for 41.1% of all participants and there were 20.9% participants presenting a good pre-pandemic status, then a sharp deterioration from the first lockdown to the second (the ‘good pre-pandemic and deteriorating at the second lockdown’ trajectory class).
3.3. Participant profiles in distinct trajectory classes
Logistic and multinomial regression models were fitted to examine factors associated with belonging to distinct trajectory classes.
The associations between background and pandemic-related characteristics and belonging to each latent class for anxiety score are shown in Table 2 . Participants aged 23–49 years (OR = 2.25, 95% CI: 1.26–4.04) and female participants (OR = 1.76, 95% CI: 1.19–2.60) were more likely to belong to the ‘consistently fair’ class than in the ‘no pre-pandemic anxiety, slight increase’ class.
Table 2.
Associations between basic and pandemic-related characteristics and being in latent classes for anxiety symptoms.
| Variables | Overall (n = 609)a |
No pre-pandemic anxiety, slight increase^ (n = 359, 58.9%) |
Consistently fair (n = 250, 41.1%) |
|
|---|---|---|---|---|
| n (%) | n (%) | n (%) | OR (95% CI) | |
| Age group (years) | ||||
| 50–69 | 315 (51.7) | 192 (53.5) | 123 (49.2) | - |
| 23–49 | 90 (14.8) | 33 (9.2) | 57 (22.8) | 2.25 (1.26–4.04)⁎⁎ |
| 70 and over | 204 (33.5) | 134 (37.3) | 70 (28.0) | 0.88 (0.57–1.32) |
| Sex | ||||
| Male | 303 (49.8) | 206 (57.4) | 97 (38.8) | - |
| Female | 306 (50.2) | 153 (42.6) | 153 (61.2) | 1.76 (1.19–2.60)⁎⁎ |
| Marital status | ||||
| As a coupleb | 402 (66.0) | 240 (66.9) | 162 (64.8) | - |
| Other | 207 (34.0) | 119 (33.1) | 88 (35.2) | 0.77 (0.50–1.19) |
| Education | ||||
| Diploma level BAC+ 3 or higher | 293 (48.1) | 173 (48.2) | 120 (48.0) | - |
| General baccalaureate or diploma level BAC + 2 | 166 (27.3) | 90 (25.1) | 76 (30.4) | 1.31 (0.85–2.01) |
| Less than general baccalaureate | 138 (22.7) | 90 (25.1) | 48 (19.2) | 0.94 (0.58–1.51) |
| Place of residence | ||||
| Rural area (fewer than 5000 inhabitants) | 121 (19.9) | 72 (20.1) | 49 (19.6) | - |
| Municipality inhabitants: 5000–30,000 | 261 (42.9) | 157 (43.7) | 104 (41.6) | 0.84 (0.52–1.36) |
| Municipality inhabitants: ≥30,000 | 211 (34.6) | 122 (34.0) | 89 (35.6) | 0.91 (0.54–1.54) |
| Alcohol use | ||||
| Once a month or less | 127 (20.9) | 70 (19.5) | 57 (22.8) | - |
| More than once a month | 453 (74.4) | 273 (76.0) | 180 (72.0) | 0.96 (0.62–1.50) |
| Tobacco consumption | ||||
| Ex- or non-smoker | 516 (84.7) | 308 (85.8) | 208 (83.2) | - |
| Current smoker | 63 (10.3) | 35 (9.7) | 28 (11.2) | 1.07 (0.59–1.92) |
| Having outdoor space during the 1st lockdown | ||||
| No | 69 (11.3) | 34 (9.5) | 35 (14.0) | - |
| Yes | 521 (85.6) | 314 (87.5) | 207 (82.8) | 0.76 (0.41–1.40) |
| Personal living space during the 1st lockdown | ||||
| >30 m2 | 514 (84.4) | 316 (88.0) | 198 (79.2) | - |
| 30 m2 or less | 73 (12.0) | 30 (8.4) | 43 (17.2) | 1.29 (0.70–2.37) |
| Clinical diagnosis or positive COVID-19 test during the 1st lockdownc | ||||
| No | 475 (78.0) | 286 (79.7) | 189 (75.6) | - |
| Yes | 134 (22.0) | 73 (20.3) | 61 (24.4) | 1.16 (0.75–1.79) |
| Clinical diagnosis or positive COVID-19 test during the 2nd lockdownc | ||||
| No | 350 (57.5) | 216 (60.2) | 134 (53.6) | - |
| Yes | 259 (42.5) | 143 (39.8) | 116 (46.4) | 1.27 (0.87–1.85) |
Bold value: <0.05. **: P<0.01. ^: reference group. -: reference group.
Note: Missing values were handled using multiple imputation.
There were 4 participants with missing values concerning GAD at all three waves.
Marriage, civil partnership or cohabitation with a spouse/partner.
Clinical diagnosis or positive COVID-19 test for the participants, family members, friends or acquaintances.
Table 3 displays the associations between basic and pandemic-related characteristics and latent classes for depressive score. Being female (OR = 3.68, 95% CI: 1.77–7.67) and participants with clinical diagnosis or positive COVID-19 test for the participants, their family members, friends or acquaintances during the first lockdown (OR = 2.72, 95% CI: 1.32–5.60) were more likely to belong to the ‘increasing and clinically significant at the second lockdown’ trajectory.
Table 3.
Associations between basic and pandemic-related characteristics and being in latent classes for depressive symptoms.
| Variables | Overall (n = 612)a |
Consistently very low^ (n = 212, 34.6%) |
Consistently low (n = 343, 56.1%) |
Increasing and clinically significant at the second lockdown (n = 57, 9.3%) |
||
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | |
| Age group (years) | ||||||
| 50–69 | 316 (51.6) | 116 (54.7) | 170 (49.6) | - | 30 (52.6) | - |
| 23–49 | 91 (14.9) | 19 (9.0) | 61 (17.8) | 1.74 (0.89–3.43) | 11 (19.3) | 1.84 (0.67–5.01) |
| 70 and over | 205 (33.5) | 77 (36.3) | 112 (32.7) | 1.11 (0.73–1.69) | 16 (28.1) | 1.09 (0.51–2.32) |
| Sex | ||||||
| Male | 304 (49.7) | 142 (67.0) | 143 (41.7) | - | 19 (33.3) | - |
| Female | 308 (50.3) | 70 (33.0) | 200 (58.3) | 2.68 (1.75–4.10)⁎⁎⁎ | 38 (66.7) | 3.68 (1.77–7.67)⁎⁎⁎ |
| Marital status | ||||||
| As a coupleb | 403 (65.8) | 154 (72.6) | 215 (62.7) | - | 34 (59.6) | - |
| Other | 209 (34.2) | 58 (27.4) | 128 (37.3) | 1.14 (0.71–1.83) | 23 (40.4) | 1.16 (0.54–2.48) |
| Education | ||||||
| Diploma level BAC+ 3 or higher | 295 (48.2) | 102 (48.1) | 164 (47.8) | - | 29 (50.9) | - |
| General baccalaureate or diploma level BAC + 2 | 166 (27.1) | 52 (24.5) | 100 (29.2) | 1.30 (0.82–2.07) | 14 (24.6) | 0.88 (0.39–1.95) |
| Less than general baccalaureate | 138 (22.5) | 53 (25.0) | 71 (20.7) | 1.17 (0.72–1.90) | 14 (24.6) | 1.04 (0.44–2.47) |
| Place of residence | ||||||
| Rural area (fewer than 5000 inhabitants) | 121 (19.8) | 39 (18.4) | 69 (20.1) | – | 13 (22.8) | - |
| Municipality inhabitants: 5000–30,000 | 263 (43.0) | 101 (47.6) | 141 (41.1) | 0.67 (0.40–1.12) | 21 (36.8) | 0.49 (0.20–1.17) |
| Municipality inhabitants: ≥30,000 | 212 (34.6) | 68 (32.1) | 122 (35.6) | 0.80 (0.45–1.39) | 22 (38.6) | 0.78 (0.31–1.93) |
| Alcohol use | ||||||
| Once a month or less | 127 (20.8) | 44 (20.8) | 65 (19.0) | - | 18 (31.6) | - |
| More than once a month | 455 (74.3) | 157 (74.1) | 262 (76.4) | 1.59 (0.98–2.58) | 36 (63.2) | 0.90 (0.43–1.89) |
| Tobacco consumption | ||||||
| Ex- or non-smoker | 518 (84.6) | 183 (86.3) | 287 (83.7) | - | 48 (84.2) | - |
| Current smoker | 63 (10.3) | 18 (8.5) | 39 (11.4) | 1.16 (0.61–2.20) | 6 (10.5) | 0.90 (0.30–2.72) |
| Having outdoor space during the 1st lockdown | ||||||
| No | 69 (11.3) | 19 (9.0) | 43 (12.5) | - | 7 (12.3) | - |
| Yes | 523 (85.5) | 187 (88.2) | 287 (83.7) | 0.92 (0.47–1.80) | 49 (86.0) | 1.64 (0.51–5.29) |
| Personal living space during the 1st lockdown | ||||||
| >30 m2 | 73 (11.9) | 187 (88.2) | 282 (82.2) | - | 47 (82.5) | - |
| 30 m2 or less | 516 (84.3) | 19 (9.0) | 46 (13.4) | 1.34 (0.68–2.66) | 8 (14.0) | 1.08 (0.35–3.28) |
| Clinical diagnosis or positive COVID-19 test during the 1st lockdownc | ||||||
| No | 477 (77.9) | 177 (83.5) | 265 (77.3) | - | 35 (61.4) | - |
| Yes | 135 (22.1) | 35 (16.5) | 78 (22.7) | 1.35 (0.83–2.20) | 22 (38.6) | 2.72 (1.32–5.60)⁎⁎ |
| Clinical diagnosis or positive COVID-19 test during the 2nd lockdownc | ||||||
| No | 353 (57.7) | 129 (60.8) | 198 (57.7) | - | 26 (45.6) | - |
| Yes | 259 (42.3) | 83 (39.2) | 145 (42.3) | 1.03 (0.69–1.54) | 31 (54.4) | 1.54 (0.78–3.03) |
Bold value: <0.05. *: P< 0.05. **: P<0.01. ***: P<0.001. ^: Reference group. -: Reference group.
Note: Missing values were handled using multiple imputation.
There was 1 participant with missing values concerning PHQ at all three waves.
Marriage, civil partnership or cohabitation with a spouse/partner.
Clinical diagnosis or positive COVID-19 test for the participants, family members, friends or acquaintances.
Concerning the trajectory classes of self-perceived mental health (Table 4 ), female participants (OR = 4.53, 95% CI: 2.19–9.37) and participants with clinical diagnosis or positive COVID-19 test for the participants, their family members, friends or acquaintances during the first lockdown (OR = 2.49, 95% CI: 1.02–6.12) were more likely to belong to the ‘good pre-pandemic and deteriorating at the second lockdown’ trajectory.
Table 4.
Associations between basic and pandemic-related characteristics and being in latent classes for self-perceived mental health.
| Variables | Overall (n = 613) |
Very good^ (n = 68, 11.1%) |
Very good and slightly improving (n = 126, 20.6%) |
Good and stable (n = 241, 39.3%) |
Good pre-pandemic and deteriorating at the second lockdown (n = 178, 29.0%) |
|||
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | |
| Age group (years) | ||||||||
| 50–69 | 316 (51.5) | 37 (54.4) | 71 (56.3) | - | 118 (49.0) | - | 90 (50.6) | - |
| 23–49 | 92 (15.0) | 6 (8.8) | 16 (12.7) | 1.10 (0.35–3.41) | 42 (17.4) | 1.49 (0.52–4.32) | 28 (15.7) | 1.48 (0.49–4.46) |
| 70 and over | 205 (33.4) | 25 (36.8) | 39 (31.0) | 0.82 (0.41–1.64) | 81 (33.6) | 1.31 (0.70–2.45) | 60 (33.7) | 1.43 (0.73–2.79) |
| Sex | ||||||||
| Male | 304 (49.6) | 51 (75.0) | 76 (60.3) | - | 113 (46.9) | - | 64 (36.0) | - |
| Female | 309 (50.4) | 17 (25.0) | 50 (39.7) | 1.75 (0.83–3.70) | 128 (53.1) | 3.46 (1.72–6.95)⁎⁎⁎ | 114 (64.0) | 4.53 (2.19–9.37)⁎⁎⁎ |
| Marital status | ||||||||
| As a couplea | 403 (65.7) | 49 (72.1) | 79 (62.7) | - | 169 (70.1) | - | 106 (59.6) | - |
| Other | 210 (34.3) | 19 (27.9) | 47 (37.3) | 0.99 (0.46–2.15) | 72 (29.9) | 0.56 (0.27–1.15) | 72 (40.4) | 0.78 (0.37–1.66) |
| Education | ||||||||
| Diploma level BAC+ 3 or higher | 295 (48.1) | 33 (48.5) | 65 (51.6) | - | 113 (46.9) | - | 84 (47.2) | - |
| General baccalaureate or diploma level BAC + 2 | 166 (27.1) | 14 (20.6) | 26 (20.6) | 0.99 (0.43–2.28) | 67 (27.8) | 1.86 (0.88–3.94) | 59 (33.1) | 1.97 (0.90–4.30) |
| Less than general baccalaureate | 138 (22.5) | 21 (30.9) | 31 (24.6) | 1.02 (0.49–2.15) | 54 (22.4) | 1.05 (0.53–2.11) | 32 (18.0) | 0.86 (0.40–1.85) |
| Place of residence | ||||||||
| Municipality inhabitants: ≥30,000 | 212 (34.6) | 15 (22.1) | 39 (31.0) | - | 85 (35.3) | - | 73 (41.0) | - |
| Municipality inhabitants: 5000–30,000 | 264 (43.1) | 32 (47.1) | 66 (52.4) | 0.87 (0.40–1.92) | 96 (39.8) | 0.50 (0.24–1.05) | 70 (39.3) | 0.49 (0.23–1.07) |
| Rural area (<5000 inhabitants) | 121 (19.7) | 21 (30.9) | 18 (14.3) | 0.39 (0.15–0.99)⁎ | 52 (21.6) | 0.54 (0.24–1.23) | 30 (16.9) | 0.35 (0.15–0.85) |
| Alcohol use | ||||||||
| Once a month or less | 127 (20.7) | 16 (23.5) | 27 (21.4) | - | 48 (19.9) | - | 36 (20.2) | - |
| More than once a month | 455 (74.2) | 51 (75.0) | 94 (74.6) | 1.33 (0.62–2.87) | 180 (74.7) | 1.53 (0.75–3.12) | 130 (73.0) | 1.72 (0.81–3.67) |
| Tobacco consumption | ||||||||
| Ex- or non-smoker | 518 (84.5) | 61 (89.7) | 110 (87.3) | - | 203 (84.2) | - | 144 (80.9) | - |
| Current smoker | 63 (10.3) | 6 (8.8) | 11 (8.7) | 1.06 (0.36–3.11) | 24 (10.0) | 0.91 (0.33–2.47) | 22 (12.4) | 1.19 (0.42–3.33) |
| Having outdoor space during the 1st lockdown | ||||||||
| No | 69 (11.3) | 4 (5.9) | 16 (12.7) | - | 22 (9.1) | - | 27 (15.2) | - |
| Yes | 524 (85.5) | 64 (94.1) | 104 (82.5) | 0.68 (0.19–2.44) | 210 (87.1) | 0.86 (0.25–2.98) | 146 (82.0) | 0.67 (0.19–2.33) |
| Personal living space during the 1st lockdown | ||||||||
| >30 m2 | 73 (11.9) | 4 (5.9) | 11 (8.7) | - | 35 (14.5) | - | 23 (12.9) | - |
| 30 m2 or less | 517 (84.3) | 64 (94.1) | 109 (86.5) | 1.01 (0.27–3.77) | 197 (81.7) | 1.91 (0.59–6.17) | 147 (82.6) | 1.60 (0.47–5.48) |
| Clinical diagnosis or positive COVID-19 test during the 1st lockdownb | ||||||||
| No | 478 (78.0) | 61 (89.7) | 96 (76.2) | - | 194 (80.5) | - | 127 (71.3) | - |
| Yes | 135 (22.0) | 7 (10.3) | 30 (23.8) | 2.15 (0.86–5.41) | 47 (19.5) | 1.66 (0.68–4.03) | 51 (28.7) | 2.49 (1.02–6.12)⁎ |
| Clinical diagnosis or positive COVID-19 test during the 2nd lockdownb | ||||||||
| No | 353 (57.6) | 50 (73.5) | 70 (55.6) | - | 138 (57.3) | - | 95 (53.4) | - |
| Yes | 260 (42.4) | 18 (26.5) | 56 (44.4) | 1.75 (0.88–3.49) | 103 (42.7) | 1.69 (0.89–3.24) | 83 (46.6) | 1.83 (0.93–3.60) |
Bold value: <0.05. *: P< 0.05. **: P<0.01. ***: P<0.001. ^: Reference group. -: Reference group.
Note: Missing values were handled using multiple imputation.
Marriage, civil partnership or cohabitation with a spouse/partner.
Clinical diagnosis or positive COVID-19 test for the participants, family members, friends or acquaintances.
For self-perceived physical health (Table 5 ), female individuals (OR = 2.58, 95% CI: 1.29–5.18) had higher odds of presenting a ‘good pre-pandemic and deteriorating at the second lockdown’ trajectory. Individuals who drank more frequently than once a month (OR = 1.97, 95% CI: 1.02–3.80) were more likely to be in the general class, i.e., the ‘good and stable’ class.
Table 5.
Associations between basic and pandemic-related characteristics and being in latent classes for self-perceived physical health.
| Variables | Overall (n = 613) |
Best and improving^ (n = 76, 12.4%) |
Best and slightly improving (n = 157, 25.6%) |
Good and stable (n = 252, 41.1%) |
Good pre-pandemic and deteriorating at the second lockdown (n = 128, 20.9%) |
|||
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | |
| Age group (years) | ||||||||
| 50–69 | 316 (51.5) | 43 (56.6) | 89 (56.7) | - | 125 (49.6) | - | 59 (46.1) | - |
| 23–49 | 92 (15.0) | 9 (11.8) | 16 (10.2) | 1.10 (0.39–3.09) | 44 (17.5) | 1.56 (0.59–4.13) | 23 (18.0) | 1.93 (0.67–5.56) |
| 70 and over | 205 (33.4) | 24 (31.6) | 52 (33.1) | 0.97 (0.50–1.86) | 83 (32.9) | 1.40 (0.76–2.59) | 46 (35.9) | 1.67 (0.84–3.33) |
| Sex | ||||||||
| Male | 304 (49.6) | 49 (64.5) | 86 (54.8) | - | 118 (46.8) | - | 51 (39.8) | - |
| Female | 309 (50.4) | 27 (35.5) | 71 (45.2) | 1.46 (0.75–2.84) | 134 (53.2) | 2.34 (1.25–4.38)⁎⁎ | 77 (60.2) | 2.58 (1.29–5.18)⁎⁎ |
| Marital status | ||||||||
| As a couplea | 403 (65.7) | 51 (67.1) | 97 (61.8) | - | 178 (70.6) | - | 77 (60.2) | - |
| Other | 210 (34.3) | 25 (32.9) | 60 (38.2) | 1.11 (0.55–2.24) | 74 (29.4) | 0.60 (0.31–1.19) | 51 (39.8) | 0.79 (0.38–1.67) |
| Education | ||||||||
| Diploma level BAC+ 3 or higher | 295 (48.1) | 37 (48.7) | 76 (48.4) | - | 119 (47.2) | - | 63 (49.2) | - |
| General baccalaureate or diploma level BAC + 2 | 166 (27.1) | 19 (25.0) | 38 (24.2) | 0.84 (0.40–1.73) | 73 (29.0) | 1.25 (0.64–2.45) | 36 (28.1) | 1.16 (0.55–2.44) |
| Less than general baccalaureate | 138 (22.5) | 19 (25.0) | 37 (23.6) | 1.03 (0.49–2.14) | 56 (22.2) | 1.07 (0.53–2.14) | 26 (20.3) | 0.85 (0.38–1.91) |
| Place of residence | ||||||||
| Municipality inhabitants: ≥30,000 | 212 (34.6) | 22 (28.9) | 50 (31.8) | - | 86 (34.1) | - | 54 (42.2) | - |
| Municipality inhabitants: 5000–30,000 | 264 (43.1) | 33 (43.4) | 73 (46.5) | 0.95 (0.47–1.93) | 114 (45.2) | 0.89 (0.46–1.76) | 44 (34.4) | 0.62 (0.29–1.31) |
| Rural area (<5000 inhabitants) | 121 (19.7) | 19 (25.0) | 28 (17.8) | 0.63 (0.27–1.45) | 47 (18.7) | 0.71 (0.33–1.56) | 27 (21.1) | 0.63 (0.27–1.50) |
| Alcohol use | ||||||||
| Once a month or less | 127 (20.7) | 21 (27.6) | 32 (20.4) | - | 46 (18.3) | - | 28 (21.9) | - |
| More than once a month | 455 (74.2) | 52 (68.4) | 119 (75.8) | 1.55 (0.78–3.09) | 193 (76.6) | 1.97 (1.02–3.80)⁎ | 91 (71.1) | 1.91 (0.91–4.01) |
| Tobacco consumption | ||||||||
| Ex- or non-smoker | 518 (84.5) | 69 (90.8) | 137 (87.3) | - | 212 (84.1) | - | 100 (78.1) | - |
| Current smoker | 63 (10.3) | 4 (5.3) | 13 (8.3) | 1.31 (0.39–4.39) | 27 (10.7) | 1.86 (0.61–5.67) | 19 (14.8) | 2.91 (0.91–9.26) |
| Having outdoor space during the 1st lockdown | ||||||||
| No | 69 (11.3) | 6 (5.9) | 11 (7.0) | - | 30 (11.9) | - | 22 (17.2) | - |
| Yes | 524 (85.5) | 69 (94.1) | 137 (87.3) | 1.06 (0.32–3.51) | 215 (85.3) | 0.51 (0.17–1.53) | 103 (80.5) | 0.44 (0.14–1.41) |
| Personal living space during the 1st lockdown | ||||||||
| >30 m2 | 517 (84.3) | 69 (90.8) | 135 (86.0) | - | 208 (82.5) | - | 105 (82.0) | - |
| 30 m2 or less | 73 (11.9) | 6 (7.9) | 13 (8.3) | 1.13 (0.36–3.58) | 36 (14.3) | 1.47 (0.51–4.23) | 18 (14.1) | 1.37 (0.43–4.34) |
| Clinical diagnosis or positive COVID-19 test (the participants) during the 1st lockdownb | ||||||||
| No | 609 (98.9) | 76 (100) | 155 (98.7) | / | 248 (98.4) | / | 127 (99.2) | / |
| Yes | 7 (1.1) | 0 (0) | 2 (1.3) | / | 4 (1.6) | / | 1 (0.8) | / |
| Clinical diagnosis or positive COVID-19 test (the participants) during the 2nd lockdown | ||||||||
| No | 590 (96.2) | 74 (97.4) | 153 (97.5) | - | 246 (97.6) | - | 117 (91.4) | - |
| Yes | 23 (3.8) | 2 (2.6) | 4 (2.5) | 1.05 (0.18–6.07) | 6 (2.4) | 0.77 (0.14–4.26) | 11 (8.6) | 3.05 (0.59–15.73) |
Bold value: <0.05. *: P< 0.05. **: P<0.01. ***: P<0.001. ^: Reference group. -: Reference group.
Note: Missing values were handled using multiple imputation.
Marriage, civil partnership or cohabitation with a spouse/partner.
This variable was not adjusted in the multinomial regression model.
4. Discussion
Taking advantage of the French MAVIE cohort study, we found that among the French population people spent less time on average seeking epidemic information in different forms during the second lockdown due to the COVID-19 pandemic than during the first lockdown. Average mental health status (anxiety and depressive symptoms, and self-perceived mental health status) deteriorated from pre-lockdown to the first and second lockdowns. Average self-perceived physical health status improved from pre-lockdown to the first lockdown, and returned to a level similar to the pre-lockdown level at the second lockdown (Fig. 1). In addition, we found using latent class mixed models that most individuals exhibited trajectories with a relatively low level of anxiety (58.9%) and depressive symptoms (90.7%), stable and good self-perceived mental health status (71.0%) and physical health status (79.1%). Those who were younger, female, and with clinical diagnosis of or a positive test for COVID-19 were found to be more vulnerable in terms of mental health. Being female was associated with a better pre-pandemic self-perceived physical health, but deterioration during lockdowns.
Excessive media coverage at the beginning of pandemic (Bergeron and Sanchez, 2005) could partly explain why people spent more time on average searching for COVID-19 news during the first lockdown than the second. This study identified that the French population spent less time on average seeking COVID-19 epidemic information in different forms, i.e., traditional media, websites and social media during the second lockdown than during the first, which may potentially be due to growing public awareness of the COVID-19 pandemic and a course of adaptation.
The average anxiety and depressive symptoms deteriorated over time, unlike the anxiety and PTSD symptoms among the Spanish population during lockdown and its de-escalation process which showed a downward trend (González-Sanguino et al., 2021). Our findings also differed from those concerning anxiety and depression levels among British people, both of which declined across the first 20 weeks following the introduction of lockdown (Fancourt et al., 2021). Given the fact that the assessment tools used in the UK study (Fancourt et al., 2021) were the same as those we used, it should, however, be noted that the multiple assessments were distributed at different time points of the two countries' first lockdown rather than in distinct lockdown periods as our study did, and their results were from the fitted model with the latent growth modeling, which may explain the disparities.
Only one other study assessed the trajectory classes of anxiety and depressive symptoms during the pandemic, i.e., a study in Australian adults (Batterham et al., 2021) using the same assessment tools for anxiety (GAD-7) and depressive symptoms (PHQ-9) as in our study. As in Australia, a majority (77.0%) of individuals showed stable and low anxiety symptoms, but participants with other trajectories showed more severe levels of average anxiety symptoms than those in our study. As regard to depressive symptoms, similar proportions (9.8% in Australia vs. 9.3% in France) of individuals belonged to a deteriorating depressive symptoms class. Another study from the UK identified five trajectory classes for mental health (Pierce et al., 2021), which was unlike our results for self-perceived mental health. The different evaluating tools used could partly explain this inconsistency, i.e., Pierce et al. used the General Health Questionnaire (GHQ-12) and we used a single question. In addition, measures and provisions to stem the coronavirus pandemic and the epidemic situation differed among countries and regions, which could partially result in the disparities of mental health status of their citizens.
Most participants showed both superior mental and physical status pre-lockdown and remained stable over the three time points in our study. One study in the UK showed that the differences in mental health at baseline are probably attributable to pre-existing social inequalities, which have been exacerbated over the past decade (Marmot, 2020). Obviously, there were great heterogeneities concerning people's responses to COVID-19 isolation policy. The latent class mixed models helped us to identify people with homogeneous trajectories.
Nations issued different crisis management and policy responses in fighting the COVID-19 pandemic and the mitigation of its impact varied greatly. In France, there was an easing of lockdown between the three nationwide lockdowns. One study among Italian students showed that depressive symptoms worsened during lockdown, compared with before lockdown, but changes vanished quickly as the lockdown was lifted (Meda et al., 2021). Apart from the effects of lockdown itself, a process of adaptation was adopted by some people (Fancourt et al., 2021) over the different phases of the COVID-19 pandemic (including the lockdown and release period). On the other hand, a previous study showed that data on suicides and mental health care utilization indicators did not suggest an increased demand during the first lockdown phase, so the increase in mental health problems could be regarded as general distress and is to be expected during a global health crisis (Richter et al., 2021).
We found that women were more likely to be in the vulnerable trajectories of anxiety symptoms, depressive symptoms, self-perceived mental and physical health. Vulnerability for anxiety symptoms was also observed among the younger adults (23–49 years). This is in line with previous studies indicating that women and younger adults were more likely to have a higher prevalence of mental health problems than their counterparts during COVID-19 lockdown (Niedzwiedz et al., 2021; Pieh et al., 2020; Ramiz et al., 2021; Wathelet et al., 2020). One meta-analysis showed that the general population living in rural areas suffered from more severe anxiety symptoms than those living in urban areas during the COVID-19 pandemic (Wang et al., 2020). In our study we did not find any association of this kind, as indicated previously, and there were spatial variations concerning death rates, i.e., in the 1918–1919 influenza pandemic in which 30–40% higher rates were noted in cities and towns compared with rural areas in England and Wales (Chowell et al., 2008). Potential spatial variations of transmissibility and of death rates in the COVID-19 pandemic may be related to the general population's mental health status, which should be further analyzed.
Suspected or confirmed COVID-19 precipitated a wide range of psychological problems, including a high level of anxiety symptoms, insomnia, depressive symptoms and post-traumatic stress symptoms, poor well-being and even suicidality (Dsouza et al., 2020; Epstein et al., 2020; Mamun and Griffiths, 2020; Vindegaard and Benros, 2020; Wu et al., 2020) that also triggered family members' poor mental health status (Fiorillo and Gorwood, 2020; Ying et al., 2020). This is consistent with the positive association we found between having a clinical diagnosis or positive COVID-19 test (for the participants, family members, friends or acquaintances) during the first lockdown and presenting an ‘increasing and clinically significant at the second lockdown’ anxiety score trajectory. It was also consistent with the British study revealing that confirmed or suspected SARS-CoV-2 infection was associated with a subsequent increase in GHQ-12 score (Pierce et al., 2021). The physical impact of COVID-19 has been reported elsewhere (Evans et al., 2021), while we did not find any significant association between participants' experience of a clinical diagnosis or positive test and a vulnerable physical health trajectory. It should be noted that only 1.1% and 3.8% of our sample reported a clinical diagnosis or positive COVID-19 test during the first and second lockdowns, respectively, and we used a combination of clinical diagnosis or positive COVID-19 test for the participants, family members, friends or acquaintances in the regression models. A sample selection bias could lead to potential estimation bias, which should be further explored in a larger sample. Finally, previous study showed the association between increased alcohol unit consumption and deterioration in physical health (Oldham et al., 2021), and we found that those with more frequent alcohol use had greater odds of not belonging to the best self-perceived physical health trajectory class.
In comparison with most studies that have only explored the associations during one specific lockdown with a cross-sectional design, our longitudinal study extends the existing literature by identifying detailed trajectory classes of mental and physical health before lockdown and during the first and second lockdowns among the French population, as well as vulnerable groups that may require targeted support in future crises.
Among potential limitations of our study, the health outcomes of interest were only assessed once prior to the pandemic, and health status post-lockdown could not be fitted in the model. Second, given the unusual shape of the growth trajectory, it was clear that a linear model was inappropriate. Although the latent class mixed model was adopted, the robustness of these models may be weakened due to the fact that only three time points were available (Diallo et al., 2017). Lastly, the unsatisfactory sample size may have reduced representativeness.
In conclusion, our longitudinal study shows that consumption of COVID-19 epidemic information from the media decreased during the second COVID-19 lockdown among the French population. Although most individuals had a stable and relatively good mental and physical health status from pre-lockdown to the first and second lockdowns, individuals with deteriorating health status should be supported during the pandemic. It is of great importance to find practical approaches to the targeting of vulnerable groups to improve their health status during such a global crisis.
CRediT authorship contribution statement
Neither the manuscript, nor its content, have been published, or not being considered for publication, elsewhere. All co-authors have contributed to the study, read the manuscript and agreed with its content. There is no conflict of interest concerning the authors in conducting this study and preparing the manuscript.
Financial support
The Institut de recherche en santé publique (IReSP) [CONV 067-00187II], the Agence Nationale de Sécurité du Médicament et des Produits de Santé [conv 2014S029], the Université de Bordeaux and the Région Nouvelle Aquitaine as part of the Cassiopée project [conv 2014-1R30504-00003101]. The MAVIE observatory is coordinated by the INSERM U1219-IETO team and Calyxis, pôle d'expertise du risque, with the support of the mutual insurance companies MAIF, MAAF, MACIF and Decathlon.
Ethical standards
The French Data Protection Authority (CNIL) approved the protocol of the MAVIE cohort, declared to the CNIL under the file number 912292. Identifying data (name, surname, and email address) were stored on servers located in a different location from those hosting the main database. Electronic informed consent was collected from all adult participants. The participation of children was done under the responsibility and with the consent of a legal guardian.
Availability of data and materials
More information can be obtained by emailing Dr. Emmanuel Lagarde at emmanuel.lagarde@u-bordeaux.fr.
Conflict of interest
None.
Acknowledgements
We thank all the participants who took part in this study. The authors are grateful for technical support in statistics (the latent class mixed model) from Dr. Chang Chen, Viviane Philipps and Dr. Cécile Proust-Lima.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.04.095.
Appendix A. Supplementary data
Supplementary material
References
- Alleaume C., Verger P., Peretti-Watel P. Psychological support in general population during the COVID-19 lockdown in France: needs and access. PloS one. 2021;16 doi: 10.1371/journal.pone.0251707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batterham P.J., Calear A.L., McCallum S.M., Morse A.R., Banfield M., Farrer L.M., Gulliver A., Cherbuin N., Rodney Harris R.M., Shou Y., Dawel A. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med. J. Aust. 2021;214:462–468. doi: 10.5694/mja2.51043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck F., Leger D., Cortaredona S., Verger P., Peretti-Watel P. Would we recover better sleep at the end of Covid-19? A relative improvement observed at the population level with the end of the lockdown in France. Sleep Med. 2021;78:115–119. doi: 10.1016/j.sleep.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeron S.L., Sanchez A.L. Media effects on students during SARS outbreak. Emerg. Infect. Dis. 2005;11:732–734. doi: 10.3201/eid1105.040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu F., Steptoe A., Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc. Sci. Med. (1982) 2020;265:113521. doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S., Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J. Stat. Softw. 2010;45:1–67. [Google Scholar]
- Castro M.Y.R., Orriols L., Contrand B., Dupuy M., Sztal-Kutas C., Avalos M., Lagarde E. Cohort profile: MAVIE a web-based prospective cohort study of home, leisure, and sports injuries in France. PLoS One. 2021;16 doi: 10.1371/journal.pone.0248162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowell G., Bettencourt L.M., Johnson N., Alonso W.J., Viboud C. The 1918-1919 influenza pandemic in England and Wales: spatial patterns in transmissibility and mortality impact. Proceedings. Biol. Sci. 2008;275:501–509. doi: 10.1098/rspb.2007.1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diallo T.M.O., Morin A.J.S., Lu H. Performance of growth mixture models in the presence of time-varying covariates. Behav. Res. Methods. 2017;49:1951–1965. doi: 10.3758/s13428-016-0823-0. [DOI] [PubMed] [Google Scholar]
- Dsouza D.D., Quadros S., Hyderabadwala Z.J., Mamun M.A. Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edjolo A., Dartigues J.F., Pérès K., Proust-Lima C. Heterogeneous long-term trajectories of dependency in older adults: the PAQUID cohort, a population-based study over 22 years. J. Gerontol. A Biol. Sci. Med. Sci. 2020;75:2396–2403. doi: 10.1093/gerona/glaa057. [DOI] [PubMed] [Google Scholar]
- Epstein D., Andrawis W., Lipsky A.M., Ziad H.A., Matan M. Anxiety and Suicidality in a Hospitalized Patient with COVID-19 Infection. Eur. J. Case Rep. Intern. Med. 2020;7 doi: 10.12890/2020_001651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans R.A., McAuley H., Harrison E.M., Shikotra A., Singapuri A., Sereno M., Elneima O., Docherty A.B., Lone N.I., Leavy O.C., Daines L. MedRxiv; 2021. Physical, Cognitive and Mental Health Impacts of COVID-19 Following Hospitalisation–A Multi-centre Prospective Cohort Study. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63 doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fluharty M., Bu F., Steptoe A., Fancourt D. Coping strategies and mental health trajectories during the first 21 weeks of COVID-19 lockdown in the United Kingdom. Soc. Sci. Med. (1982) 2021;279:113958. doi: 10.1016/j.socscimed.2021.113958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.A., Saiz J., Muñoz M. Mental health consequences of the Covid-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2020.110219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herle M., Smith A.D., Bu F., Steptoe A., Fancourt D. Trajectories of eating behavior during COVID-19 lockdown: longitudinal analyses of 22,374 adults. Clin. Nutr. ESPEN. 2021;42:158–165. doi: 10.1016/j.clnesp.2021.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocalevent R.D., Hinz A., Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2013;35:551–555. doi: 10.1016/j.genhosppsych.2013.04.006. [DOI] [PubMed] [Google Scholar]
- Kokou-Kpolou C.K., Megalakaki O., Laimou D., Kousouri M. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in french population. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., Herzberg P.Y. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care. 2008;46:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Mamun M.A., Griffiths M.D. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. Health equity in England: the marmot review 10 years on. BMJ (Clin. Res. Ed.) 2020;368 doi: 10.1136/bmj.m693. [DOI] [PubMed] [Google Scholar]
- McCulloch C.E., Lin H., Slate E.H., Turnbull B.W. Discovering subpopulation structure with latent class mixed models. Stat. Med. 2002;21:417–429. doi: 10.1002/sim.1027. [DOI] [PubMed] [Google Scholar]
- Meda N., Pardini S., Slongo I., Bodini L., Zordan M.A., Rigobello P., Visioli F., Novara C. Students' mental health problems before, during, and after COVID-19 lockdown in Italy. J. Psychiatr. Res. 2021;134:69–77. doi: 10.1016/j.jpsychires.2020.12.045. [DOI] [PubMed] [Google Scholar]
- Muthén B., Asparouhov T. Longitudinal Data Analysis. 2008. Growth mixture modeling: analysis with non-Gaussian random effects; p. 143165. [Google Scholar]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D., Craig P., Demou E., Leyland A., Pearce A., Thomson R., Whitley E., Katikireddi S.V. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. J. Epidemiol. Community Health. 2021;75:224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldham M., Garnett C., Brown J., Kale D., Shahab L., Herbec A. Characterising the patterns of and factors associated with increased alcohol consumption since COVID-19 in a UK sample. Drug Alcohol Rev. 2021;40:890–899. doi: 10.1111/dar.13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peretti-Watel P., Verger P., Launay O. The french general population's attitudes toward lockdown against COVID-19: a fragile consensus. BMC Public Health. 2020;20:1920. doi: 10.1186/s12889-020-10048-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136 doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., McManus S., Hope H., Hotopf M., Ford T., Hatch S.L., John A., Kontopantelis E., Webb R.T., Wessely S., Abel K.M. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021;8:610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proust-Lima C., Séne M., Taylor J.M., Jacqmin-Gadda H. Joint latent class models for longitudinal and time-to-event data: a review. Stat. Methods Med. Res. 2014;23:74–90. doi: 10.1177/0962280212445839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proust-Lima C., Philipps V., Liquet B. arXiv; 2015. Estimation of Extended Mixed Models Using Latent Classes and Latent Processes: The R Package lcmm. preprint arXiv:1503.00890. [Google Scholar]
- R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2020. https://www.R-project.org
- Ramiz L., Contrand B., Rojas Castro M.Y., Dupuy M., Lu L., Sztal-Kutas C., Lagarde E. A longitudinal study of mental health before and during COVID-19 lockdown in the french population. Glob. Health. 2021;17:29. doi: 10.1186/s12992-021-00682-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter D., Riedel-Heller S., Zürcher S.J. Mental health problems in the general population during and after the first lockdown phase due to the SARS-Cov-2 pandemic: rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021;30 doi: 10.1017/S2045796021000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RStudio Team . RStudio; PBC, Boston, MA: 2020. RStudio: Integrated Development Environment for R.http://www.rstudio.com/ [Google Scholar]
- Saunders R., Buckman J.E.J., Fonagy P., Fancourt D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol. Med. 2021:1–9. doi: 10.1017/S0033291721000957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M., Butter S., McBride O., Murphy J., Gibson-Miller J., Hartman T.K., Levita L., Mason L., Martinez A.P., McKay R., Stocks T.V.A., Bennett K., Hyland P., Bentall R.P. Refuting the myth of a 'tsunami' of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol. Med. 2021:1–9. doi: 10.1017/S0033291721001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tan Y., Lin X., Wu D., Chen H., Jiang Y., He T., Yin J., Tang Y. Different trajectories of panic and the associated factors among unmarried Chinese during the COVID-19 pandemic. Appl. Psychol. Health Well Being. 2020;12:967–982. doi: 10.1111/aphw.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van De Schoot R., Sijbrandij M., Winter S.D., Depaoli S., Vermunt J.K. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct. Equ. Model. Multidiscip. J. 2017;24:451–467. [Google Scholar]
- Venables W.N., Ripley B.D. Fourth edition. Springer; 2002. Modern applied Statistics With S. [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Kala M.P., Jafar T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M., Duhem S., Vaiva G., Baubet T., Habran E., Veerapa E., Debien C., Molenda S., Horn M., Grandgenèvre P., Notredame C.E., D'Hondt F. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C., Hu X., Song J., Yang D., Xu J., Cheng K., Chen D., Zhong M., Jiang J., Xiong W., Lang K., Tao Y., Lin X., Shi G., Lu L., Pan L., Xu L., Zhou X., Song Y., Wei M., Zheng J., Du C. Mental health status and related influencing factors of COVID-19 survivors in Wuhan. China. Clin. Transl. Med. 2020;10 doi: 10.1002/ctm2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying Y., Ruan L., Kong F., Zhu B., Ji Y., Lou Z. Mental health status among family members of health care workers in Ningbo, China, during the coronavirus disease 2019 (COVID-19) outbreak: a cross-sectional study. BMC Psychiatry. 2020;20:379. doi: 10.1186/s12888-020-02784-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
More information can be obtained by emailing Dr. Emmanuel Lagarde at emmanuel.lagarde@u-bordeaux.fr.