Abstract
Background
Severe acute respiratory syndrome coronavirus type 2 infections in pregnancy have been associated with maternal morbidity, admission to intensive care, and adverse perinatal outcomes such as preterm birth, stillbirth, and hypertensive disorders of pregnancy. It is unclear whether medically assisted reproduction additionally affects maternal and neonatal outcomes in women with COVID-19.
Objective
To evaluate the effect of medically assisted reproduction on maternal and neonatal outcomes in women with COVID-19 in pregnancy.
Study Design
A total of 1485 women with COVID-19 registered in the COVID-19 Related Obstetric and Neonatal Outcome Study (a multicentric, prospective, observational cohort study) were included. The maternal and neonatal outcomes in 65 pregnancies achieved with medically assisted reproduction and in 1420 spontaneously conceived pregnancies were compared. We used univariate und multivariate (multinomial) logistic regressions to estimate the (un)adjusted odds ratios and 95% confidence intervals for adverse outcomes.
Results
The incidence of COVID-19-associated adverse outcomes (eg, pneumonia, admission to intensive care, and death) was not different in women after conceptions with COVID-19 than in women after medically assisted reproduction pregnancies. Yet, the risk of obstetrical and neonatal complications was higher in pregnancies achieved through medically assisted reproduction. However, medically assisted reproduction was not the primary risk factor for adverse maternal and neonatal outcomes including pregnancy-related hypertensive disorders, gestational diabetes mellitus, cervical insufficiency, peripartum hemorrhage, cesarean delivery, preterm birth, or admission to neonatal intensive care. Maternal age, multiple pregnancies, nulliparity, body mass index >30 (before pregnancy) and multiple gestation contributed differently to the increased risks of adverse pregnancy outcomes in women with COVID-19 independent of medically assisted reproduction.
Conclusion
Although women with COVID-19 who conceived through fertility treatment experienced a higher incidence of adverse obstetrical and neonatal complications than women with spontaneous conceptions, medically assisted reproduction was not the primary risk factor.
Key words: assisted reproduction, cohort study, COVID-19, fertility treatment, maternal outcomes, neonatal outcomes, pregnancy, preterm birth, SARS-CoV-2 infection
AJOG at a Glance.
Why was the study conducted?
To evaluate the risk of adverse pregnancy outcomes by mode of conception in women with COVID-19.
Key findings
Medically assisted reproduction is not the primary risk factor for adverse maternal and neonatal outcomes in pregnancies with COVID-19.
What does this add to what is known?
Pregnancies with COVID-19 and pregnancies achieved through medically assisted reproduction are at a higher risk of adverse pregnancy outcomes. This study shows that in women with COVID-19, factors other than medically assisted reproduction such as maternal age, multiple pregnancies, body mass index >30, or multiple gestation are the key drivers for adverse maternal and neonatal outcomes.
Introduction
During the COVID-19 pandemic, concerns arose as to whether infection by the SARS-CoV-2 virus adversely affects pregnancy outcomes. Indeed, observational cohort studies report SARS-CoV-2 infections in pregnancy to be associated with severe maternal morbidity and mortality and neonatal complications compared with noninfected individuals.1, 2, 3, 4, 5 Data from the Covid-19-Related Obstetric and Neonatal Outcome Study (CRONOS) registry in Germany, which prospectively enrolls women with confirmed SARS-CoV-2 infection during their pregnancy, suggest a higher risk of preterm birth and stillbirth and confirm a high rate of severe COVID-19, requiring intensive care in these women.6 , 7 This is especially true for pregnant women with comorbidities such as obesity, diabetes mellitus, hypertension, and older women.8, 9, 10, 11 These factors are also often present in women seeking fertility treatment. However, there are limited data on whether the interaction of risk factors and infertility treatment further worsens outcomes in pregnancies with COVID-19.
At the beginning of the pandemic in March 2020, fertility clinics postponed treatments for several weeks to months because of great uncertainty. Centers returned to their regular programs after the introduction of safety measures and the availability of vaccinations. Nevertheless, many patients are still unsure and have a high need for advice about the risks of SARS-CoV-2 infection, especially as pregnancies after fertility treatment are already associated with a significantly higher incidence of adverse obstetrical and neonatal outcomes such as preeclampsia, fetal growth restriction, and preterm birth compared with spontaneous conceptions.12, 13, 14, 15
For better counseling, it is important to know whether COVID-19 specifically affects outcomes in women undergoing fertility treatment more often than in women who conceive after spontaneous conception. Therefore, we evaluated the risk of adverse maternal and neonatal outcomes in SARS-Cov-2 infections by the mode of conception, emphasizing on symptomatic women with COVID-19.
Material and Methods
Study design and setting
CRONOS is a multicentric, prospective, observational study established by the German Society of Perinatal Medicine (DGPM) in April 2020 to rapidly provide data to counsel women with SARS-CoV-2 infection during their pregnancy. Information on the study is available at www.dgpm-online.org and from the German Clinical Trials Register (DRKS00021208); part of the study results have been published recently.7 Ethical approval was obtained for the study (University Hospital Schleswig-Holstein in Kiel, file number D 451/20, and separate for each study side respectively). Women with clinically confirmed SARS-CoV-2 infection were eligible for inclusion.
All German maternity hospitals were invited to participate in the CRONOS registry. By August 24, 2021, obstetricians and neonatologists from 157 German hospitals and from the Kepler University Hospital in Linz, Austria, confirmed to participate. Of these, 115 hospitals actively provided data to CRONOS. These maternity units attended 224,647 deliveries in 2020, accounting for 29.1% of the births in Germany. Participating hospitals were asked to register all women with SARS-CoV-2 infection independent of the time point of infection during pregnancy.
Data capture and study variables
For collecting data, a reporting form was developed using the cloud-based electronic data capture platform of the service provider castoredc.com (Amsterdam, Netherlands). After the patients had given informed consent, information on the demographic characteristics, comorbidities, previous and current pregnancy characteristics, SARS-CoV-2-specific symptoms and treatments, pregnancy- and birth-specific events, and neonatal outcomes were entered by each treating hospital in the data capture platform.7
Cohort
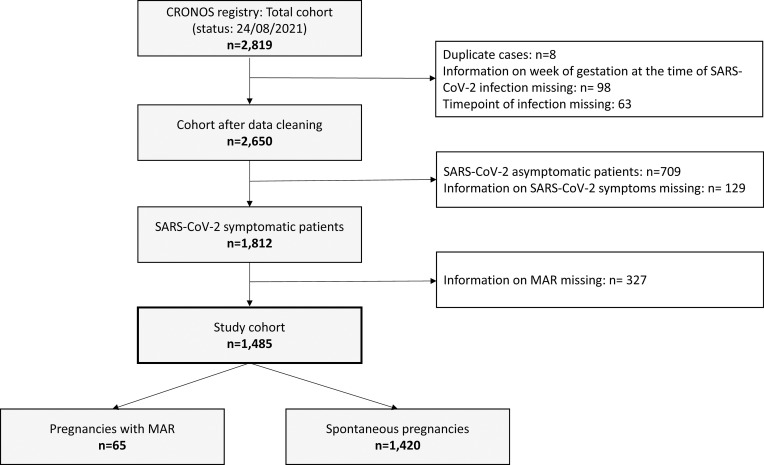
The data presented here were collected between April 3, 2020 and August 24, 2021 by 115 hospitals comprising a total cohort of 2819 cases. During the review of the registry and the plausibility check, duplicate entries were suspected in 10 cases; 8 of the cases were confirmed and excluded after contact with the entering hospital. In 98 cases, the week of gestation at the time of infection remained unknown, and they were excluded, as this was considered mandatory information. In 63 other cases, it remained unclear whether women had been infected during or before their pregnancy; these were also excluded. From the remaining 2,650 women with confirmed SARS-CoV-2 infection during their pregnancy, 1812 (68.3%) were symptomatic, 709 (26.8%) were asymptomatic, and data on symptoms were not provided in 129 (4.9%) cases (Figure ). The final study cohort for the analyses consisted of patients with COVID-19 (symptomatic SARS-CoV-2 infection) with valid information on whether or not medically assisted reproduction (MAR) had been conducted before the present pregnancy (n=1485). Of these, 1331 (89.6%) had a confirmed SARS-CoV-2 infection via a viral RNA detected by polymerase chain reaction testing, 30 (2.0%) via a detection of maternal SARS-CoV-2 antibodies, 45 (3.0%) via an antigen testing, and for 75 cases, (5.1%) no information about the exact diagnostic test of SARS-CoV-2 infection was available.
Figure.
Flowchart of the study cohort
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
Statistical analyses
For evaluating whether pregnancies after fertility treatment involve a greater risk of adverse maternal and neonatal outcomes than spontaneous pregnancies, a stepwise statistical analysis strategy was performed. Firstly, the baseline data were analyzed to identify statistically significant differences in the baseline risks between pregnancy with MAR and spontaneous conceptions (Table 1 ). Secondly, it was evaluated whether COVID-19 associated clinical outcomes (Table 2 ) and maternal and neonatal complications differed in a statistically significant way between MAR pregnancies and spontaneous conceptions (Supplemental Table 1). Thirdly, for those maternal and neonatal outcomes with statistically significant differences between the 2 study groups, separate multivariate models were calculated (Supplemental Tables 2 and 3).
Table 1.
Baseline and pregnancy characteristics of the study participants
| Maternal characteristics | |||
|---|---|---|---|
| MAR pregnancies n=65 | Spontaneous pregnancies n=1420 | P value | |
| Maternal age (y) | 34.09±5.12 | 30.90±5.14 | <0.001 |
| 15–24 | 2 (3.1) | 168 (11.8) | 0.001 |
| 25–34 | 35 (53.8) | 899 (63.3) | |
| 35–49 | 28 (43.1) | 353 (24.9) | |
| Nulliparity | 42/65 (64.6) | 529/1399 (37.8) | <0.001 |
| Smoking (before pregnancy) | 4/63 (6.3) | 107/1398 (7.7) | 0.70 |
| Maternal comorbidities | |||
| BMI >30 (before pregnancy) | 18/63 (28.6) | 275/1324 (20.8) | 0.14 |
| Cardiovascular comorbidities | 3 (4.6) | 53 (3.7) | 0.73a |
| Diabetes mellitus (preexisting) | 1 (1.5) | 18 (1.3) | 0.58a |
| Pulmonary comorbidities | 3 (4.6) | 49 (3.5) | 0.49a |
| Hematologic comorbidities | 2 (3.1) | 16 (1.1) | 0.18a |
| Current pregnancy characteristics | |||
| Multiple gestation | 8/64 (12.5) | 29/1416 (2.0) | <0.001 |
| Gestational age (wk) at onset of COVID-19 symptoms | 27.25±9.56 | 27.60±9.92 | 0.78 |
| First trimester | 8 (12.3) | 188 (13.2) | 0.97 |
| Second trimester | 21 (32.3) | 460 (32.4) | |
| Third trimester | 36 (55.4) | 772 (54.4) | |
The data are presented as mean±standard deviation or absolute or relative frequencies (percentage).
BMI, body mass index; MAR, medically assisted reproduction.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
Fisher exact test.
Table 2.
COVID-19-associated maternal and neonatal outcomes after medically assisted reproduction and spontaneous conceptions
| Outcomes | MAR pregnancies n=65 | Spontaneous pregnancies n=1420 | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Maternal outcomes | |||||
| COVID-19-associated need for inpatient treatmenta | 10/61 (16.4) | 243/1349 (18.0) | 0.89 | 0.45–1.78 | .75 |
| Pneumonia | 6/60 (10.0) | 135/1345 (10.0) | 0.99 | 0.43–2.36 | .99 |
| ICU admission | 2/61 (3.3) | 75/1349 (5.6) | 0.58 | 0.14–2.40 | .45 |
| Mortality | 0/61 (0.0) | 4/1349 (0.3) | n.a. | n.a. | .99 |
| COVID-19-associated indication for cesarean delivery | 2/31 (6.5) | 44/421 (10.5) | 0.59 | 0.14–2.56 | .48 |
| COVID-19-associated reason for pregnancy termination | 2/56 (3.6) | 48/1185 (4.1) | 0.88 | 0.21–3.71 | .86 |
| Delivery necessary for further maternal COVID-19 treatment | 0/56 (0.0) | 32/1185 (2.7) | n.a. | n.a. | .99 |
| Neonatal outcomes | |||||
| Delivery within 4 wk after onset of COVID-19 symptoms | 21/57 (36.8) | 445/1177 (37.9) | 0.96 | 0.55–1.66 | .88 |
| Combined perinatal outcomeb | 9/21 (42.9) | 105/445 (23.6) | 2.43 | 1.00–5.93 | .05 |
| Stillbirth | 0/21 (0.0) | 11/444 (2.5) | n.a. | n.a. | .99 |
| NICU admission | 9/21 (42.9) | 94/440 (21.4) | 2.76 | 1.13–6.75 | .03 |
| Neonatal death | 0/21 (0.0) | 1/428 (0.2) | n.a. | n.a. | .99 |
Data are presented as absolute or relative frequencies (percentage).
CI, confidence interval; ICU, intensive care unit; MAR, medically assisted reproduction; n.a., not applicable; NICU, neonatal intensive care unit; OR, odds ratio.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
The combined endpoint is composed of the following: pneumonia, ICU admission, and mortality
Based on women who delivered within 4 weeks after the onset of COVID-19 symptoms and ≥24 weeks of gestation and is composed of the following endpoints: NICU admission, stillbirth, and neonatal death.
For comparing the categorical variables between pregnancies after MAR and spontaneous conceptions, the absolute and relative frequencies are presented for each group separately. The statistical significance was tested for the categorical baseline variables by using the chi-square tests or Fisher exact tests, and univariate (multinominal) logistic regression models were applied for the categorical maternal and neonatal outcomes. The continuous variables are shown as means and standard deviations for each group. The statistical significance was tested for the continuous baseline variables by using independent t tests and univariate analysis of covariance for continuous maternal and neonatal outcomes.
In addition to P values, risk estimators (odds ratios [OR] or mean difference [MD]) and corresponding 95% confidence intervals (95% Cl) were calculated for a comparison of maternal and neonatal complications. For the calculation of adjusted estimators in multivariate (multinominal) logistic regression models, the baseline variables that significantly differed between both the groups (confounders) or those that are known risk factors for adverse outcomes were included in the models.
Statistical analyses were performed using Statistical Package for Social Sciences (SPSS; version 28; IBM Corp, Armonk, NY) for Windows (Microsoft, Redmond, WA). SPSS, by default, conducts analyses by dropping cases for which there are missing values, so the sample sizes may differ in the statistical analyses. Inferential statistics were used in a descriptive manner. Thus, neither global nor local significance levels were determined, and no adjustment for multiplicity was applied. However, P values <.05 were considered to be statistically significant.
Results
The baseline maternal demographic and clinical characteristics of 1420 (95.6%) women with spontaneous conceptions and those of 65 (4.38%) women with pregnancies achieved after MAR are presented in Table 1. Of all MAR pregnancies, most (n=43; 66.2%) were achieved through assisted reproductive technology (ART) (ie, in vitro fertilization [IVF] or intracytoplasmic sperm injection [ICSI]). Six women (n=9.2%) conceived after ovulation induction (OI) with (n=3) or without (n=3) intrauterine insemination (IUI), and fertility treatment was not further specified in 16 women (24.6%).
Overall, women who conceived through MAR were significantly older and were more likely to be nulliparous or carry multiple pregnancies than those having conceived spontaneously. The gestational age at onset of COVID-19 was comparable between both the groups.
The COVID-19-associated maternal outcomes, for example, need for inpatient treatment, pneumonia, maternal admission to intensive care unit (ICU), and maternal mortality, were not different among MAR and spontaneous conceptions (Table 2). Moreover, the odds of COVID-19- associated cesarean delivery, pregnancy termination, or delivery were comparable between both the conception groups.
Adverse neonatal outcomes following birth within 4 weeks after the onset of COVID-19 resulted primarily from a significantly higher rate of neonatal intensive care unit (NICU) admissions in the MAR group, which is also the main driver behind the borderline significant difference in the combined perinatal outcome (P=.05) (Table 2). This significant difference is mainly driven by the higher number of multiple pregnancies in MAR conceptions, as the adjusted OR for the mode of conception is not significant anymore when it is controlled for multiple gestations (Supplemental Table 3). Although 11 stillbirths (2.5%) and 1 neonatal death (0.2%) occurred in pregnancies after spontaneous conception, no such cases were registered in MAR conceptions.
Other maternal and perinatal outcomes of births following spontaneous conceptions or after MAR independent of the onset of COVID-19 are shown in Supplemental Table 1. Women after MAR were more likely to be diagnosed with gestational diabetes mellitus (odds ratio [OR], 1.97; 95% confidence interval [CI], 1.00–3.86), cervical insufficiency (OR, 4.65; 95% CI, 1.72–12.56) and were more likely to undergo cesarean delivery (OR, 2.19; 95% CI, 1.26–3.82). However, the cesarean delivery rate in multiple pregnancies was comparable between the conception groups (OR, 0.88; 95% CI, 0.16–4.71). Peripartum hemorrhage occurred more often in MAR pregnancies (OR, 3.33; 95% CI, 1.35–8.21). Furthermore, the rate of pregnancy-related hypertensive disorders was higher though not statistically significantly different (OR, 2.39; 95% CI, 0.99–5.75; P=.053). Children from MAR conceptions were delivered preterm (OR, 2.98; 95% CI, 1.66–5.33) and admitted to the NICU (OR, 2.28; 95% CI, 1.25–4.16) more often than those by birth from spontaneous conceptions. Although a rare event, neonatal death occurred proportionally more often in MAR pregnancies (1/57=1.8% vs 3/1,145=0.3%). Neonatal death was not clinically linked to COVID-19 in any of the cases.
The results from multivariate (nominal) logistic regression models for selected maternal and neonatal outcomes are shown in Supplemental Tables 2 and 3. For estimating the adjusted OR for MAR vs that for spontaneous conceptions, the variables of maternal age, nulliparity, and multiple gestation, which significantly differed at baseline between both the groups, were included as a covariate. Because women with a BMI >30 kg/m2 were proportionally more common in the MAR group, and obesity is a known risk factor for adverse outcomes, BMI >30 was also taken into account. However, it was not statistically significant in the study sample. Pregnancy-related hypertensive disorders showed a borderline significant difference. Therefore, a multivariate model was also calculated for this important outcome.
In the context of COVID-19, the multivariate models demonstrate that MAR was not a statistically significant predictor of gestational diabetes mellitus, pregnancy-related hypertensive disorders, cesarean delivery, cervical insufficiency, peripartum hemorrhage, NICU admission, and the combined perinatal outcomes of NICU admission, stillbirth, and neonatal death following delivery within 4 weeks after the onset of COVID-19. However, the risks are still descriptively higher in the MAR group (OR >1). MAR significantly increased the risk of preterm birth (OR, 2.32; 95% CI, 1.19–4.53), yet, multiple gestation was the primary risk factor for preterm birth (OR, 15.92; 95% CI, 6.82–37.16).
All other multivariate analyses demonstrate that risk factors other than MAR are the main drivers for adverse outcomes. Gestational diabetes mellitus is associated with BMI >30 (OR, 3.25; 95% CI, 2.25–4.70); pregnancy-related hypertensive disorders are associated with BMI >30 (OR, 2.37; 95% CI, 1.36–4.13) and nulliparity (OR, 2.74; 95% CI, 1.57–4.77); cesarean delivery is associated with maternal age (OR, 1.04; 95% CI, 1.01–1.06), BMI >30 (OR, 1.80; 95% CI, 1.34–2.43), and nulliparity (OR, 1.46; 95% CI, 1.12–1.91); cervical insufficiency is connected with multiple gestation (OR, 14.46; 95% CI, 5.35–39.09); peripartum hemorrhage is associated with maternal age (OR, 1.07; 95% CI, 1.00–1.13) and multiple gestation (OR, 3.47; 95% CI, 1.11–10.86); NICU admission is connected to maternal age (OR, 1.07; 95% CI, 1.03–1.10) and multiple gestation (OR, 11.38; 95% CI, 5.10–25.37); and finally, the combined perinatal outcome is associated with multiple gestations (OR, 6.14; 95% CI, 1.90–19.91).
Comment
Principal findings
We report that in women with MAR pregnancies, the risk of COVID-19-associated adverse outcomes, for example, the need for inpatient treatment, pneumonia, oxygen ventilation, maternal death, and delivery and also stillbirth and neonatal death following birth within 4 weeks of the onset of COVID-19 was comparable with pregnancies after spontaneous conceptions. MAR was also not the primary risk factor of adverse maternal or neonatal outcomes in pregnancies affected by COVID-19. Instead, other factors, such as maternal age, nulliparity, BMI >30, or multiple gestation were the key drivers. However, MAR conceptions were associated with descriptively higher risks of gestational diabetes mellitus, peripartum hemorrhage, cervical insufficiency, cesarean delivery, preterm birth, and admission to NICU.
Results in the context of what is known
Several cohort studies report an association between COVID-19 in pregnancy and substantially increased maternal and neonatal morbidity and mortality than pregnant women without a diagnosis of COVID-19.10 This involves preeclampsia,3 , 16 , 17 gestational hypertension,18 maternal death,19 stillbirth,19 preterm delivery,17 , 20 and poor fetal growth, among others.18 , 21 The risks are significantly higher in women with comorbidities, eg, diabetes mellitus, hypertension, and obesity; the risks are also higher in older age.8, 9, 10, 11
Insight on the outcomes of pregnancies achieved through MAR and COVID-19 is sparse. The first data were provided by the ESHRE COVID-19 Working Group. It collected 80 cases from 32 countries, including 67 live births, 10 miscarriages, 2 stillbirths, and 1 maternal death.22 One-third of the reported cases had an asymptomatic infection, whereas 31.4% were treated in the hospital. The authors concluded that infections in pregnancies after MAR do not lead to a higher risk of adverse outcomes than those after spontaneous conceptions. This is somehow in line with our results, which demonstrate that the conception mode is not the primary risk factor for adverse obstetrical and neonatal complications in COVID-19-affected women. Particularly encouraging is also the fact that comparable incidences of complications were reported for those directly associated with COVID-19 (eg, pneumonia, ICU admission, and death).
Engels Calvo et al reported a higher incidence of preeclampsia and cesarean delivery in a cohort of symptomatic and asymptomatic SARS-CoV-2-infected women after IVF than with spontaneous pregnancies.23 This is in contrast to our observations for both the outcomes. One main difference in the analysis is the adjustment for important confounders, which included maternal age and clinical presentation in the Spanish study.23 In the cohort, 36 out of 74 women conceived with donor oocytes, which was not a covariate in the multinomial logistic regression model but is one of several well-known risk factors for preeclampsia.24, 25, 26 In addition, the higher rate of cesarean delivery in IVF patients than in spontaneous conceptions can particularly be explained by the increased rate of multiple births in the Spanish study. Our multinominal logistic regression model included the clinical characteristics (eg, age, nulliparity, and multiple gestation), which significantly differed between MAR pregnancies and spontaneous conceptions and also known potential confounders (eg, BMI >30) for the respective outcome. The models developed suggest that the (still) elevated though not statistically significant risk of MAR pregnancies would be further reduced if additional risk factors were considered. In our cohort of spontaneous conceptions, a significant number of stillbirths (2.5%) occurred within 4 weeks of COVID-19 onset, which is higher than the expected stillbirth rate of approximately 0.4% in Germany and requires further attention. None of these cases were present in the MAR group, which may be because of the low number of registered pregnancies on the one hand and the possibly better monitoring and earlier delivery of these high-risk pregnancies per se on the other.
Compared with spontaneous conceptions, adverse maternal and neonatal outcomes are more common among conceptions after MAR independent of the onset of COVID-19 in pregnancy.27 , 28 The main driver for the adverse outcomes is the higher risk of multiple gestations in IVF.29 As the field moves toward single embryo transfer, and as the rate of multiple gestations decreases, it also becomes clear that other factors, eg, the choice of a programmed protocol in frozen-thawed embryo transfer cycles30, 31, 32 or subfertility33 itself make a significant contribution to a higher incidence of adverse outcomes. Subfertile women carry risk factors for pregnancy complications more often, eg, higher age, obesity, or metabolic alterations.12 , 34 , 35 Beside an expected higher rate of multiple gestations, we confirmed these observations in our infertile cohort, which was older and more often obese. The rate of nulliparity, which is a risk factor for hypertensive disorders of pregnancy,36 was also higher. The results from our multivariate models demonstrate that MAR itself is not the primary risk factor for adverse outcomes of pregnancies affected by COVID-19, for example, gestational diabetes mellitus, peripartum hemorrhage, cervical insufficiency, cesarean delivery, preterm birth, and admission to NICU, but that these women enter pregnancy with a higher baseline risk. In this context, maternal age, multiple gestation, and BMI >30 were the main predictors of obstetrical and neonatal complications.
Clinical implications
Our findings are of clinical importance during an ongoing pandemic with a so far unknown end. They will help advise couples seeking fertility treatment and will provide reassurance that the fertility treatment itself will not add to the potential risk of adverse maternal and neonatal outcomes when a patient is affected by COVID-19. Nevertheless, our data clearly show again that other, potentially avoidable, risk factors (eg, multiple gestation) lead to a poorer outcome.
Strengths and limitations
In this study, we took advantage of a well-supervised prospective registry study using a standardized electronic clinical report form. Items specifically targeting MAR were incorporated and linked to COVID-19 and obstetrical and neonatal outcomes. A particular strength of our study is the differentiation between the methods of conception such as IVF or ICSI and OI with or without IUI, which ensures the quality of the data entries. Because asymptomatic cases are most likely considered as “incidental SARS-CoV-2 infection” cases requiring hospitalization for other reasons, we focused our analysis on symptomatic women. In our experience this approach avoids including women who present to the hospital primarily because of obstetrical complications, eg, spontaneous preterm delivery, fetal growth restriction, or preeclampsia.
Our study has a variety of limitations, including a relatively small sample size of MAR pregnancies, and therefore, differing cohort sizes. These factors make it difficult to reliably show statistical correlations. Nevertheless, our cohort reflects the reality in Germany, with approximately 4% of births occurring through MAR. Because of the cohort design as a registry study, no conclusion can be drawn about the actual incidences of complications in COVID-19-affected women in both the conception groups.7 Similarly, owing to the currently low case numbers, no final statement can be made regarding the risk factors for severe maternal courses and neonatal infections. Beside, a comparison to women without COVID-19 is not possible, so the direct impact on outcomes (COVID-19 vs no SARS-CoV-2 infection) cannot be derived.
Conclusion and future directions
COVID-19 during pregnancy after MAR was not associated with a substantially higher risk of COVID-19-associated adverse outcomes. However, maternal and neonatal morbidity was increased compared with outcomes after spontaneous conceptions. The data provide important information for counseling couples who seek fertility treatment and to provide reassurance about the risks that are not primarily driven by MAR but other individual risk factors compared with spontaneous conceptions with COVID-19 during pregnancy. With the growing number of SARS-CoV-2 infections worldwide, further research is needed to confirm our observations and to elucidate the impact of different SARS-CoV-2 variants and of infections after previous immunization on obstetrical and neonatal outcomes.
Acknowledgments
The authors wish to thank all the participating hospitals for providing clinical information to the CRONOS database. This research would not have been possible without their efforts.
Footnotes
The authors declare no conflict of interest.
CRONOS has been funded by Krumme-Stiftung, the German Society of Perinatal Medicine (DGPM), and the Federal State of Schleswig-Holstein
Cite this article as: Ziert Y, Abou-Dakn M, Backes C, et al. Maternal and neonatal outcomes of pregnancies with COVID-19 after medically assisted reproduction: results from the prospective COVID-19-Related Obstetrical and Neonatal Outcome Study. Am J Obstet Gynecol 2022;227:495.e1-11.
Supplementary Data
Maternal and neonatal outcomes of pregnancies with COVID-19 after medically assisted reproduction.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
Maternal and neonatal outcomes of pregnancies with COVID-19 after medically assisted reproduction.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
Appendix
Supplemental Table 1.
Maternal and neonatal outcomes of women with COVID-19 after medically assisted reproduction and spontaneous conceptions
| Outcomes | MAR pregnancies n=65 | Spontaneous pregnancies n=1420 | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Maternal outcomes | |||||
| Gestational diabetes mellitus | 11/65 (16.9) | 133/1420 (9.4) | 1.97 | 1.00–3.86 | .048 |
| Pregnancy-related hypertensive disordersa | 6/65 (9.2) | 58/1419 (4.1) | 2.39 | 0.99–5.75 | .053 |
| Stillbirthb | 1/57 (1.8) | 15/1170 (1.3) | 1.36 | 0.18–10.6 | .76 |
| Early and late miscarriage | 0/57 (0.0) | 13/1190 (0.9) | n.a. | n.a. | .99 |
| Mode of delivery | |||||
| Spontaneous vaginal delivery | 23/57 (40.4) | 694/1189 (58.4) | |||
| Vaginal-operative delivery | 3/57 (5.2) | 69/1189 (5.8) | 1.31 | 0.38–4.48 | .67 |
| Cesarean delivery | 31/57 (54.4) | 426/1189 (35.8) | 2.19 | 1.26–3.82 | .005 |
| Premature labor | 2/65 (3.1) | 67/1419 (4.7) | 0.64 | 0.15–2.67 | .54 |
| Premature rupture of membranes | 9/65 (13.8) | 125/1419 (8.8) | 1.67 | 0.80–3.44 | .17 |
| Cervical insufficiency | 5/65 (7.7) | 25/1419 (1.8) | 4.65 | 1.72–12.56 | .002 |
| Gestational cholestasis | 2/65 (3.1) | 19/1419 (1.3) | 2.34 | 0.53–10.26 | .26 |
| Peripartum hemorrhage | 6/56 (10.7) | 41/1179 (3.5) | 3.33 | 1.35–8.21 | .009 |
| Neonatal outcomes | |||||
| Fetal growth restriction | 0/65 (0.0) | 37/1419 (2.6) | n.a. | n.a. | .99 |
| Gestational age (wk) at birth | 38.21±3.4 | 39.01±3.42 | −0.79c | −1.71 to 0.11 | .09 |
| Preterm birth (<37 gestational wk)b | 18/57 (22.8) | 158/1177 (13.4) | 2.98 | 1.66–5.33 | <.001 |
| Birthweight percentiles | |||||
| <10th percentile | 3/51 (5.9) | 79/1120 (7.1) | 1.24 | 0.38–4.09 | .72 |
| 10th–90th percentiles | 44/51 (86.3) | 932/1120 (83.2) | |||
| >90th percentile | 4/51 (7.8) | 109/1120 (9.7) | 1.29 | 0.45–3.65 | .64 |
| 5 min Apgar | 9.16±1.46 | 9.234±1.73 | −0.08c | −0.53 to 0.38 | .75 |
| 5 min Apgar <7 | 1/57 (1.8) | 52/1172 (4.4) | 0.39 | 0.05–2.83 | .35 |
| Congenital malformations | 3/57 (5.3) | 26/1176 (2.2) | 2.46 | 0.72–8.37 | .15 |
| NICU admission | 16/57 (28.1) | 172/1178 (14.8) | 2.28 | 1.25–4.16 | .007 |
| NICU admission (excluding multiple gestations) | 10/50 (20.0) | 159/1154 (13.8) | 1.21 | 0.57–2.55 | .22 |
| Respiratory support | 9/57 (15.8) | 102/1178 (8.7) | 1.98 | 0.94–4.15 | .07 |
| Neonatal death | 1/57 (1.8) | 3/1145 (0.3) | 6.79 | 0.69–66.39 | .09 |
Data are shown as absolute or relative frequencies (percentage).
CI, confidence interval; HELLP, hemolysis, elevated liver enzymes and low platelets; ICU, intensive care unit; MAR, medically assisted reproduction; n.a., not applicable; NICU, neonatal intensive care unit; OR, odds ratio.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
HELLP + other hypertensive disorders of pregnancy (eg, pregnancy-induced hypertension, preeclampsia)
Based on delivery ≥ 24 weeks of gestation
Mean difference.
Supplemental Table 2.
Multivariate model results for selected maternal outcomes of women with COVID-19 after medically assisted reproduction and spontaneous conceptions
| Outcomes | Level | OR | 95% CI | P value |
|---|---|---|---|---|
| Gestational diabetes mellitus | ||||
| Mode of conception | MAR | 1.71 | 0.82–3.57 | .16 |
| Maternal age (y) | 1.0 | 0.98–1.06 | .32 | |
| Nulliparity | Present | 0.89 | 0.60–1.32 | .55 |
| BMI >30 (before pregnancy) | Present | 3.25 | 2.25–4.70 | <.001 |
| Multiple gestation | Present | 1.27 | 0.46–3.51 | .65 |
| Pregnancy-related hypertensive disordersa | ||||
| Mode of conception | MAR | 1.29 | 0.49–3.42 | .60 |
| Maternal age (y) | 1.04 | 0.99–1.09 | .16 | |
| Nulliparity | Present | 2.74 | 1.57–4.77 | <.001 |
| BMI >30 (before pregnancy) | Present | 2.37 | 1.36–4.13 | .002 |
| Multiple gestation | Present | 2.74 | 0.88–8.47 | .08 |
| Mode of delivery (Spontaneous vaginal delivery [reference]) | ||||
| Vaginal-operative delivery | ||||
| Mode of conception | MAR | 0.93 | 0.26–3.32 | .91 |
| Maternal age (y) | 1.01 | 0.96–1.07 | .62 | |
| Nulliparity | Present | 6.51 | 3.51–12.10 | <.001 |
| BMI >30 (before pregnancy) | Present | 1.29 | 0.66–2.55 | .45 |
| Multiple gestation | Present | n.a. | n.a. | n.a. |
| Cesarean delivery | ||||
| Mode of conception | MAR | 1.66 | 0.93–2.97 | .09 |
| Maternal age (y) | 1.04 | 1.01–1.06 | .004 | |
| Nulliparity | Present | 1.46 | 1.12–1.91 | .005 |
| BMI >30 (before pregnancy) | Present | 1.80 | 1.34–2.43 | <.001 |
| Multiple gestation | Present | 1.78 | 0.85–3.73 | .13 |
| Cervical insufficiency | ||||
| Mode of conception | MAR | 2.86 | 0.89–9.14 | .08 |
| Maternal age (y) | 1.04 | 0.96–1.13 | .33 | |
| Nulliparity | Present | 1.39 | 0.59–3.24 | .45 |
| BMI >30 (before pregnancy) | Present | 0.57 | 0.18–1.76 | .32 |
| Multiple gestation | Present | 14.46 | 5.35–39.09 | <.001 |
| Peripartum hemorrhage | ||||
| Mode of conception | MAR | 2.02 | 0.76–5.38 | .16 |
| Maternal age (y) | 1.07 | 1.00–1.13 | .047 | |
| Nulliparity | Present | 1.63 | 0.86–3.07 | .13 |
| BMI >30 (before pregnancy) | Present | 0.92 | 0.43–1.97 | .83 |
| Multiple gestation | Present | 3.47 | 1.11–10.86 | .03 |
aOR adjusted for the effects of maternal age (years), nulliparity, BMI >30 (before pregnancy) and multiple gestation.
aOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; HELLP, hemolysis, elevated liver enzymes and low platelets; MAR, medically assisted reproduction; OR, odds ratio.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
HELLP + other hypertensive disorders of pregnancy (eg, pregnancy-induced hypertension, preeclampsia).
Supplemental Table 3.
Multivariate model results for selected neonatal outcomes of women with COVID-19 after medically assisted reproduction and spontaneous conceptions
| Outcomes | Level | OR | 95% CI | P value |
|---|---|---|---|---|
| Preterm birth (<37 gestational wk)a | ||||
| Mode of conception | MAR | 2.32 | 1.19–4.53 | .01 |
| Maternal age (y) | 1.03 | 1.00–1.07 | .10 | |
| Nulliparity | Present | 0.71 | 0.48–1.03 | .07 |
| BMI >30 (before pregnancy) | Present | 0.93 | 0.60–1.42 | .73 |
| Multiple gestation | Present | 15.92 | 6.82–37.16 | <.001 |
| NICU admission | ||||
| Mode of conception | MAR | 1.39 | 0.71–2.75 | .34 |
| Maternal age (y) | 1.07 | 1.03–1.10 | <.001 | |
| Nulliparity | Present | 1.09 | 0.76–1.56 | .66 |
| BMI >30 (before pregnancy) | Present | 1.34 | 0.91–1.98 | .14 |
| Multiple gestation | Present | 11.38 | 5.10–25.37 | <.001 |
| Combined perinatal outcomesa,b | ||||
| Mode of conception | MAR | 1.23 | 0.45–3.38 | .69 |
| Maternal age (y) | 1.08 | 1.03–1.13 | <.001 | |
| Nulliparity | Present | 1.53 | 0.93–2.50 | .09 |
| BMI >30 (before pregnancy) | Present | 1.86 | 1.10–3.20 | .02 |
| Multiple gestation | Present | 6.14 | 1.90–19.91 | .001 |
aOR adjusted for the effects of maternal age (years), nulliparity, BMI >30 (before pregnancy) and multiple gestation.
aOR, adjusted odds ratio; BMI, body mass index; CI, confidence interval; MAR, medically assisted reproduction; NICU, neonatal intensive care unit; OR, odds ratio.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
Based on delivery ≥ 24 weeks of gestation
Combined endpoint composed of NICU admission, stillbirth, and neonatal death.
References
- 1.Trevisanuto D., Cavallin F., Cavicchiolo M.E., Borellini M., Calgaro S., Baraldi E. Coronavirus infection in neonates: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2021;106:330–335. doi: 10.1136/archdischild-2020-319837. [DOI] [PubMed] [Google Scholar]
- 2.Amaral W.N.D., Moraes C.L., Rodrigues A., Noll M., Arruda J.T., Mendonça C.R. Maternal coronavirus infections and neonates born to mothers with SARS-CoV-2: a systematic review. Healthcare (Basel) 2020;8:511. doi: 10.3390/healthcare8040511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conde-Agudelo A., Romero R. SARS-CoV-2 infection during pregnancy and risk of preeclampsia: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;226:68–89.e3. doi: 10.1016/j.ajog.2021.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Figueiro-Filho E.A., Yudin M., Farine D. COVID-19 during pregnancy: an overview of maternal characteristics, clinical symptoms, maternal and neonatal outcomes of 10,996 cases described in 15 countries. J Perinat Med. 2020;48:900–911. doi: 10.1515/jpm-2020-0364. [DOI] [PubMed] [Google Scholar]
- 5.Flaherman V.J., Afshar Y., Boscardin W.J., et al. Infant outcomes following maternal infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): first report from the Pregnancy Coronavirus Outcomes Registry (PRIORITY) Study. Clin Infect Dis. 2021;73:e2810–e2813. doi: 10.1093/cid/ciaa1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takla A., Matysiak-Klose D., Bogdan C., et al. Empfehlung und Begründung der STIKO zur Impfung gegen COVID-19 von Schwangeren und Stillenden. Epidemiologisches Bulletin. 2021;38:10–29. [Google Scholar]
- 7.Pecks U., Kuschel B., Mense L., Oppelt P., Rüdiger M. Pregnancy and SARS-CoV-2 infection in Germany-the CRONOS Registry. Deutsches Arzteblatt International. 2020;117:841–842. doi: 10.3238/arztebl.2020.0841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zambrano L.D., Ellington S., Strid P., et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1641–1647. doi: 10.15585/mmwr.mm6944e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei S.Q., Bilodeau-Bertrand M., Liu S., Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193:E540–E548. doi: 10.1503/cmaj.202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Villar J., Ariff S., Gunier R.B., et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: The INTERCOVID multinational cohort study. JAMA Pediatr. 2021;175:817–826. doi: 10.1001/jamapediatrics.2021.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allotey J., Stallings E., Bonet M., et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinborg A., Wennerholm U.B., Romundstad L.B., et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19:87–104. doi: 10.1093/humupd/dms044. [DOI] [PubMed] [Google Scholar]
- 13.Jackson R.A., Gibson K.A., Wu Y.W., Croughan M.S. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol. 2004;103:551–563. doi: 10.1097/01.AOG.0000114989.84822.51. [DOI] [PubMed] [Google Scholar]
- 14.Helmerhorst F.M., Perquin D.A., Donker D., Keirse M.J. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261. doi: 10.1136/bmj.37957.560278.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Opdahl S., Henningsen A.A., Tiitinen A., et al. Risk of hypertensive disorders in pregnancies following assisted reproductive technology: a cohort study from the CoNARTaS group. Hum Reprod. 2015;30:1724–1731. doi: 10.1093/humrep/dev090. [DOI] [PubMed] [Google Scholar]
- 16.Papageorghiou A.T., Deruelle P., Gunier R.B., et al. Preeclampsia and COVID-19: results from the INTERCOVID prospective longitudinal study. Am J Obstet Gynecol. 2021;225:289.e1–289.e17. doi: 10.1016/j.ajog.2021.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marchand G., Patil A.S., Masoud A.T., et al. Systematic review and meta-analysis of COVID-19 maternal and neonatal clinical features and pregnancy outcomes up to June 3, 2021. AJOG Glob Rep. 2022;2:100049. doi: 10.1016/j.xagr.2021.100049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun S., Savitz D.A., Wellenius G.A. Changes in adverse pregnancy outcomes associated with the COVID-19 pandemic in the United States. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.29560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chmielewska B., Barratt I., Townsend R., et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:e759–e772. doi: 10.1016/S2214-109X(21)00079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angelidou A., Sullivan K., Melvin P.R., et al. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.7523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Piekos S.N., Roper R.T., Hwang Y.M., et al. The effect of maternal SARS-CoV-2 infection timing on birth outcomes: a retrospective multicentre cohort study. Lancet Digit Health. 2022;4:e95–e104. doi: 10.1016/S2589-7500(21)00250-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ESHRE COVID-19 Working Group. Ata B., Gianaroli L., et al. Outcomes of SARS-CoV-2 infected pregancies after medically assisted reproduction. Hum Reprod. 2021;36:2883–2890. doi: 10.1093/humrep/deab218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Engels Calvo V., Cruz Melguizo S., Abascal-Saiz A., et al. Perinatal outcomes of pregnancies resulting from assisted reproduction technology in SARS-CoV-2-infected women: a prospective observational study. Fertil Steril. 2021;116:731–740. doi: 10.1016/j.fertnstert.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blázquez A., García D., Rodríguez A., Vassena R., Figueras F., Vernaeve V. Is oocyte donation a risk factor for preeclampsia? A systematic review and meta-analysis. J Assist Reprod Genet. 2016;33:855–863. doi: 10.1007/s10815-016-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masoudian P., Nasr A., de Nanassy J., Fung-Kee-Fung K., Bainbridge S.A., El Demellawy D. Oocyte donation pregnancies and the risk of preeclampsia or gestational hypertension: a systematic review and metaanalysis. Am J Obstet Gynecol. 2016;214:328–339. doi: 10.1016/j.ajog.2015.11.020. [DOI] [PubMed] [Google Scholar]
- 26.Pecks U., Maass N., Neulen J. Oocyte donation: a risk factor for pregnancy-induced hypertension: a meta-analysis and case series. Dtsch Arztebl Int. 2011;108:23–31. doi: 10.3238/arztebl.2011.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sazonova A., Källen K., Thurin-Kjellberg A., Wennerholm U.B., Bergh C. Obstetric outcome after in vitro fertilization with single or double embryo transfer. Hum Reprod. 2011;26:442–450. doi: 10.1093/humrep/deq325. [DOI] [PubMed] [Google Scholar]
- 28.Kenigsberg S., Bentov Y. Does contemporary ART lead to pre-eclampsia? A cohort study and meta-analysis. J Assist Reprod Genet. 2021;38:651–659. doi: 10.1007/s10815-021-02061-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kulkarni A.D., Jamieson D.J., Jones H.W., Jr., et al. Fertility treatments and multiple births in the United States. N Engl J Med. 2013;369:2218–2225. doi: 10.1056/NEJMoa1301467. [DOI] [PubMed] [Google Scholar]
- 30.von Versen-Höynck F., Schaub A.M., Chi Y.Y., et al. Increased preeclampsia risk and reduced aortic compliance with in vitro fertilization cycles in the absence of a corpus luteum. Hypertension. 2019;73:640–649. doi: 10.1161/HYPERTENSIONAHA.118.12043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosalik K., Carson S., Pilgrim J., et al. Effects of different frozen embryo transfer regimens on abnormalities of fetal weight: a systematic review and meta-analysis. Hum Reprod Update. 2021;28:1–14. doi: 10.1093/humupd/dmab037. [DOI] [PubMed] [Google Scholar]
- 32.Waschkies F., Kroning L., Schill T., et al. Pregnancy outcomes after frozen-thawed embryo transfer in the absence of a corpus luteum. Front Med (Lausanne) 2021;8:727753. doi: 10.3389/fmed.2021.727753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henningsen A.K., Pinborg A., Lidegaard Ø., Vestergaard C., Forman J.L., Andersen A.N. Perinatal outcome of singleton siblings born after assisted reproductive technology and spontaneous conception: Danish national sibling-cohort study. Fertil Steril. 2011;95:959–963. doi: 10.1016/j.fertnstert.2010.07.1075. [DOI] [PubMed] [Google Scholar]
- 34.Luke B. Pregnancy and birth outcomes in couples with infertility with and without assisted reproductive technology: with an emphasis on US population-based studies. Am J Obstet Gynecol. 2017;217:270–281. doi: 10.1016/j.ajog.2017.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raatikainen K., Kuivasaari-Pirinen P., Hippeläinen M., Heinonen S. Comparison of the pregnancy outcomes of subfertile women after infertility treatment and in naturally conceived pregnancies. Hum Reprod. 2012;27:1162–1169. doi: 10.1093/humrep/des015. [DOI] [PubMed] [Google Scholar]
- 36.Bartsch E., Medcalf K.E., Park A.L., Ray J.G. High Risk of Pre-eclampsia Identification Group. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ. 2016;353:i1753. doi: 10.1136/bmj.i1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Maternal and neonatal outcomes of pregnancies with COVID-19 after medically assisted reproduction.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.
Maternal and neonatal outcomes of pregnancies with COVID-19 after medically assisted reproduction.
Ziert et al. Adverse pregnancy outcomes by mode of conception in women with COVID-19. Am J Obstet Gynecol 2022.