Abstract
There are currently 2.2 million people incarcerated in United States prisons and jails, representing a 500% increase over the past 40 years. An emerging literature suggests the impact of mass incarceration extends beyond the prison, jail, or detention center to the families of incarcerated individuals. Less scholarship has considered consequences of parental incarceration for their children’s physical health. We conduct a critical review of the literature investigating an association between parental incarceration and children’s physical health outcomes from infancy to adulthood. Studies varied substantially in study design, sample composition, and methodological approach. Most studies suggest an association between parental incarceration and adverse physical health outcomes. Evidence is more consistent for outcomes such as infant and child mortality, lower healthcare access, and negative health behaviors and more mixed for measures such as self-reported/general health. We propose a multi-level model of mechanistic pathways to stimulate future research on the potential pathways through which parental incarceration could influence children’s physical health..
Keywords: Adverse Childhood Experiences, Child Health, Jails, Prisons
Introduction
Between 1970 and 2015, the number of people incarcerated in the United States increased from roughly 350,000 to over 2.2 million, representing a rate increase of 500% (Garland, 2001). An emerging literature suggests the impact of mass incarceration extends beyond the prison, jail, or detention center to the families and children of incarcerated individuals (Alexander, 2010). Most incarcerated individuals are also parents. According to the Bureau of Justice Statistics, 52% of state and 63% of federal inmates reported being parents to an estimated 1.7 million children at midyear 2007 (Glaze & Maruschak, 2008). Communities with the highest rates of parental incarceration tend to be the most racially and socioeconomically disadvantaged in the United States (Glaze & Maruschak, 2008). Youth from racially marginalized backgrounds experience increased risk of parental incarceration. Black and Latinx children are 7.5 and 2.5 times more likely, respectively, to have an incarcerated parent than white children (Glaze & Maruschak, 2008).
It is increasingly important for researchers to critically evaluate the potential harms of mass incarceration, with a special emphasis on parental incarceration. Research from a wide range of disciplines (e.g. psychology, social work, sociology) has linked parental incarceration to increased likelihood of economic and psychosocial difficulties during childhood, adolescence, and young adulthood (Arditti et al. 2003; Geller et al. 2009; Murray & Murray 2010; Schwartz-Soicher et al. 2011; Arditti, 2012; Murray et al. 2012; Miller & Barnes 2015; Heard-Garris et al. 2019). There are several reasons to hypothesize parental incarceration could undermine youth’s physical health. First, decades of research have demonstrated the parent-child relationship is fundamental for child health and well-being (Bowlby, 2008; Ranson & Urichuk 2008). Particularly at earlier ages, children depend on stable relationships and contact with primary caregivers and when a responsive caregiver is not present, there are downstream impacts on children’s socioemotional and physical health (Tottenham 2012; World Health Organization, 2004). Secondly, research in animal models indicates early adversity can affect the way many systems and organs develop in ways which persist into adulthood (Weaver et al. 2004). This is particularly true for the developing brain, hypothalamic-pituitary-adrenal (HPA) axis and the immune system (McCrory et al. 2010; Hunter et al. 2011; Hostinar & Gunnar 2013). Correlational studies in humans suggest a similar pattern (Miller et al. 2011). An emerging field of study has begun to document similarly poor health outcomes for children with incarcerated parents, such as increased risk of infant and childhood morbidity and mortality (Murray et al. 2012; Wildeman, 2012; Wildeman et al. 2014). There is evidence that these adverse physical health outcomes even persist into adulthood (Lee et al. 2013; Heard-Garris et al. 2018).
The goal of this paper is to a) critically review the emerging literature on parental incarceration and children’s physical health, and b) propose a theoretically plausible model to explain how parental incarceration might influence their children’s health across the life-course. In doing so we ask: What is the state of the evidence in this literature? How effectively are alternative explanations addressed? Is the evidence for an association stronger or weaker at specific stages of the life-course? If the evidence suggests that a relationship exists, how might we illustrate in a model how broader structural disadvantages fit into explaining physical health effects?
Methods
Previous reviews have described associations between parental incarceration and children’s mental health, drug use, attachment problems, psychopathology, behavioral outcomes, and educational outcomes (Geller et al. 2009; Murray et al. 2009; Murray & Murray 2010; Murray et al. 2012). Reviews have also examined physical health and well-being more broadly (Wildeman, 2012; Boch & Ford, 2018). Our narrower focus on physical health facilitates more in-depth synthesis of the evidence and allows more space to identify gaps and best approaches to move this emerging field forward.
Inclusion/exclusion criteria
For inclusion in this review studies needed to be a peer-reviewed publication, examine parental incarceration as a predictor, and include a children’s physical health outcome. For the purposes of this review, parental incarceration refers to any kind of confinement in a jail, prison, or detention center of a child’s parent or primary guardian. Children’s physical health outcomes refers to physical health outcomes of children with incarcerated parents, not necessarily those measured before the age of 18. Subsequently, this review includes health outcomes assessed in adulthood. We define physical health outcomes as processes indicating the presence or absence of illness or injury, health behaviors, and/or physical health needs. We exclude studies focusing on mental health and/or substance use (see Murray et al. 2012 for systematic review and meta-analysis). To improve causal inference, studies were also excluded if they did not include a comparison group of children unexposed to parental incarceration.
Search strategy
Searches were conducted between January 10, 2021 and January 25, 2021. We intentionally cast a wide net and did not limit the year of publication for our search. Keywords were entered into electronic databases and internet search engines. These included PubMed, PsychINFO, and Google Scholar. Keywords included: (incarcerat*, or imprison*, or jail, or prison) and (parent*, or paternal, or maternal, or father, or mother, or caregiver) and (child*, or youth, or young adult*, or family, or infant) and (health, or physical, or health behaviors, or sleep, or asthma, or disease, or cancer, or cardio*, or metabolic, or morbidity, or mortality). We also consulted bibliographies of studies which met inclusion criteria, and bibliographies or prior reviews examining parental incarceration and children’s outcomes.
Results
Study characteristics
Table 1 presents summary characteristics of the 27 studies included in this review. Most studies were published after 2009 (n = 21) and utilized retrospective longitudinal designs (n = 15). The studies primarily employed random, whole population, or probability sampling (n = 20), and were conducted in the United States (n = 22). Five studies focused on current incarceration, with the others focusing on recent incarceration (n=6) or child or parent’s lifetime incarceration (n = 16). Fourteen studies relied on self or parent reported physical health outcomes, while the remainder employed objective measures of physical health such as medical records or measurement by trained professionals.
Table 1.
Study Characteristics
| Characteristic | Category | N |
|---|---|---|
|
| ||
| Study Design | Retrospective Longitudinal | 14 |
| Prospective Longitudinal | 1 | |
| Cross-Sectional | 11 | |
| Publication Year | 1994–2009 | 6 |
| 2010–2019 | 20 | |
| Sampling Method | Whole population or probability | 19 |
| Convenience or case-control | 7 | |
| Incarceration Measure | Current | 5 |
| Recent (within 1–5 years) | 6 | |
| Lifetime History | 15 | |
| Health Outcome Measure | Self or parent report | 14 |
| Objective | 12 | |
| Region of Study | United States | 21 |
| Europe | 2 | |
| Australia | 3 | |
| Sample Size | > 400 | 23 |
| ≤ 400 | 3 | |
| Age of child at outcome | Infant | 11 |
| 0–18 | 10 | |
| 18+ | 6 | |
Methodological quality
Most studies suggest parental incarceration is associated with negative outcomes ranging from unmet health needs, lower healthcare access, chronic disease incidence, and premature mortality. In our synthesis we give greatest narrative weight to studies with greater methodological rigor, defined here as having higher Cambridge Quality Checklist scores (Murray et al. 2009), longitudinal study designs, and appropriate adjustment for covariates. We also recognize there may be considerable variation in associations between parental incarceration by developmental stage of physical health outcome assessment (Adam et al. 2015). As such this section is organized into 3 subsections of the life-course: infancy, early childhood to late adolescence, and adulthood. Table 2 provides summaries of key study characteristics by subsection. Table 2 is organized by study quality (in decreasing order) and study design (longitudinal followed by cross-sectional studies). See Supplemental Tables 1–3 for extended study details and a full list of covariates for each study. Study quality ratings were assessed with the Cambridge Quality Checklist (Murray, Farrington, & Eisner 2009). A summary of study quality ratings and calculations can be found in supplemental table 4.
Table 2.
Parental Incarceration and Physical Health Outcomes Across the Life-course
|
Parental Incarceration and Infant Physical Healt Outcomes
| ||||||
| Reference | Study Design | N | Parent | Incarceration Measure(s) | Health Outcome, measurement, effect a | CQC Rating |
| Dowell et al 2018a | Retrospective longitudinal | 18,902 | Mother | Incarceration up to 5 years before to 1 year after birth, | Infant mortality (+) | 5 |
| Dowell et al 2018b | Retrospective longitudinal | 42,674 | Mother | Incarceration before, during, or after pregnancy, | Infant mortality (+) | 5 |
| Dowell et al 2019 | Retrospective longitudinal | 25.544 (indigenous); 16366 (non-indigenous) | Mother | History of incarceration before, during, or after pregnancy, | LBW < 2500 g (+) | 5 |
| Walker et al 2014 | Cross-sectional | 40,907 | Mother | At least 5 days full-time detention in correctional facility | PTB <37 weeks (+); LBW <2500 g (+); Apgar score <7 (+); esuscitation(n); Neonatal hospital admission (+) |
5 |
| Reichman et al. 2008 | Retrospective longitudinal | 2,412 | Father | Father life-time incarceration history | LBW <2500 g (n) | 4 |
| Martin et al 1997 | Cross-sectional | 4708 | Mother | Prison incarceration before, during or after pregnancy | Infant birth weight (+); LBW <2500 g (+) | 3 |
| Bell et al. 2004 | Cross-sectional | 5,456 | Mother | Current incarceration in county jail | Infant birth weight (+); PTB (+) |
3 |
| Wildeman 2012 | Cross-sectional | 2,244 | Mother or Father | Recent incarceration in prison or jail (past year) | Early infant mortality (+) | 2 |
| Terk et al 1993 | Cross-sectional | 76 | Mother | Current incarceration in state prison | Very LBW <1000 g − medical records; LBW <2500 g (+); Premature birth (+); Neonatal mortality (n); Apgar score <7 (n) | 2 |
| Mertens et al 2001 | Cross-sectional | 122 | Mother | County jail incarceration during pregnancy | LBW <2500 g (+) | 2 |
| Kyei-Aboayge et al. 2000 | Cross-sectional | 149 | Mother | Current incarceration | Infant birth weight (+); Apgar scores (+) | 2 |
|
| ||||||
|
Parental incarceration and early childhood to late adolescence physical health outcomes
| ||||||
| Reference | Study Design | N | Parent | Incarceration Measure(s) | Health Outcome, measurement, effect a | CQC Rating |
| Wildeman et al. 2014 | Prospective Longitudinal | 30, 146 (boys); 28, 702 (girls) | Mother or Father | Child life-time incarceration history, leaded incarceration history | Child mortality (+) | 5 |
| Mitchell et al 2017 | Retrospective Longitudinal | 2,437 | Father | Child life-time incarceration history | Telomere length (+) | 4 |
| Geller et al 2009 | Retrospective Longitudinal | 4,898 | Mother, Father, or Both | Incarceration parent life-time | General health (n) | 3 |
| Geller et al 2012 | Retrospective Longitudinal | 3,000 | Father | Incarceration parent life-time and past 2 years | Subjective Health (n) | 3 |
| Jackson & Vaughn 2017 | Retrospective Longitudinal | Ranged from 2100 – 2388 | Mother, Father, or Both | Parent life-time history of time spent jail or prison | Short sleep duration (+); Sweets and soda (+) consumption (+); Starch consumption (+); Salty snacks consumption (+); Fast food consumption (+) | 3 |
| Haskins & McCauley 2015 | Retrospective Longitudinal | 1,664 | Mother, Father, or Both | Parental incarceration history | General health at age 9 (n) | 3 |
| Branigan & Wildeman 2019 | Retrospective Longitudinal | 2412 | Mother, Father, or Both | Parental incarceration history | Parent-reported overall health (n) | 3 |
| Hiolski et al. 2019 | Cross-sectional | 119, 029 | Parent/guardian | Current incarceration and former incarceration history | Physical activity (+); Fruit and vegetable consumption (+); Fast food consumption (+); Sugar-sweetened beverage (+) consumption (+); 8 hrs of sleep (+); (Self-report) General Health (+) − self reported | 3 |
| Turney 2014 | Cross-sectional | 95,677 | Mother, Father or non-parental guardian | Child life-time incarceration history | Overall health status (+); Asthma (n); Obesity (n); Diabetes (n); bone, joint or muscle problems (n); brain injury or concussion; disability/activity (n) limitations (+); chronic school absence due to injury or illness (n) | 2 |
| Turney 2017 | Cross-sectional | 95,531 | Mother, Father or Non-parental guardian | Child life-time incarceration history | Fair/Poor Health (+); activity limitations (+); chronic conditions (+); unmet health needs (+) | 2 |
| Sykes & Pettit 2015 | Cross-sectional | 95,600 | Mother or Father | Child lives with a parent or guardian who served time in jail or prison | Unmet and delayed health needs (+) | 2 |
|
| ||||||
|
Parental incarceration and adulthood health outcomes
| ||||||
| Reference | Study Design | N | Parent | Incarceration Measure(s) | Health Outcome, measurement, effect a | CQC Rating |
| Boch & Ford 2015 | Retrospective Longitudinal | n = 5,396 males and n = 6,447 females for maternal incarceration; n = 4,956 males and n = 5,860 females for paternal incarceration. | Mother or Father | Parent incarceration (ever) occurring in the child's lifetime; Frequency and timing of incarceration with respect to child's age (0–18 years) | Systemic inflammation hs-CRP (+),moderated by parent and child gender | 4 |
| Lee, Fang, Luo 2013 | Retrospective Longitudinal | 5,470 | Mother, Father, or Both | Parent lifetime history of time spent in prison or jail | Cancer (n); high cholesterol (+); diabetes (n), heart disease (n), asthma (+), HIV/AIDS (+), hepatitis C (n), Obesity (n), fair/poor health (+), moderated by parent gender | 3 |
| Miller & Barnes 2015 | Retrospective Longitudinal | 15,701 | Father | Child life-time incarceration history | Serious injury in past year (+); asthma/bronchitis/emphysema (n); general health problems (n) | 3 |
| Nino & Cai 2020 | Retrospective Longitudinal | 13,365 | Mother or Father | Incarceration history in childhood, pre-adolescence, or adulthood | Allostatic load (+) | 4 |
| Foster & Hagan 2017 | Retrospective Longitudinal | 9,418 | Mother or Father | Life-time incarceration history in jail, prison, or juvenile detention center | Unmet healthcare needs (+),Health insurance, economic marginality | 3 |
| Heard-Garris 2018 | Retrospective Longitudinal | 13, 084 | Mother or Father | Child life-time incarceration history in jail, prison, or juvenile detention center | Forgone healthcare (+), Receipt of annual dental exam (+); Usual source of health care ED (+); Worsening health problems due to reduced healthcare access (+); <50 hours of TV watched/week (+); sugary drink consumption (+); sunblock use (+); fast food consumption (n); fitness center use (n) | 3 |
Notes
Effect significance and directionality – study reports increased risk of adverse health outcome among children with incarcerated parent(s) (+), study reports no significant effect (n); LBW – Low birth weight; PTB – Pre-term birth; CQC – Cambridge Quality Checklist
Parental incarceration and infant outcomes
The following subsection critically reviews evidence for an association between parental incarceration and infant health outcomes (ages 0–1 years). This is the subject of 11 studies in this review. Table 1 provides a detailed summary of key study characteristics and findings of all studies in this subsection. Most studies focused on maternal incarceration (n=10) and was assessed by either prison or administrative records (n=9). Most common infant health outcomes were low birth weight (n= 7), infant mortality (n=3), infant birth weight (n=3), pre-term birth (n=3), and low Apgar scores (n=3). Some studies also examined post-delivery complications such as hospital admission or neonatal resuscitation (n=3), and perinatal and neonatal death (n=2). Most infant health outcomes were assessed from birth certificates or medical records (n=9), with one study relying on mother report (n=1). One study did not identify how the infant health outcome was determined (n=1).
Ten out of 11 studies suggest maternal incarceration is associated with adverse infant health, with the highest quality evidence being from retrospective longitudinal studies (36% n=4), which controlled for demographic covariates to rule out the possibility that the observed findings reflect underlying demographic variations in exposure to parental incarceration. We weight our discussion to studies with the strongest methodological rigor which examine infant mortality, low birth weight, and pre-term birth.
Infant mortality.
Three studies examined the association between parental incarceration and infant mortality defined as the death of an infant before their first birthday. Parental incarceration was defined differently in each of the three above-mentioned studies. In one study parental incarceration was defined as incarceration of a mother up to 5 years before birth and up to one year after birth. In another study parental incarceration was defined as incarceration during pregnancy, before (but not during) pregnancy, or after birth. The final study defined parental incarceration as recent incarceration of a mother or father in the past year. All three studies found evidence suggesting parental incarceration irrespective of duration is associated with an increased risk of infant mortality, compared to infants without a parent incarcerated. The highest quality studies on infant mortality find evidence for maternal incarceration, with some weaker evidence suggesting paternal incarceration may also predict infant mortality.
Two studies by Dowell and colleagues examined an association between maternal incarceration and infant mortality. Each study used linked data from the Western Australian Data Linkage System (WADLS). Using this data source, the first study found that infants whose mothers were incarcerated up to 5 years before birth or within their first year after birth were over 2.2 times as likely to die within the first year compared to infants with mothers with no corrections record (Dowell et al. 2018a). Using the same data source, Dowell and colleagues found that indigenous infants with mothers incarcerated at any time relative to pregnancy (before, during, or after) had increased likelihood of infant mortality (Dowell et al. 2018b).
Wildeman et al. (2012) examined the association between parental incarceration and early infant mortality, defined as death of an infant occurring within the first four months after birth. This study used data from the Pregnancy Risk Assessment Monitoring System (PRAMS), a project of the Centers for Disease Control and Prevention. The authors found that infants with mothers or fathers recently incarcerated (in the past year) experienced a 49 percent increase in the odds of early infant mortality.
Pre-term birth (PTB) and low birth weight (LBW).
Most of the earlier studies examining LBW (< 2500 grams) and PTB (delivery < 37 weeks of gestational age) published between 1994–2001 used fairly small samples consisting of < 200 births and reported mixed findings, some reporting higher rates of PTB and LBW among infants with mothers currently incarcerated, and others reporting no difference. Many of the earlier studies examining LBW and PTB published between 1994–2001 are difficult to interpret because of the overall lower quality ratings, small samples, majority cross-sectional designs, and lack of adjustment for confounds such as race/ethnicity, socioeconomic status, and prenatal care quality.
Two later studies examining PTB and LBW are worth noting for their stronger methodological rigor. First, one study used linked medical records, and found babies born to women incarcerated during pregnancy were at an increased likelihood to be LBW, pre-term, and re-admitted to the hospital after birth compared to community controls (Walker et al. 2014). Dowell et al. 2019 found that maternal imprisonment before or during pregnancy remained associated with infant LBW even after adjusting for significant pregnancy risks.
Parental incarceration and early childhood to late adolescence health outcomes
The following subsection reviews evidence for an association between parental incarceration and adverse health outcomes from early childhood to late adolescence (ages 0–18 years), the subject of 10 studies in this review. Most studies examined a combination of mothers and fathers (n=8), primarily by mother report (n=8). The outcomes assessed were parent-reported general health (n=5), parent-reported health behaviors (n=2), unmet or delayed health needs and health care utilization (n=2), cellular aging (n=1), and child mortality (n=1).
Seven out of 10 studies suggest parental incarceration is associated with adverse childhood health. Patterns are evident among some domains (child mortality, cellular aging, and health behaviors), yet equivocal or non-existent in others (i.e. self-reported health). All studies controlled for demographic confounds, reducing the chance of spurious associations. Highest quality evidence comes from longitudinal studies (n=7).
Subjective health.
Seven of the 11 studies included in the early childhood to late adolescence section examined self or parent-reported health with mixed findings (Geller et al. 2009; Geller et al. 2012; Turney, 2014; Turney, 2017; Haskins & McCauley, 2019; Hiolski et al. 2019; Branigan & Wildeman, 2019). After adjusting for range of covariates (for full list see supplemental table 1) only one study found significant associations between parental incarceration and subjective health.
Negative health behaviors.
Two studies examined associations between parental incarceration and children’s health behaviors at age 5 and in a separate adolescent sample. Both studies suggested that children exposed to parental incarceration had shorter sleep durations and negative eating behaviors such as higher fast-food consumption and lower consumption of fruits and vegetables compared to children without this exposure (Jackson & Vaughn 2017; Hiolski et al. 2019).
Unmet or delayed health needs and healthcare utilization.
Two studies examined the relationship between parental incarceration and unmet or delayed health needs in childhood. Using data from the National Survey of Children’s Health (NSCH) from 2011–2012, Sykes & Petit 2015 showed the percentage of children under 18 with unmet and delayed health needs was two times higher for children who currently lived with a parent with a lifetime history parental incarceration. Turney (2017) also found that parental incarceration during a child’s lifetime was associated with 1.26 times the odds of having any unmet healthcare needs.
Cellular aging.
One study examined the association between father loss due to incarceration and cellular aging as reflected in telomere length from saliva samples. Using FFCWS sample data the authors found children aged 9 with recent father incarceration showed a 10% reduction in telomere length compared to children who did not lose a parent and lived in a 2-parent household. This study uniquely measured father loss due to incarceration prospectively. The authors found the association between father incarceration and child telomere length was mediated 30% by income, suggesting economic strain related to father incarceration may be a pathway linking father incarceration with health (Mitchell et al. 2017).
Child mortality.
One study examined the relationship between parental incarceration and child mortality from ages 0 to 19 (Wildeman et al. 2014). Using a prospective cohort design of 58,848 Danish citizens born in 1991, Wildeman and colleagues found that boys with a father incarcerated were twice as likely to die before the age of 19 compared to boys without a father incarcerated. The authors did not observe the same pattern in child mortality for girls. Mother incarceration did not significantly predict boys or girl’s mortality. Findings suggest both child and parent gender may moderate the relationship between parental incarceration and child health. This study employed a prospective longitudinal design, and reduced recall and selection bias which come with retrospective and case-control study designs.
Parental incarceration and adulthood health outcomes
This final subsection critically reviews evidence for an association between parental incarceration and adulthood health outcomes. This is the subject of six studies in this review. Table 2 provides a summary of key study characteristics and findings for this subsection.
Most studies examined mother and father incarceration history in a prison, jail, or detention center assessed by a combination of mother and father reports (n=5). Adulthood health outcomes were self-reported health (n=2), healthcare access and/or need (n=2), chronic disease risk such as asthma and HIV/AIDS risk (n=2), systemic inflammation (n=1), allostatic load (n=1), health behaviors (n=1), and serious injury (n=1). Most health outcomes were measured via self-report (n=4).
Most studies suggest a relationship between parental incarceration and adulthood health, although there are conflicting findings for asthma. All studies used the National Longitudinal Study of Adolescent Health (Add Health), a 4-wave longitudinal study following a nationally representative probability sample of adolescents in grades 7 through 12 between 1994–1996 (39). Most studies used a combination of Wave 1 (WI) and Wave 4 (WIV) Add Health data (67% n=5). Two studies incorporated additional waves into their analyses.
Systemic inflammation.
One study assessed the relationship between parental incarceration and systemic inflammation as assessed via high sensitivity C-reactive protein (hs-CRP) levels in adulthood at WIV of Add Health (Boch & Ford, 2015). Boch and colleagues examined the association between parental incarceration during childhood and hs-CRP levels in adulthood. The authors found adult women whose biological fathers were incarcerated when they were less than 18 years of age, were more likely to exhibit low-grade inflammation (3–10 mg/L) than women whose fathers were never incarcerated. They also found that frequency of parental incarceration was associated with increased likelihood of low-grade inflammation.
Allostatic load.
One study examined how parental incarceration in childhood or adulthood related to adulthood indices of allostatic load. Using wave IV data from Add health, the authors found that young adults with either parent incarcerated had increased allostatic load scores (Nino & Cai, 2020). Allostatic load was based on nine biomarkers and represented the cumulative wear and tear exacted on important regulatory systems due to the repeated activation of stress response systems. The authors also found that this relationship between parental incarceration and worse allostatic load was present for adults who experienced parental incarceration during childhood, but not present if parental incarceration occurred in adulthood.
Health behaviors, health care access, and utilization.
One study examined how parental incarceration relates to adulthood health behaviors using wave IV data from Add health, Heard-Garris et al. 2018 found that young adults aged 24–34 with father’s incarcerated were at increased risk for risky amount of tv watched per week (>50 h) sugary drink and fast-food consumption. Additionally, two studies examined associations between parental incarceration and healthcare access in adulthood. Heard-Garris et al. 2018 also examined the association of parental incarceration with healthcare use in young adulthood and found that maternal incarceration was associated with increased odds of forgone healthcare, lower likelihood of receiving an annual dental examination, greater likelihood of a child’s usual source of care being in ED or non-primary care setting, and worsening health problems due to reduced access. Foster & Hagan (2017) found that lifetime incarceration of a mother or father was associated with lower likelihood of receiving medical care after adjusting for covariates (Foster & Hagan, 2017).
Lee, Fang, & Luo (2013) examined both mother and father incarceration finding strongest evidence for father incarceration. Father history of incarceration was associated with an increased likelihood of having asthma, migraines, high cholesterol, of fair/poor health, and a four-fold increase in likelihood of having HIV/AIDS. Father incarceration was not associated with risk of cancer, hypertension, diabetes, heart disease, or hepatitis. In comparison, mother incarceration was not associated with any physical health outcomes.
Asthma.
Two studies examined parental incarceration and self-reported physician diagnosis of “asthma/bronchitis/emphysema” with mixed findings. Lee Fang and colleagues found an association between parental incarceration and self-reported asthma in adulthood. However, Miller and Barnes (2015) did not find effects on risk for asthma/bronchitis/emphysema when adjusting for a range of covariates (Supplemental Table 3). It is possible disparate findings are because Lee et al. 2013 used a smaller subsample for which there was complete WI and WIV data.
Interim summary
The findings from this emerging body of literature examining the relationship between parental incarceration and children’s physical health outcomes provide support for three broad conclusions. First, despite considerable variability in sample composition and methodological approach, most studies reviewed suggest an association between parental incarceration and adverse physical health outcomes, and this relationship seems to be apparent from infancy through adulthood. Evidence is more consistent for some health outcomes (infant and child mortality, lower healthcare access, negative health behaviors, and relevant biomarkers) and more mixed among other outcomes (i.e. self-reported/general health). Most associations persisted after adjusting for sociodemographic differences, reducing concerns that findings simply reflect sociodemographic vulnerability.
This review suggests heterogeneity in the strength of the association between parental incarceration and children’s physical health outcomes, and hints gender is a moderator. For example, studies of infancy generally found maternal incarceration was associated with adverse infant health, whereas studies of later periods generally found male children exposed to paternal incarceration had the worst health outcomes. The literature was inconclusive regarding whether race/ethnicity moderates the association parental incarceration and adverse physical health.
Major review limitations and directions for future research
There are a few major limitations present studies did not address. First, no study provided a strong basis for causal inference in the relationship between parental incarceration and children’s physical health. Most studies were either cross-sectional or retrospective longitudinal and measured health outcomes at one time point. Additionally, some studies also lack appropriate statistical control for potential confounding variables, raising the possibility that an unmeasured third variable is creating spurious associations, or that parental incarceration is a proxy for another causal agent. Future studies will need to seriously grapple with these limitations by employing stronger study designs. Below we have outlined three study designs that could be useful in this regard.
First, prospective longitudinal designs would clarify remaining uncertainty about reverse causality, selection biases, and unmeasured confounding variables. Secondly, we think there is opportunity for studies to leverage natural experiments and/or quasi-experimental designs in understanding the relationship between parental incarceration and children’s physical health. Natural experiments could also help mitigate concerns about bias from unmeasured variables and reverse causality (Morgan & Winship, 2015). Lastly sibling comparison design may also be a viable avenue for future research. Sibling comparison designs are useful because they help clarify the role personality traits and/or genetics play in the association parental incarceration and children’s physical health. For instance, future studies might employ sibling comparison designs that compare children of siblings where one parent is incarcerated and the other is not and/or compare siblings when one parent is incarcerated during some critical window, like ages 0–5. These analyses would help control for family differences common to both siblings.
Another major limitation of the studies is the relatively imprecise measurement of parental incarceration. For instance, few studies distinguish between jail and prison, or duration and frequency of parental incarceration. This lack of specificity makes it difficult to determine to gain a full picture of the impact incarceration has on children’s physical health. Additionally, there is room for improvement in the methodological assessment of health outcomes. Future studies will need to find more objective measures of physical health outcomes and ideally measure health at more than one time-point to strengthen conclusions that changes are associated with parental incarceration and not other unmeasured variables.
Lastly, studies were limited in their assessment of mechanisms explaining the association between parental incarceration and children’s physical health. We hope the proposed model is a first step in theorizing multi-level pathways by which parental incarceration might undermine children’s physical health.
Intergenerational and chronic stress of parental incarceration: a multi-level model of potential pathways
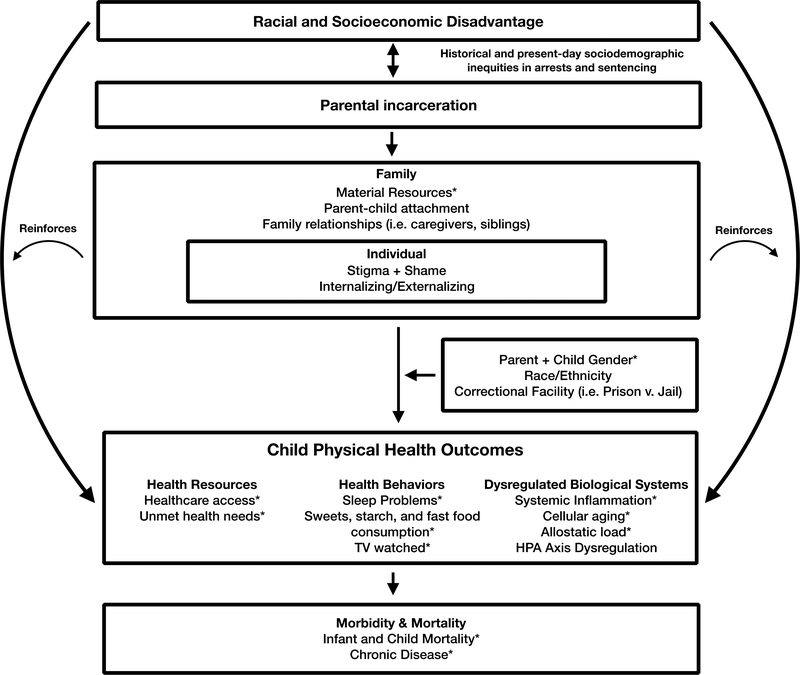
Building upon evidence from the studies evaluated in this review and literature on the biological mechanisms of childhood adversity, we propose a multi-level model to help explain mechanistically how parental incarceration might influence children’s physical health. We include knowledge from perspectives on child and family development (Arditti, 2012; Bronfenbrenner, 1977; Poehlmann et al. 2010), public health (Krieger, 1994), health psychology (Miller et al. 2011), and sociology (Foster & Hagan, 2015). This model proposes parental incarceration as a source of chronic stress, which exacerbates prior childhood disadvantage across several domains and provides unique stressors shown to compromise physical health. We identify mediators and moderators of the relationship between parental incarceration and children’s physical health. We propose these mediators may reinforce broader structural race and class-based disadvantages, exacerbating health disparities for children with incarcerated parents. See figure 1 for a graphic representation of our proposed model.
Figure 1.
Intergenerational and chronic stress of parental incarceration: a proposed model. Constructs found in the extant literature review as a mediator, moderator, and/or outcome are noted with an asterisk (*).
First, our model posits that structural racism and socioeconomic inequalities are fundamental contexts by which we can understand the parental incarceration and physical health relationship. We argue these factors are exogenous variables which predict worse children’s physical health outcomes across the life-course, regardless of parental incarceration status. The relationship between physical health outcomes and low family socioeconomic status and belonging to a marginalized racial group is well-documented internationally (Marmot et al. 2012; Williams, 2012). These structural disadvantages also establish vulnerability to experiencing parental incarceration. Researchers across historical, sociological and legal studies have theorized racial and socioeconomic disadvantage as strong determinants parental incarceration due to cultural and historical antecedents of mass incarceration such as the War on Drugs, mandatory minimum sentences, and long-standing inequities in arrests and sentencing (Alexander, 2010; Thompson, 2010). Thus, parental incarceration may explain, in part, broader racial and socioeconomic disparities.
Next, the model proposes parental incarceration is associated with mediators across family and individual levels. We highlight specific stressors across each level investigated in previous research. Building upon multi-level theories of how the social world affects child development and physical health (Bronfenbrenner, 1977; Poehlmann et al. 2010; Miller et al. 2011), we hypothesize factors across family and individual levels influence each other, shaping children’s experiences across the life-course.
Lastly, we organize children’s health outcomes included in the present review by temporal pathways. Shorter term and/or behavioral, resource, and physiological intermediates outcomes are distinguished from longer term outcomes such as morbidity and mortality. Morbidity/mortality across the life-course tend to result from longer term physiological and behavioral processes that take time to develop. We argue future research would benefit from increased specificity on types of health outcomes assessed, and where in the sequelae of biological and behavioral processes outcomes health outcomes are situated to guide study design and types of questions that are asked. Constructs found in the extant literature review as a mediator, moderator, and/or outcome are noted with an asterisk. Proposed mechanisms (without an asterisk) should be interpreted as hypotheses to test in future research.
Family-level mediators
Material resources.
Parental incarceration reduces material resources and is associated with additional financial costs which can affect their children. This is due to the loss of a potential income, loss of child support, and new expenses associated with incarceration such as bail and the costs of visits and phone calls, and decreased labor earnings potential once parents are released from prison (Alexander, 2010; Pager, 2008). Decreased material resources and increase in material strains have implications for health across the life-course. Individuals who have lower socioeconomic status consistently have poorer health across a variety of diseases and risk factors for disease(Adler et al. 1994). Additional costs, and reduced income and earnings potential to families may be one pathway by which parental incarceration predicts worse child health outcomes for future research to address. One study in this review found that loss of material resources from parental incarceration was a mediating factor (Mitchell et al. 2017). Future studies will need to extend this line of research.
Parent-child attachment.
Parental incarceration also has implications for parent-child attachment. Edin et al. (2004) found that incarcerated parents with consistent contact with their child prior to incarceration, report that incarceration yielded a pronounced negative effect on their relationship with their child. And in qualitative interviews of youth aged 9 and older, Shlafer & Poehlmann (2010) found children with a lack of contact with incarcerated parents reported decreased attachment compared to children who maintained contact with the incarcerated parent. Research suggests insecure attachment styles are linked to risk of inflammation, cortisol, and cardiometabolic risk (Ehrlich & Cassidy, 2019). Future studies will need to examine parent-child attachment as a potential mediator of the relationship between parental incarceration and child health.
Family relationships.
Parental incarceration affects broader family dynamics such as caregiving arrangements, and family structure (Glaze & Maruschak, 2008). Most parental incarceration is of fathers, so most children with incarcerated fathers tend to live with their mothers during the incarceration period. In contrast, children with incarcerated mothers are more likely to live with their grandparents, other family members, or in institutional care such as foster care (Glaze & Maruschak, 2008). Changes to the household may be accompanied by stress and strain on the remaining caregivers who tend to be low-income and/or people of color with few economic resources. Instability in family relationships may be introduced and/or exacerbated following parental incarceration, with implications for child health. Future research will need to examine how changes in the quality and structure of family relationships mediates the relationship between parental incarceration and children’s health.
Individual-level mediators
Stigma and shame.
Stigma may be another individual-level factor mediating the relationship between parental incarceration and children’s health. Data suggest parental incarceration carries a stigma because it does not engender the same support or compassion from neighbors and friends as parental death or illness, because parents are seen as responsible for the separation (Phillips & Gates, 2011). This has downstream influences on children and in some cases may contribute to isolation. Children with incarcerated parents report being unsure who to talk about with their experiences and tending to keep things to themselves to prevent judgment (Nesmith & Ruhland, 2008). Due to stigma of parental incarceration some parents and caregivers do not tell their children the truth about their parent’s situation which can increase feelings of abandonment and confusion as to why the parent is gone (Bocknek et al. 2009). Both stigma and shame are particularly detrimental for physical health (Kemeny et al. 2004; Hatzenbuehler & Link, 2014). How stigma and shame operates to influence children’s physical health is a factor for future research to examine.
Internalizing and externalizing behaviors.
Externalizing behaviors are characterized primarily by actions in the external world, such as antisocial behavior, hostility, and aggression. In contrast internalizing behaviors are characterized primarily by processes within the self, such as anxiety and depression. There is some evidence parental incarceration is associated with increased internalizing and externalizing symptoms in children, with gender differences (Shlafer & Poehlmann, 2010). Future research should investigate the role of internalizing and externalizing in the relationship between parental incarceration and children’s physical health outcomes across the life-course.
Moderators
Parent and child gender.
Variation in the effect of parental incarceration on children’s health by both parent and child gender are demonstrated in this review. Researchers have proposed a “gendered loss hypothesis” by which girls and women may respond with internalizing symptoms while boys and men respond with externalizing and/or risk-taking behaviors (Umberson, 2003; Foster & Hagan, 2015). Future research will need to examine the specific ways parent and child gender moderate the relationship between parental incarceration and children’s physical health.
Child age.
Both child age at incarceration, and age of health outcome assessment may be moderators for future research to examine. The studies in this review were unable to differentiate if the effects of parental incarceration were stronger (or weaker) at different ages. Future studies which examine age of parental incarceration and age of health outcome assessment as moderators of the relationship between parental incarceration and children’s health will be helpful in increasing our understanding.
Correctional facilities.
We hypothesize facility type (i.e. prison vs. jail) may have implications for long-term child health. US jails are often located closer to the incarcerated individual’s family members while state prisons are often located further away from home (Mumola, 2000). For children who do stay in contact with an incarcerated parent, correctional facilities are not inviting places and may cause stress and feelings of alienation during and after visiting (Poehlmann et al. 2010). Future research will need to examine ways that correctional facilities shape experiences of the parent and child following incarceration and the implications this has for children’s physical health.
Conclusion
An emerging literature indicates that parental incarceration is associated with adverse physical health problems in some domains, but not others. We hope the critical review and multi-level model offered here is useful to researchers. Future research is needed to build on this emerging literature and extend our understanding of the mechanistic pathways that might explain causally how an association between parental incarceration and children’s physical health arises. Future research will need to employ methods extending across multiple levels of analysis and be multidisciplinary in scope, cross-cutting the biological and social sciences. Health researchers, practitioners, and community members could join ongoing efforts to improve the health of the children, families and communities impacted by parental incarceration.
Supplementary Material
Acknowledgments
Funding: Manuscript preparation was supported by NIH Grant 1T37MD014248-01.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
Ethics Statement: Ethical approval was not applicable to this article as no human or animal subjects were used in the current study
Data Availability Statement:
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- Adam EK, Heissel JA, Zeiders KH, Richeson JA, Ross EC, Ehrlich KB, Levy DJ, Kemeny M, Brodish AB, Malanchuk O, Peck SC, Fuller-Rowell TE, & Eccles JS (2015). Developmental histories of perceived racial discrimination and diurnal cortisol profiles in adulthood: A 20-year prospective study. Psychoneuroendocrinology, 62, 279–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, & Syme SL (1994). SES and health: the challenge of the gradient. American Psychologist Journal, 49(1), 15–24. [DOI] [PubMed] [Google Scholar]
- Alexander M (2010). The new Jim Crow: mass incarceration in the age of colorblindness. New York, New York: New Press [Google Scholar]
- Arditti JA, Lambert-Shute J, & Joest K (2003). Saturday morning at the jail: Implications of incarceration for families and children. Family Relations, 52(3), 195–204. [Google Scholar]
- Arditti JA (2012). Parental incarceration and the family: Psychological and social effects of imprisonment on children, parents, and caregivers. NYU Press. [Google Scholar]
- Bell JF, Zimmerman FJ, Cawthon ML, Huebner CE, Ward DH, & Schroeder CA (2004). Jail incarceration and birth outcomes. Journal of Urban Health, 81(4), 630–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boch SJ, & Ford JL (2015). C-reactive protein levels among US adults exposed to parental incarceration. Biological Research For Nursing, 17(5), 574–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boch SJ, & Ford JL (2018). Health outcomes of youth in the United States exposed to parental incarceration: An integrative review. Journal of Forensic Nursing, 14(2), 61–71. [DOI] [PubMed] [Google Scholar]
- Bocknek EL, Sanderson J, & Britner PA (2009). Ambiguous loss and posttraumatic stress in school-age children of prisoners. Journal of Child and Family Studies, 18(3), 323–333. [Google Scholar]
- Bowlby J (2008). A secure base: Parent-child attachment and healthy human development. Basic books. [Google Scholar]
- Branigan AR, & Wildeman C (2019). Parental Incarceration and Child Overweight: Results from a Sample of Disadvantaged Children in the United States. Public Health Reports, 134(4), 363–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. [Google Scholar]
- Dowell CMM, Mejia GC, Preen DB, & Segal L (2018). Maternal incarceration, child protection, and infant mortality: a descriptive study of infant children of women prisoners in Western Australia. Health Justice, 6(2), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowell CMM, Mejia GC, Preen DB, & Segal L (2018). Determinants of infant mortality for children of women prisoners: A longitudinal linked data study. BMC Pregnancy and Childbirth, 18(1), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edin K, Nelson TJ, & Paranal R (2001). Fatherhood and incarceration as potential turning points in the criminal careers of unskilled men. Evanston, IL: Institute for Policy Research, Northwestern University. [Google Scholar]
- Ehrlich K, & Cassidy J (2019). Attachment and physical health: Introduction to the special issue. Attachment &Human Development, 21(1), 1–4. [DOI] [PubMed] [Google Scholar]
- Foster H, & Hagan J (2015). Punishment regimes and the multilevel effects of parental incarceration: Intergenerational, intersectional, and interinstitutional models of social inequality and systemic exclusion. Annual Review of Sociology, 41, 135–158. [Google Scholar]
- Foster H, & Hagan J (2017). Maternal imprisonment, economic marginality, and unmet health needs in early adulthood. Preventive Medicine, 99, 43–48. [DOI] [PubMed] [Google Scholar]
- Garland D (Ed.). (2001). Mass imprisonment: Social causes and consequences. Sage. [Google Scholar]
- Geller A, Garfinkel I, Cooper CE, Mincy RB (2009). Parental incarceration and child well-being: Implications for urban families. Social Science Quarterly, 90(5), 1186–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller A, Cooper CE, Garfinkel I, et al. (2012). Beyond Absenteeism: Father Incarceration and Child Development. Demography, 49(1), 49–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaze LE, & Maruschak LM (2008). Parents in prison and their minor children (Bureau of Justice Statistics Special Report). Washington, DC: Bureau of Justice Statistics. [Google Scholar]
- Haskins AR, & McCauley EJ (2019). Casualties of context? Risk of cognitive, behavioral and physical health difficulties among children living in high-incarceration neighborhoods. Journal of Public Health (Germany), 27(2), 175–183. [Google Scholar]
- Hatzenbuehler ML, & Link BG (2014). Introduction to the special issue on structural stigma and health. Social Science & Medicine, 103, 1–6. [DOI] [PubMed] [Google Scholar]
- Heard-Garris N, Sacotte KA, Winkelman TN, Cohen A, Ekwueme PO, Barnert E, Carnethon M, Davis MM (2019). Association of childhood history of parental incarceration and juvenile justice involvement with mental health in early adulthood. JAMA Network Open, 2(9), e1910465–e1910465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heard-Garris N, Winkelman TN, Choi H, Miller AK, Kan K, Shlafer R, & Davis MM (2018). Health care use and health behaviors among young adults with history of parental incarceration. Pediatrics, 142(3). [DOI] [PubMed] [Google Scholar]
- Hiolski K, Eisenberg ME, & Shlafer RJ (2019). Youth self-reported health and their experience of parental incarceration. Families, Systems, & Health, 37(1), 38–45. [DOI] [PubMed] [Google Scholar]
- Hostinar CE, & Gunnar MR (2013). The developmental effects of early life stress: An overview of current theoretical frameworks. Current Directions in Psychological Science, 22(5), 400–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter AL, Minnis H, & Wilson P (2011). Altered stress responses in children exposed to early adversity: a systematic review of salivary cortisol studies. Stress, 14(6), 614–626. [DOI] [PubMed] [Google Scholar]
- Jackson DB, & Vaughn MG (2017). Parental Incarceration and Child Sleep and Eating Behaviors. The Journal of Pediatrics, 185, 211–217. [DOI] [PubMed] [Google Scholar]
- Kemeny ME, Gruenewald TL, & Dickerson SS (2004). Shame as the emotional response to threat to the social self: Implications for behavior, physiology, and health. Psychological Inquiry, 15(2), 153–160. [Google Scholar]
- Kyei-Aboagye K, Vragovic O, & Chong D (2000). Birth outcome in incarcerated, high-risk pregnant women. Obstetrical & Gynecological Survey, 55(11), 682–684. [PubMed] [Google Scholar]
- Krieger N (1994). Epidemiology and the web of causation: has anyone seen the spider? Social Science Medicine, 39(7), 887–903. [DOI] [PubMed] [Google Scholar]
- Lee RD, Fang X, & Luo F (2013). The impact of parental incarceration on the physical and mental health of young adults. Pediatrics, 131, e1188–e1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M, Allen J, Bell R, Bloomer E, & Goldblatt P (2012). WHO European review of social determinants of health and the health divide. The Lancet, 380(9846), 1011–1029. [DOI] [PubMed] [Google Scholar]
- McCrory E, De Brito SA, & Viding E (2010). Research review: the neurobiology and genetics of maltreatment and adversity. Journal of Child Psychology and Psychiatry, 51(10), 1079–1095. [DOI] [PubMed] [Google Scholar]
- Mertens DJ (2001). Pregnancy outcomes of inmates in a large county jail setting. Public Health Nursing, 18(1), 45–53. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, & Parker KJ (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller HV, & Barnes JC (2015). The association between parental incarceration and health, education, and economic outcomes in young adulthood. American Journal of Criminal Justice, 40(4), 765–784. [Google Scholar]
- Mitchell C, McLanahan S, Schneper L, Garfinkel I, Brooks-Gunn J, & Notterman D (2017). Father loss and child telomere length. Pediatrics, 140(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan SL, & Winship C (2015). Counterfactuals and causal inference. Cambridge University Press. [Google Scholar]
- Mumola CJ (2000). Incarcerated parents and their children. US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. [Google Scholar]
- Murray J, Farrington DP, & Eisner MP. Drawing conclusions about causes from systematic reviews of risk factors: The Cambridge Quality Checklists. J Exp Criminol 2009;5(1):1–23. [Google Scholar]
- Murray J, Farrington DP, Sekol I, & Olsen RF (2009). Effects of parental imprisonment on child antisocial behaviour and mental health: A systematic review. Campbell Systematic Reviews, 5(1), 1–105. [Google Scholar]
- Murray J, & Murray L (2010). Parental incarceration, attachment and child psychopathology. Attachment & Human Development, 12(4), 289–309. [DOI] [PubMed] [Google Scholar]
- Murray J, Farrington DP, & Sekol I (2012). Children’s antisocial behavior, mental health, drug use, and educational performance after parental incarceration: a systematic review and meta-analysis. Psychological Bulletin, 138(2), 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesmith A, & Ruhland E (2008). Children of incarcerated parents: Challenges and resiliency, in their own words. Children and Youth Services Review, 30(10), 1119–1130. [Google Scholar]
- Niño MD, & Cai T (2020). Timing of parental incarceration and allostatic load: a developmental life course approach. Annals of Epidemiology, 43, 18–24. [DOI] [PubMed] [Google Scholar]
- Pager D (2018). Marked: Race, crime, and finding work in an era of mass incarceration (pp. 260–268). Routledge. [Google Scholar]
- Phillips S, & Gates T (2011) A conceptual framework for understanding the stigmatization of children of incarcerated parents. Journal of Child and Family Studies, 20, 286–294. [Google Scholar]
- Poehlmann J, Dallaire D, Loper AB, & Shear LD (2010). Children’s contact with their incarcerated parents: research findings and recommendations. American Psychologist, 65(6), 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranson KE, & Urichuk LJ (2008). The effect of parent–child attachment relationships on child biopsychosocial outcomes: a review. Early Child Development and Care, 178(2), 129–152. [Google Scholar]
- Schwartz-Soicher O, Geller A, & Garfinkel I (2011). The effect of paternal incarceration on material hardship. Social Service Review, 85(3), 447–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shlafer RJ, & Poehlmann J (2010). Attachment and caregiving relationships in families affected by parental incarceration. Attachment & Human Development, 12(4), 395–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terk JV, Martens MG, & Williamson MA (1993). Pregnancy outcomes of incarcerated women. Journal of Maternal-Fetal Medicine, 2(5), 246–250. [Google Scholar]
- Thompson HA (2010). Why mass incarceration matters: Rethinking crisis, decline, and transformation in postwar American history. Journal of American History, 97(3), 703–734. [Google Scholar]
- Tottenham N (2012). Human amygdala development in the absence of species-expected caregiving. Developmental Psychobiology, 54(6), 598–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turney K (2014). Stress proliferation across generations? Examining the relationship between parental incarceration and childhood health. Journal of Health and Social Behavior, 55(3), 302–319. [DOI] [PubMed] [Google Scholar]
- Turney K (2017). Unmet Health Care Needs among Children Exposed to Parental Incarceration. Maternal Child Health Journal, 21(5), 1194–1202. [DOI] [PubMed] [Google Scholar]
- Umberson D (2003). Death of a parent: Transition to a new adult identity. Cambridge University Press. [Google Scholar]
- Walker JR, Hilder L, Levy MH, & Sullivan EA (2014). Pregnancy, prison and perinatal outcomes in New South Wales, Australia: a retrospective cohort study using linked health data. BMC Pregnancy and Childbirth, 14(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver IC, Cervoni N, Champagne FA, D’Alessio AC, Sharma S, Seckl JR, Dymov S, Szyf M, Meaney MJ (2004). Epigenetic programming by maternal behavior. Nature Neuroscience, 7(8), 847–854. [DOI] [PubMed] [Google Scholar]
- Wildeman C, Andersen SH, Lee H, & Karlson KB (2014). Parental incarceration and child mortality in Denmark. American Journal of Public Health, 104(3), 428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C (2012). Imprisonment and Infant Mortality. Social Problems, 59(2), 228–257. [Google Scholar]
- Williams DR (2012). Miles to go before we sleep: Racial inequities in health. Journal of Health and Social Behavior, 53(3), 279–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2004). The importance of caregiver-child interactions for the survival and healthy development of young children: A review.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.