Abstract
Purpose
The standard treatment for locally advanced cervical cancer (LACC) is concomitant chemoradiotherapy with cisplatin (CDDP) followed by brachytherapy. The presence of comorbidities are risk factors for nephrotoxicity and are associated with lower survival. Gemcitabine is a radiosensitizing drug that has shown efficacy and safety in this context. The effectiveness of concomitant chemoradiotherapy with gemcitabine was evaluated versus cisplatin in LACC patients with comorbidities and preserved renal function.
Materials and Methods
An observational, longitudinal and paired study was carried out that included patients treated between February 2003 and December 2015. The primary objectives were to evaluate response rates, progression-free survival, and overall survival; the secondary objectives were to evaluate toxicity and renal function.
Results
Sixty-three patients treated with gemcitabine at 300 mg/m2 weekly and 126 patients treated with CDDP 40 mg/m2 weekly were included. There were no significant differences in response rates and survival rates. Treatment with cisplatin presented a higher frequency of hematological toxicities, while gemcitabine presented a higher frequency of gastrointestinal toxicities. A decrease in glomerular filtration rate (GFR; baseline vs. 1-year post-treatment) was observed in the cisplatin group (p=0.002), while not in the gemcitabine group (p=0.667). In a multivariate analysis, it is observed that only CDDP correlates with the decrease in GFR (hazard ratio, 2.42; p=0.012).
Conclusion
In LACC patients with comorbidities, gemcitabine and CDDP show the same efficacy, with different toxicity profiles. Treatment with cisplatin is associated with a significant decrease in GFR during follow-up, compared to treatment with gemcitabine that does not decrease it.
Keywords: Locally advanced cervical cancer, Comorbidities, Nephrotoxicity, Gemcitabine
Introduction
Cervical cancer (CC) represents a public health problem worldwide, being the fourth cause of cancer incidence and mortality in women, with 569,847 cases per year and 311,365 deaths per year [1]. In Mexico, it represents the third cause of cancer incidence in women (11 cases per 100,000 inhabitants) and the second cause of death (5.8 cases per 100,000 inhabitants) [1,2].
The standard of treatment in locally advanced disease is concomitant chemoradiotherapy (CT-RT) followed by brachytherapy, with an absolute improvement in overall survival (OS) of 6% and in progression-free survival (PFS) of 8% when compared to chemotherapy. The most commonly used regimen in concomitance is cisplatin (CDDP, cis-diaminodichloroplatin II) at a dosage of 40 mg/m2/wk for a period of 5–6 weeks [3,4]. The main adverse events associated with CDDP are nephrotoxicity, nausea, vomiting, neurotoxicity and ototoxicity [5]. Studies have shown that the main dose limitation for its use is nephrotoxicity, therefore, the choice of this drug as a radio sensitizer requires a careful evaluation of renal function before deciding its administration [6].
It has been documented that the presence of comorbidities are risk factors for presenting acute kidney injury with CDDP and are associated with lower survival [7,8]. Also, patients with cancer and comorbidities—measured by the Charlson Index (CI)—present an unfavorable prognosis in OS [9]. The CI is a system for evaluating life expectancy at ten years, depending on the comorbidities and the age of the subject (19 items) [10]. These data are relevant, since in our country 10.3% of the population older than 20 years has type 2 diabetes mellitus (T2DM) and 18.4% has systemic arterial hypertension (SAH) [11], which is reflected in CC patients.
The risk of toxicity associated with treatment with CDDP and the presence of comorbidities in our population has led to the search for radiosensitizing drugs with the same efficacy as CDDP, but without the associated toxicities [12,13].
Gemcitabine is a specific deoxycytidine analog, with activity in the S phase of the cell cycle, this antimetabolite has shown cytotoxic effects against a wide variety of tumor cells in vitro and antitumor effects in vivo in animal models [14]. The radiosensitizing property of gemcitabine in CC has been evaluated in multiple clinical studies, demonstrating efficacy and a different toxicity profile when used at doses ranging from 100 to 1,000 mg/m2/wk. Several studies have evaluated the efficacy of gemcitabine at different doses. The first study to evaluate the efficacy and safety of gemcitabine was conducted by McCormack and Thomas [15] in CC patients treated with gemcitabine at doses of 50 to 150 mg/m2/wk, authors reported adequate tolerance, however, the limiting dose of toxicity was not determined. Boualga et al. [16] evaluated gemcitabine at a dose of 300 to 600 mg/m2/wk in CC patients, a low toxicity profile and a complete response rate (RR) of 89% were documented. Pattaranutaporn et al. [17], demonstrated adequate tolerance of gemcitabine at a weekly dose of 300 mg/m2 with a benefit in PFS of 84%, 1 year OS of 100%, and complete RRs of 89%. Verma et al. [18] demonstrated that gemcitabine at a dose of 150 mg/m2/wk can be used as an alternative to CDDP in patients with comorbidities; however, the complete RR was only 70%. In a similar study, Kundu et al. [19] demonstrated a complete RR of 69% using gemcitabine at a dose of 150 mg/m2/wk, inferior to the RR described for CDDP. These studies demonstrate that gemcitabine at a dose of 150 mg/m2/wk is inferior to the RR reported with a dose of 300 mg/m2/wk. Also, Cetina et al. [20] showed that gemcitabine could be used even in patients with compromised renal function at a dose of 300 mg/m2/wk with a complete RR of 89%.
The purpose of the present study is to evaluate the effectiveness of concomitant CT-RT with gemcitabine, using a dose of 300 mg/m2/wk, compared to CDDP, at a dose of 40 mg/m2/wk, in locally advanced CC (LACC) patients with comorbidities and preserved renal function (glomerular filtration rate [GFR] ≥ 60 mL/min).
Materials and Methods
1. Study design
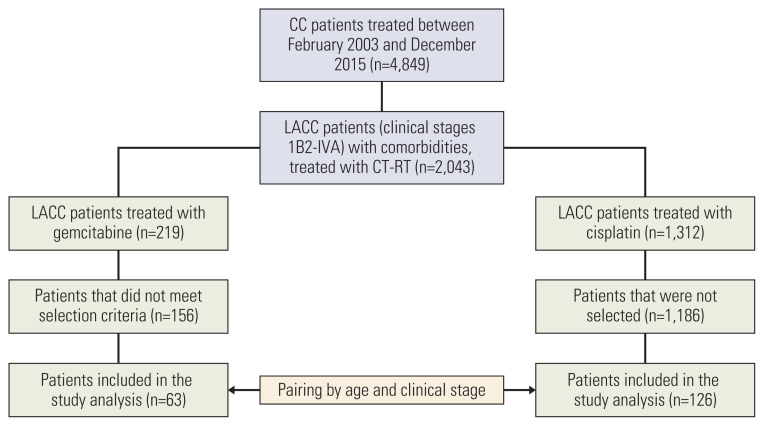
An observational, longitudinal, paired and retrolective study was carried out that included LACC patients with comorbidities treated between February 2003 and December 2015 in a single institution. Two groups were established: group 1, patients treated with CT-RT with gemcitabine; and group 2, patients treated with CT-RT with cisplatin (Fig. 1). The total number of CC patients treated at the Instituto Nacional de Cancerología (National Cancer Institute of Mexico) between February 2003 and December 2015 was 4,849 patients. From these, the number of LACC patients that also presented comorbidities was 2,043. From these, all patients treated with gemcitabine were 219, and the number of patients that met the eligibility criteria (as described below) and were selected for the study was 63. For the second group, from the 2,043 LACC patients with comorbidities, 1,312 were treated with cisplatin. From these, patients that met eligibility criteria were matched by age and clinical stage 2:1 with the 63 patients from the gemcitabine group, therefore 126 patients treated with cisplatin were included in the study. We performed a propensity score matching analysis using the variables age, clinical stage, and GFR. We estimated the average treatment on the treated in the RR, and additionally the effect in the unmatched (data not shown). We found that the matching does not represent a relevant impact among treatment groups.
Fig. 1.
Study population. An observational, longitudinal, paired and retrolective study was carried out that included locally advanced cervical cancer (LACC) patients with comorbidities treated between February 2003 and December 2015. Patients treated with gemcitabine were paired by age and clinical stage with patients treated with cisplatin. CC, cervical cancer; CT-RT, concomitant chemoradiotherapy.
The primary objectives of the study were to evaluate RR, PFS, and OS. The secondary objectives were to evaluate toxicity and renal function.
2. Patients
Eligibility criteria included an adequate functional status (Eastern Cooperative Oncology Group of 0–2) and creatinine clearance ≥ 60 mL/min, assessed by CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). The inclusion criteria were histological confirmation of CC; locally advanced disease (International Federation of Gynecology and Obstetrics 2008); no previous history of surgery, chemotherapy or radiotherapy; and diagnosis of any associated comorbidity. The comorbidities studied were T2DM, SAH, history of acute kidney injury and others (ischemic heart disease, congestive heart failure, rheumatoid arthritis, systemic lupus erythematosus, Sjögren’s syndrome, progressive systemic sclerosis, dermatomyositis and mixed connective tissue disease). Patients diagnosed with a second neoplasm, histology of small cells or neuroendocrine tumor were excluded; pregnant or lactating patients were also excluded. As described above, patients treated with CT-RT with gemcitabine were matched 1:2—by age and clinical stage—with those treated with CDDP.
3. Treatment
The drug selected for concomitance treatment was determined by the physician’s preference. The most used regimen in concomitance was cisplatin. The main parameter used for choosing gemcitabine was the presence of acute kidney injury, other factors that weighed in the physician’s decision to use gemcitabine were a deteriorated performance status, the presence of comorbidities or geriatric age; however, this is not an institutional policy, but it has been a medical behavior. Patients treated with gemcitabine at a dose of 300 mg/m2 weekly or treated with CDDP at a dose of 40 mg/m2 weekly, concomitantly with external radiotherapy (RT), followed by brachytherapy, were included. Chemotherapy (CT) was administered intravenously since the beginning of RT. Patients received at least 3 weekly cycles of CT, and its duration could be extended to seven cycles until the completion of RT. The patients received external RT of 50.4 Gy to the pelvic region in 28 sessions of 1.8 Gy/day, 5 days a week, during the weeks of CT. External beam RT was administered using a standard 4-field box technique (anteroposterior, posteroanterior, and 2 lateral) for energy sources greater than 6 MeV. Immediately after completing the CT-RT, the patients underwent brachytherapy. Brachytherapy was administered either at a high dose intracavitary radiation rate of 6–7 Gy/4–5 fx or at a low dose intracavitary radiation rate of 17–20 Gy/1–2 fx.
4. Response and toxicity assessment
Response was established by physical examination, cervical cytology and imaging studies—using the Response Evaluation Criteria In Solid Tumors (RECIST v1.1)—at the follow-up visit, 2 months after RT. The imaging studies performed could include abdominopelvic computed tomography, magnetic resonance imaging (MRI).
Patient follow-up was carried out after the completion of CT-RT and consisted of visits every 3 months for the first 2 years, every 6 months for the next 3 years, and annually thereafter. PFS was defined as the period from the start of treatment to local/systemic relapse, implying that they achieved complete remission. Pattern of failure was defined as disease recurrence after 6 months of complete remission, according to the site of recurrence: (1) local (disease recurrence confined to the cervix, parametria, and vagina); (2) locoregional (disease recurrence to cervix, parametria, vagina and additionally bladder, rectum, and pelvic lymph nodes); (3) distant metastasis (disease recurrence to para-aortic, paracaval, intercavo-aortic, infradiaphragmatic, supradiaphragmatic, mediastinal, axillary, neck, cervical and inguinal lymph nodes, liver, lung, pancreas, bone, brain, meninges, and peritoneal carcinomatosis); (4) locoregional and distant metastasis (disease progression to both, locoregional and distant tissues); and (5) persistent disease (lack of complete remission or disease recurrence before 6 months after complete remission). OS was defined as the period from the start of treatment to death (by any cause) or date of last contact with the patient. If a patient was lost to follow-up, that patient was censored from the date of the last contact.
Weekly monitoring performed by a medical oncologist during CT-RT, consisted of a complete physical examination and laboratory tests, including complete blood count and blood chemistry. Adverse events were reported in weekly medical visits and follow-up, using the Common Terminology Criteria of Adverse Events (v.4.03).
Glomerular filtration rate (GFR) was calculated by the CKD-EPI method [21]. Measurements were made before starting treatment, immediately and 1 year after treatment completion.
5. Statistical analysis
A descriptive analysis of the variables was carried out. For quantitative variables, measures of central tendency and dispersion (mean±standard deviation and median [interquartile range]) were estimated, and for qualitative variables, absolute and relative frequencies were reported.
Comparisons between the two groups were carried out using the chi-square test, Student t test and/or Wilcoxon test. A value of p < 0.05 was considered statistically significant. The analysis of PFS and OS was estimated by the Kaplan-Meier method, using log-rank. A multivariate analysis was performed using logistic regression to assess the increase or decrease in GFR. The data collected was analyzed in the IBM SPSS Statistics ver. 23.0 package (IBM Corp., Armonk, NY) and PRISM ver. 9 (GraphPad Software Inc., San Diego, CA).
Results
1. Characteristics of the patients
A total of 4,849 CC patients treated between February 2003 and December 2015 were identified. LACC patients with comorbidities treated with CT-RT were selected (n=2,043); of these, 219 patients received treatment with gemcitabine, but 156 did not meet the selection criteria. Therefore, 63 patients were included in the gemcitabine group. These patients were paired with 126 patients selected from 1,312 patients who received treatment with cisplatin (Fig. 1). Table 1 describes baseline clinical characteristics of patients. The mean age was 56.3 years, the most prevalent clinical stage was IIB (57%) and the histopathological examination revealed squamous cell carcinoma in 83.1% of patients. There were no statistically significant differences in age, performance status, clinical stage, histological type of tumor, and number of comorbidities among groups; however, the types of comorbidities were different among groups (Table 1).
Table 1.
Clinical characteristics of locally advanced cervical cancer patients
| Characteristic | Total patients (n=189) | Cisplatin (n=126) | Gemcitabine (n=63) | p-value |
|---|---|---|---|---|
| Age (yr) a) | 56.3±11.5 | 55.4±10.9 | 57.9±12.5 | 0.668b) |
| Performance status c) | ||||
| ECOG 0 | 77 (40.7) | 47 (37.3) | 30 (47.6) | 0.348d) |
| ECOG 1 | 107 (56.6) | 76 (60.3) | 31 (49.2) | |
| ECOG 2 | 5 (2.6) | 3 (2.4) | 2 (3.2) | |
| Clinical stage e) | ||||
| IB2 | 12 (6.3) | 8 (6.3) | 4 (6.3) | 0.975d) |
| IIA | 6 (3.2) | 4 (3.2) | 2 (3.2) | |
| IIB | 108 (57.1) | 72 (57.1) | 36 (57.1) | |
| IIIA | 1 (0.5) | 1 (0.8) | 0 | |
| IIIB | 59 (31.2) | 39 (31.0) | 20 (31.7) | |
| IVB | 3 (1.6) | 2 (1.6) | 1 (1.6) | |
| Hemoglobin (g/dL) | 12.8±2.04 | 12.9±2.02 | 12.7±2.05 | 0.574b) |
| Histology | ||||
| Squamous cell carcinoma | 157 (83.1) | 102 (81.0) | 55 (87.3) | 0.536d) |
| Adenocarcinoma | 23 (12.2) | 17 (13.5) | 6 (9.5) | |
| Adenosquamous carcinoma | 9 (4.8) | 7 (5.6) | 2 (3.2) | |
| Comorbidities | ||||
| Number | 1.24±0.48 | 1.23±0.50 | 1.26±0.44 | 0.051b) |
| Comorbidities=1 | 148 (78.3) | 102 (80.9) | 46 (73.9) | 0.212d) |
| Comorbidities ≥ 2 | 41 (21.6) | 24 (19.0) | 17 (26.9) | |
| T2DM | 89 (46.8) | 57 (45.2) | 32 (50.8) | < 0.001d) |
| SAH | 112 (58.9) | 81 (64.3) | 31 (49.2) | |
| Acute kidney injury | 19 (10.0) | 14 (11.1) | 5 (7.9) | |
| Other | 15 (7.9) | 3 (2.4) | 12 (19.0) | |
| Response rates f) | ||||
| Complete response | 165 (87.3) | 109 (86.5) | 56 (88.9) | 0.094d) |
| Partial response | 9 (4.7) | 4 (3.2) | 5 (7.9) | |
| Disease progression | 15 (7.9) | 13 (10.3) | 2 (3.2) | |
| Pattern of failure | ||||
| Local | 12 (6.3) | 7 (5.5) | 5 (7.9) | 0.917d) |
| Locoregional | 9 (4.7) | 6 (4.7) | 3 (4.7) | |
| Distant metastasis | 35 (18.5) | 22 (17.4) | 13 (20.6) | |
| Locoregional+distant metastasis | 16 (8.4) | 14 (11.1) | 2 (3.1) | |
| Persistent disease | 13 (6.8) | 10 (7.9) | 3 (4.7) | |
Values are presented as mean±SD or number (%). SAH, systemic arterial hypertension; SD, standard deviation; T2DM, type 2 diabetes mellitus.
Kolmogorov-Smirnov test (normal distribution is assumed),
Student T test for independent samples,
Assessed according to the Eastern Cooperative Oncology Group (ECOG),
Chi-square test,
According to the International Federation of Gynecology and Obstetrics (2008),
Assessed by Response Evaluation Criteria in Solid Tumors (v1.1).
2. Treatment characteristics
Regarding the treatment received, we did not find statistically significant differences among groups in the number of CT cycles, total RT dose (78.7 Gy vs. 79.8 Gy), protraction time (75.4 days vs. 76.8 days), and the type of established brachytherapy (high rate, 53.2% vs. 55.6% and low rate, 46.8% vs. 44.4%) for CDDP and gemcitabine, respectively (S1 Table).
3. RRs and survival
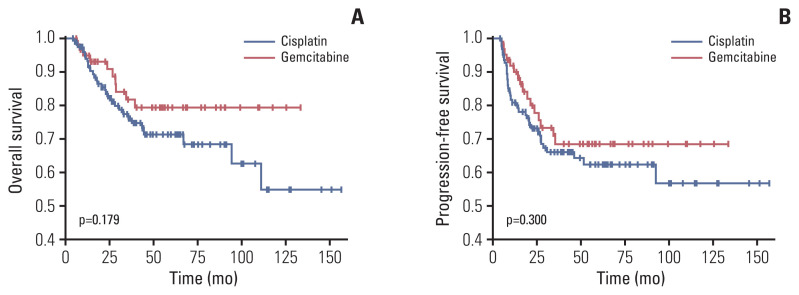
A complete response (CR) was presented in approximately 87.3% patients—with no significant differences among groups (p=0.094) (Table 1). The pattern of failure was similar among treatment groups (p=0.9) (Table 1), distant metastasis was the most frequent pattern of failure, in 18.5% patients. There were no significant differences in OS among cisplatin and gemcitabine groups (Fig. 2A). Similarly, in PFS no significant differences were observed among treatment groups (Fig. 2B).
Fig. 2.
(A) Overall survival of patients treated with gemcitabine (red line) and patients treated with cisplatin (blue line). Overall survival was estimated by the Kaplan-Meier method, using log-rank. (B) Progression-free survival of patients treated with gemcitabine (red line) and patients treated with cisplatin (blue line). Progression-free survival was estimated by the Kaplan-Meier method, using log-rank.
4. Renal toxicities and function
No treatment-related deaths were recorded. Statistically significant differences were observed in adverse events presented by patients in each treatment group. In the cisplatin group, neutropenia, leukopenia, lymphopenia, and neuropathy occurred more frequently—hematologic toxicity was more severe, with G3–4 in 43% of cases. In the group treated with gemcitabine, vomiting, constipation, diarrhea, fever, fatigue and non-infectious cystitis were more frequent—gastrointestinal toxicity being the most prevalent and severe, with G3–4 in 12% of cases (Table 2).
Table 2.
Acute toxicity according to treatment groupsa)
| Toxicity | Cisplatin (n=126) | Gemcitabine (n=63) | p-valueb) | ||
|---|---|---|---|---|---|
|
|
|
||||
| G1–2 | G3–4 | G1–2 | G3–4 | ||
| Neutropenia | 57 (45.2) | 7 (5.5) | 24 (38.0) | 4 (6.3) | 0.646 |
|
| |||||
| Leukopenia | 98 (77.7) | 13 (10.3) | 29 (46.0) | 3 (4.8) | < 0.001 |
|
| |||||
| Lymphopenia | 70 (55.5) | 35 (27.8) | 9 (14.3) | 1 (1.6) | < 0.001 |
|
| |||||
| Anemia | 22 (17.4) | - | 11 (17.4) | 2 (3.2) | 0.132 |
|
| |||||
| Thrombocytopenia | 7 (5.5) | - | 4 (6.3) | - | 0.530 |
|
| |||||
| Nausea | 110 (87.3) | 7 (5.6) | 59 (93.6) | - | 0.155 |
|
| |||||
| Vomit | 69 (54.7) | 4 (3.2) | 49 (77.7) | - | 0.003 |
|
| |||||
| Constipation | 14 (11.1) | - | 18 (28.5) | - | 0.003 |
|
| |||||
| Diarrhea | 63 (50.0) | 5 (4.0) | 44 (69.8) | 8 (12.7) | < 0.001 |
|
| |||||
| Pruritus | 3 (2.4) | - | 3 (4.7) | - | 0.318 |
|
| |||||
| Fever | 3 (2.4) | - | 11 (17.5) | - | < 0.001 |
|
| |||||
| Neuropathy | 8 (6.3) | - | 1 (1.6) | - | 0.047 |
|
| |||||
| Cephalea | 9 (7.1) | - | 5 (7.9) | - | 0.522 |
|
| |||||
| Anorexia | 3 (2.4) | - | 3 (4.7) | 1 (1.6) | 0.244 |
|
| |||||
| Fatigue | 71 (56.3) | - | 55 (87.3) | 1 (1.6) | < 0.001 |
|
| |||||
| Edema | 2 (1.6) | - | 5 (7.9) | - | 0.042 |
|
| |||||
| Abdominal pain | 37 (29.3) | - | 27 (42.8) | - | 0.065 |
|
| |||||
| Non-infectious cystitis | 23 (18.2) | 1 (0.8) | 27 (42.8) | - | 0.001 |
|
| |||||
| Proctitis | 14 (11.1) | 10 (7.9) | 4 (6.3) | 3 (4.8) | 0.381 |
|
| |||||
| Dermal toxicity | 14 (11.1) | 1 (0.8) | 3 (4.7) | 1 (1.6) | 0.516 |
Values are presented as number (%).
Assessed by Common Terminology Criteria for Adverse Events (v.4.03),
Chi-square test.
The analysis of the change in GFR (pretreatment vs posttreatment at 1-year follow-up) revealed a statistically significant decrease in GFR in the cisplatin group, while in the gemcitabine group the baseline GFR was maintained in the posttreatment evaluation. When comparing the change in GFR between groups, differences were observed (Table 3). It is relevant to highlight that there were no statistically significant differences in the change in GFR when we compared pre-treatment vs immediate posttreatment, among treatment groups (CDDP −1.9 vs. gemcitabine −0.7; p=0.35).
Table 3.
Change in glomerular filtration rate a) by treatment groups
| Treatment group | Pre-treatment | Post-treatment (1 year) | ΔGFR | p-valueb) |
|---|---|---|---|---|
| Cisplatin | 94.5 | 90.9 | −3.6 | 0.002 |
| Gemcitabine | 93.2 | 95.1 | +1.9 | 0.667 |
| p=0.025c) |
GFR, glomerular filtrationrate.
Assessed with the Chronic Kidney Disease Epidemiology Collaboration formula (mL/min/1.73 m2),
Wilcoxon test,
Difference between groups, Mann-Whitney U test.
A multivariate analysis was performed through logistic regression (Table 4). The model included the following variables: type of treatment, number of comorbidities, clinical stage and age. Only the type of treatment correlated with the change in GFR (odds ratio, 2.425; p=0.012). In this study, we found that treatment with CDDP increases 1.42 times the risk of reducing GFR compared to gemcitabine.
Table 4.
Multivariate analysis of variables associated with change in GFRa)
| Variable | OR | 95% CI | p-value |
|---|---|---|---|
| Type of treatment | |||
| Gemcitabine | 1 (reference) | ||
| Cisplatin | 2.425 | 1.211–4.858 | 0.012 |
| No. of comorbidities | |||
| 1 | 1 (reference) | ||
| ≥ 2 | 0.659 | 0.301–1.444 | 0.298 |
| Clinical stage | |||
| IB2, IIA, IIB | 1 (reference) | ||
| IIIA, IIIB, IVB | 1.446 | 0.718–2.912 | 0.301 |
| Age | 0.975 | 0.946–1.004 | 0.095 |
CI, confidence interval; GFR, glomerular filtrationrate; OR, odds ratio.
Assessed with the Chronic Kidney Disease Epidemiology Collaboration formula (mL/min/1.73 m2).
Discussion
In Mexico, CC continues to be a major health problem. Our report establishes that treatment with gemcitabine in LACC patients with comorbidities has similar response and survival rates as standard treatment with CDDP, but with a different toxicity profile. The main toxicities associated with cisplatin were hematological (neutropenia, leukopenia, and lymphopenia), while for gemcitabine they were gastrointestinal (vomiting, constipation and diarrhea). Strategies to reduce the toxicity effects of treatment were performed. During the concomitance, each patient underwent complete clinical evaluations and determination of biochemical laboratory parameters on a weekly basis, prior to the subsequent administration of CT. In case of documenting a grade 2–3 adverse event, treatment dose adjustment was performed (a reduction of 25% of the total dose), and in the event of neutropenia, colony stimulating factor was used as prophylaxis for the next CT cycle.
Gemcitabine treatment did not impair GFR, while cisplatin CT-RT was associated with a significant decrease in renal function at one year of follow-up. This research establishes gemcitabine as an alternative regimen to cisplatin in patients at risk of presenting dose-limiting nephrotoxicity.
These data are novel, because to our knowledge there are no studies that compare these treatment schemes in this population group; however, we recognize that the main limitations of this study lie in its retrospective nature, to homogenize the sample a pairing of variables, such as age and clinical stage, was performed.
The number of comorbidities present in cancer patients is related to lower OS [22] and greater toxicity associated with CT treatment. Although there is general agreement that comorbidities are more prevalent among cancer patients, the magnitude is difficult to assess. In their review of the impact of comorbidities on CT use and outcomes in patients with solid tumors, Lee et al. [23] reported a wide range of prevalence of comorbidities from 0.4% to 90%. Yancik [24], in an American demographic study of more than 7,600 people with cancer, found that patients between 55–64 years had 2.9 comorbidities, with hypertension in 42% and T2DM in 12%. In our study, with a mean age of 56.3 years, there were 1.24 comorbidities—the most prevalent being SAH in 58% and T2DM in 46%. These discrepancies in the figures could be due to the fact that the prevalence of the comorbidity measured varies, depending on the source and the measurement instrument used, the study population and the type of cancer [25]. Mizuno et al. [7], evaluated approximately 1,700 cancer patients treated with systemic CDDP, finding that the main risk factors for nephrotoxicity were cardiovascular disease (RR, 3.61) and T2DM (RR, 3.45).
CT with CDDP concomitantly with radiotherapy has been the standard of treatment in LACC in the last two decades; however, renal toxicity can cause kidney damage [8]. Mathe et al. [8] reported that in patients with lung cancer treated with CDDP, in the presence of comorbidities (SAH and T2DM), a deterioration of GFR was observed, when compared with patients without comorbidities. However, Ferrandina et al. [26] reported that associated comorbidities in LACC patients treated with preoperative CT-RT did not negatively impact PFS and OS, this could be explained because the subgroup of patients with comorbidities was only 11%. Our study confirms a statistically significant reduction in GFR with CDDP at one year of follow-up, not being the case with treatment with gemcitabine.
Gemcitabine is a potent radiosensitizer in CC cell lines, and concomitant treatment with gemcitabine and radiotherapy has been shown to be effective [17–20]. Pattarranutaporn et al. [17]. conducted a study with gemcitabine at 300 mg/m2 weekly, obtaining CR rates of 89%. The efficacy of gemcitabine has also been tested in patients with comorbidities and/or with established renal impairment, confirming its safety. Cetina et al. [20] conducted a pilot study in patients with renal failure associated with ureteral obstruction, which assessed the use of concomitant gemcitabine at a dose of 300 mg/m2 weekly, obtaining 89% CR, with adequate safety. In our study, the CR rates in both treatment groups were not statistically different, 86.5% in the CDDP group and 88.9% in the gemcitabine group. This is similar to what was reported in the referred studies carried out in patients without comorbidities and with comorbidities. It is important to note that the complete RR was defined by imaging studies—using the RECIST v1.1 [27]—at the follow-up visit, 2 months after RT treatment completion. The imaging studies performed included either abdominopelvic computed tomography, MRI, or both.
The present study was based on the assumption that concomitant gemcitabine treatment would reduce the risk of renal toxicity compared to CDDP, while this is true, our results reveal a different toxicity profile for each treatment. The gemcitabine group more frequently presented gastrointestinal toxicity with vomiting in 77.8% of cases, constipation in 28.6%, and diarrhea in 82.6%; with a G3–4 gastrointestinal toxicity of 12%. The presence of fatigue was also frequent (88.9%). The most common acute toxicities that have been documented in a population without comorbidities are nausea and vomiting in 70% and diarrhea in 15%–20%, generally G1–2. Pattaranutaporn et al. [17], in a study of 19 patients, reported nausea and vomiting in 42% and diarrhea in 47% of patients, with G3–4 in only 5% of cases. The gastrointestinal toxicity reported by Verma et al. [18] in 20 patients was nausea/vomiting in 35% and diarrhea in 70%; with G3–4 for 25% patients. Also, in a population with comorbidities, Cetina et al. [20] reported fatigue in 88% patients and nausea/vomiting in all patients, the latter being G3–4 in 55%.
In our study, we observed that cisplatin reduces GFR by 3.6 mL/min in 59% of the sample, while treatment with gemcitabine shows an improvement in GFR of 1.9 mL/min in 61% of the sample. In a multivariate logistic regression analysis, it was observed that only the type of treatment correlates with the change in GFR. These data are in agreement with the article published by Venook et al. [28] who found that the administration of gemcitabine is safe even in patients with high creatinine levels and does not require dose adjustment.
It is relevant to highlight that there were no differences in GFR immediately after treatment, these were observed after 1 year, and could be justified due to the late toxicity associated with RT [29]. This incidence of RT-associated kidney injury tends to be unreported due to its long latency. If no changes in GFR are seen within 2 years after RT, subsequent chronic injury is unlikely [29].
The main toxicity limiting dose of CDDP is nephrotoxicity, therefore, its choice as a radiosensitizer requires a careful evaluation of renal function before deciding on its administration. Clinically, nephrotoxicity caused by this CT manifests as a lower GFR, it is believed that it can lead to a subclinical but permanent reduction in GFR [30]. The presence of comorbidities as T2DM and history of cardiovascular disease are risk factors for developing long-term nephrotoxicity [7].
We can conclude that in LACC patients with comorbidities, gemcitabine vs. CDDP has the same efficacy, with a different toxicity profile. Gemcitabine-associated toxicities were well tolerated. Treatment with cisplatin is associated with a significant decrease in GFR during follow-up, compared to treatment with gemcitabine.
These results are promising, which is why it is necessary to carry out double-blind randomized clinical trials to confirm that the application of gemcitabine presents similar survival and RRs, and to evaluate its safety profile, with emphasis on renal toxicity. In this way, gemcitabine can be established as an option to consider where there is a contraindication to the application of cisplatin.
Footnotes
Ethical Statement
The local Ethics and Research Committees approved the study (No. 2019/0021). This is a retrospective study, approved by the Ethics and Research Comittees. For this retrospective study, the informed consent from the patient was not required. All the information used in this study was collected from the medical records. However, all patients that undergo cancer treatment at our Institution sign an infomed consent, in which they express their agreement to receive the treatment proposed by their physician.
Author Contributions
Conceived and designed the analysis: Cetina-Pérez L.
Collected the data: Brau-Figueroa H, Arango-Bravo E, Galicia-Carmona T, Abraham Lugo-Alferez L.
Contributed data or analysis tools: Brau-Figueroa H, Jiménez-Lima R.
Performed the analysis: Brau-Figueroa H, Arango-Bravo E, Castro-Eguiluz D.
Wrote the paper: Brau-Figueroa H, Arango-Bravo E, Castro-Eguiluz D.
Manuscript editing: Castro-Eguiluz D.
Guarantor of integrity of study: Cruz-Bautista I.
Conflicts of Interest
Conflict of interest relevant to this article was not reported.
Electronic Supplementary Material
Supplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Rizo Ríos P, Sierra Colindres MI, Vázquez Pinon G, Cano Guadiana MC, Meneses Garcia A, Mohar A. Cancer hospital registry: cancer compendium 2000–2004. Cancerologia. 2007;2:208–87. [Google Scholar]
- 3.Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340:1144–53. doi: 10.1056/NEJM199904153401502. [DOI] [PubMed] [Google Scholar]
- 4.Datta NR, Stutz E, Liu M, Rogers S, Klingbiel D, Siebenhuner A, et al. Concurrent chemoradiotherapy vs. radiotherapy alone in locally advanced cervix cancer: a systematic review and meta-analysis. Gynecol Oncol. 2017;145:374–85. doi: 10.1016/j.ygyno.2017.01.033. [DOI] [PubMed] [Google Scholar]
- 5.Tan LT, Zahra M. Long-term survival and late toxicity after chemoradiotherapy for cervical cancer: the Addenbrooke’s experience. Clin Oncol (R Coll Radiol) 2008;20:358–64. doi: 10.1016/j.clon.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Niho S, Yamanaka T, Umemura S, Matsumoto S, Yoh K, Goto K, et al. Renal toxicity caused by brand-name versus generic cisplatin: a comparative analysis. Jpn J Clin Oncol. 2013;43:390–5. doi: 10.1093/jjco/hyt020. [DOI] [PubMed] [Google Scholar]
- 7.Mizuno T, Ishikawa K, Sato W, Koike T, Kushida M, Miyagawa Y, et al. The risk factors of severe acute kidney injury induced by cisplatin. Oncology. 2013;85:364–9. doi: 10.1159/000356587. [DOI] [PubMed] [Google Scholar]
- 8.Mathe C, Bohacs A, Duffek L, Lukacsovits J, Komlosi ZI, Szondy K, et al. Cisplatin nephrotoxicity aggravated by cardiovascular disease and diabetes in lung cancer patients. Eur Respir J. 2011;37:888–94. doi: 10.1183/09031936.00055110. [DOI] [PubMed] [Google Scholar]
- 9.Zhao L, Leung LH, Wang J, Li H, Che J, Liu L, et al. Association between Charlson comorbidity index score and outcome in patients with stage IIIB–IV non-small cell lung cancer. BMC Pulm Med. 2017;17:112. doi: 10.1186/s12890-017-0452-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 11.Romero-Martinez M, Shamah-Levy T, Vielma-Orozco E, Heredia-Hernandez O, Mojica-Cuevas J, Cuevas-Nasu L, et al. National Health and Nutrition Survey 2018–19: methodology and perspectives. Salud Publica Mex. 2019;61:917–23. doi: 10.21149/11095. [DOI] [PubMed] [Google Scholar]
- 12.Nam EJ, Lee M, Yim GW, Kim JH, Kim S, Kim SW, et al. Comparison of carboplatin- and cisplatin-based concurrent chemoradiotherapy in locally advanced cervical cancer patients with morbidity risks. Oncologist. 2013;18:843–9. doi: 10.1634/theoncologist.2012-0455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coronel JA, Cetina Ldel C, Cantu D, Cerezo O, Hernandez CS, Rivera L, et al. A randomized comparison of cisplatin and oral vinorelbine as radiosensitizers in aged or comorbid locally advanced cervical cancer patients. Int J Gynecol Cancer. 2013;23:884–9. doi: 10.1097/IGC.0b013e3182915c69. [DOI] [PubMed] [Google Scholar]
- 14.Csoka K, Liliemark J, Larsson R, Nygren P. Evaluation of the cytotoxic activity of gemcitabine in primary cultures of tumor cells from patients with hematologic or solid tumors. Semin Oncol. 1995;22:47–53. [PubMed] [Google Scholar]
- 15.McCormack M, Thomas H. A phase Ib study of gemcitabine (GEM) and concurrent radiotherapy (RT) in carcinoma of the cervix. Ann Oncol. 2000;11(Suppl 4):88–9. [Google Scholar]
- 16.Boualga K, Aksil N, Ayad M, Hasnaoui N, Moussaoui D. Phase I/II study of gemcitabine (GEM) and concomitant radiotherapy (RT) in locally advanced carcinoma of the cervix (LACC) J Clin Oncol. 2005;23(16 Suppl):5142. [Google Scholar]
- 17.Pattaranutaporn P, Thirapakawong C, Chansilpa Y, Therasakvichya S, Ieumwananontachai N, Thephamongkhol K. Phase II study of concurrent gemcitabine and radiotherapy in locally advanced stage IIIB cervical carcinoma. Gynecol Oncol. 2001;81:404–7. doi: 10.1006/gyno.2001.6197. [DOI] [PubMed] [Google Scholar]
- 18.Verma AK, Arya AK, Kumar M, Kumar A, Gupta S, Sharma D, et al. Weekly cisplatin or gemcitabine concomitant with radiation in the management of locally advanced carcinoma cervix: results from an observational study. J Gynecol Oncol. 2009;20:221–6. doi: 10.3802/jgo.2009.20.4.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kundu S, Basu S, Acharya S, Dastidar A, Roy A. Chemoradiation in locally advanced cervical cancer: a randomized trial. Indian J Med Paediatr Oncol. 2008;29:12–8. [Google Scholar]
- 20.Cetina L, Rivera L, Candelaria M, de la Garza J, Duenas-Gonzalez A. Chemoradiation with gemcitabine for cervical cancer in patients with renal failure. Anticancer Drugs. 2004;15:761–6. doi: 10.1097/00001813-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL., Jr Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004;291:2441–7. doi: 10.1001/jama.291.20.2441. [DOI] [PubMed] [Google Scholar]
- 23.Lee L, Cheung WY, Atkinson E, Krzyzanowska MK. Impact of comorbidity on chemotherapy use and outcomes in solid tumors: a systematic review. J Clin Oncol. 2011;29:106–17. doi: 10.1200/JCO.2010.31.3049. [DOI] [PubMed] [Google Scholar]
- 24.Yancik R. Cancer burden in the aged: an epidemiologic and demographic overview. Cancer. 1997;80:1273–83. [PubMed] [Google Scholar]
- 25.Sarfati D, Koczwara B, Jackson C. The impact of comorbidity on cancer and its treatment. CA Cancer J Clin. 2016;66:337–50. doi: 10.3322/caac.21342. [DOI] [PubMed] [Google Scholar]
- 26.Ferrandina G, Lucidi A, Paglia A, Corrado G, Macchia G, Tagliaferri L, et al. Role of comorbidities in locally advanced cervical cancer patients administered preoperative chemoradiation: impact on outcome and treatment-related complications. Eur J Surg Oncol. 2012;38:238–44. doi: 10.1016/j.ejso.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 27.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–47. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 28.Venook AP, Egorin MJ, Rosner GL, Hollis D, Mani S, Hawkins M, et al. Phase I and pharmacokinetic trial of gemcitabine in patients with hepatic or renal dysfunction: Cancer and Leukemia Group B 9565. J Clin Oncol. 2000;18:2780–7. doi: 10.1200/JCO.2000.18.14.2780. [DOI] [PubMed] [Google Scholar]
- 29.Dawson LA, Kavanagh BD, Paulino AC, Das SK, Miften M, Li XA, et al. Radiation-associated kidney injury. Int J Radiat Oncol Biol Phys. 2010;76:S108–15. doi: 10.1016/j.ijrobp.2009.02.089. [DOI] [PubMed] [Google Scholar]
- 30.Pabla N, Dong Z. Cisplatin nephrotoxicity: mechanisms and renoprotective strategies. Kidney Int. 2008;73:994–1007. doi: 10.1038/sj.ki.5002786. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.